神戸市の基幹病院である当院には、外科手術を必要とする患者さんが数多く来院されます。当科では、これらの患者さん皆様に質の高く安心した医療を提供できるよう、様々なことに積極的に取り組んでいます。
患者さん一人一人に優しい治療
我々の扱う疾患の多くが悪性疾患(癌)です。癌に対する手術は、癌そのものだけでなく周りの組織も含めて広く切除する根治手術が必要ですので、患者さんの体に対する負担は非常に大きくなります。また切除されたことによる臓器の機能の低下を免れることはできません。ですから、外科手術の必要性を決定するには慎重な判断が必要で、当院では外科のみならず癌診療に携わる全ての診療科(消化器内科、腫瘍内科、放射線科、緩和医療部門、病理診断部門)との連携を密に取ることにより、患者さんの状況に応じた最もふさわしい治療が行えるような体制を整えております。そして、手術が必要であると判断された患者さんは、その背景や症状、病気の進み具合(進行度)に応じて術後のQOLを考えつつ、多職種で術式を検討したうえで、ご本人やそのご家族と相談、同意を得て治療方針を決定しています。手術の前にやさしくていねいに説明を繰り返し十分なインフォームド・コンセントを得ることはもっとも大切なこととらえております。また、他の医師の意見が聞きたい場合はセカンドオピニオンを受けることも可能です。
最新の知識と技術を取り入れた高度、かつ安全な癌治療
近年、癌に対する研究が進むにつれ、その診断や手術を含む治療法が細分化され、医師はより専門的な知識や技術が必要とされてきています。当院の外科スタッフは全員、外科学会認定医/専門医/指導医、または消化器外科専門医/指導医の資格を持った経験豊富な医師です。さらに高度な専門医資格として内視鏡外科学会技術認定医:6名、肝胆膵外科高度技能指導医/専門医:3名、移植外科学会認定医、食道学会専門医を各1名、を有しています。また近年発達の目覚ましいロボット手術(DaVinci)は10名が執刀医としての資格を持っており、さらにうち5名が指導医資格も有しております。このように各自がそれぞれの専門分野を生かし、高度でかつ安全な最良の医療を患者さんに提供します。また国内外の学会に積極的に参加して最新の知識や技術を吸収することにより、最高峰の治療レベルの維持を心がけています。
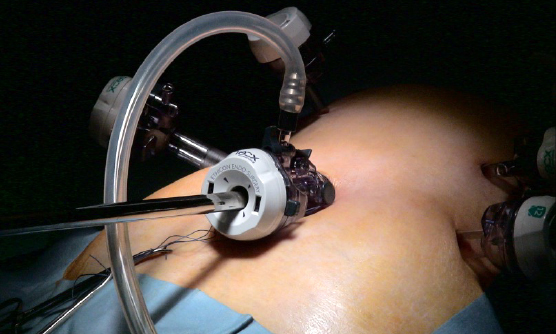
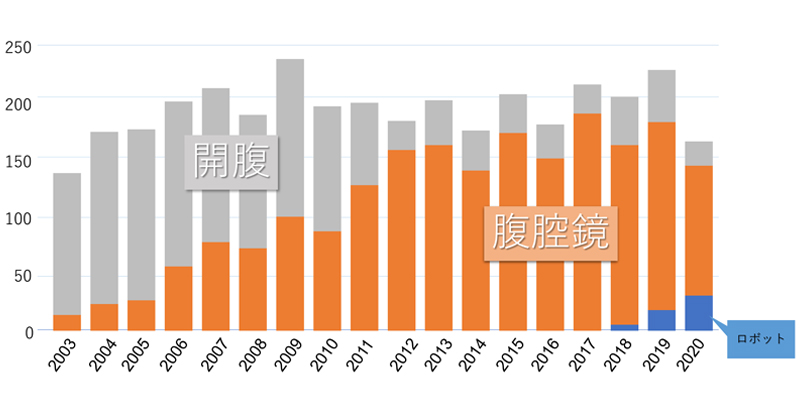
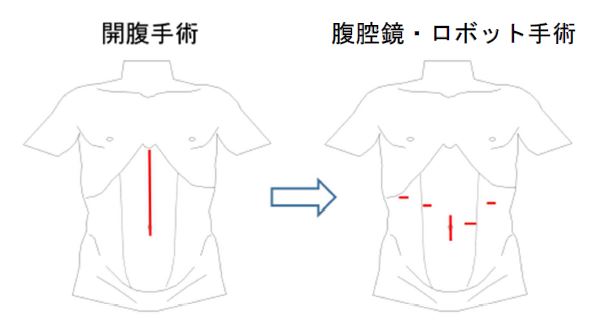
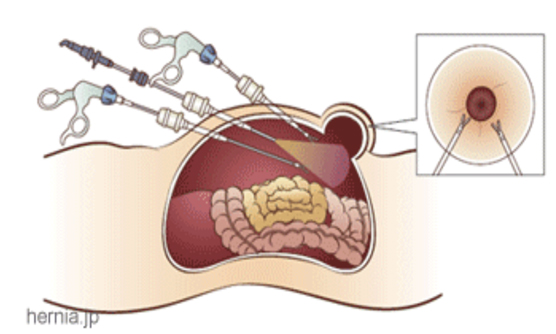
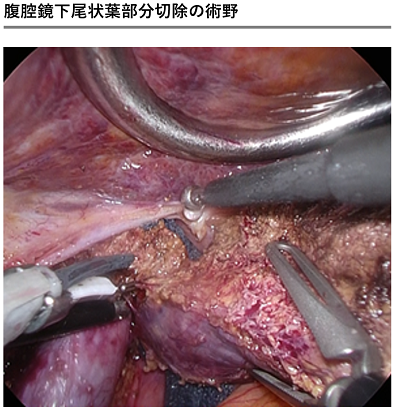
腹腔鏡の手術は、従来の開腹手術と比べると体に対する負担が小さく術後の回復が早いのが大きな特徴ですが、一方で高度な技術を要する手術です。当科では、腹腔鏡手術の高度な技術を持つと認められた内視鏡外科学会技術認定医が中心となり、腹腔鏡下手術を大幅に取り入れています。胆石症は言うに及ばず、食道癌、胃癌、大腸癌、肝臓癌、膵臓癌、などほぼ全ての悪性疾患から、鼠径ヘルニアや虫垂切除術、胃十二指腸潰瘍穿孔などの緊急手術まで多くの疾患に行っています。また近年はロボット手術の手術数も飛躍的に増加してきており、より体に負担の少ない高度な医療を提供しています(☞別項参照)。このことは、患者さんへの負担を軽減するとともに入院期間の短縮に大きく貢献しています。
一方で、肝臓癌、膵臓癌などの最も難易度が高くより専門的な知識や技術、経験が必要な手術についても、肝胆膵外科高度技能指導医/専門医の資格を持つ経験豊富な医師が担当となり数多く治療にあたっています。また大学病院以外では珍しく、生体肝臓移植も行っています。
神戸市の基幹病院としての断らない医療の実践
当院は神戸市民の救急医療の最後の砦(とりで)という意識のもと、断らない医療をスローガンとして掲げています。当科もその方針に従い、日中/夜間を問わずベテランスタッフ医師と若手医師がペアーとなり24時間/365日待機する体制をとり、年間に約300例と数多くの緊急手術を行っています。また、多発外傷や複雑な損傷を伴う場合は他診療科との協力で緊急手術を行うこともあり、救急部や他の診療科との連携を密に取りながら一緒に診療にあたる体制を整えております。
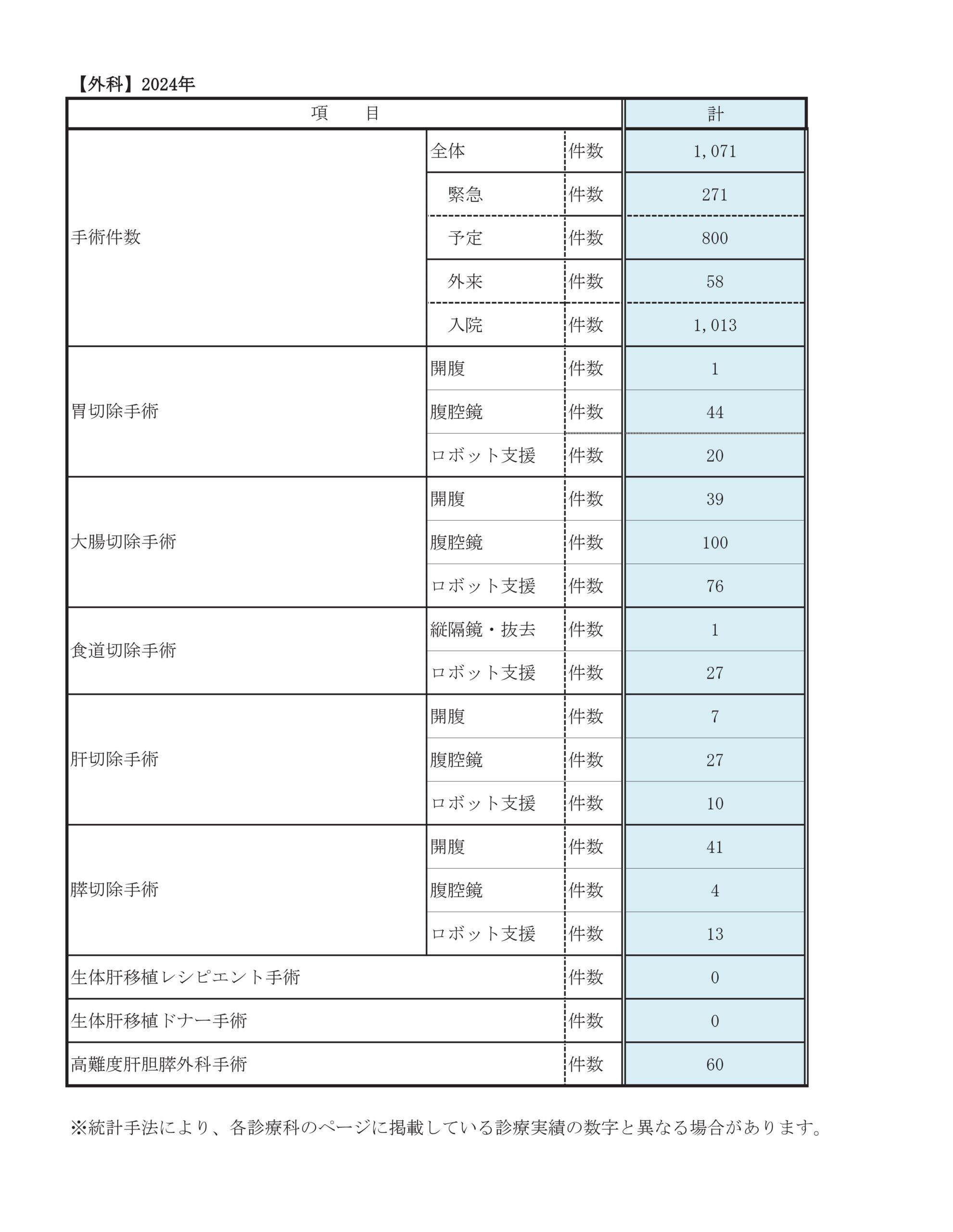
診療実績
このページでは外科消化器外科での手術数の統計をお示しします。
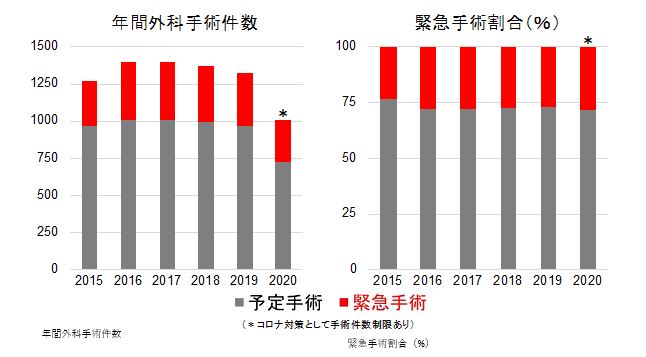
年間手術件数
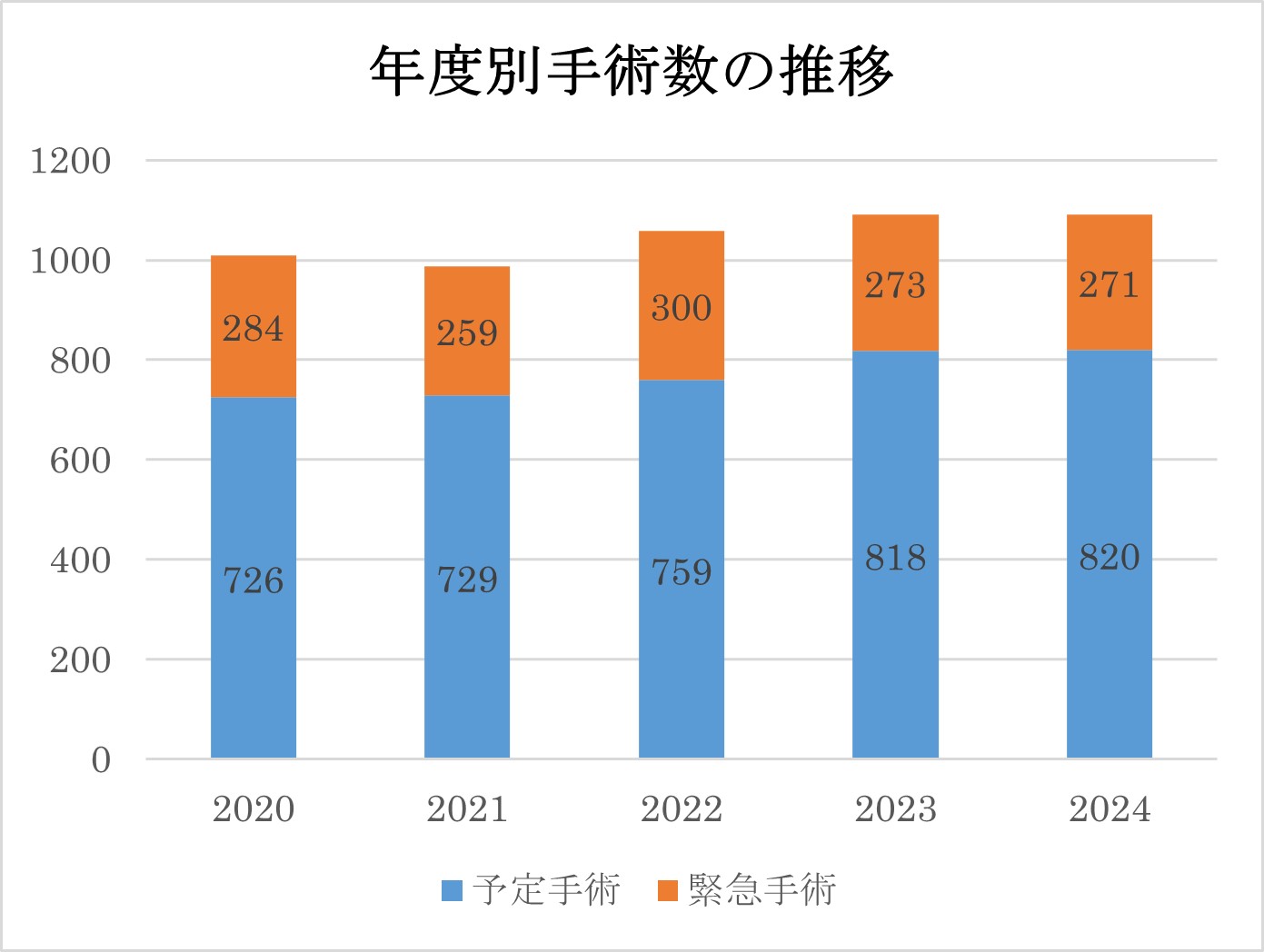
年間手術件数は毎年1300-1400件で推移していました。しかし2020年に新型コロナ感染症の治療に伴う通常診療の制限により予定手術・緊急手術ともに大きく減少いたしましたが、それ以降徐々に回復してきています(内訳は次章を参照ください)。
臓器別手術件数
| 2020年 | 2021年 | 2022年 | 2023年 | 2024年 | |
| 食道 | 22 | 21 | 20 | 17 | 32 |
|---|---|---|---|---|---|
| 胃十二指腸 | 95 | 63 | 71 | 76 | 66 |
| 結腸 | 153 | 124 | 157 | 132 | 166 |
| 直腸 | 43 | 58 | 59 | 65 | 49 |
| 肝胆道 | 73 | 58 | 59 | 61 | 49 |
| 肝臓移植 | 0 | 0 | 0 | 0 | 0 |
| 膵臓 | 51 | 48 | 51 | 43 | 58 |
| 胆嚢 | 155 | 173 | 164 | 183 | 161 |
| 虫垂 | 84 | 62 | 95 | 85 | 89 |
| ヘルニア | 100 | 126 | 110 | 122 | 124 |
| イレウス | 32 | 43 | 42 | 42 | 38 |
腹腔鏡手術について
当院では低侵襲手術としての腹腔鏡下手術およびロボット手術を積極的に取り入れております。内視鏡外科学会より腹腔鏡手術の技術を認定された『内視鏡外科技術認定医』の資格を持つスタッフ医師が中心となり、腹腔鏡手術を安全かつ確実に行う体制を整えています。またロボット手術ではロボット手術の指導医5名の指導の下で手術を行っています。
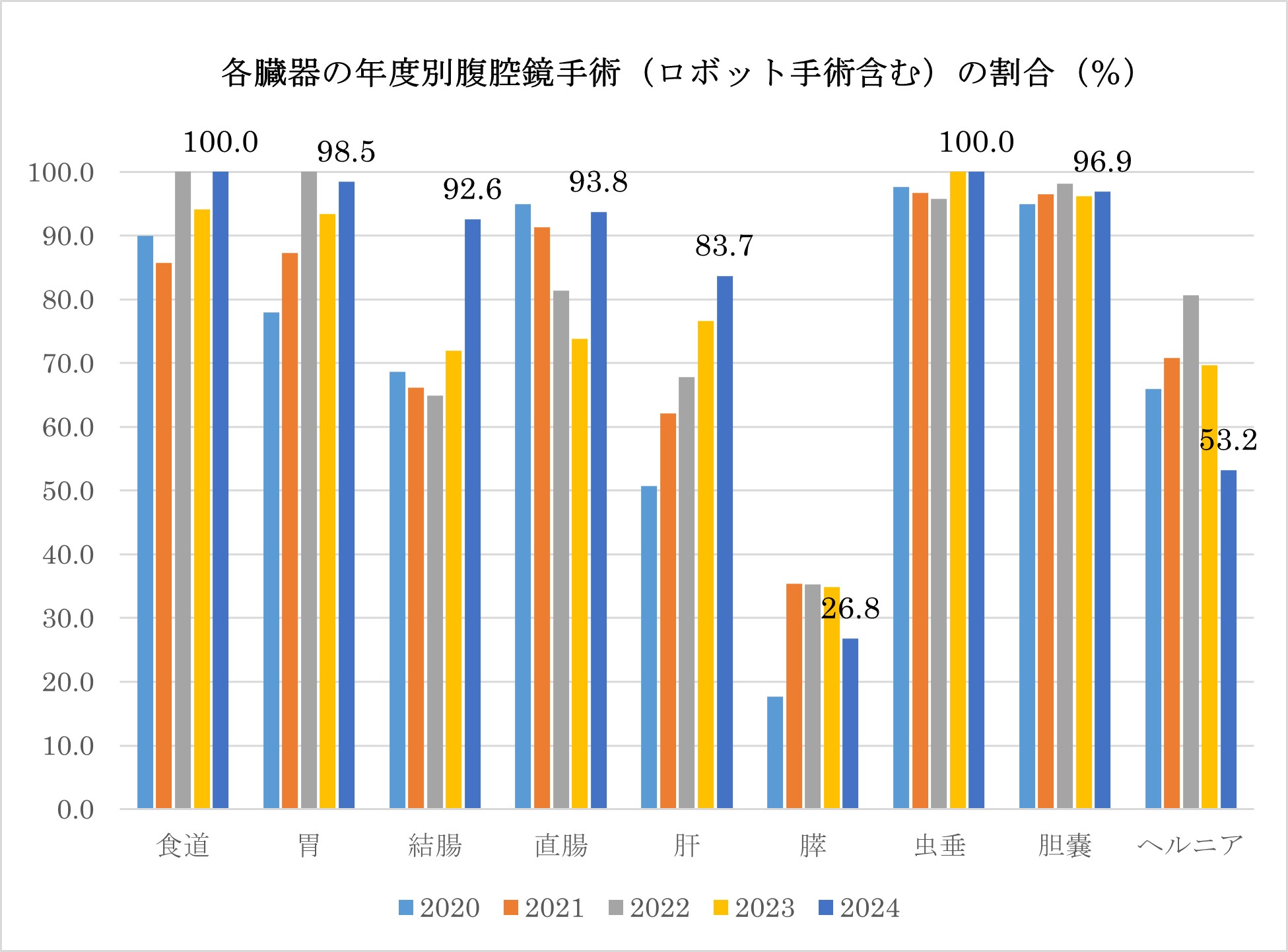
腹腔鏡/ロボットによる低侵襲手術症例の占める割合を臓器別にグラフで示します。①消化管の手術は緊急手術を除けば、ほぼ全例が腹腔鏡/ロボットによる低侵襲手術であること、②肝臓の腹腔鏡/ロボットによる低侵襲手術割合が増加してきていること、が特徴です。 また近年はロボット手術も増加してきております。
(「外科におけるロボット支援(ダヴィンチ)手術に関して」を参照ください。)
肝胆膵高度技能対象疾患
肝臓、膵臓、胆道の悪性疾患(癌)の手術は難易度の高い手術です。そこで『日本肝胆膵外科学会』が肝臓、膵臓、胆道の癌手術に関して高度な設備・技術水準を有する施設、高度な手術手技を有する医師、を認定する基準を作成しております。そしてこれらの基準に基づいた審査の結果、当院は『肝胆膵高度技能認定施設』の中でも最も取得の困難な『A群』に認定されております。また『肝胆膵高度技能指導医または専門医』が3名在籍しており、これら医師が中心となり肝臓、膵臓、胆道の癌手術を積極的に行っております。
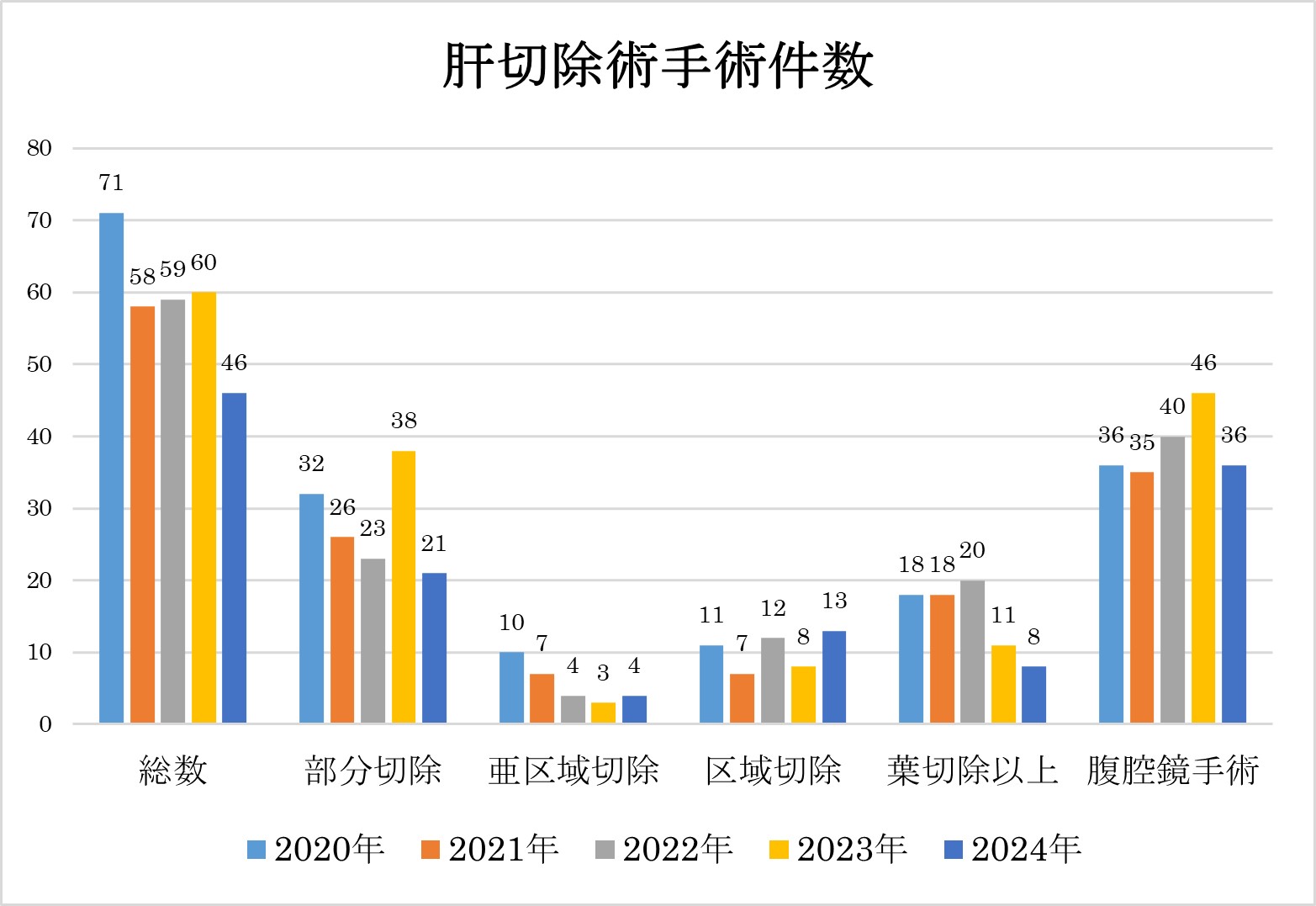
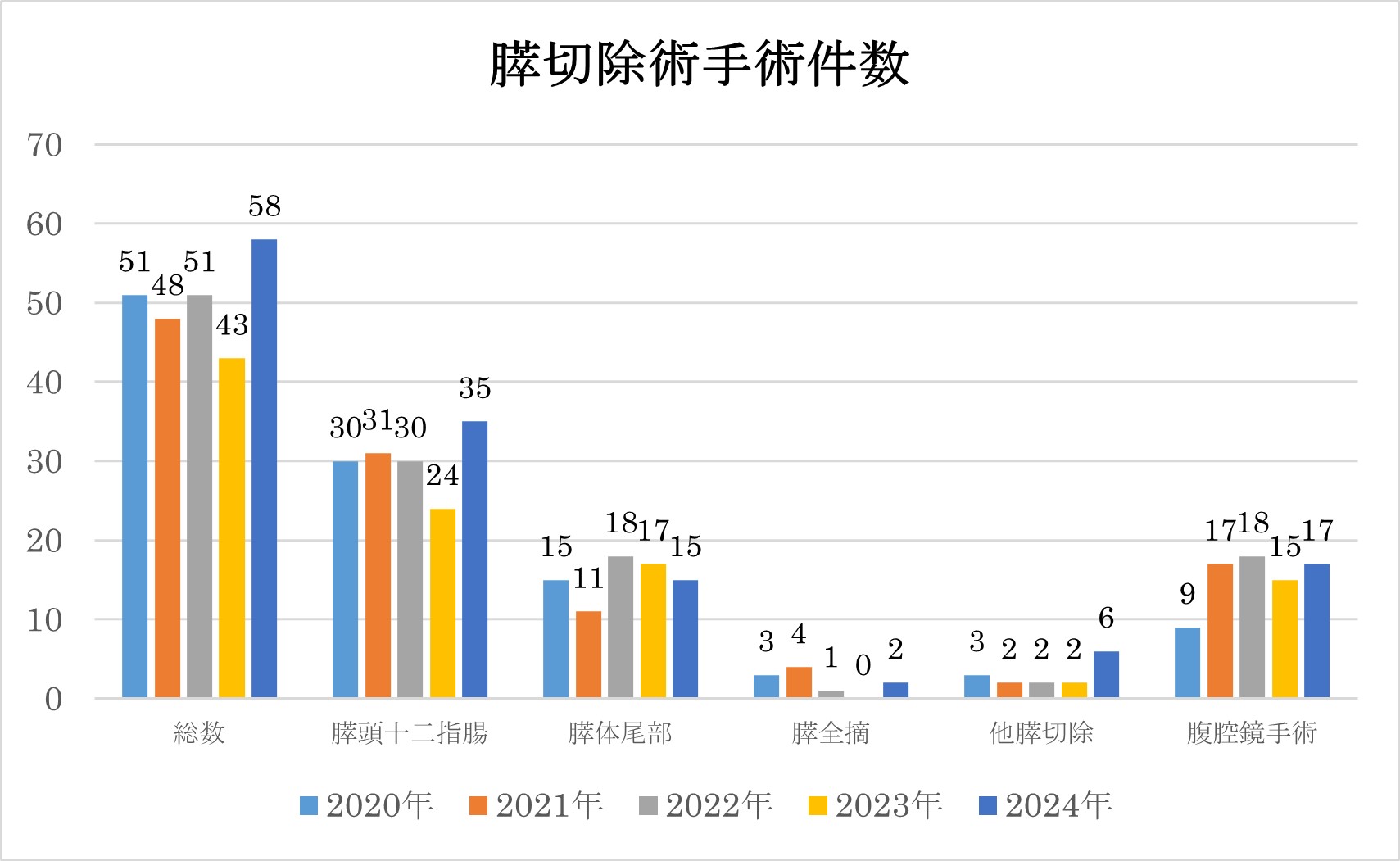
以下に、肝切除、膵切除術の症例の内訳を以下に示します。
診療科別統計
主な疾患・治療法
食道について
食道癌について
Ⅰ)食道癌の特徴
日本人の食道癌による死亡数は男性では第6位、女性では第13位とそれほど多くありません。しかし、もともと頻度の少ない病気(生涯罹患リスクは52人に1人。胃癌は9人に1人)ということを考慮すれば、悪性度の高い癌と言えます。
食道癌の発生に関してはこれまでに非常に多くの研究がなされていますが、はっきりした原因は解明されていません。現時点では、 遺伝的因子も重要ですが、環境因子、特に飲酒と喫煙が食道癌の危険因子とされています。
食道癌の早期のものは無症状で、多くは健診などで発見されます。進行した癌では食事のつまり感や、飲み込みにくいといった症状が出現します。さらに進行すると、胸痛、食欲不振、体重減少なども生じます。頚部のリンパ節腫脹や咳、嗄声(声がかれること)を契機として見つかることもあります。これは「反回神経」と呼ばれる発声を司る神経が、その周囲のリンパ節転移の影響で麻痺することによります。
Ⅱ)食道癌の進行度、病期(ステージ)
癌が見つかったら、どれだけ進行しているのか検査ではっきりさせることが必要になります。進行度によって治療方法が変わってくるからです。
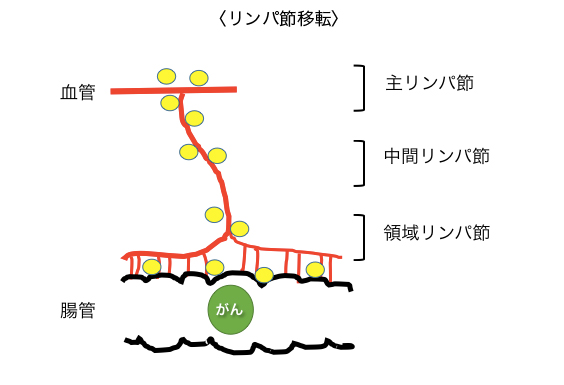
食道癌は食道の粘膜から発生し、はじめは粘膜内にとどまっていますが、進行するに伴って次第に粘膜下層、筋層、外膜へと達します(a. 壁深達度)。また、進行する過程で一部の癌細胞は血管やリンパ管に入り込んで、リンパ節に飛んだり(b. リンパ節転移)、肝臓や肺などの離れた臓器に飛んだりします(c. 血行性転移)。
a.壁深達度
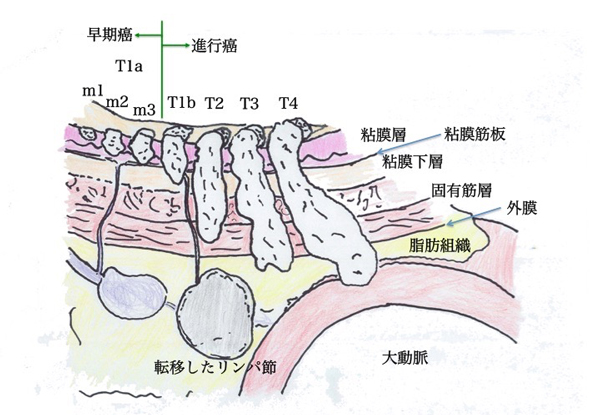
b.リンパ節転移
c.血行性転移
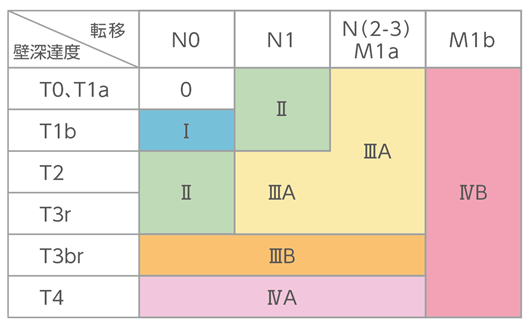
これら3つの要素から、食道癌の進行度を判定します(Stage 0〜IVb)。
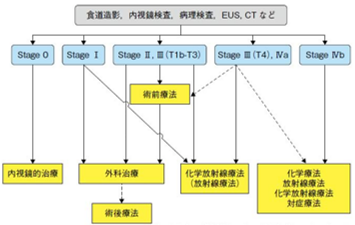
Ⅲ)食道癌の治療について
食道癌は非常に予後の悪い病気で、治療しなければ、進行して、出血、閉塞を来たし、最終的には全身病となって生命を脅かす病気です。
治療法は、進行度や全身状態などから総合的に判断していく必要があります。日本食道学会から「食道癌診断・治療ガイドライン」が発表されており、基本的にはこれに沿って治療方針を決定していますが、それには専門的知識と経験、判断力が必要です。当院では食道癌で受診された患者さん全員について、消化器内科、消化器外科、放射線治療科、腫瘍内科の食道癌診療に関わる全科の専門医師が揃って行う「食道疾患合同カンファレンス」で治療方針を検討しています。進行度0期の食道癌は内視鏡治療での治癒が見込めます。進行度Ⅰ〜Ⅲ度の食道癌の治療は原則手術です。手術治療と同様に化学放射線療法の治療効果も高く、将来的には手術よりも主流になることが期待されています。しかし、現状では手術に較べると治療成績かかなり劣り、遺残・再発時の手術 (救済手術salvage surgeryといいます)は身体への負担が非常に大きくなるため、進行度と体力が許せば、なるべく手術治療を行なうのが基本的な方針です。
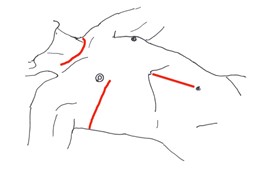
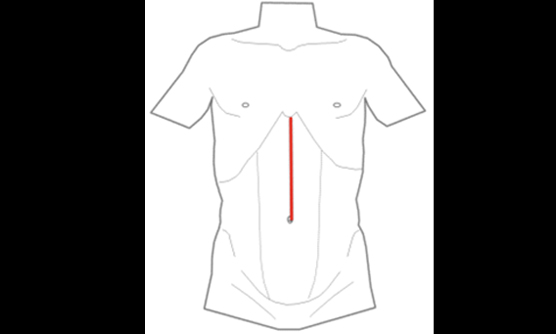
食道癌の手術
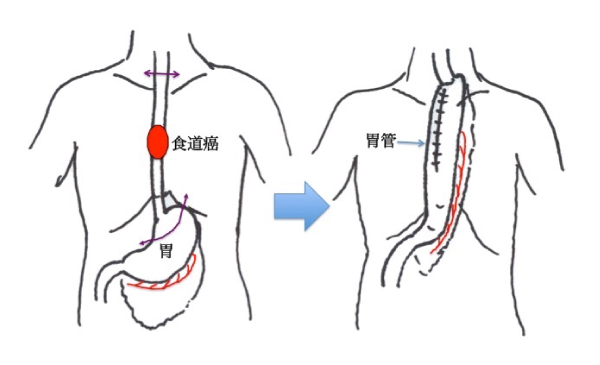
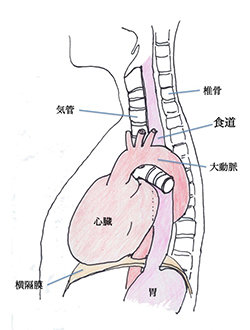
食道をとったあとの食べ物の通り道は、残った胃を細長く管状にのばして(これを胃管といいます)持ち上げ、頚部の食道とつなぎます。したがって開胸だけでなく、お腹もあけて(開腹といいます)、頚部も少しあけて手術をすることになります。
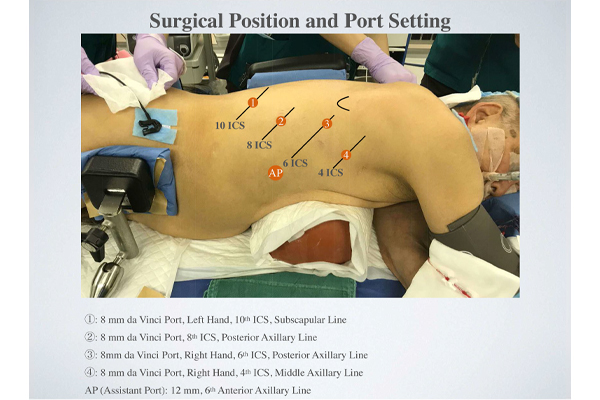
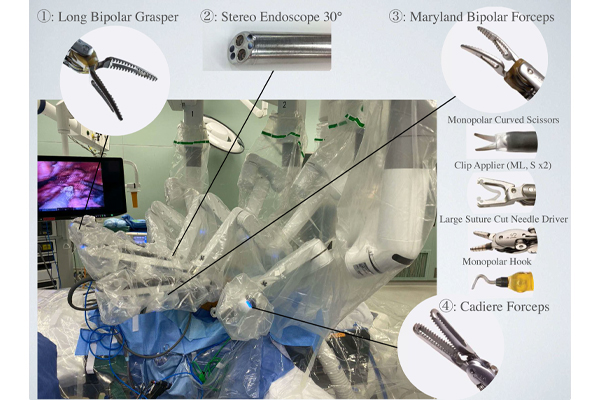
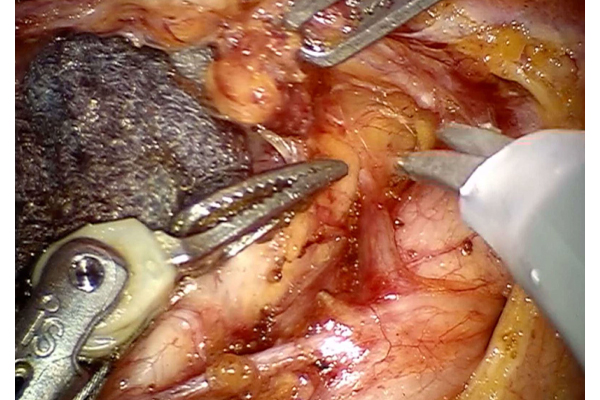
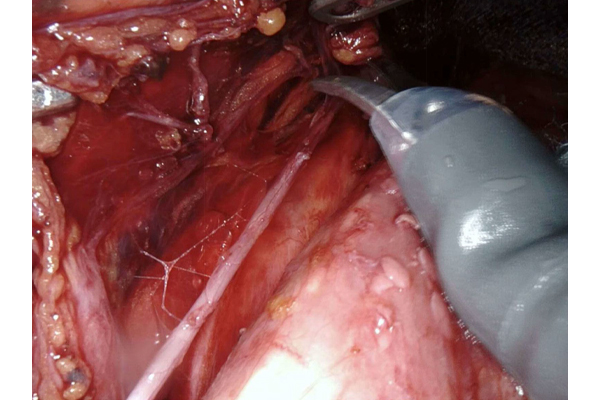
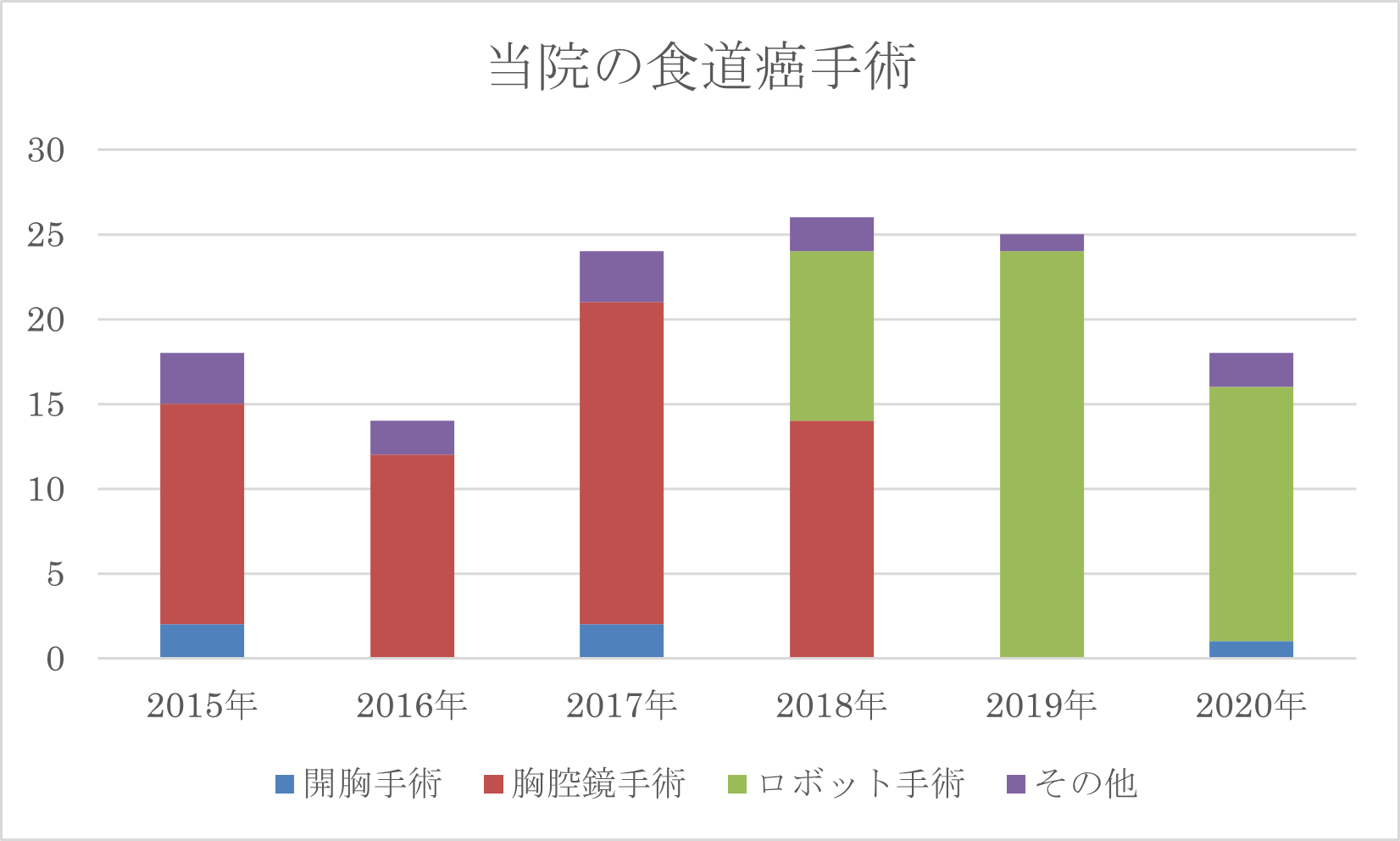
8〜10時間程かかるたいへん大きな手術です。当院では、胸腔鏡下手術を1998年から導入しており、200例以上の経験を蓄積してきました。創が小さい、肺に与える影響が少ないなど、開胸手術よりも身体への負担が少ないのはもちろんですが、狭い胸腔内で高精度カメラでの拡大視効果により、より精度の高い(その結果治る可能性が高くなる)手術が可能と考えています。2018年からはロボット支援下手術を導入して、より精細で合併症の危険が少ない手術を行なうことが可能になっています。また開胸や胸腔操作なしで、頸部と腹部の傷から食道を切除する術式(縦隔鏡下食道手術)も、より身体に負担の少ない手術として適応症例(低肺機能、高齢の方など)には行なっています。
術式によって多少異なりますが、術後1週間ぐらいで飲水、経口摂取を開始します。順調なら術後2〜3週間で退院できます。
手術の合併症
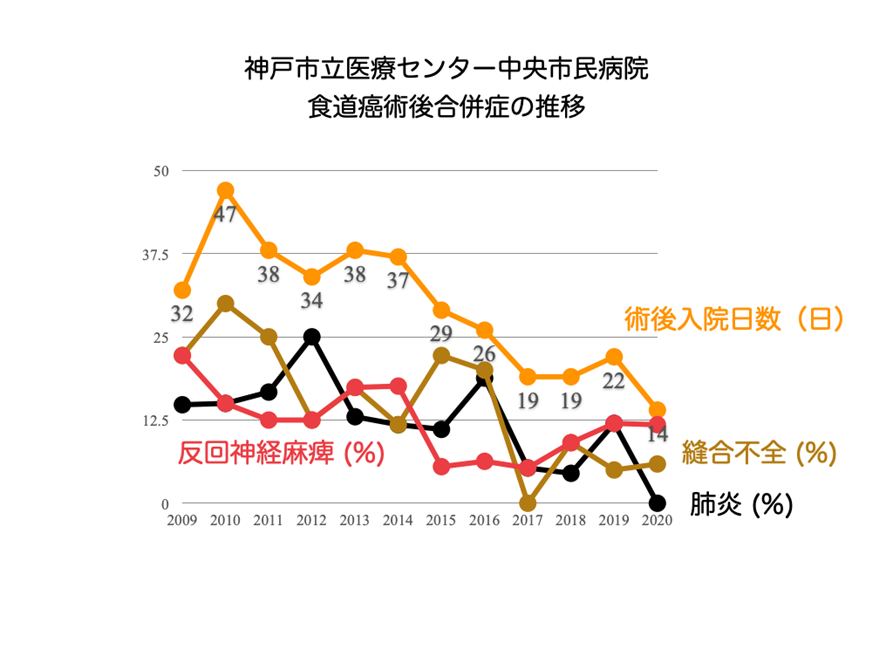
食道の手術は大手術と言われており、手術中や手術後に様々な問題(合併症と呼びます)が起こる危険性は、他の手術に比べて大きいと言わざるを得ません。医療技術や知識・経験の積み重ねにより、食道の手術によって患者さんが死亡することは以前に比べて非常に少なくなってきました。2011年の全国登録では、合併症率は41.9%、術後死亡率は3.4%でした(National Clinical Database; NCDより)。これは欧米の手術治療成績よりは、かなり良いデータですが、それでも危険性は他の手術に比べて非常に高いといわれています[1]。食道癌術後の3大合併症は、肺炎、反回神経麻痺、縫合不全です。
1)呼吸器合併症(肺炎、15%; NCD)
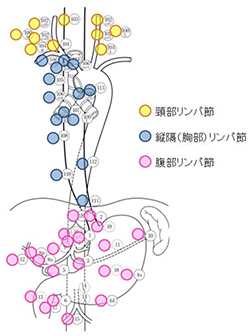
縦隔内の気管周辺のリンパ節には食道癌の転移が起こりやすいため、その場所のお掃除(リンパ節郭清と言います)が必要です。そのため術後に充分大きな呼吸をしたり、咳をして痰を出したりすることが困難になります。また、嚥下運動も障害されやすいことから、誤嚥(上手く呑み込むことが困難になり、気道に飲食物が流れ込むこと)を起こしやすくなります。その結果、肺炎(10%)や無気肺などの呼吸器合併症を起こすことがあります。短期であれば、気管支ファイバーで吸痰することなどで対応できますが、気道、呼吸管理(喀痰吸引や人工呼吸など)が長期化する場合、気管切開を置いて長期的に治療していく必要があります。胸腔鏡下手術の導入以後、減少しましたが、依然として生命に関わる合併症です。
2)反回神経麻痺(約20%; NCD)
声帯を動かす神経は、胸腔内の大血管(右-鎖骨下動脈、左-大動脈弓)を反回して、気管の脇を通って声帯に入ります。この反回神経周囲のリンパ節は食道癌のリンパ節転移が最も多い場所で、郭清する必要があります。そのため、比較的高率に麻痺症状が出現します。軽ければ、嗄声(させい)と言って、声がかすれるだけですが、呼吸がしにくくなったり誤嚥の原因になったりすることがあります。大抵は6ヶ月以内に神経の働きが戻って改善しますが、機能が回復しなければ、声帯の手術をすることもあります。
3)縫合不全(13.3%; NCD)
胃を頚部まで吊り上げて吻合、再建しますので、先端付近は血流不良となりやすいため、繋ぎ目がしっかりとくっつかなければ、唾液や胃液が漏れる状態になります。これを縫合不全といいます。漏れが軽度ならば、創処置だけで治癒していきます。長期間の絶食が必要になることがあります。胃管の広い範囲が血流障害に陥ると、胃管壊死(2-3%)と言って胃管が腐ってしまうことがあり、緊急手術が必要になります。縦隔炎を来すと生命の危険があります。
この他にも、乳び胸、術中・術後出血、創感染、敗血症、深部静脈血栓症などの合併症のリスクがあります。
当院では、手術を安心して受けていただくために、合併症の予防対策に特に力を入れており、全国的に見ても良好な治療成績を達成しています[2,3]。その結果、術後に退院するまでに要する日数が短縮しています。
周術期管理
せっかく頑張って手術を受けても、合併症を乗り越えられなくては「癌を治す」という目標が達成できません。外科医が中心となる手術、術後管理が大切なのは勿論ですが、術前の口腔ケア(歯科医)や呼吸リハビリ(理学療法士)、術後早期からの集中治療(麻酔科)、呼吸・嚥下リハビリ(理学療法士)、服薬指導(薬剤師)、栄養指導(栄養士)など、多職種の連携によるチーム医療が必要であり、病院全体の機能が問われる病気と言えます。
外来通院について
術後しばらくは体調をみるため、その後は癌の再発や転移を早期発見するために外来通院して頂きます。
「5年生存率」という言葉がよく使われるように、癌が治っていると判断できるまで長期的に検査を受ける必要があります。3〜6ヶ月に一度、採血やCT検査を中心に、リンパ節転移や血行性転移による再発のチェックを行ないます。再発しても手術や放射線治療で治すことができる可能性があるからです。 また、食道癌には「咽頭・喉頭領域の重複癌」が多い特徴があり、これを早期発見するために最低でも1年に1回は上部消化管内視鏡検査を受けていただいています。
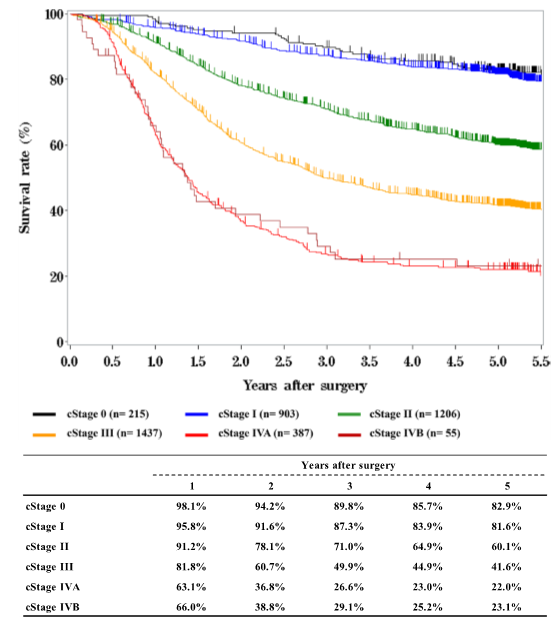
手術の成績
日本食道学会の「全国食道がん登録調査報告」では、手術で切除できた場合の5年生存率は55.6%になりました。治療成績は良くなってきていますが、それでも消化器系悪性腫瘍のなかで、特に予後不良の病気であることは間違いなく、治療に難渋することもあります。
参考文献:
- Takeuchi H, Miyata H, Ozawa S, Udagawa H, Osugi H, Matsubara H, Konno H, Seto Y, Kitagawa Y. Comparison of Short-Term Outcomes Between Open and Minimally Invasive Esophagectomy for Esophageal Cancer Using a Nationwide Database in Japan. Ann Surg Oncol 2017;24:1821-7
- Kobayashi H, Kondo M, Mizumoto M, Hashida H, Kaihara S, Hosotani R. Technique and surgical outcomes of mesenterization and intra-operative neural monitoring to reduce recurrent laryngeal nerve paralysis after thoracoscopic esophagectomy: A cohort study. Int J Surg 2018;56:301-6.
- Kobayashi H, Kondo M, Kita R, Hashida H, Shiokawa K, Iwaki K, Kambe H, Mizuno R, Kawarabayashi T, Sumi T, Kaihara S, Hosotani R. Cause of recurrent laryngeal nerve paralysis following esophageal cancer surgery and preventive surgical technique along the left recurrent laryngeal nerve. Mini-invasive Surg 2020;30.
- Tachimori Y, Ozawa S, Numasaki H, Ishihara R, Matsubara H, Muro K, Oyama T, Toh Y, Udagawa H, Uno T, Registration Committee for Esophageal Cancer of the Japan Esophageal S. Comprehensive registry of esophageal cancer in Japan, 2012. Esophagus 2019;16:221-45.
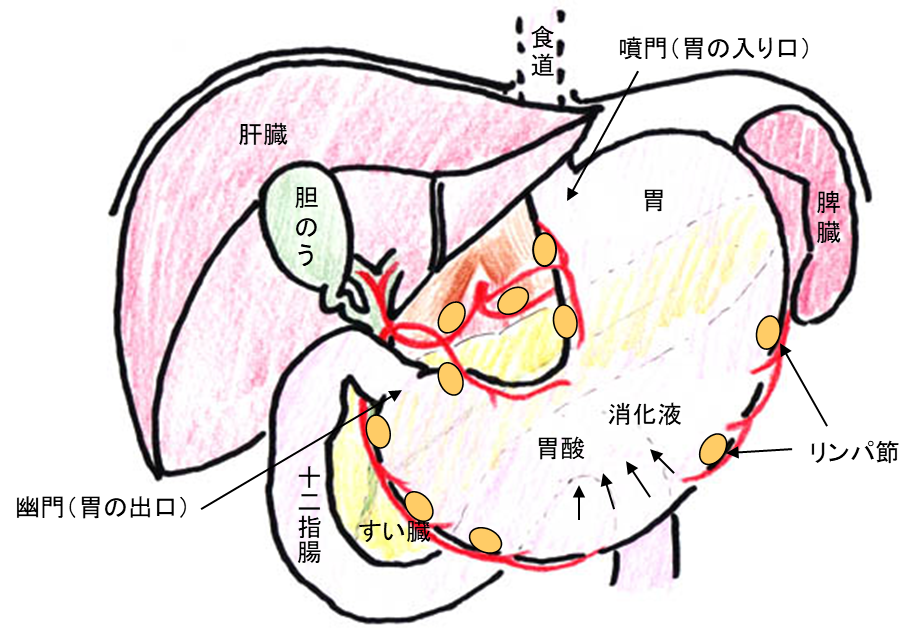
胃の形とはたらき
胃は、食べ物を消化吸収する臓器のひとつですが、袋状になっており、食道(喉から胃までの筒状の臓器)と十二指腸(膵臓や肝臓からの消化液がまじわる臓器)との間にあります。食道との境目となる胃の入り口部分は噴門(ふんもん)とよばれ、十二指腸へとつながっていく胃の出口部分は幽門(ゆうもん)とよばれています。
主な役割は、食事をいったん蓄えておき、粥状になるまで小さくこなして、幽門より少しずつ十二指腸(小腸)へ送りだすことです。胃を手術すると、これらの機能が低下したりなくなったりします。それを補うためには食事療法が必要となります。(後述)
胃の腫瘍(しゅよう)について
胃がん
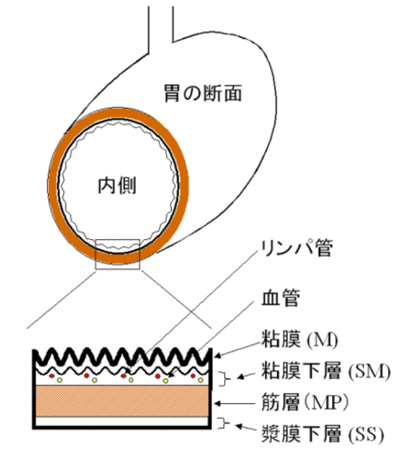
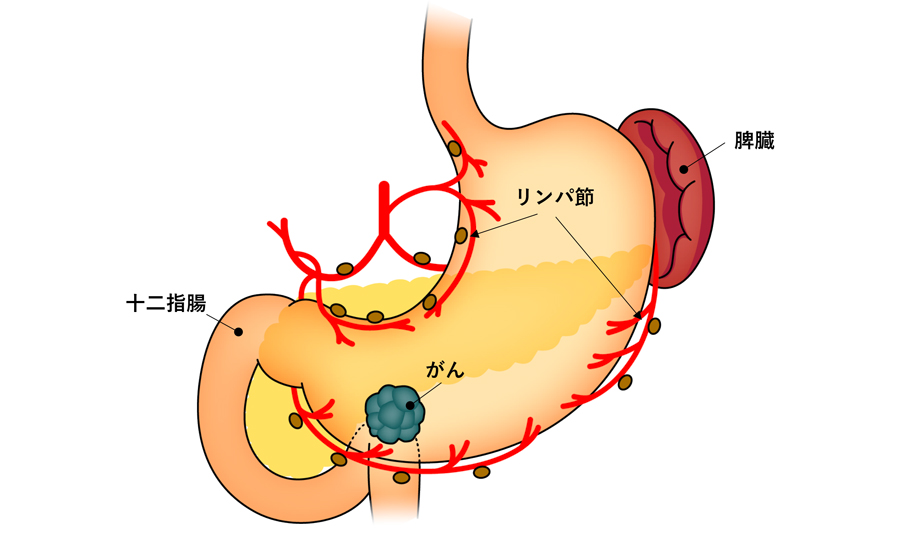
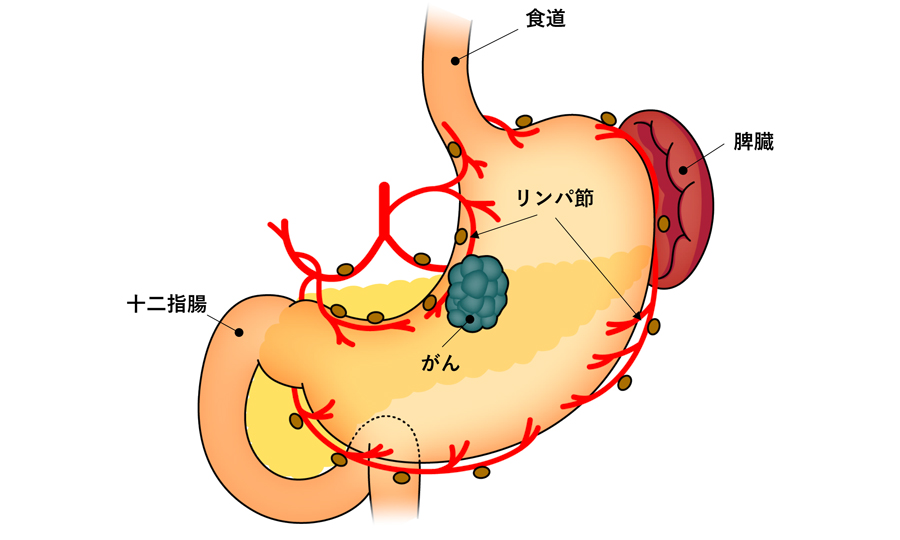
Ⅰ)胃がんの成り立ちと進み方
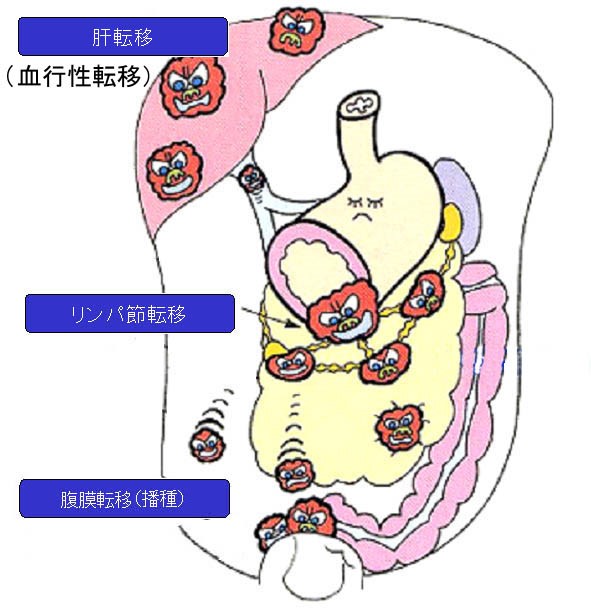
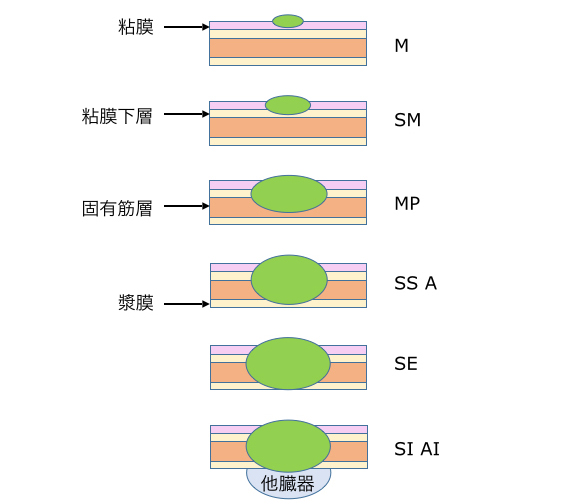
胃にできる腫瘍のうち最も頻度が高く有名なものが胃がんになります。胃がんは胃の粘膜から発生し、次第に粘膜下層、筋層、漿膜下層へと深く達していきます(壁深達度)。その途中で、一部のがん細胞は胃の壁にあるリンパ管や血管に入り込んで、リンパ流にそってリンパ節に飛んだり、血流にそって肝臓や肺など離れた臓器に飛んだりします。これを転移といい、胃がんが「悪性」腫瘍といわれる所以です。
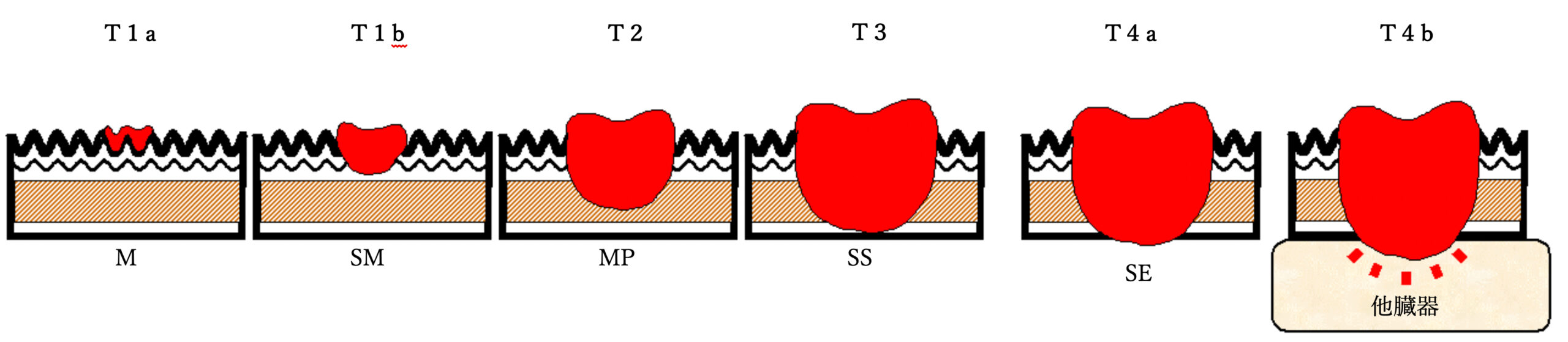
a.壁深達度
胃がんがどの深さまで達しているかは、下図のようにT1からT4までに分類することになっています。胃がんが深くなると、転移を起こしやすくなるので、一般に粘膜下層までの浅い胃がん(T1)を転移の可能性の低い早期胃がんとし、筋層あるいはそれ以上に深く、転移の可能性が充分考えられる胃がんを進行胃がんとして取り扱います。胃がんが漿膜をやぶって胃の外側に出てくると(T3)、がん細胞がおなかの中にこぼれて、腹膜に転移することがあります(腹膜転移や播種といわれる)。また、周囲の内臓にくいこんで一体となることを浸潤といい(T4)、胃がんの切除の時に他の臓器も一緒に切除しなければならなくなることがあります。これらは実際におなかの中を覗いてみないとわかりませんが、胃カメラやCT検査などである程度予想して治療方針を立てていきます。
T1
粘膜~粘膜下層にとどまっているがん(早期胃がん)
T2
筋層まで進んでいるがん
T3
胃の外側近くまで出てきているがん
T4
胃の外側に出たり更に他の内臓や組織に食い込んでいるがん
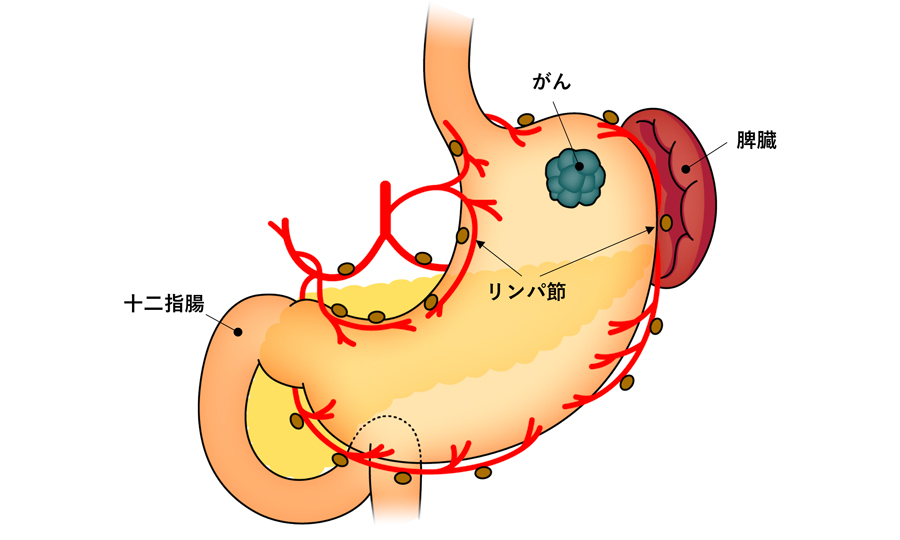
b.移転
がんの転移には大きく分けて、①リンパ節転移、②血行性転移(肝臓や肺など)、③腹膜転移(播種)の3種類があります。胃がんでは、このなかでも比較的初期からリンパ節転移を起こすことが多いことが知られています。また、しばらくの間は胃の近くのリンパ節の転移にとどまっていることが多いことがわかっています。このため、胃がんに対する治療は、転移している可能性のある胃の周りのリンパ節を胃の病巣と一緒に切除する方法が定型手術として定着しています。
また、リンパ節転移は胃がんの進み具合を決める上でも重要です。すなわち、胃がんの進み具合は、胃がんの深さとリンパ節転移の程度で決めることになっています(進行度、ステージ)。
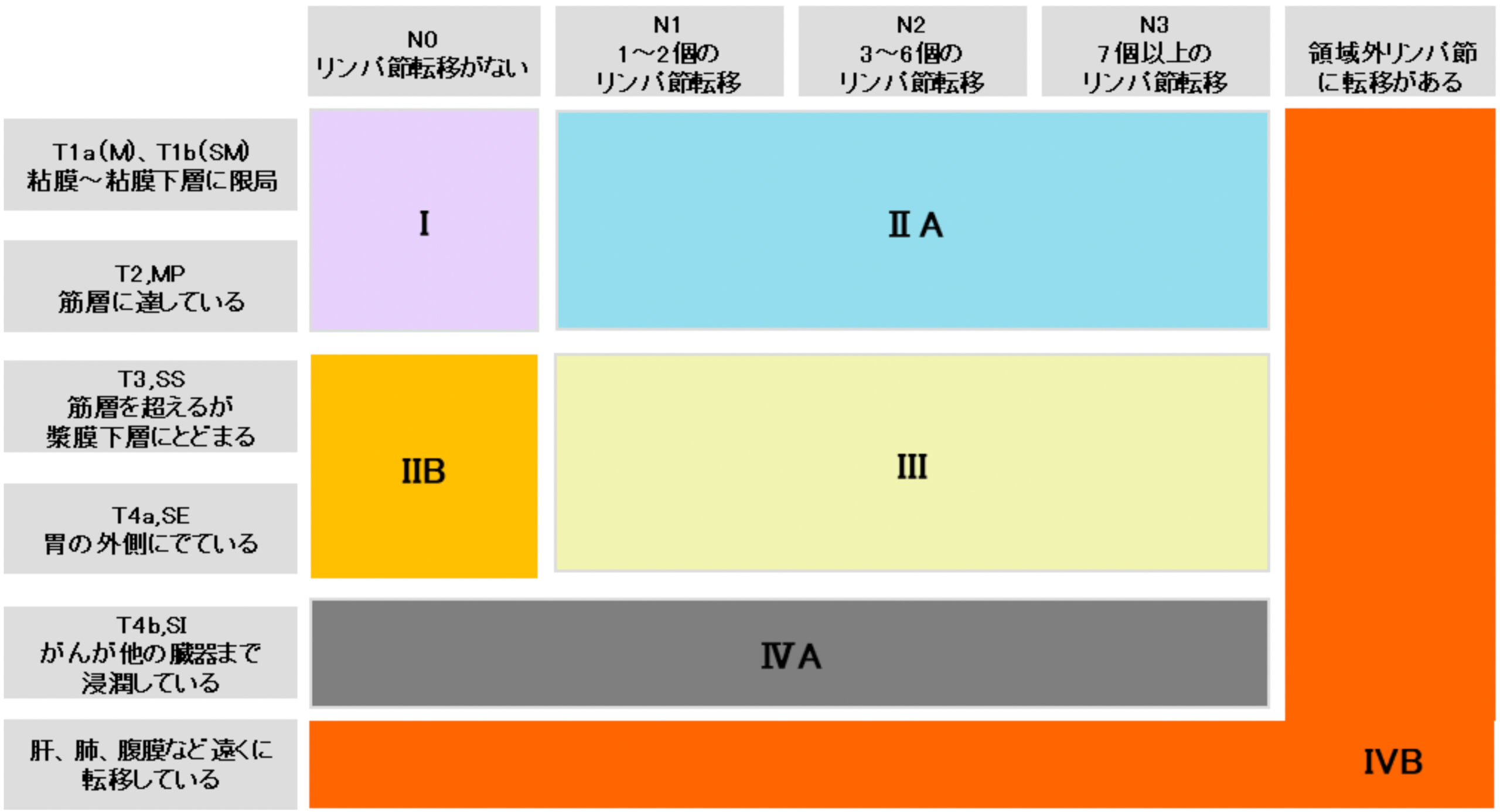
Ⅱ)胃がんの進み具合(進行度、ステージ)
胃がんの進み具合(進行度、またはステージと呼んでいます)は、現在 日本胃癌学会の胃癌取り扱い規約という取り決めにしたがって、治療前は I、ⅡA、ⅡB、Ⅲ、ⅣA、ⅣBの6段階に分類されます。胃カメラやCT検査などの結果、予想されるあなたの胃がんの進み具合を考慮し、治療方法を選択することになります。また、治療をした場合の胃がんの治りやすさも進み具合によって違ってきます。
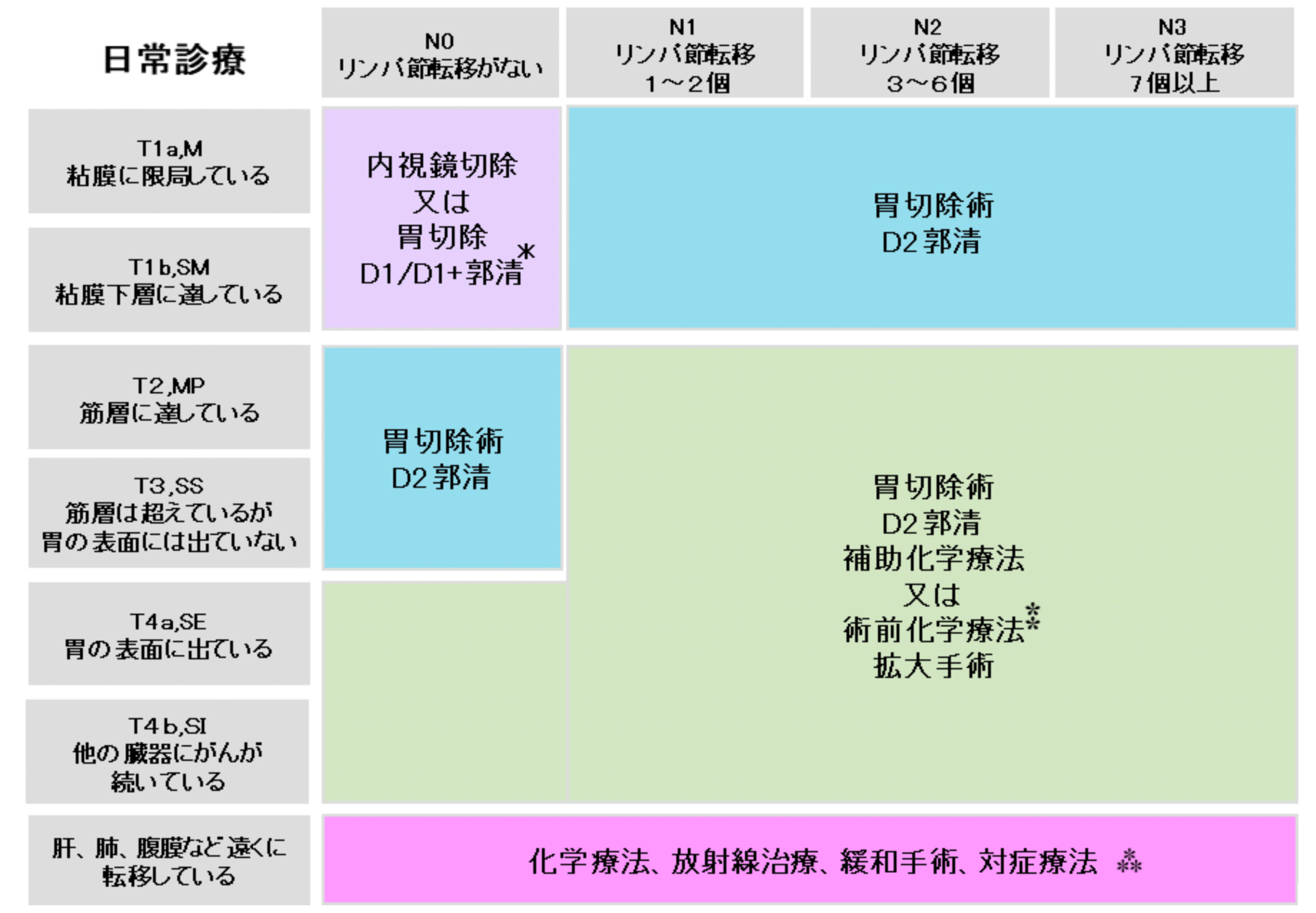
Ⅲ)胃がんの治療について
以下にあげた表は、日本胃癌学会による胃癌治療ガイドライン(2018年1月改訂)に準拠したものです。現在広く一般に行われており妥当と考えられる治療方法が胃がんの進み具合に応じて、日常診療としてあげられています。
胃がんの治療方法には、①内視鏡治療(胃カメラでの粘膜切除)、②手術、③化学療法(抗がん剤)、④放射線療法があります。粘膜にとどまるような早期がんは内視鏡治療の対象となることが多いですが、たとえ早期がんであってもリンパ節に転移している可能性があるものや、それ以外の進行がんに関しては手術が最も有効な治療法とされています。手術は胃の切除と胃の周りのリンパ節を一緒に切除する方法になりますが、後の項目で説明するように、胃を部分的に残せる場合(幽門側胃切除や噴門側胃切除)と、胃を全部とる場合(胃全摘)とがあります。また、がんが大きくなって他の臓器につながっている場合には、その臓器も一緒に取る(合併切除)必要が出てくる場合もあります。
ただ、さらに遠くの臓器やリンパ節に転移がある場合(ステージIVB)は手術で取りきることはできないため、化学療法が治療法の中心となります。この場合でも、腫瘍で胃が詰まったり腫瘍からの出血が続く場合など、症状改善目的のための姑息手術(こそくしゅじゅつ)を行うこともあります。
- *がんの進行度によって切除するリンパ節の範囲が異なり、D1、D1+、D2と数字が大きくなるに従い範囲が大きくなります
- ⁑手術と補助化学療法を行っても再発率が高いような進行がんに対しては術前化学療法と手術を組み合わせるような集学的治療も行っています
- ⁂ステージⅣであっても化学療法後に緩和手術ではない通常の胃切除を行う場合もあります
また、病理検査といって、切除した胃がんを顕微鏡で詳しく調べて正確なステージを確認します。この場合は手術前のステージ分類と異なり、ⅠA、ⅠB、ⅡA、ⅡB、ⅢA、ⅢB、ⅢC、Ⅳといった更に細かく8段階に分類されます。通常は手術後2-3週間で結果がでますので、退院後最初に来ていただく外来で説明させていただきます。その病理検査結果のステージに応じて、手術後に補助化学療法(再発予防目的に期間限定で行う抗がん剤治療のこと)をお勧めする場合があります。
これ以外にも、がんが胃の外側に出ていないかどうか、腹膜播種がないかどうかなどを調べるために腹腔鏡でおなかの中をのぞくような検査(審査腹腔鏡)や、手術前に抗がん剤を用いる(術前化学療法)ことで、根治性(完全にがんを治す事)を出来るだけ高めることを目指す集学的治療なども積極的に行っています。
胃癌治療ガイドラインで推奨されている治療法以外にも、胃がんの治療法は多岐にわたっています。手術を行う場合でもロボット支援手術、腹腔鏡手術、開腹手術と異なったアプローチ法があります。患者様個々人のお体の状態、がんの進行状況などを踏まえた上で、ガイドラインに記載されていないような臨床試験なども含め、御本人に最良と思われる治療の選択枝を提案させていただくよう努めています。当院では、消化器疾患について定期的に消化器内科、腫瘍内科、放射線画像診断科、病理診断科、外科と合同のカンファレンス(会議)を行っており、診断から治療まで様々な科の協力のもとに日常診療を行っておりますので、診断や手術以外の治療法に関しても遠慮なくご相談ください。
胃がんの手術について
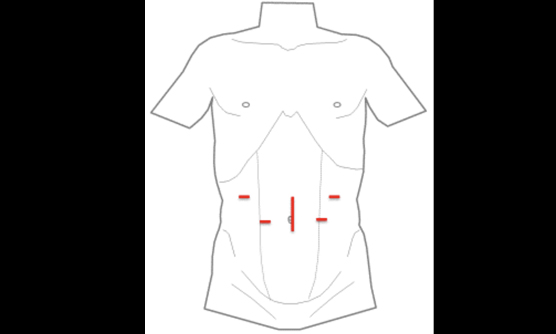
Ⅰ)患者様にやさしい低侵襲手術 腹腔鏡手術、ロボット支援手術
腹腔鏡下手術とは、おなか(腹腔内)を炭酸ガスでふくらませて、おへそからカメラ(腹腔鏡)を挿入した状態で、おなかの4-5カ所に直径1㎝程度の筒を入れて、そこから手術用の器具を出し入れして行う手術のことです。ロボット支援手術はこれを発展させたものになります。
最近ではほとんどの胃がん手術は腹腔鏡やロボットでの手術になっています。患者様の病状によっては通常の開腹手術を行う場合もございますので、お気軽に医師までお問合せ下さい。
腹腔鏡手術は、傷が小さくて患者様への負担が少ないだけでなく、拡大視効果により繊細で出血の少ない手術が可能となります。
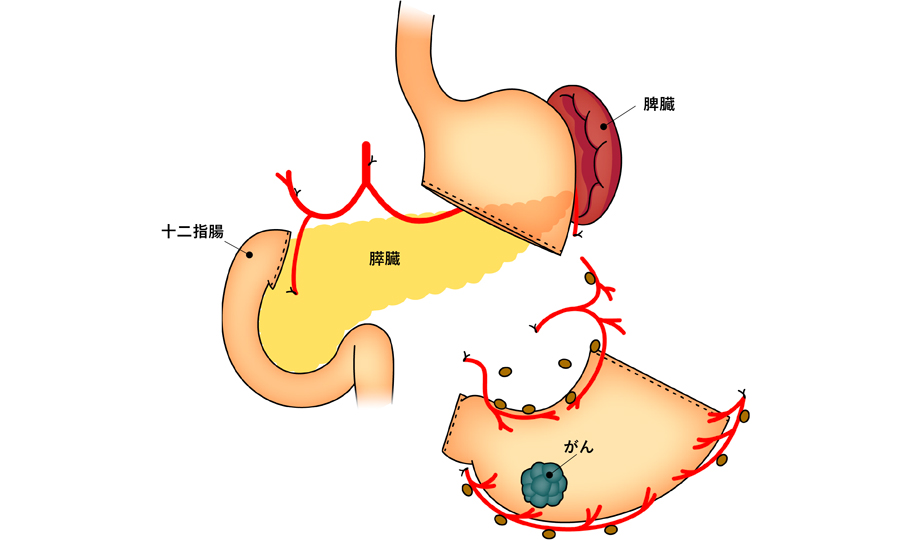
Ⅱ)胃切除の範囲 幽門側胃切除術、胃全摘術、噴門側胃切除術
胃がんに対する手術は、胃の切除と周辺リンパ節の切除とからなります。癌の場所や進行度によって切除する範囲はかわります。術後患者様のQOL(生活の質)を重視するために出来るだけ胃全摘術を避けるなど、さまざまな工夫を行っています。
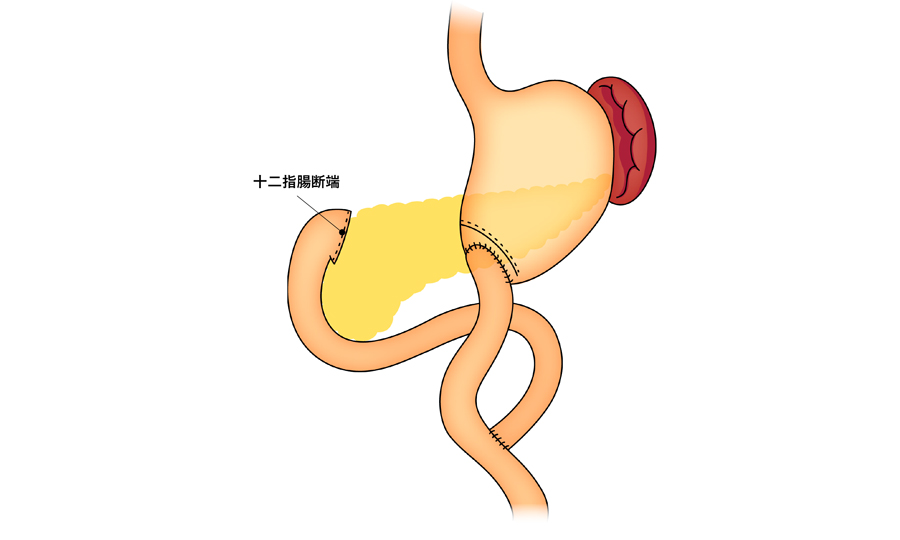
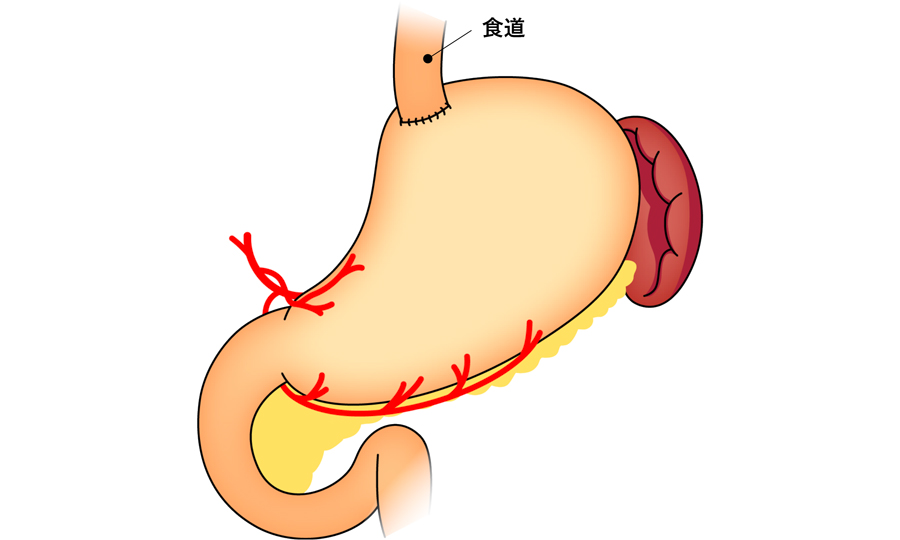
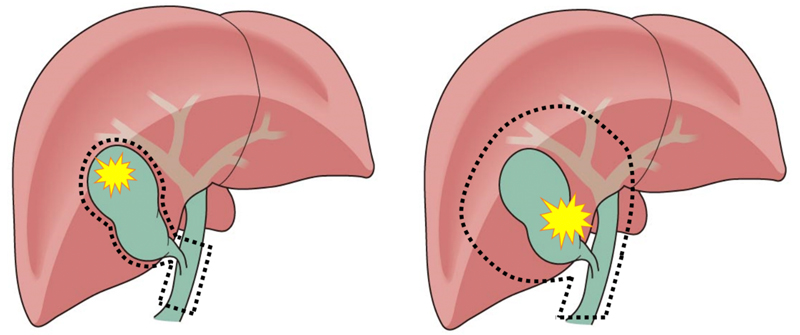
a.幽門側胃切除術
がんが胃の中央部から出口(幽門)側に存在しているときには幽門を含めた出口側の胃約3分の2~4分の3程度を切除し、入口(噴門)側の胃を残すことができます。これを幽門側胃切除とよんでいます。残った胃と十二指腸を直接つないだり、小腸を持ちあげて胃とつないだりすることで、食べ物や消化液が通るようにします。
b.胃全摘術
がんが噴門近くまで広がっている場合は、胃を全部切除する手術が必要となります。胃袋が完全になくなりますので、食道と持ち上げた小腸をつなぐことで通り道を作ります。
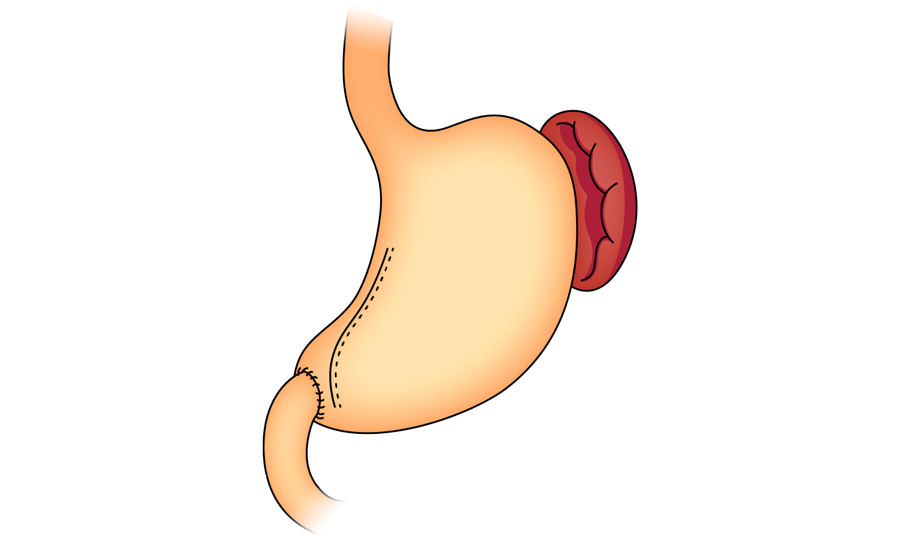
c.噴門側胃切除術
胃の噴門近くにある早期がんの場合は、胃全摘を避けるために噴門側胃切除という術式を行っています。胃が半分以上残るため、胃全摘の術後に比べて術後の体重減少や栄養状態の低下が少ないといわれています。
胃切除の範囲は、がんの場所や広がりだけでなくがんの進行度や患者様の年齢、体力などを総合的に判断して決めています。これ以外の術式を提案させていただくことや、手術中の状況に応じて切除範囲や術式を変更することもありえます。
手術に関連した取り組み
胃がんと告知を受けたり、手術が必要と説明されたりすると、様々な不安や疑問点が生じると思います。実際に手術を受けていただく患者さんのために、われわれが行っている取り組みをご紹介します。
Ⅰ)口腔ケア
手術を受けていただくことが決定した場合、患者様皆様に紹介状を手渡して歯科医受診をしていただいています。口腔内を清潔に保つことは術後肺炎という合併症を予防する観点からとても重要視されています。それだけでなく、胃切除をした後は咀嚼(かむこと)も大切ですので、術前より齲歯(虫歯)の治療や抜歯、義歯(入れ歯)作成などを含めてたくさんの開業医の方々と連携して行っています。
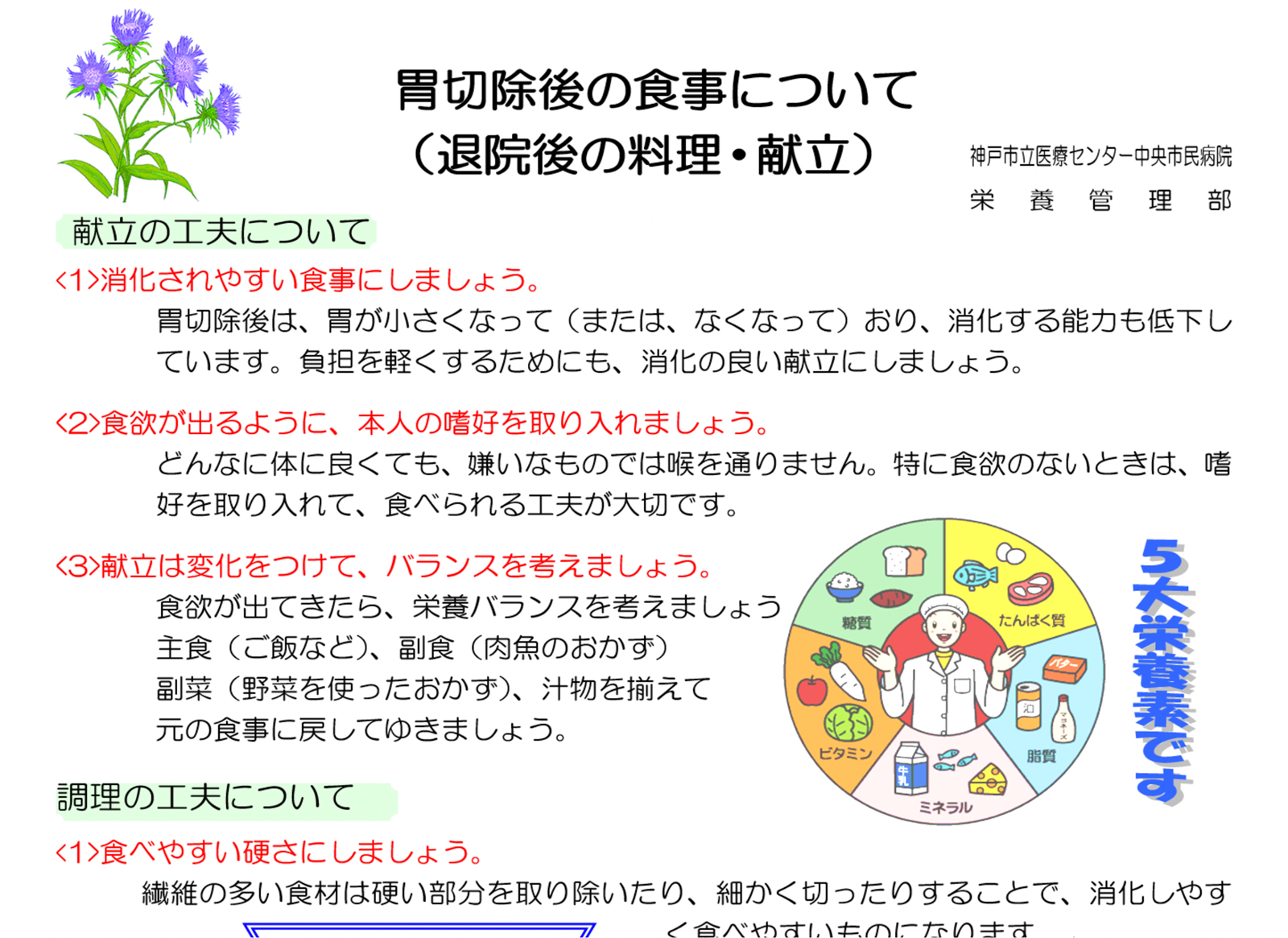
Ⅱ)栄養指導、ONS
胃を切除することで、様々な胃切除後障害が生じてしまう可能性があります。胃の働きは、食べた食事をためておき、それを蠕動により細かくしてさらに胃酸により消毒、消化して腸管に送り込むという作用があります。胃が小さくなるあるいはなくなることによりこれらの機能が失われた症状が現れます。具体的には、まず、1回で食べられる食事の量が減少します。それから、消化吸収能力が低下するために下痢をしやすくなります。また、食事が直接小腸に入るために、ダンピング症候群といって、食後早期におなかが張って痛いとか、食後2時間くらいで低血糖により冷や汗がでたり、目の前が真っ暗になったりする症状などがあります。これらの症状は月の単位で徐々に改善してくることが多いですが、完全にはとれません。体重は術後一時的に数%から10%以上も減少することがあります。徐々に再び増加しますが、胃がんが治ったとしても元通りの体重には戻りません。これらの症状を少しでも改善したり、体重減少を出来るだけ少なくしたり、体力保持のために大切となるのが食事療法です。
当院では管理栄養士による食事療法の栄養指導を入院中は2回(入院時と退院前)、そして退院後も外来にて行っています。具体的には分割食といって1回の食事量を減らして回数を増やす方法をベースに、効率よい食事の仕方や注意点などを事細かに説明しています。外来では、自宅での食事療法がスムーズに行えているかどうか、必要な栄養素を摂取できているかどうかなども評価しています。外食やアルコール摂取等について質問される方もいらっしゃいます。また、ONS(Oral Nutrition Supplementation:経口的栄養補助)といって通常の食事に経腸栄養剤や濃厚流動食を飲んでいただくことで不足分の栄養を積極的に補うことも行うなど、患者様の栄養状態が少しでも良くなるように入院中から外来まで様々な取り組みをしています。
上記のような文書に従って説明いたします。
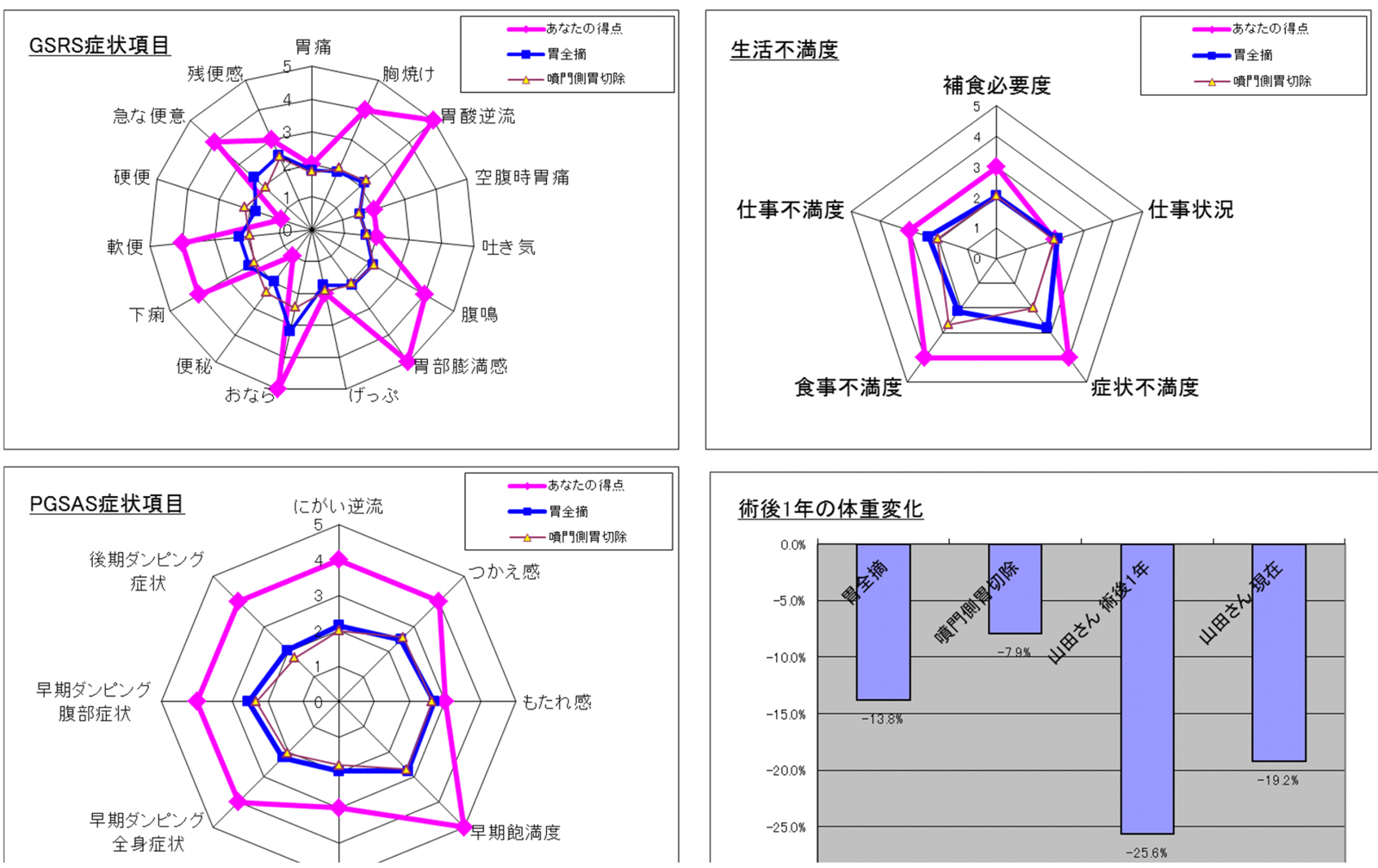
また、当院は「胃外科・術後障害研究会」の施設会員です。胃切除後も患者さんに快適な日常生活を送っていただくために研究会が作成した冊子やプリントを活用したり、研究会が提供しているPGSASアプリなどを用いたりして、ご自身の食生活の現状をより深くご理解いただけるよう努めています。
PGSASアプリによる胃がん術後評価表。患者さんが記入した質問票内容と術式などの情報を入力することで、その時点での胃切除後障害の実態を視覚的に理解することが可能となります。
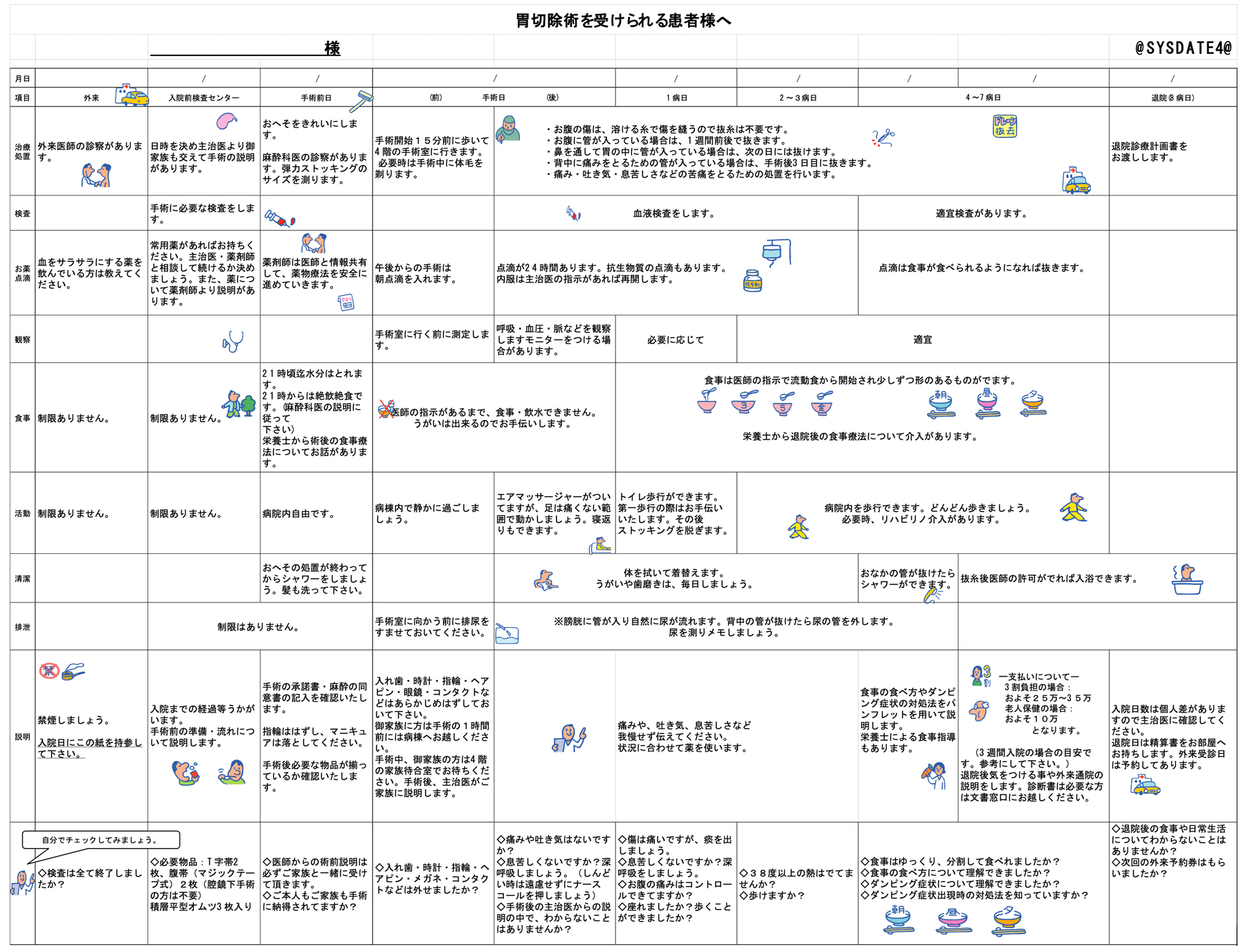
Ⅲ)クリニカルパス、胃癌地域連携パス
胃がん手術を受けられる際に、入院してから具体的にどのような経過をたどるのか、様々な疑問点があると思います。そういった医療行為がいつ行われるのかを、おおまかなスケジュール表にしてわかりやすくしたものの事をクリニカルパスといいます。当院では胃がん患者様に関してはほぼすべての術式に同一のクリニカルパスを用いています。
クリニカルパスを導入することによって、皆さまには入院後手術してからの検査や治療の流れがスケジュール表のようになっていて理解していただきやすいという利点があります。我々医療従事者にとっては、そのパス通りに経過しているかどうかを客観的に判断することで胃がん治療の標準化が可能となるだけでなく、担当している職種間(医師、看護師、薬剤師、管理栄養士等)での情報共有化を通じ、更なる医療の質の向上を目指すことができます。入院の手続きをして頂く際にお渡しし説明いたします。
手術前日の入院、術後約1週間での退院を目指します。
通常のクリニカルパスは入院から手術そして退院までの内容のみとなっています。当科では退院後の外来通院においても検査の予定や通院日程などスケジュール化したものを導入しており、「胃がん地域連携パス」と呼んでいます。主として早期胃がんの患者さんが対象となりますが、たくさんの開業医の方々と連携しており、退院してからも安心して通院していただけるように心がけています。
実際の胃がん手術を受けていただく際には説明文書に沿ってお話させて頂きます。手術という治療法を選択していただく理由、具体的な術式と、術後のリスク(合併症など)についてしっかりと理解していただき、納得してから同意を頂いています。
胃癌手術説明文書はこちら現在用いている術前説明文書になります。この文書に沿って説明いたします。
合併症について
手術後早期合併症としては、出血、縫合不全(胃と腸等をつないだところがうまくくっつかないこと)、膵液ろう、吻合部狭窄(つなぎ目が浮腫などで一時的に通りが悪くなること)などが起こってしまうことがあります。
また、胃の術後の後遺症としてダンピング症候群(胃の貯留能の低下、消失等が原因で起こる様々な症状)や逆流性食道炎、胃内容排出遅延、腸閉塞、胆石症等が起こってしまうことがあります。
外科的治療過程では、ほとんどの場合、クリニカルパスを用いて治療にあたります。
順調にいけば、おおよそ術後7〜10日程度で退院可能となります。その間に、管理栄養師と連携し2回程度入院中に栄養指導をし、胃が小さくなったり、なくなったりした場合の食事の仕方を指導します。
外来通院について
早期胃癌に関しては、再発の可能性が少ないため、外来通院は半年~1年に1回程度になります。胃がん地域連携パスに準じての外来通院です。
進行癌に関しては、術後補助療法をおすすめすることが多くなります。抗癌剤治療に関しては当院では腫瘍内科と連携して行っていますので、抗癌剤治療中は腫瘍内科にいったんバトンタッチしますが、抗癌剤加療が終了すれば、また、外科で3〜6か月毎に通院していただきます。
早期胃癌、進行胃癌ともに手術後5年間程度は外来通院して頂きますが、再発なく経過した場合、その後は、基本的には地域の先生に引き続きお願いすることが多いです。
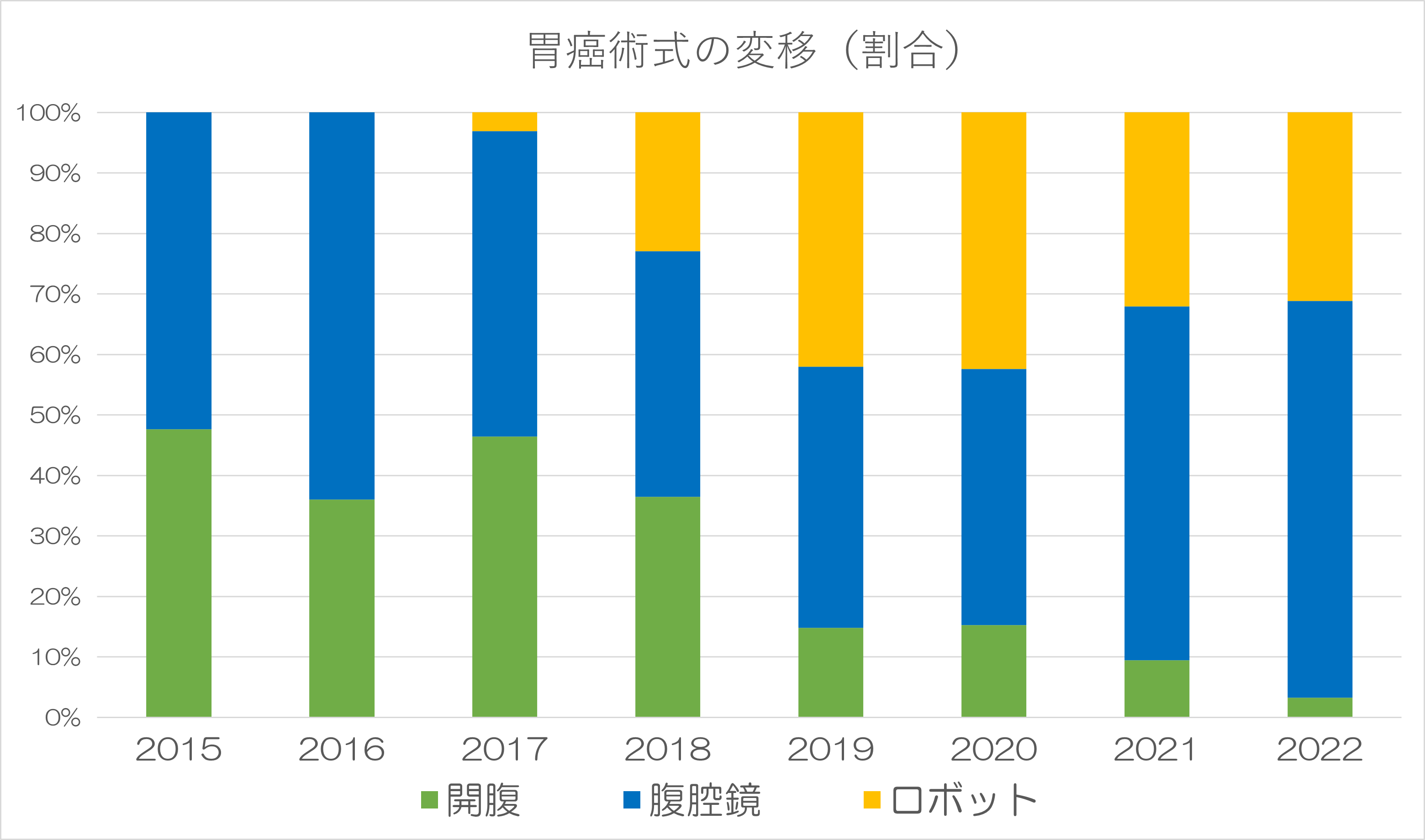
当科における手術数
当科における胃がん手術数は、年間80件から100件以上になります。そのうち低侵襲手術となる腹腔鏡手術やロボット手術の占める割合は年々増加しており、2022年では95%にまで達しています。より身体にやさしく、質の高い手術を提供できるように、複数の内視鏡外科技術認定医やロボット手術支援プロクターのスタッフが中心となり治療を行っております。
胃粘膜下腫瘍
ほとんどは消化管間葉系腫瘍(GIST:Gastrointestinal Stromal Tumorの略語)と呼ばれる腫瘍になります。胃がんとは異なり、胃の粘膜からではなく、胃の壁(筋肉)の部位から発生することが多いです。リンパ節転移はほとんどありませんが、大きくなると肝臓への転移や腹膜播種を生じる可能性が高くなります。
治療方法
胃がんと異なりリンパ節を切除する必要がないため術式はまったく違うものになります。大きさが小さいもの(5cm未満)に関しては腹腔鏡手術で行っています。なかでも胃の内側に発育しているものは、通常の腹腔鏡手術では腫瘍の位置がわからず、余分に正常な胃壁を切除してしまうことで胃の変形や狭窄(狭くなること)をきたすことがあります。そのような症例に関しては、内視鏡(胃カメラ)手術と腹腔鏡手術と合同で行うLECS手術(LECS:Laparoscopy & Endoscopy Cooperative Surgery)を行っています。消化器内科と外科とでのコラボレーション手術になります。
大腸がんについて
大腸がんは、大腸粘膜の細胞から発生し、腺腫という良性腫瘍の一部が悪性化して発生したものと正常粘膜から直接発生するものがあります。その進行はゆっくりですが、放置した場合、大きくなった癌が大腸の内腔を塞いで腸閉塞を起こしたり、腫瘍から出血したり、肝臓や肺などの他臓器への転移を起こす等して、生命に危険が及ぶことが予想されます。がんを取り除き、そのような危険を回避するために治療が必要です。
大腸がんの治療には、手術、抗がん剤、放射線などがありますが、治療の中心は外科手術になります。
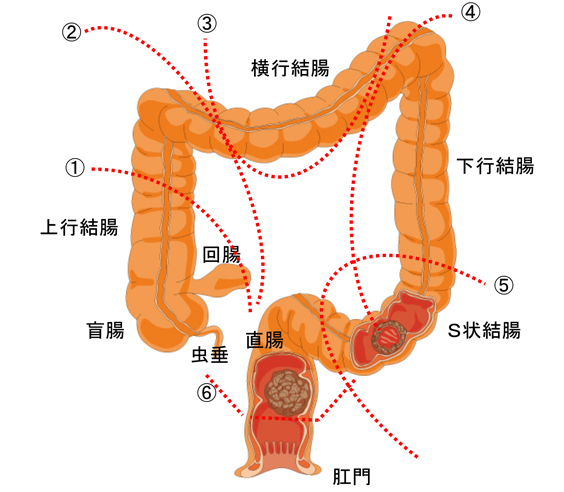
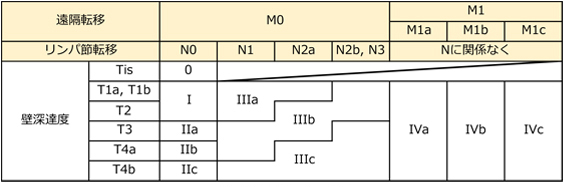
手術の種類は、①回盲部切除、②右半結腸切除、③横行結腸切除、④左半結腸切除、⑤S状結腸切除、⑥直腸切除術、直腸切断術(人工肛門造設)など、がんの局在に応じて変わります。手術の方法としては、従来から行われている開腹手術と、お腹に5mmから1cmの小さな傷を5ヶ所ほどつけて大腸を切除する腹腔鏡手術が中心となっています。
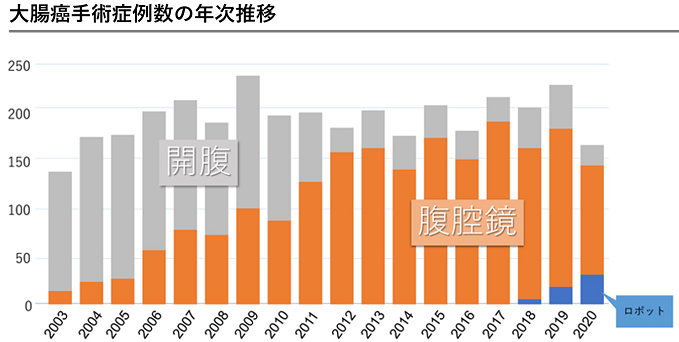
当科における大腸がん手術数は、2019年は218件の大腸がん患者に手術を行いました。そのうち179件(82%)を腹腔鏡手術で施行し、大腸がん手術の年間手術数は近隣府県の中でもトップクラスになっています。
当院では、大腸がん手術において、積極的に腹腔鏡手術に取り組んでいます。特に、腹腔鏡手術の高度技能医として学会から付与される内視鏡外科学会技術認定医の資格を持つ複数のスタッフが中心となり、より身体にやさしく、質の高い手術治療を提供できるように取り組んでいます。
また、高齢者や肥満者も腹腔鏡手術の適応外とはせず、開腹手術既往者もできる限り癒着に注意して腹腔鏡手術を行っています。全身状態(心・肺・肝・腎機能)不良者でも全身麻酔に耐えられれば適応としています。
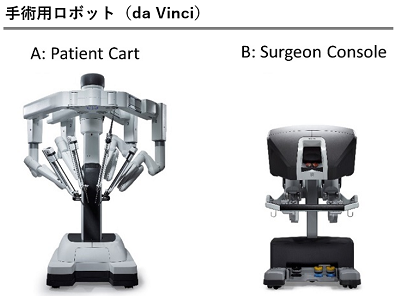
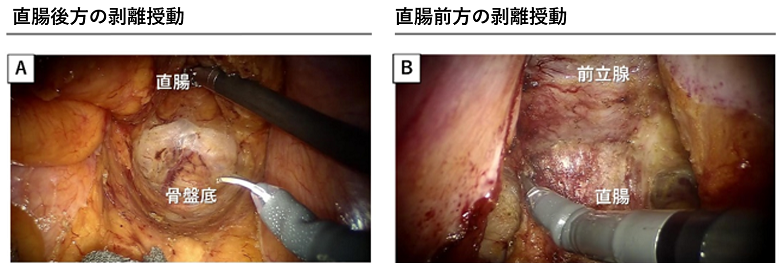
ロボット支援下直腸手術について
大腸は臓器の構造や位置の違いを目安として、結腸と直腸に大きく分類されています。ロボット支援による結腸および直腸切除術は、腹腔鏡下結腸・直腸切除術をロボット支援下に行うものです。現在は、“ダヴィンチ”というアメリカで開発された手術支援ロボットを中心として使用していますが、近年開発された国産のロボット機器などを含めて、最先端機器の導入も予定しています。
外科におけるロボット支援(ダヴィンチ)手術に関してロボット支援下手術は、従来の開腹手術と比較して、傷が小さく痛みが軽度で、術後の回復が早い、術中の出血量が少ないなど、従来の腹腔鏡手術がもつ利点を同じく有しています。特筆すべきは、ロボット機器の最大の特徴である「複雑に曲がるロボット鉗子の支援」があるために、手術機器の先端を指のように自由に曲げることが実現できるため、術野での繊細かつ緻密な操作が可能となり、腹腔鏡手術では実現が困難な手術手技が可能になるという利点も有しています。ですので、従来の開腹や腹腔鏡手術と同様以上の利点に加えて「より繊細かつ精密な手術」が可能になります。
繊細かつ緻密な手術を行うことは、周囲臓器へのダメージの軽減、根治性の向上が期待できます。特に直腸の場合は、密接する骨盤神経叢(排尿や性機能を担っている神経)を繊細な操作で丁寧に温存することにより、術後の排尿・性機能の保持や早期の回復が期待でき、“後遺症の少ない・体に優しい”手術が可能となります。また、一般的に直腸がんというと人工肛門というイメージがあり、実際にがんが肛門に近くなればなるほど人工肛門となる可能性が高くなります。ロボット手術では、狭い骨盤内であっても精緻な動きを得意とするロボットの特性を十分発揮することで、骨盤奥深くまで操作ができることから、より多くの患者さんに肛門温存が可能となります。肛門等の機能温存を実現することは、患者さんにとって術後の生活の質向上に有益と考えられます。
以上の理由から、大腸がんにおいては、先行して直腸がんに対して積極的にロボット手術を取り入れてきました。そして、最近では結腸がんに対しても積極的にロボット手術を導入しています。
手術後の経過
術後の入院期間は約1週間ですが、がんの部位・進行度やお腹の中の状態(癒着や肥満)などで状況が異なります。個々の患者さん・ご家族へ説明を行い、十分な理解のもとに受けていただくように心がけています。さらに最新の術後回復強化プログラムを導入し、早期の回復に努めております。手術をすれば当然、生体に大きなダメージが加わります。手術によるダメージを可能な限り抑え込んで、できるだけ早い段階で、術前の元気な状態まで回復してもらおうというのが目的です。そのためには、医師、看護師だけでなく、薬剤師、理学療法士、栄養士、ソーシャルワーカー、医療事務など患者さんに係わる職員がチームとしてかかわっていきます。
手術に伴う危険性と合併症としては、出血、感染、縫合不全などがあり、ドレナージ手術、人工肛門造設などが必要になる場合があります。結腸癌手術では約1.5%に合併すると言われています。直腸手術にともなう後遺症では、神経障害(排尿障害、排便障害、性機能障害)などがあげられます。できるだけ合併症を回避できるよう予防し、それでも発生した場合はできるだけ早く発見し、対応・処置していきます。
大腸の手術(とくに直腸の手術)においては、人工肛門を作成することがあります。一時的なものになる場合もあれば、永久になる場合もあります。人工肛門を作成した場合には、看護師を中心にして人工肛門ケアの仕方について丁寧に指導します。当院には人工肛門ケア専門の認定看護師が複数名おり、退院後の長期的なフォローも行います(ストーマ外来)。
抗がん剤治療について
手術以外の治療は、抗がん剤治療があります。がんの進行度(ステージ)により異なります。大腸がんに対する抗がん剤治療には目覚ましい進歩があり、一定の効果が期待できるようになっています。
少し進行して、肝臓や肺などへの転移が認められても、手術が可能な病状であれば手術により根治できる場合があります。完全に切除することが難しい転移が起こってから、がんが発見された場合は、手術に加え抗がん剤治療が行われます。また、直腸がんに対しては、手術前に抗がん剤治療を行い、病気をより小さくしてから手術を行うこともあります。手術後の再発予防のために抗がん剤を使用することもあります。
手術後に再発した場合でも早い時期に見つかれば、切除により根治できる可能性がありますが、多くは抗がん剤治療が中心となります。抗がん剤治療は、当院では腫瘍内科と連携して行っています。抗がん剤治療に先立ち、効果があるかどうかを調べるために遺伝子検査を行い、また抗がん剤治療が円滑に行えるように、中心静脈リザーバーを留置します。 このように、大腸がん(結腸がん・直腸がん)対する手術技術や抗がん剤治療は日々進歩しており、特に、進行した大腸がんに対する治療は、手術のみならず、抗がん剤治療を含めた、総合的な治療戦略の構築が必要となります。当院では、腫瘍内科や関係診療科ともに、診療科の垣根を越えてより良い治療戦略を決定していく診療システムを導入しています。
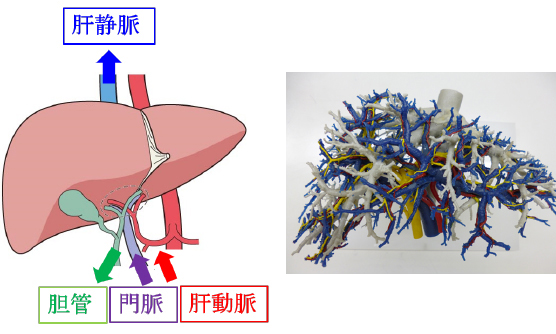
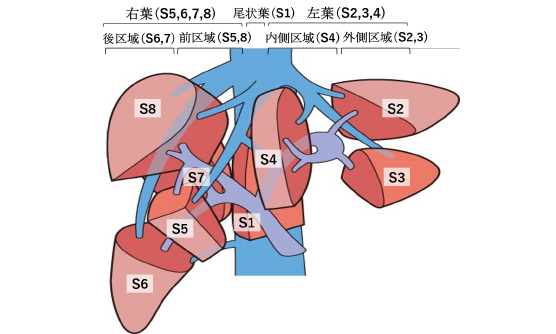
肝臓の解剖と機能
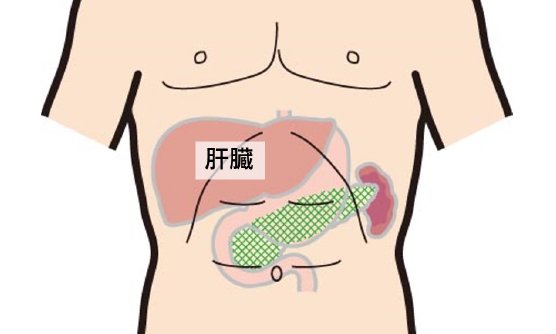
肝臓は栄養を蓄える、タンパクを作る、薬や毒物を分解する、消化液である胆汁を作る・・・など多くの機能をもっています。そこで肝臓の機能を評価するにはこれらさまざまな機能を組み合わせて総合的に行う必要があり、肝臓の治療に差し当たっては以下のChild-Pugh分類に基づいて安全な治療法を選択します。
Child-Pugh分類(チャイルド・ピュー分類)
5つの項目を用いて、肝臓の働きを評価する方法です。そしてその合計点で肝硬変を初期から末期まで分けます。
| 検査値など | 点数 | ||
| 1点 | 2点 | 3点 | |
| ビリルビン値 | 1~2 | 2~3 | >3 |
|---|---|---|---|
| アルブミン値 | >3.5 | 2.8~3.5 | <2.8 |
| 腹水 | なし | 軽度 | 中等度 |
| 脳症 | なし | 1~2 | 3~4 |
| プロトロンビン時間 | >80 | 50~80 | <50 |
肝臓の腫瘍
肝臓は良性・悪性を含む様々な腫瘍が発生し多くの腫瘍が手術の対象となりますが、外科で手術適応となる主な病気は肝癌です。肝癌には肝臓自体から発生した原発性肝癌と、他臓器の癌が肝臓に転移した転移性肝癌があります。
- 原発性肝癌は多くが肝細胞癌で、他に肝内胆管癌などがあります。
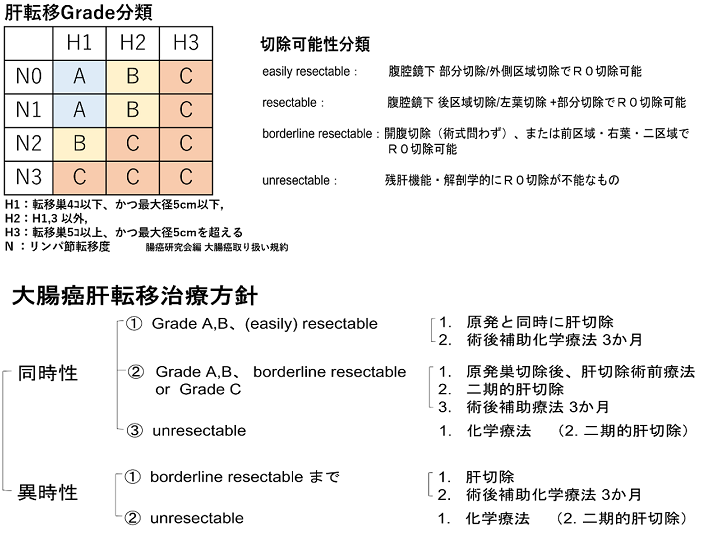
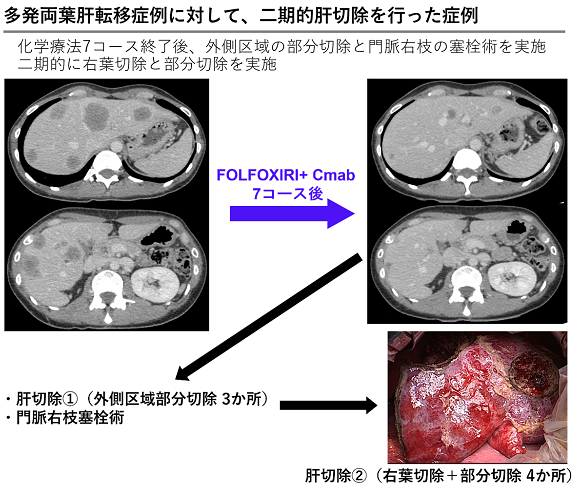
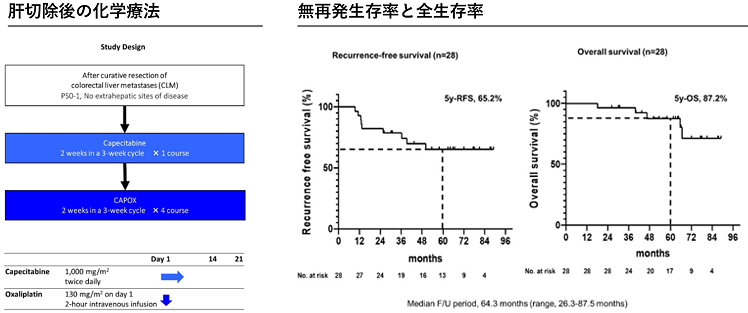
- 転移性肝癌は胃癌、大腸癌などの消化器癌の他に、肺癌や乳癌なども肝転移を来します。癌種によって治療方針は異なりますが、大腸癌からの転移性肝癌の場合は肝転移を切除することで根治できる可能性があるため、化学療法と併せて積極的に手術を行います。
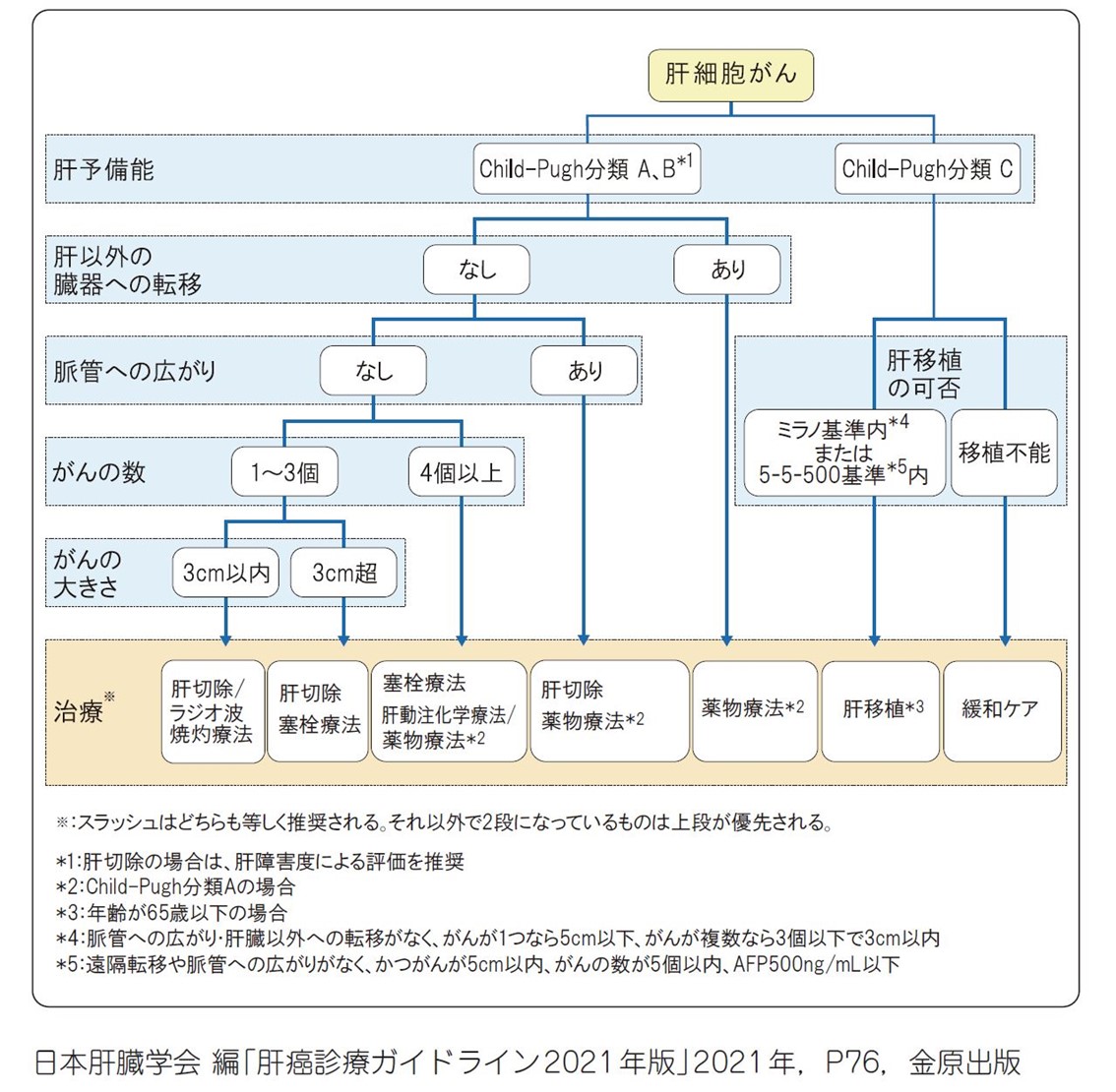
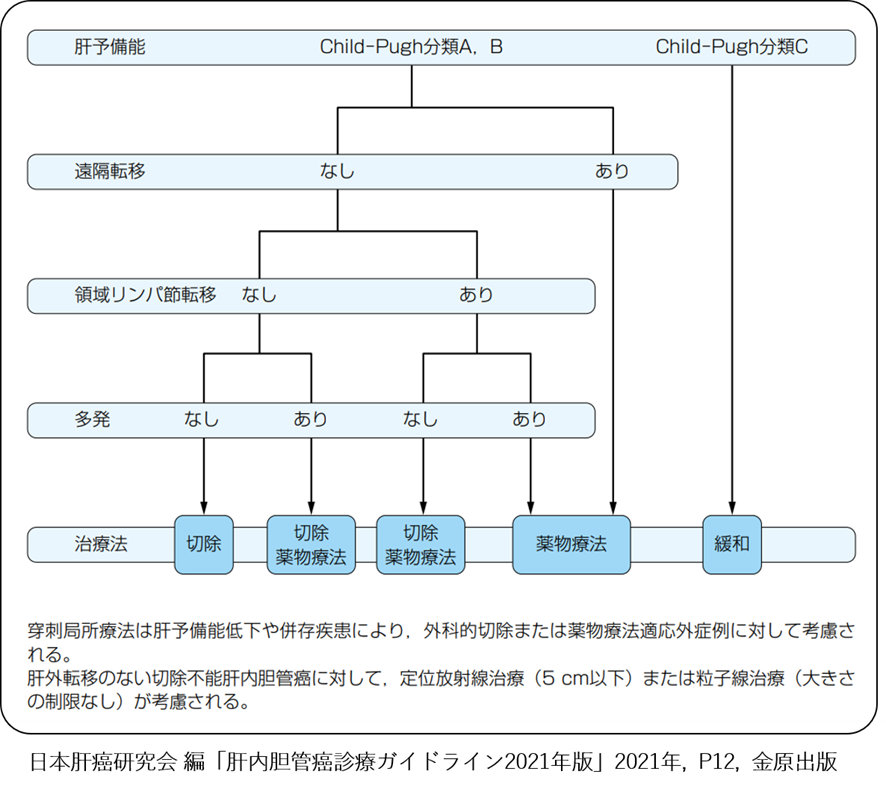
原発性肝癌の治療
肝細胞癌の治療法には、手術(肝切除)の他、ラジオ波焼却治療、塞栓療法、動注療法、薬物療法や放射線治療(詳細は当院消化器内科 – 肝癌に対する集学的治療の項を参照ください)、肝臓移植(詳細は肝臓移植の項を参照ください)などの方法があります。
これら治療のどれが治療として最も適切かは、患者さんそれぞれの状況により変わります。そこで肝臓癌の治療方針としての指針が『肝臓診療ガイドライン』として提唱されており、このガイドラインに沿って治療を行っています。
肝内胆管癌の場合、手術適応や術式は、腫瘍の占拠部位や大きさ、リンパ節転移の有無、胆管浸潤の有無、肝内転移の有無などの進展様式を考慮し選択します。
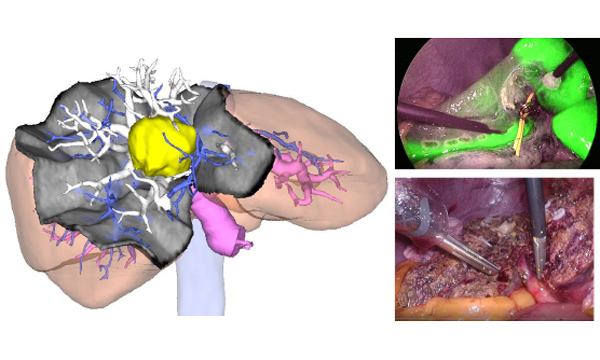
肝切除術
切除範囲

手術時間はこれら術式により、3時間ほどで切除できることもあれば10時間以上かかることもあります。
切除法
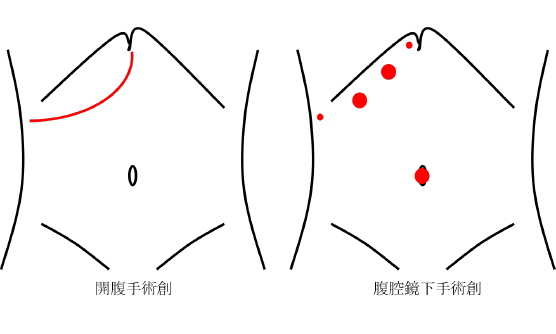
従来行われてきた開腹手術に比べて低侵襲手術は小さな創となるため術後の回復が早く整容性の面だけではなく、出血量も少ないなどのメリットはありますが、腫瘍の位置や大きさによって低侵襲でできる手術は制限されます。現在では約7割の肝切除を低侵襲手術で行っています。
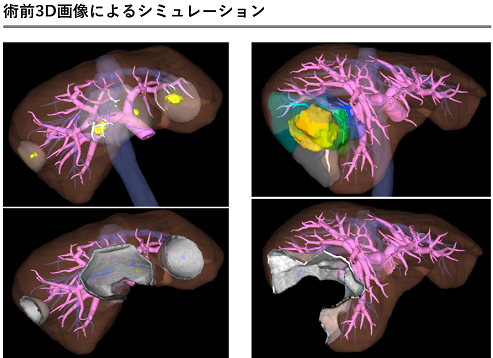
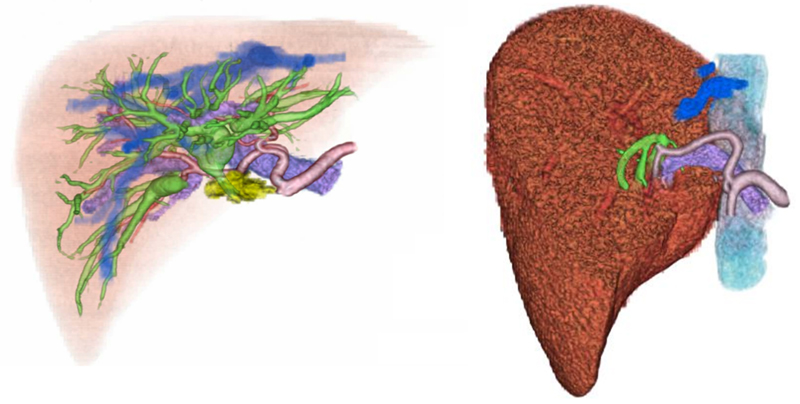
シミュレーション/ナビゲーション
術後の経過
術後は2日目くらいから食事が始まり、入院期間は早い人で1週間程、平均で2週間程です。
個人差はありますが、術後1か月程で社会復帰できます。
肝切除術後の合併症としては出血、胆汁漏、腹水や胸水、肝不全などがあり、残念ながら合併症が生じた場合は入院期間が長くなることもあります。
肝癌手術後は残った肝臓に再発する可能性がありますので、術後も3-6か月毎に採血、エコー検査、CT検査などを受けて経過を観察します。
当科では肝移植を受けられた方や生体肝移植のドナーになられた方の外来フォローを行っています。また肝移植についてのご相談も承っています。下記に肝移植の一般的なことについて簡単にご説明します。
1.生体肝移植とは
重篤な肝臓病で内科的な治療では回復が見込めない状態の方に対して別の人から提供された肝臓を移植する治療が肝移植です。健康な人から肝臓の一部を取り出して移植する手術を生体肝移植といい、脳死ドナーからの移植を脳死肝移植といいます。生体肝移植は1988年に世界で初めて行われ、日本では1989年から始められてこれまでに10,000件以上の生体肝移植が行われています。一方、脳死肝移植は日本では1999年に初めて行われ、これまでに700件余り行われています。最近は、生体肝移植が年300~400件、脳死肝移植が年60~90件ほどとなっています。
肝移植は重篤な肝疾患のため予後不良となっている、あるいはQOLが著しく損なわれている患者さんが対象となります。種々の肝疾患が適応となっていますが、概ね下記のような病気の方に移植手術が行われています。
〈対象疾患〉
- 非代償性肝硬変(肝炎ウイルス性、二次性胆汁性、肝癌合併など)
- 先天性胆道閉鎖症などの先天性肝・胆道疾患や先天性代謝異常症
- 原発性胆汁性胆管炎、Budd-Chiari症候群、原発性硬化性胆管炎など
しかし、上記の病気であれば誰でも肝移植を受けられるわけではありません。肝移植は身体的負担の大きい治療であるため、移植を受ける方(レシピエント)の年齢は70歳まで、生体ドナーとなる方の年齢も65歳までと概ねされています(施設により異なります)。
2.手術の内容
移植手術では、まず臓器提供者(ドナー)の肝臓(全部あるいは一部)が取り出されます。脳死ドナーでは肝臓全部、生体ドナーでは肝臓の一部(外側区域(肝臓全体の約1/4)、肝左葉(約1/3)、肝右葉(約1/2~2/3))を摘出します。肝臓のどれぐらいを移植するかは、レシピエントの体格と提供者の肝臓の大きさによって決められます。
レシピエントの方の肝臓は全部取り除かれて提供者からの肝臓を移植します。移植される肝臓の血管とレシピエントの血管がすべてつながれて血流が再開すると移植された肝臓は働き始めます。次に移植された肝臓の胆管とレシピエントの胆管(または腸管)を縫い合わせて胆汁の流れ道を作り直し、おなかの傷を閉じて移植手術は終了します。通常、生体ドナーの手術で6~8時間、レシピエントの手術で10~12時間ほどかかります。
3.移植手術の危険性と合併症
肝移植は大手術で多くのリスクがあり、手術により死亡する危険性がないわけではありません。手術は肝臓手術の経験が豊富な医師によって行われますが、術前の患者さんの状態が悪い場合にはそのぶん手術のリスクも高くなります。
手術の合併症としては、出血、つないだ血管の閉塞、胆汁漏や胆管狭窄、腸閉塞など種々のものがあります。またその他にも拒絶反応や感染症、人工透析が必要になるほどの腎不全などいろいろなリスクがあります。
手術直後から複数の免疫抑制剤が投与されます。免疫抑制剤は拒絶反応を防ぐために必要ですが、本来の免疫力も低下させるため感染症が起こりやすくなるため注意が必要です。また薬剤自体の副作用として高血圧や糖尿病などで治療が必要になることもあります。
拒絶反応には急性拒絶反応や慢性拒絶反応がありますが、いずれの場合も免疫抑制剤による治療が必要です。もし治療が奏功しなければ、最終的に移植した肝臓が働かなくなり肝不全となります。そのため拒絶反応を防ぐために免疫抑制剤の服用を続けることがとても重要です。
4.術後の一般的な経過
レシピエントは術後しばらく集中治療室に入り、それから一般病棟で治療が続けられ、特に問題がなければ1~2ヶ月で退院となります。入院中は血液検査や超音波検査を何度も行い、何か問題があれば、CT検査、肝生検、胆管造影、胃カメラなどの検査が検討されます。
生体ドナーは1~2週間ほどの入院が一般的で、自宅療養を経て通常の生活に戻ります。
退院後は定期的に通院します。レシピエントは生涯免疫抑制剤の服用を行うため通院の継続が必要です。生体ドナーも術後しばらくは通院して身体状態をチェックします。
5.肝移植の成績
肝移植を受けられた方の5年生存率(移植5年後に生存している方の割合)は成人で約70-80%、小児で約80-90%といわれており、脳死肝移植と生体肝移植で差はありません。しかし、病気の種類や手術前の状態などにより成功率は異なります。
生体ドナーの安全性は生体肝移植では最大の要件です。ほとんどのドナーが日常生活に復帰できるほどに回復していますが、生体肝移植でドナーが死亡したケースはこれまでに世界で10例以上報告されており日本でも1例報告されています。
6.肝移植による利益
肝移植の最大の利益は、移植を受けないと近いうちに亡くなってしまうと思われる患者さんがこの治療により健康人と同じぐらいの生活を取り戻せる可能性があるということでしょう。しかし、肝移植の歴史はまだ浅く、移植後にどれぐらい長期にわたりこの状態を維持できるかに関してはまだはっきりとはわかっていません。
胆道について
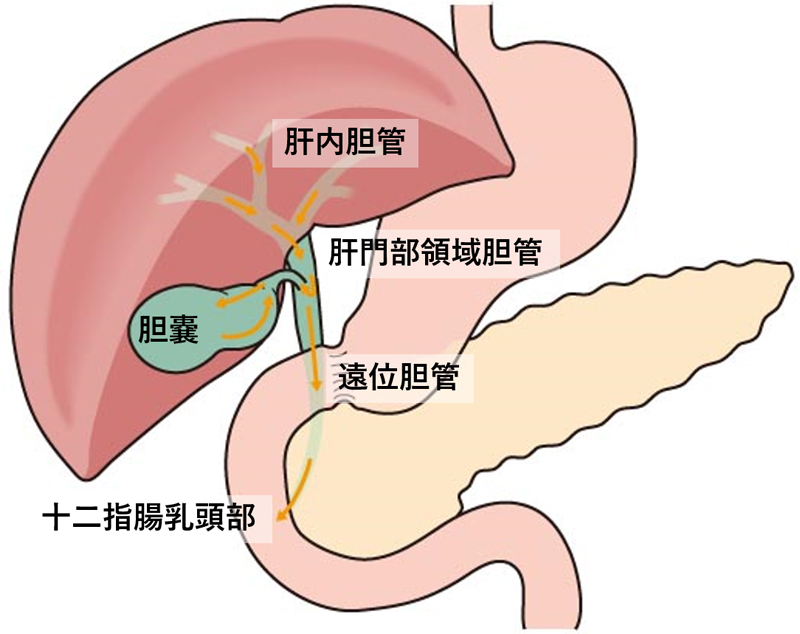
胆道の疾患 ①胆道癌
胆道癌はその発生部位によって「胆管癌」と「胆嚢癌」に分けられ、胆管癌は肝内胆管癌、肝門部領域胆管癌、遠位胆管癌、十二指腸乳頭部癌に分けられます(肝内胆管癌については肝疾患の項をご参照ください)。胆道癌は自覚症状が出にくいため早期発見することは難しいですが、病気が進行すると癌で胆管が狭くなり胆汁の流れを妨げるため黄疸(皮膚や白目が黄色くなる)の症状が現れます。また肝臓やリンパ節、その他の臓器に浸潤、転移して癌は広がっていきます。
治療法としては手術の他に化学療法(抗癌剤治療)や放射線治療などがありますが、手術が唯一治癒を望める治療法です
手術
胆道癌に対する手術の方法は癌が発生した場所によって様々で進行度によっても切除する範囲が変わります。手術内容によって手術時間は違いますが、短いものでも数時間、長い場合は10時間以上かかることもあります。
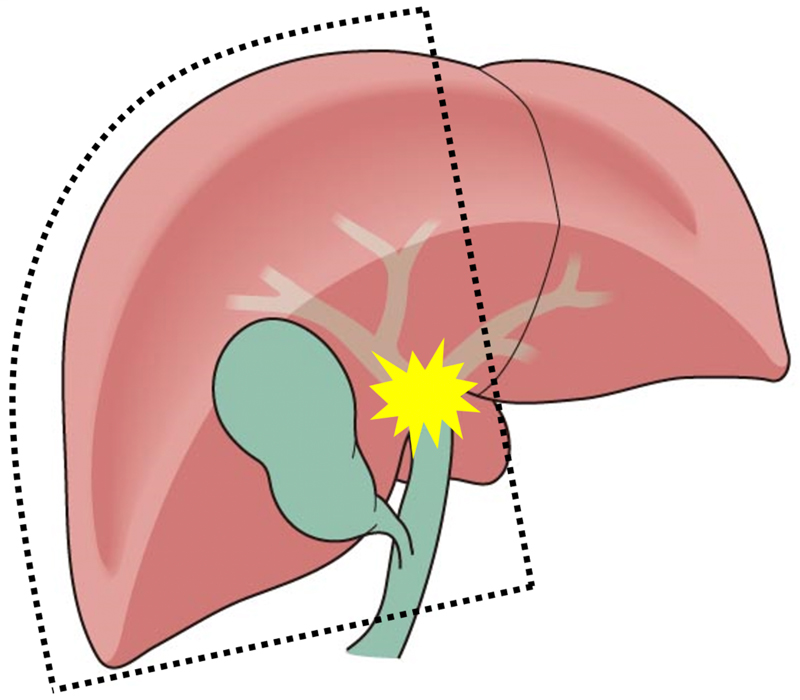
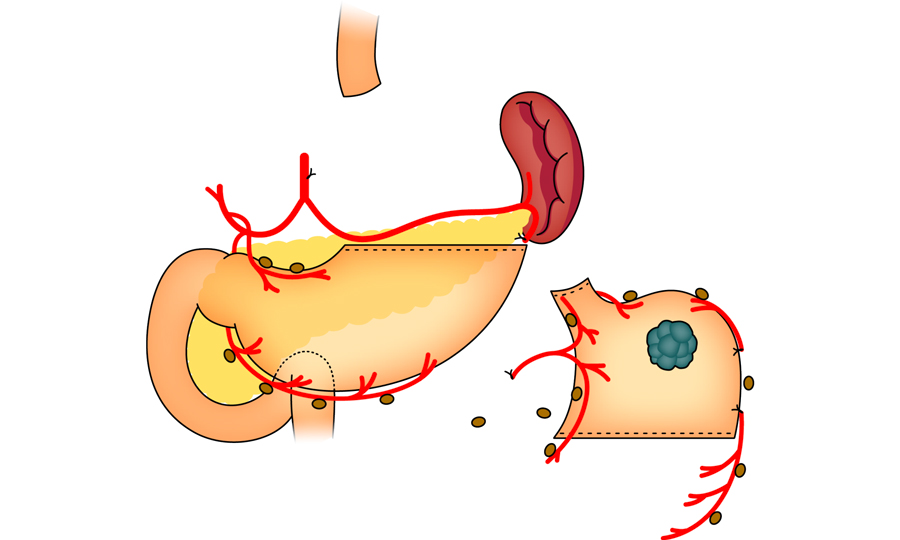
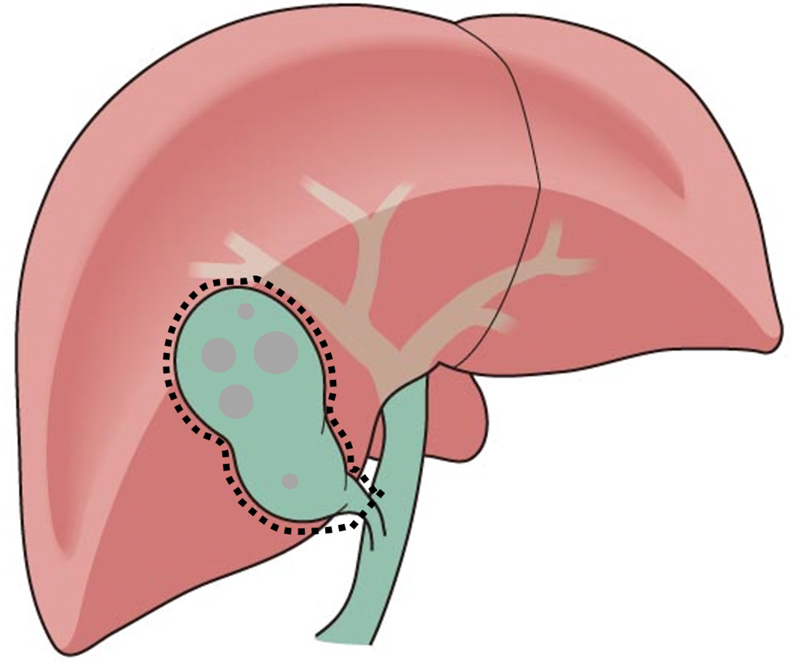
胆嚢癌の場合、初期であれば胆嚢摘出術で十分ですが、進行して隣接する肝臓や胆管、リンパ節などにも癌が広がっているときはその分切除範囲は広くなり、胆嚢だけでなく肝臓、胆管、リンパ節を含めた切除が必要になります【図4】。
手術前の準備
黄疸がある場合、手術の安全性に影響するため術前に胆道ドレナージという黄疸をとる処置を行います。内視鏡を使って胆管に管を入れる方法(内視鏡的ドレナージ)が主流です。
広範囲の肝切除が必要な場合には、術後の肝不全を防ぐため術前に切除側の肝臓の血管(門脈)をカテーテルで詰めて(門脈塞栓術)、残す側の肝臓の肥大再生を促してから手術を行うことがあります。
手術後の経過
術後は順調に経過すれば2~3週間ほどで退院できますが、出血、胆汁漏、膵液漏、感染症などの合併症の治療が必要になると入院期間は長くなります。
退院後は定期的に通院して血液検査やCT検査で再発の有無をチェックします。また病気の状況により内科と連携して化学療法(抗癌剤治療)を行うことがあります。
胆道の疾患 ②胆石症やその他の良性疾患
胆道に石ができる病気を胆石症といい、胆嚢に石ができる胆嚢結石症が一番よくみられます。無症状で腹部エコーやCT検査で偶然見つかることもありますが、胆石発作や胆嚢炎、胆嚢結石が胆管に流れて胆管結石となって症状を起こすこともあります。
症状としては食後や夜間に生じる右季肋部痛や右背部痛が比較的多いですが、胃痛や腰痛として自覚することもあり、痛みの部位や程度は様々です。通常、無症状の胆嚢結石でwは手術の必要はありませんが、一度でも胆嚢結石による症状(胆石発作、胆嚢炎、胆管結石)があった場合は手術をお勧めします。
胆嚢結石以外には胆嚢ポリープや胆嚢腺筋腫症などで手術が検討されることがあります。胆嚢ポリープの大きさが1cm以上など癌の可能性が考えられる場合には手術が勧められます。
手術
おなかに3、4か所の穴をあけて腹腔鏡や鉗子(かんし)を挿入して胆嚢を摘出します。開腹手術に比べて傷が小さいため術後の回復が早いです。しかし、以前に上腹部の手術を受けたことがある方や胆嚢の炎症が強い場合には、腹腔鏡手術が難しく開腹手術で行うことがあります。
手術後の経過
通常、腹腔鏡下胆嚢摘出術の場合、手術当日に入院して翌日退院です(1泊2日)。開腹手術の場合は1週間ほどの入院が必要になります。 胆嚢を摘出してもほとんどの場合後遺症はありません。脂肪分の消化が低下し下痢気味になることがありますが、時間の経過とともに治まります
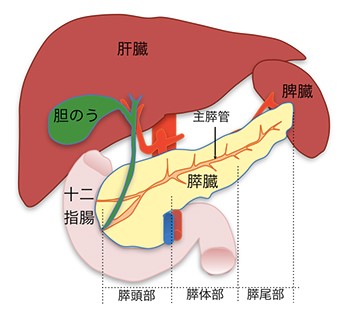
1)膵臓について
1つめは、膵液という消化液を作り、十二指腸へ分泌しています。膵液は炭水化物、たんぱく質、脂質などを分解し、食物の消化・吸収に大きな役割を果たしています。
2つめは、インスリン・グルカゴンなどのホルモンを血液中に分泌しています。これらは血液中のブドウ糖濃度(血糖値)を一定に調節するホルモンで、これらのホルモンの分泌機能に異常を生じると、糖尿病になることが知られています。したがって、膵臓を切除した場合には糖尿病が悪化する可能性があります。
2)膵疾患について
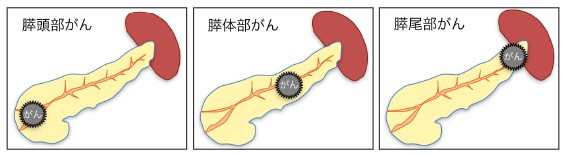
膵臓癌 (浸潤性膵管癌)
膵管から発生し、周囲に広がっていく癌です。場所により「膵頭部癌」「膵体部癌」「膵尾部癌」に分けられます。このうち膵頭部癌は十二指腸、胆管と接し、肝臓にも近いためそれらの臓器にも影響を与えます。
膵嚢胞性腫瘍
膵臓の粘液を作る細胞から腫瘍が発生したことにより「嚢胞」という大小の袋状の腫瘍が出来るものです。
| 膵管内乳頭粘液性腫瘍(IPMN) | 良性の腺腫から悪性の腺癌までさまざまなものがあり、良性から悪性へと次第に変化していきます。サイズが大きい場合や、徐々に大きくなる場合などは悪性化している可能性が高くなります。 |
|---|---|
| 膵神経内分泌腫瘍(P-NET) | 膵臓内のインスリンなどのホルモンを産生する細胞から発生する腫瘍です。ホルモンが過剰に産生されますが、症状がある場合とない場合があります。近年増加傾向にあり、悪性のリスクがあります。 |
| 粘液産生膵腫瘍(MCN) | 女性に多く40代~50代の方に多く見られます。高い頻度ではありませんが、悪性のリスクがあるとされており、診断がついた場合には手術治療が必要です。 |
| 漿液性嚢胞性腫瘍(SCN) | 中年の女性に多く、比較的大きな嚢胞の腫瘍になります。良性の可能性が高く悪性であることは稀な疾患ですが、大きさが増大する場合には手術治療が勧められます。 |
3)膵臓癌の治療について
膵臓癌の治療選択
膵臓癌の治療には外科手術、手術以外の治療、支持療法があります。
| 外科手術 | 膵臓の一部分あるいは全体を切除します。さらに状態に応じて、胃、胆道、十二指腸、脾臓、リンパ節など周辺の臓器も取り除く場合があります。 | 膵頭十二指腸切除術/膵体尾部切除術/膵全摘術/その他の外科手術/緩和手術(バイパス手術) |
|---|---|---|
| 手術以外の治療 | おもに抗がん剤による化学療法と、放射線療法があります。 | 化学療法/化学放射線療法/放射線療法/その他の抗腫瘍療法 |
| 支持療法 | 本来の治療を補助する治療で、膵がんでは術前の黄疸の治療や術後の合併症の治療、がんの症状をやわらげる治療などがあります。 | 胆道ドレナージ/十二指腸ステント/合併症・副作用の治療/緩和療法/カウンセリング |
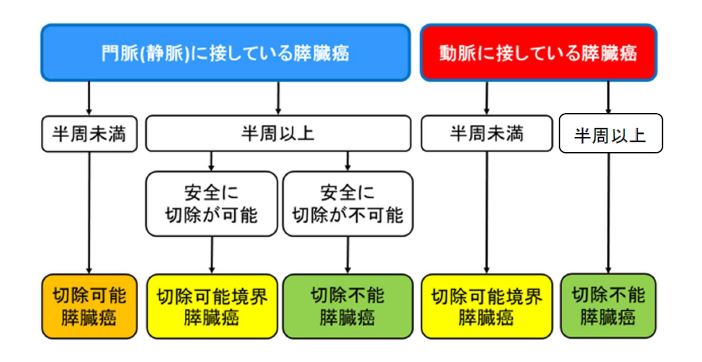
膵臓癌の分類
膵臓癌の取り残しのない手術(根治切除術)が出来るかどうかの観点から、切除可能膵臓癌、切除可能境界(ボーダーライン)膵臓癌、切除不能膵臓癌の3つに分けられます。
| 切除可能膵臓癌 | 癌が他の臓器に転移していない、もしくは膵臓の周囲の血管に浸潤していないもの |
|---|---|
| 切除可能境界(ボーダーライン)膵臓癌 | 癌が膵臓の周囲の血管に浸潤しているが切除可能なもの、もしくは化学療法で癌が小さくなり切除が出来る可能性があるもの |
| 切除不能膵臓癌 | 癌が全身に広がり他の臓器に転移している、もしくは膵臓の周囲の血管に広範囲に浸潤しているもの |
膵臓癌では、外科切除による癌細胞の完全切除(=根治切除)により完治する可能性があります。そのため切除が出来るかどうかが治療選択の大きなポイントになります。
癌が膵臓から遠い臓器やリンパ節および腹膜に転移している場合、膵臓に隣接する大血管などに浸潤がある場合などには、完全切除は不可能となり、化学療法や放射線治療を選択していくことになります。
最新のガイドラインでは術前化学療法を行うことで根治できる可能性が上がるため、切除可能膵臓癌に対しても積極的に手術前に抗がん剤治療を行うことが推奨されています。 切除可能境界(ボーダーライン)膵臓癌の場合、膵臓周囲の血管へ浸潤した癌を縮小させ、切除可能にする目的で手術前に抗癌剤治療や放射線治療を行う場合があります
膵臓癌の外科手術
膵臓癌の外科手術における切除範囲が、癌がどこの部位に発生しているか、どれくらいの進行度であるかによって異なってきます。
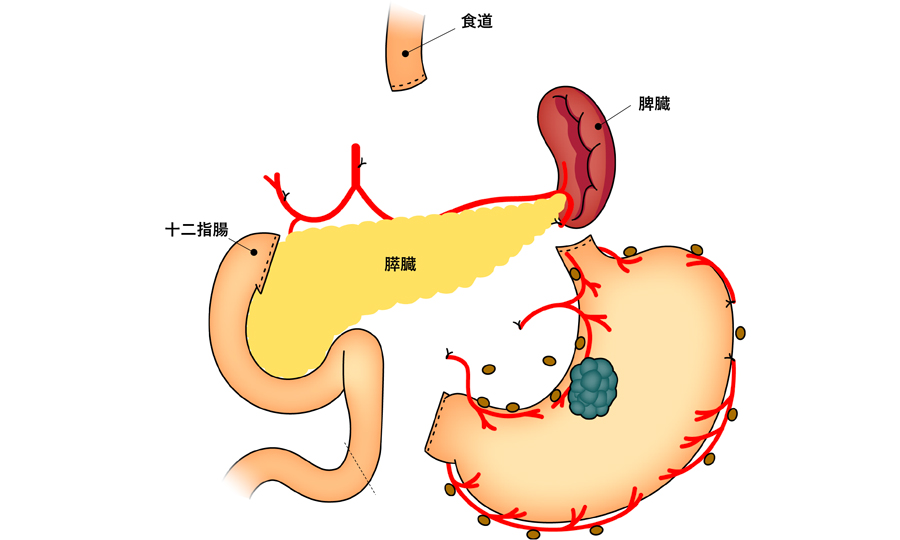
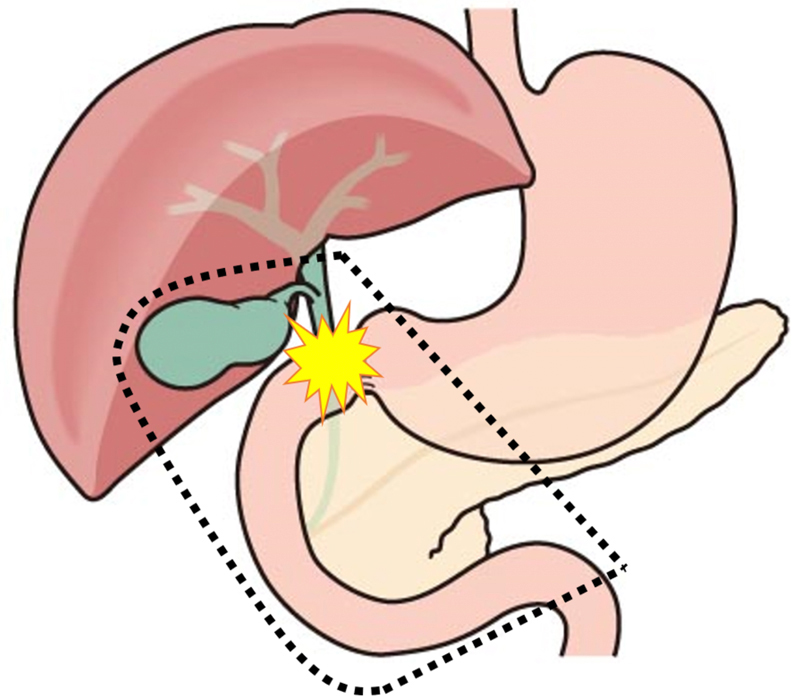
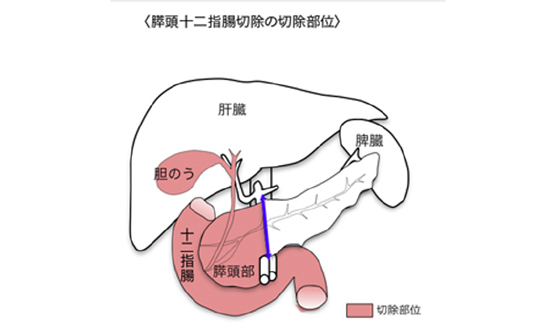
① 膵頭十二指腸切除術
癌の周囲への浸潤が強い場合は、門脈という重要な血管を一部切除した上で再建したり(=門脈合併切除)、上腸間膜動脈という動脈の周囲の神経叢を切除したりする拡大手術を行います。
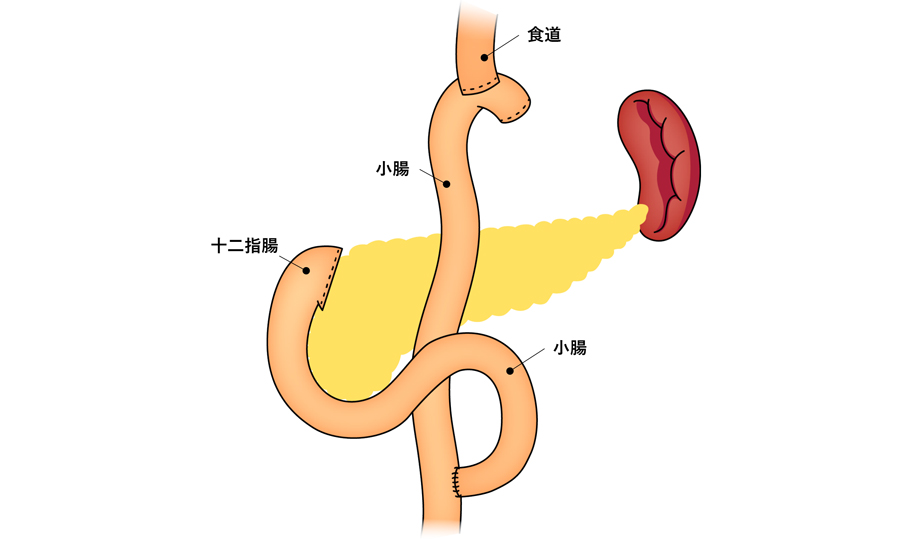
この手術では、膵臓、胆道、胃をそれぞれ空腸とつなぐ消化管の再建手術を行い、膵液、胆汁、食物を流すルートを作り直します。
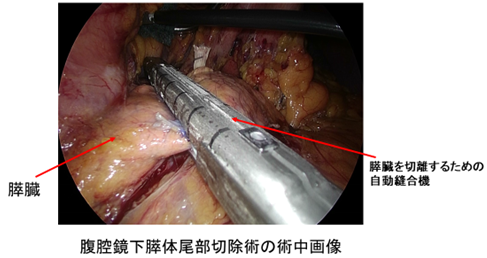
② 膵体尾部切除術
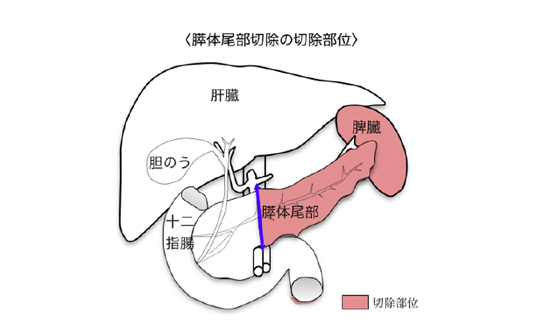
〈腹腔鏡下膵体尾部切除術〉
膵粘液性嚢胞腫瘍などは比較的若年の女性に発生しやすく、手術創が小さい低侵襲手術として当院では良性または良悪性境界疾患に対して積極的に腹腔鏡手術やロボット支援下手術を行っています。傷が小さいため整容性に優れており、からだへの負担を減らすことで手術後の早期回復につながります。また一部の膵臓癌に対しても、癌の進み具合を考慮しながら症例を選択して腹腔鏡手術やロボット支援下手術を行っています。
③ その他の外科手術
膵臓癌やIPMNなどが膵臓の広い範囲に存在している場合、膵臓全体を切除する場合があります(=膵全摘術)。この場合、インスリンが全く分泌できなくなるため、手術後にはインスリンの自己注射が不可欠となります。
癌が他の臓器への転移や周囲への浸潤のため切除不可能な場合で、胆管や十二指腸が癌によって閉塞してしまっているときには、胆汁や食物を小腸へと送る通路をつくる手術(=バイパス術)を行うこともあります。最近では胆管ステントや十二指腸ステントなどの医療機器が発達してきており、手術は行わずに治療することも多くなっています。
術前化学療法について
膵臓癌に対する術前治療が標準的となってきており、切除可能膵癌および切除可能境界膵癌に対する術前化学療法を行っています。術前化学療法の利点として、腫瘍が小さくなると根治切除率の向上が得られることや化学療法に対する感受性の判断などが出来る点があります。
術後補助療法について
外科手術の後に、ステージI期以上と診断された癌であれば再発の可能性があり抗癌剤による術後補助化学療法が推奨されます。これによって癌の再発を予防したり、再発までの期間を延ばしたりすることが期待できます。
手術後早期の合併症
術後比較的早期に起こる可能性のある合併症には、以下が挙げられます。
① 膵液漏
膵臓の手術に特有の合併症です。これは「膵頭十二指腸切除術」における膵臓と小腸をつないだ部位や、「膵体尾部切除術」における膵臓の断端などから、膵臓から分泌される消化酵素を含む膵液がお腹の中に漏れ出ることです。膵液は食物を溶かす働きがありますが、胃や腸の中では粘膜が保護しているため自分の組織まで溶かすことはありません。しかしお腹の中に膵液が漏れたときには、周囲の組織を消化するように溶かし腹膜炎を併発することがあります。血管を溶かしてしまった場合には出血することもあります。膵液が漏れる膵液漏が発生しても、膵液が腹腔内に貯まらずに外へ出るように誘導すること(=ドレナージ)が出来れば、ほとんどの場合膵液漏は自然に治癒します。膵液漏の程度によりますが、治癒まで2週間から長い場合は1ヶ月ほどの長期間の治療が必要になる場合があります。
② 出血
膵臓の周りには動脈や静脈が非常に多く、手術後に手術で操作した部位から出血する場合があります。また膵液漏に伴う合併症として出血をきたす場合もあります。輸血で対応しますが、膵液漏による動脈性の出血は血管内カテーテル治療で止血を行います。
③ 縫合不全
膵頭十二指腸切除の場合には膵臓と小腸以外にも、胆管と小腸、胃と小腸をつなぐ必要があり、つないだ場所から消化液が漏れ出る場合があります。この場合も膵液漏と同様にドレナージを行って治療をします。
④ 感染
創感染や腹腔内の膿瘍など部位と程度に応じて処置や抗生剤治療を行います。
⑤ その他
深部静脈血栓症、肺塞栓症、乳び腹水、心・肺・脳血管の合併症など
膵臓切除後の後遺症
膵臓の切除後には、長期的にいろいろな後遺症が発生することがあります。
①食事摂取量の低下、低栄養状態、ダンピング症候群、体重減少など
手術後一定の期間を経過すれば、改善していくことが見込まれます。
② 糖尿病の悪化
もともと糖尿病がない場合でも、膵臓切除によりインスリンの分泌が減り糖尿病となり、内服治療がインスリンの自己注射などが必要となる可能性があります。また既に糖尿病がある方も、術後糖尿病のコントロールが悪化する場合があります。そのような場合には、当院の糖尿病・内分泌内科の協力のもと治療を行っていきます。
③ 下痢
膵臓を切除すると、消化液である膵液の分泌が減るため、脂肪の消化がうまくいかず下痢をしやすくなることがあり、結果として脂肪肝になることがあります。膵液の代わりとなる消化酵素剤を内服して治療します。
また膵臓癌の切除のために、上腸間膜動脈という動脈の周りの神経叢を切除することで、食後の下痢を起こすことが知られています。癌の進行度合いによりますが、なるべく神経叢を温存するような手術を行うことで予防しておりますが、ある程度の症状が出る可能性があります。
4)入院から退院までの経過
通常手術前日に入院して頂きます。術後1日目から体を動かすリハビリをはじめ、水やお茶が飲めます。術後5日目にCT画像検査を行い、特に問題がなければ食事が始まり、お腹に入っている管(ドレーン)は膵液漏がないと判断されれば術後5~7日目に抜けます。合併症がなければ術後2~3週間で退院することが多いですが、膵液漏などの合併症が起こった場合は入院期間が延長します。
術後の生活として重要なポイントは、積極的に体を動かすことです。立つ練習や歩く練習をすることで順調な回復につながり、寝ている時間が長いと筋力が低下するだけでなく合併症が起きやすくなります。
術後2~3日間は傷の痛みが最も強い時期です。手術の直前に背中から入れたチューブから痛み止めの薬が持続的に入り、痛みを取り除きます。その後も定期的に痛み止めの点滴を行うなど、痛みを取り除きながらリハビリをすることが術後の良い経過につながります。
5)外来通院について
進行度によっては再発予防のための術後化学療法が推奨され、消化器内科や腫瘍内科と協力して外来で治療を行います。通常、術後5年間の外来通院が必要であり、再発していないか評価するために、定期的な血液検査とCT画像検査(または腹部超音波検査、MRI検査、PET検査)を行います。
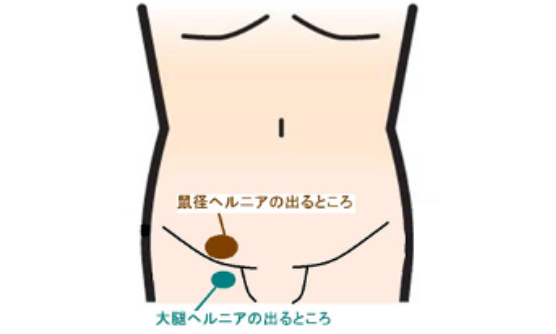
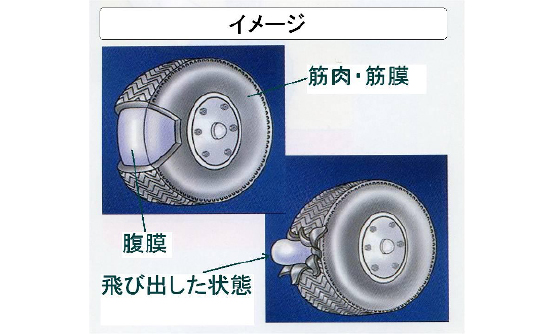
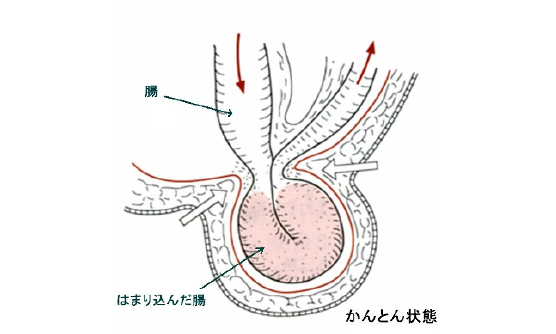
1)鼠径ヘルニアとは?
鼠径ヘルニアは、足のつけ根がふくらむ病気です。
鼠径ヘルニアは、足のつけ根がふくらむ病気です。太もものつけ根の部分(鼠径部)の筋肉の壁が弱くなって穴が開いた状態になり、その穴を通っておなかの中の腸や脂肪が腹膜という膜につつまれて袋状に飛び出す病気のことです。「ヘルニア」とは飛び出した状態のことを指します。腸が出てくることが多いので、俗に「脱腸(だっちょう)」とも言われます。
2)鼠径ヘルニアの原因と症状
子供の病気としても知られる鼠径ヘルニアですが、子供と大人では少し原因が異なります。子供の場合は生まれつきのものですが、大人の場合は年をとって体の組織が弱くなるために起こることが多いと考えられています。年齢以外にも、重いものを持つことが多いとか長時間の立ち仕事など、おなかの壁への負担が重なることで支える筋肉の壁が部分的に弱くなってだんだん穴が開いたようになり、そこから腸や脂肪が飛び出してくるのです。出てくる場所によって、鼠径ヘルニア(足の付け根)や大腿ヘルニア(太もも下寄り)と呼びます。
3)鼠径ヘルニアの手術
ヘルニアを治すためには手術が必要です。薬で治すことはできません。また、ヘルニアバンド(脱腸帯)というヘルニアのところを押さえこむベルトもありますが、根本的な治療ではありません。
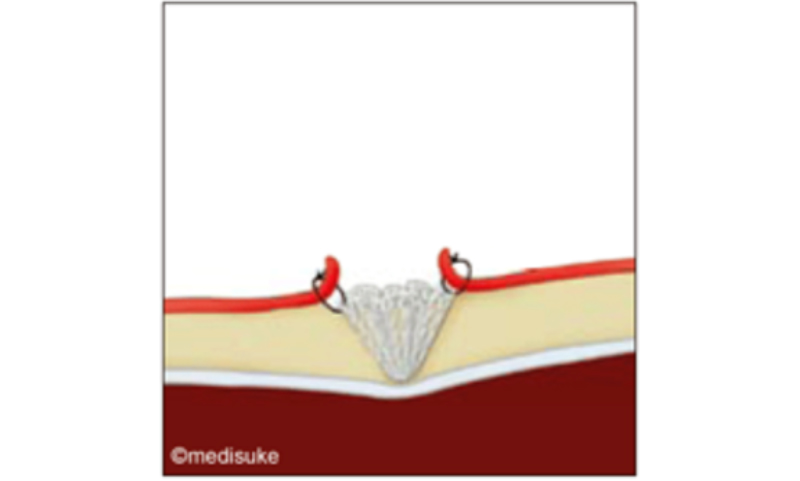
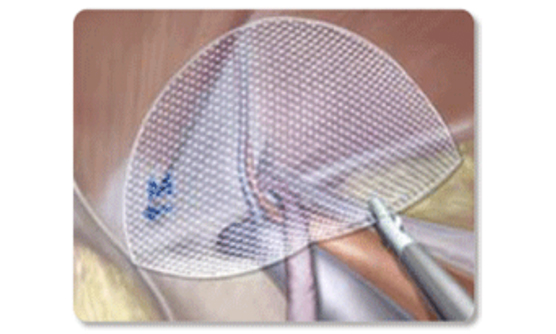
手術では、人工補強材(メッシュ)を用いて、ヘルニアの穴をふさぎ、弱くなったおなかの壁を補強します。細かい手術の方法は様々ですが、当院ではだいたい二通りの方法で手術を行っています。鼠径部を切開する方法か、腹腔鏡を用いた方法のいずれかを選択して行います。鼠径部切開法と腹腔鏡手術、どちらの方法で手術を行うかは、患者さんのお体の状態により判断しています。
鼠径部切開法では、通常、腰椎麻酔(半身麻酔)で手術を行います。場合により、全身麻酔あるいは局所麻酔で行うこともあります。鼠径部を5 cmほど切開し(おなかの厚みによって変わります)、脂肪や筋肉を分けてヘルニアの袋と穴を露出したのち、ヘルニアの袋を処理してメッシュでヘルニアの穴をおおってふさぎます(メッシュ・プラグ法、リヒテンシュタイン法、クーゲル法など)。
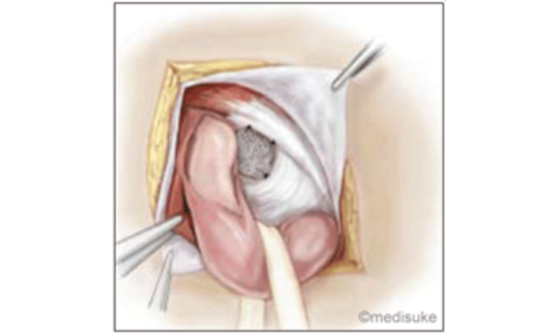
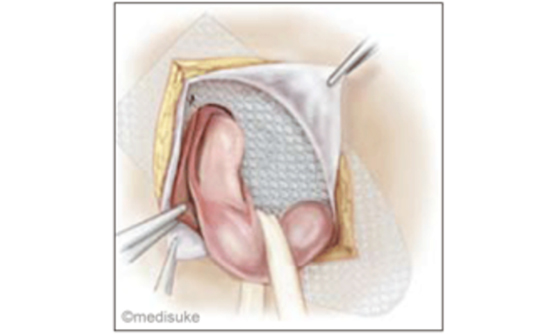
腹腔鏡手術では、全身麻酔で手術を行います。おへそと両脇の3か所に1㎝ほどの穴をあけて、そこにポートと呼ばれる筒を通し、炭酸ガスを注入しておなかをふくらませます。カメラを入れておなかの中からヘルニアの穴を観察し、ヘルニア周囲の腹膜をはがしてから、ヘルニアの穴をおおうようにメッシュを広げて溶けるピンで固定し、最後にはがした腹膜をかぶせて縫合します。
手術時間は、鼠径部切開法で1時間~1時間半、腹腔鏡手術で1時間半~2時間ぐらいです。これに麻酔のための時間が加わります。ヘルニアが大きい方、長年の間ヘルニアを持っていた方、肥満の方、再発ヘルニアの方、左右両側にヘルニアがある方などは、これより時間がかかります。
入院期間と術後の経過について
鼠径ヘルニアの手術の場合、手術当日の朝に手術室まで直接お越しいただき、担当医の手術前診察ののち手術室にお入りいただきます。手術終了後はそのまま病棟への入院となります。
手術後にもし傷の痛みがある場合は痛み止めの飲み薬を用意していますので、我慢せずに使用してください。時間がたてば、痛みは次第に良くなります。もともと膨らんでいたヘルニアの部分がしばらく腫れることがありますが、時間が経てばだんだん腫れはひいていきます。
順調に経過すれば、手術翌日には退院可能です(1泊2日入院)。退院後、診察のために、一度外来受診していただきます(1~2週間後)。傷口は溶ける糸で縫っていますので、抜糸の必要はありません。
退院後2~3週間ほどは、激しいスポーツや重い荷物を持つなどおなかに強い力がかかるような動作は控えてください。手術時のヘルニアの状態にもよりますが、1~2か月ほどすれば、普通の生活に戻っていただけます。
4)手術の合併症
合併症とは、手術によって起こりうるトラブルのことです。合併症が起きないように常に注意して手術を行っていますが、残念ながら合併症をゼロにすることはできません。どのような手術でも少ないながら一定の確率で合併症が起こりえることをどうかご理解ください。鼠径ヘルニアの手術で起こりうる合併症の主なものを以下にあげます。
①術後出血
出血していないことをしっかり確認して手術を終了しますが、ときに術後に出血したり、創部に血腫ができたりすることがあります。まれに輸血や止血のための再手術が必要となることがあります。
②感染
手術した傷口が感染して化膿することがあります。この場合、傷を開いて膿を出し、洗浄が必要になることがあります。また、もしメッシュに感染を起こすと、再手術をしてメッシュを取り除かないと感染がおさまらないことがあります。
③水がたまる
手術のあと、もともとのヘルニアの空間に水がたまり、あたかもヘルニアのように膨らむことがあります。漿液種(しょうえきしゅ)と言いますが、ほとんどの場合、時間が経てばだんだん吸収されてなくなっていきます。なかなかなくならない場合には、針を刺して水を抜く処置をすることもあります。
④術後の痛み
手術してしばらくは傷の痛みがありますが、時間が経てばだんだん和らいでいきます。少ないながら、慢性的な痛みやしびれが残ることがあります。
⑤ヘルニアの再発
メッシュで補強したところと別のところからヘルニアが起きて、以前と似たような鼠径ヘルニアの状態が起きることがあります。報告により多少異なりますが、数%程度に再発が起こると言われています。治療としてはやはり手術が必要になります。また、手術した側と反対側にヘルニアが出てくることもあります。
⑥アレルギー
人によっては、手術中に使用する抗生物質や麻酔薬などでアレルギーが出ることがあります。特定の薬剤にアレルギーがあることがわかっている場合には、事前に担当医にご相談ください。
⑦その他
麻酔の合併症、静脈血栓塞栓症、心臓や肺の合併症など他にも起こりうる合併症はありおますが、このような合併症が発生した場合には、最善と思われる処置を迅速に講じます。
(注)図は、株式会社メディコンの了解を得て、同社ホームページ・患者様向け説明文書などから抜粋して掲載させていただきました。

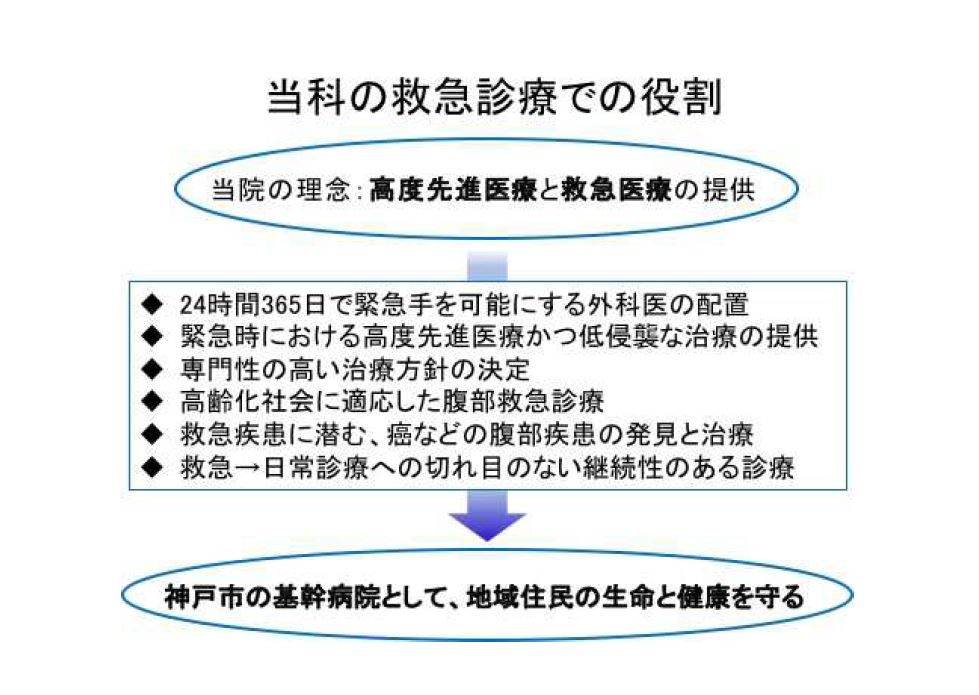
1)当科での救急診療の体制について
当院は「高度先進医療と救急医療の提供」の理念を掲げ、様々な年齢・疾患の患者さんを日々診療しながら、同時に可能な限り多くの救急患者さんを受け入れ、市民の皆様が常に安心できる医療の提供を目指してきました。当科は、この理念に従って先の項目に掲げた各臓器疾患に対する高度先進医療のみならず、救急医療の充実にも注力しています。
当院救急部では年間約36000人に及ぶ患者さんの受け入れを行っておりますが、その中には急性の腹部疾患の患者さんが多く含まれており、その症状や病態の程度によって専門的な診療や緊急手術・準緊急手術(症状が安定した後に早期に行う手術)が必要となります。この様な場合に備えて、当科では常勤外科医を当直及び待機当直として最低2名以上を常に配置し、24時間365日、可能な限り迅速に緊急手術ができる体制をとっています。
当科では年間平均1300〜1400件の手術を行っていますが、その約30%(300〜400件)を緊急手術が占めています。また、コロナ対策による手術制限がなされる環境においても緊急手術の割合は変わらず、当科の責務を果たすべく努力を続けています。そして、緊急手術においても患者さんの負担がなるべく少なくなることを目指し、腹腔鏡手術などの低侵襲で高度な先進医療を積極的に行っています。
2)高齢化社会における腹部救急診療に対する当科の役割
現在、我が国は他に類を見ない高齢化社会を迎えている国の一つです。このため、救急部を受診される患者さんのうち高齢者の割合が年々増加しています。一般に、高齢者の特徴として、1)基礎疾患(持病)が多く疾患も多岐に渡るため病態が単純でない(複雑化している)、2)症状が漫然として分かりにくい、3)意識障害や心不全の症状が併存しやすい、などが挙げられ、救急部を受診される高齢患者さんにもこれらの点が当てはまります。さらに、先に掲げた理念のもと長年に渡り救急医療に注力してきた当院の性質上、3)に相当する心不全や脳卒中など、様々な急性疾患を抱えているかかりつけの患者さんが多いことも当院の特徴の一つとなっています。
従って、腹部の急性疾患で受診される患者さんの中には、意識障害や心(循環)不全が潜んでいる場合や、逆に、実際には様々な病態が複雑に絡まったことによる全身状態の低下が引き金となり腹部の急性疾患を来しているケース、などが少なからず存在します。また、このような患者さんの診療にあたる中で、“がん”が初めて見つかる場合もあります。 このように複雑化した病態に対する救急診療では「病状の本質的原因は何か?」「どの治療から優先するのか?」、など専門性の高い診療・判断が迅速に求められます。当科は、救急部や各科の専門医と協力しながら、このような患者さんに対しても迅速かつ適切な救命治療を提供できるように努力しています。また、全身状態が低下した高齢患者さんの救命率を上げるために、緊急手術を行う場合であってもできるだけ患者さんの身体的負担が少ない腹腔鏡手術などを取り入れ、日常診療で行なっている高度先進医療かつ低侵襲な治療を行っています。
3)腹部の主な救急疾患について
緊急手術が必要となる腹部の救急疾患の例として下記があります。
急性胆のう炎(きゅうせいたんのうえん)
胆石などが原因で胆のうに急激に強い炎症が起きる疾患です。炎症が強い場合には、胆のうが壊死や穿孔(腐ってしまったり破れてしまう事)に至ることで全身に細菌が広がってしまい、時には生命に係わる危険性があります。症状は、発熱やみぞおちの痛みであったり、だるさや食欲低下を訴える方もおられます。
抗生物質で治療を行ったり、皮膚から胆のうの中に管を入れて膿を体外へ出す処置を行います。緊急手術が必要と判断される場合は、可能と判断すれば腹腔鏡手術を行っており、2019年/2020年の腹腔鏡手術の施行率は89%でした。
急性虫垂炎(きゅうせいちゅうすいえん)
一般の方が俗に“モーチョー炎”と呼ぶ疾患です。医学的には、盲腸に付着している虫垂という細い尻尾のような部分が炎症を起こす病態を指します。虫垂の中に膿がたまったり、ひどい時には破れてお腹全体に膿が広がり腹部全体の腹膜炎に至ることもあります。初期症状はみぞおちやお臍辺りの痛みで胃腸炎と診断される場合もありますが、病状が進むと発熱や右下腹の痛みなどがみられます。
炎症の程度が軽い場合には抗生物質で治すことも可能ですが、その後も繰り返すケースがあります。虫垂炎を繰り返すと手術が難しくなるケースもあり、受診された時点で緊急手術を行った方が安全で確実に治療可能と考えられる場合には手術をお勧めしています。手術は基本的に開腹ではなく腹腔鏡手術を行っており、近年2016-2020年ではほぼ100%で腹腔鏡手術で行っております。
*最近では、術後の合併症を減らすことを目的として、重度の虫垂炎の場合であっても抗生物質や膿を体外に出す治療などで炎症を沈静化させて緊急手術を回避し、日を改めて腹腔鏡での手術を行う治療も行なっています。
腸閉塞(ちょうへいそく)
腸が詰まって閉塞してしまう疾患です。症状はおなかの張りや腹痛、吐気や嘔吐などです。多くの場合、腹部手術後に傷が治る過程において、“癒着”といって腸と手術の傷が、あるいは、腸同士がべったりとくっつく現象が起きるために、偶然に腸がねじれたり折れ曲がったりすることが原因となります。初期の段階であれば、絶食と点滴で治療を始めます。時には鼻から管を入れて腸の中の食べ物や消化液を外へ出すことで治療します。
上記の治療で改善しない場合や、ねじれが強いために血の巡りが悪くなり腸自体が腐ってしまうような場合には、緊急で手術を行います。近年では、可能と判断すればこのような病態に対しても腹腔鏡手術を取り入れています。
*大腸がんが原因で腸閉塞が起きることもあり、消化器内科と合同で治療を行うこともあります。
消化管穿孔(しょうかかんせんこう)
胃や腸に穴があいて、食べ物や便などがおなかに広がり腹膜炎という状態になる疾患です。かなり激しい腹痛を伴い、時には循環不全(ショック)状態に陥ることもあります。ほとんどが緊急手術を要しますが、穴が開いている部位によって治療法や経過が大きく異なります。
胃や十二指腸で潰瘍が原因となって穴があいた場合は、手術をせずに治療したり、手術で破れた部分を縫い合わせるだけで改善が見込めるような比較的軽い病態が多くなります。
一方、大腸が破れた場合は、便による腹膜炎から全身に細菌が広がる菌血症(きんけつしょう)や、それが原因で全身が弱くなる敗血症(はいけつしょう)に陥りやすくなります。このため、緊急手術で人工肛門をつくったり、全身状態悪化が長引いて集中治療室での治療を要したり、最悪の場合は残念ながら救命出来ない場合もありえます。
*癌が原因で腸に穴があくことが起きることもあります。
外傷による腹腔内臓器損傷(ふくくうないぞうきそんしょう)
当院では事故による外傷の患者さんも救急車で運び込まれてきます。特に重症の方は、救急部を中心として様々な診療科が協力して治療にあたります。治療に関しては、手術だけでなく血管のなかにカテーテルという管を入れて血管を詰めて出血を止めたりする治療(放射線科医師による)を組み合わせたりしながら、救命に全力を尽くしています。
その他の疾患
上記以外にも、鼠径ヘルニア嵌頓(かんとん、詳しくは鼠径ヘルニアの説明をご参照ください)、大腸憩室炎など、様々な腹部の救急疾患があります。疾患だけでなく、患者さんの年齢や全身の状態も異なりますので、患者さんごとに、疾患とそれに対する適切と思われる治療法、起こりうる合併症などをしっかりと説明しご理解して頂いた上で、オーダーメイドの治療を行っていくように心がけています。
外科におけるロボット支援(ダヴィンチ)手術に関して
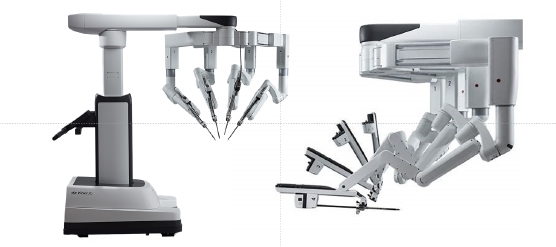
外科におけるロボット支援(ダヴィンチ)手術
当院では、胃癌に関しては2018年6月から、食道癌と直腸癌に関しては2018年10月からいち早く保険診療として施行しております。最近では通常の大腸癌や膵臓癌、肝臓癌に対しても導入しており、適応疾患や症例は年々増加傾向にあります。
現在当科では、2023年5月時点で内視鏡外科学会が認定するロボット支援手術プロクターが5名在籍(臓器別で食道1名、胃1名、直腸2名、膵臓1名)しています。これはロボット支援内視鏡手術の術者として標準的な技量を取得し、他者によるロボット支援手術を円滑且つ安全に指導できる指導者(プロクター)を認定するものであり、数多くの経験と技量が必要な資格となります。
我々は、癌の根治を目指すだけでなく、術後のより良い生活を患者様に提供できる様に、出来るだけ胃を残し胃全摘回避するための噴門側胃切除や、排尿神経温存、肛門機能温存を意識した直腸手術など、ロボット手術の特性を生かすべく術後QOL(quality of life)を重視した手術も積極的に行っています。
それぞれの臓器や疾患についてダヴィンチ手術に関連したご質問等ございましたら、気軽に外科外来までご相談ください。臓器毎にプロクターをはじめとした専門医がいますので適宜対応させていただきます。
2023年5月時点で既に350人近くの患者様が外科でダヴィンチ手術を受けられています。
令和5年5月現在
胃癌
約130例
直腸癌
約120例
経腸癌
約 10例
食道癌
約 80例
膵臓癌
約 15例
当院特有の鼠径ヘルニア治療について
鼠径ヘルニア術後疼痛に対する当院での治療について
鼠径ヘルニア術後慢性疼痛とは?
近年、鼠径部ヘルニア手術の術後合併症の一つとして、「鼠径(そけい)ヘルニア術後(じゅつご)慢性(まんせい)疼痛(とうつう)(CPIP)」が知られるようになってきました。
一般的に、鼠径ヘルニア手術後の痛みは手術後1~2週間以内をピークに、徐々に改善していきます。中には1~2週間を過ぎても痛みが続く場合もありますが、ほとんどが鎮痛薬を内服することにより痛みをコントロールすることができ、時間の経過とともに痛みは軽減し、最終的には消失します。ところが、鼠径ヘルニアの手術後3ヶ月たっても痛みが治まらない場合があり、痛みにより日常生活に支障を来す場合があります。このような状態を「鼠径ヘルニア術後慢性疼痛(CPIP)」と診断します。鼠径ヘルニア手術前には見られなかった太ももや睾丸(こうがん)の痛み、また性交時の痛みもCPIPの一つとして考えられています
鼠径ヘルニア術後慢性疼痛の頻度
CPIPは2000年頃から欧米を中心に報告されてきた疾患であり、以降たくさんの研究報告がなされています。痛みの程度によりその頻度は様々ですが、2018年にスウェーデンから発表された報告では、鼠径ヘルニア手術を受けた2万2917人の患者さんを対象にアンケート調査を行った結果、前方切開法術後の15%、腹腔鏡手術後の18%の患者さんで、術後1年たっても日常生活に支障を来す痛みがありました(Br J Surg 2018; 105: 106–112)。また、同じく2018年に報告されたドイツ・オーストリア・スイスの577施設による研究では、腹腔鏡下ヘルニア根治術を施行した2万4人の患者さんのうち、9.5%にあたる1900人で術1年後の運動時痛がありました。また、治療が必要になった患者さんは520人と、全体の2.6%を占めていました(Surg Endosc. 2018;32:1971-1983)。一度CPIPに陥ると、患者さんは痛みによる精神的ストレスのため消耗(しょうもう)し、日常生活が立ちゆかなくなります。このような背景から、海外でCPIPは鼠径ヘルニア手術の最も忌むべき術後合併症として、医療者はもちろんのこと手術を受ける患者さんにも広く認識されている疾患です。
一方、日本では海外と比べてその発症頻度は低いと報告されていますが、具体的な頻度に関しては現在調査中です。いずれにせよ、本邦では医療者にとってもまだまだなじみの薄い疾患です。
鼠径ヘルニア術後慢性疼痛の原因とその種類
現在、鼠径ヘルニア手術の標準術式はメッシュを使った根治術が一般的であることから、CPIPに陥った患者さんのほとんどがメッシュ使った手術後の患者さんです。その一方で、メッシュを入れずに手術をうけられてCPIPが発症された方もおられます。また、腹腔鏡手術は術後疼痛が少なくCPIP発症率が低い、と報告されていますが、上述のごとく腹腔鏡下手術術後にCPIPを発症する患者さんもいらっしゃいます。つまり、CPIPはどのような術式でも起こりうる術後合併症であることを認識しておく必要があります。
CPIPの痛みの種類には3種類あります。①神経障害性疼痛、②体性痛、③睾丸痛です。
①神経障害性疼痛
鼠径部には3本、骨盤腔(こつばんくう)には2本の痛みを感知する知覚神経が走行しています。手術後の創傷治癒により組織が堅くなっていくことを瘢痕化(はんこんか)といいますが、瘢痕化の過程でこれら神経をまきこんでしまうことにより発症する痛みを神経障害性疼痛といいます。また、ヘルニア手術で使用されているメッシュは時間の経過とともに縮んでいくことも知られています。縮んだメッシュに神経が引き込まれ、神経の圧迫や引きつれが起こる場合にも、この神経障害性疼痛が起こります。薬や注射の治療でも効果が見られないCPIPの多くがこの神経障害性疼痛です。
②体性痛
一方、挿入されたメッシュが周囲の組織、特に筋肉を巻き込んで縮むことにより、鼠径部や骨盤の柔軟な動きを邪魔することにより違和感や痛みを起こす場合や、骨盤内でメッシュがよれたりねじれたりすることにより堅い団子のようになり、違和感や痛みを起こす場合もあります。このような痛みを体性痛といいます。日常生活上問題になる痛みにまで発展する患者さんは多くはありませんが、いったんCPIPになってしまうと、外来での治療は困難となります。
③睾丸痛
メッシュを留置する場所は精子が運搬される輸精管のすぐ隣になります。輸精管とメッシュが固着することにより、輸精管と並んで走行している神経をメッシュが圧迫したり引きつれを起こしたりすることにより睾丸痛が起こります。輸精管自体にメッシュがめり込んで浸食することにより睾丸痛を来すこともあります。これらの場合も外来での治療は非常に困難です。
鼠径ヘルニア術後慢性疼痛の診断と治療、その成績
「痛み」は第三者がみて分かるものではなく、血液検査やレントゲンで評価できるものでもありません。そのため、病状に関して周りから理解されないことも多く、悩まれる患者さんがたくさんおられます。痛みを理解されず、適切な治療を受けられないことにより、精神的ストレスが累積し、うつ病を発症する方もいらっしゃいます。CPIPに対して有効な治療を行うためには、何が原因で痛みがおこっているかということを正確に知ることが最も重要であり、先述した「痛みの種類」を診断することが重要です。
CPIPの治療方法に確立したものはなく、国内外を問わずガイドラインでも治療に関する具体的な記載はありません。そのため、CPIPの治療は困難を極めます。
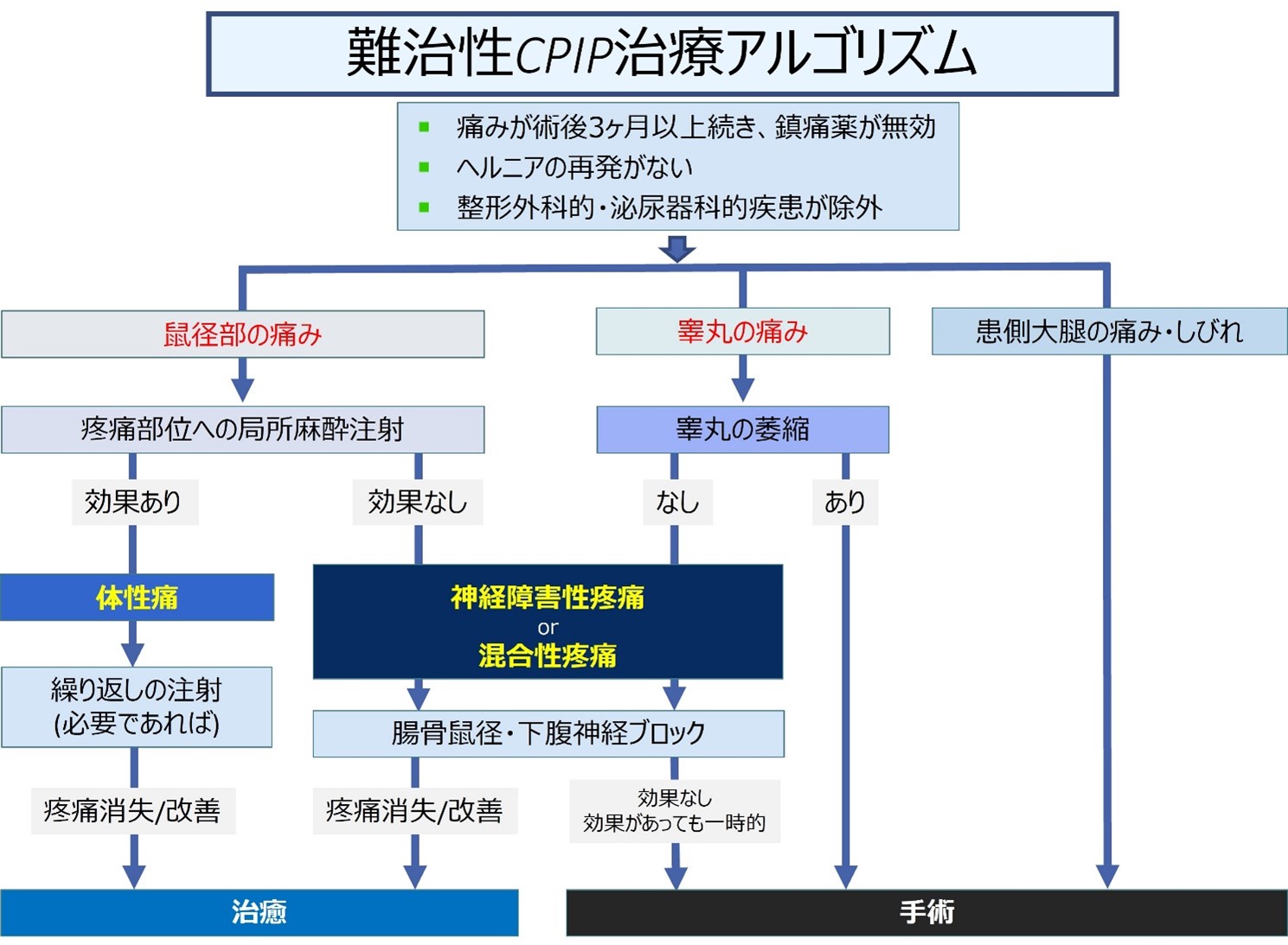
当院では「鼠径ヘルニア術後慢性疼痛」の患者さんに対して積極的に治療を行っています。段階的な診察および治療から痛みの種類・程度を診断する必要があるため、何度も病院に足を運んでいただく必要があります。当科で作成した鼠径ヘルニア術後慢性疼痛の治療アルゴリズムをご参照ください。
2023年10月現在までに鼠径ヘルニア術後慢性疼痛と診断された83人の患者さんに対してこのアルゴリズムに従って治療を行いました。手術を行わずに治療できた患者さんが29人であるのに対して、手術が必要となった患者さんは54人でした。つまり、難治性CPIPに対しては、アルゴリズムを用いた治療により疼痛を緩和させることができる一方で、手術が必要になる患者さんが数多く存在することも事実です。
CPIPに対する手術加療は一般的な手術と異なり、確立していません。そのため、患者さんの症状や前回に受けた手術内容、メッシュの留置部位などを加味して十分に術式を検討した上で行います。
一般的に手術は一定のリスクを伴うものであり、時には出血・心筋梗塞・脳梗塞・肺塞栓などの致死的な合併症を起こす場合もあります。それに加えてCPIPの手術は、メッシュを摘出し、神経障害性疼痛の場合は原因となっている神経を同定・摘出する必要があるため、非常に難易度の高い手術となります。さらにCPIPの手術に関しては、「手術の結果生じるリスク」も考慮すべきです。具体的には、「手術をしても思ったように痛みが取れない可能性」「手術前にはなかった痛みが新たに出てくる可能性」「鼠径ヘルニアが再発する可能性」などがあげられます。そのため、安易な手術の実施はしていません。十分に適応を検討し、患者さんおよびご家族と時間をかけて相談した結果、行うようにしています。
手術を受けられた患者さんにアンケート調査を行った結果、90%以上の患者さんが手術に対して「非常にもしくは概ね満足した」とお答えいただきましたが、逆に言うと100%の患者さんが満足しているわけではありません。そのためわれわれは、「手術をすれば必ずしも痛みがとれる」というわけではないことを十分にご理解いただいたうえで手術を行っています。
鼠径ヘルニア術後3-6ヶ月後にも痛みが続く方は是非ご相談ください。
本症状に関しては、毎週木曜午後の「ヘルニア外来」に問い合わせ・ご紹介いただくようお願いします。
鼠径ヘルニア手術(脱腸に対する手術)では、ポリプロピレンもしくはポリエステル製の人工補強材(メッシュと呼ばれます)を使う手術が一般的に行われており、ガイドラインでもメッシュの使用が推奨されています。メッシュがない1990~2000年以前は、自分自身の組織を縫い合わすことによりヘルニアを治していましたが、再発率が10~35%と高いため、人工補強材であるメッシュの使用が推奨されるようになった、という歴史的な背景があります。
しかし、ヘルニアという良性疾患に対して永久になくなることない異物であるメッシュを体に入れることが本当にいいことなのでしょうか?
近年、アメリカ・カナダ・ヨーロッパを中心とした海外では、メッシュを使用したヘルニア手術後の鼠径部の痛み(慢性疼痛といいます)・性交時の痛みが、メディアおよびソーシャルネットワーク上で大きくとりあげられています。専門科による詳細な分析では、メッシュをいれた場合といれない場合での慢性疼痛が起こる割合に変わりはない、と言われていますが、異物を入れることにより体内の組織(特に神経・輸精管)に悪影響を及ぼす、という報告も散見しています。2018年に発表された報告ですが、スウェーデンで鼠径ヘルニア手術を受けた2万2917人の患者さんを対象にアンケート調査を行った結果、メッシュを使った前方切開法術後の15%、腹腔鏡手術後の18%の患者さんが、術後1年たっても日常生活に支障を来す痛みがある、という回答をしています(Br J Surg 2018; 105: 106–112)。このような背景から、イギリスの国営放送であるBBCニュースでは、3度にわたってヘルニアメッシュの合併症、特に慢性疼痛に対する特集を行うなど(https://www.bbc.co.uk/search?q=Hernia+mesh&seqId=df20bf20-56a2-11ee-a0ab-558b52201976&d=SEARCH_PS)、海外ではメッシュを使用しない手術が徐々に見直されてきていることも事実です。
当院でもこれまでにメッシュをつかったヘルニア手術の後に慢性疼痛を発症し、苦しまれた患者さんを数多く診療してきました。中には、薬や注射による治療が効果なく、手術によりメッシュを摘出する必要になった患者さんも数多くいらっしゃいます。
メッシュが実際に使用されてから約20年たちますが、挿入されたメッシュが長い年月を経て人体にどのような影響を及ぼすのか、誰にもわかりません。メッシュを構成する原材料に関しても不明です。年月とともにメッシュが体内臓器(輸精管・膀胱・腸管)に侵食していく、という報告もあります (Ann Surg. 2018;267:569-575.)。当院で慢性疼痛に対して手術をうけた患者さんの中には、メッシュを入れて10年以上経った後に痛みがあり、メッシュを摘出した患者さんも多数いらっしゃいます。
当院でもガイドラインに則って、メッシュを使用した鼠径ヘルニア手術を行っていますが、メッシュをいれない手術(組織(そしき)修復法(しゅうふくほう)といいます)も行っており、患者さん本人に選んでいただけます。組織修復法にはいろいろな方法がありますが、当院で採用しているのはShouldice(ショールダイス)法という方法で、術後再発・慢性疼痛の起こる頻度が少なく、組織修復法の中で最も優れている術式です。Shouldice法の術後再発率は、発祥の地であるShouldice clinicからの報告では1.15%で、原法通りに手術を行えばメッシュを用いた手術と同等、もしくははるかに上回る成績を収めることができます。当院ではそけいヘルニア手術をうけられる患者さんに対してクリティカル・パスを全例で導入しており、メッシュを使わない手術の入院日数は2泊3日となりますが、運動制限などは腹腔鏡手術・メッシュを使った手術と全く同じです。
当院外科医師の成田は、Shouldice法発祥の地であるカナダのオンタリオ州にあるShouldice Hospitalに手術見学に行き、3日間にわたり、15件の手術に参加し、Staff surgeonに直接手術手技を細かく指導してもらいました。それ以降、Shouldice法による組織修復法を患者さん本人と相談の上、慎重に行っています。Shouldice法を用いた組織修復法はすでに保険診療で認められている手術であるため、実際に行うことに何ら問題はありません。なお、前立腺がんに対する根治手術を受けた後の患者さんや、大腿ヘルニアの患者さんはこの手術を受けることができません。そけいヘルニアの再発に対する手術の場合も適応から外れることがあります。

もし、鼠径ヘルニア手術を受ける方で、「メッシュなし」の手術を希望される方は当院外科外来にご連絡ください。
本症状に関しては、毎週木曜午後の「ヘルニア外来」に問い合わせ・ご紹介いただくようお願いします。
臨床研究
当科では臨床上の様々な疑問点を解決すべく臨床研究を行っています。観察研究とは直接の同意は頂かずこの啓示を持って同意して頂いたものとして実施されています。また院内の臨床研究倫理委員会にて審査・認可された介入研究や観察研究ではその対象となる患者さん個人に説明し同意を頂いた上で実施しています。
また我々の教室ではこれらで得られた知見を積極的に国内外の学会発表や論文で報告しています。
主な臨床研究(観察、介入研究を含む)
| 研究課題名 | 当院責任者 | 説明文 (PDF) |
| 高齢者に対する低侵襲胃癌手術 胃全摘回避の手技と工夫(胃癌に対する機能温存手術) | 近藤正人 | |
|---|---|---|
| 保存オルガノイドを用いた横断的ながんの診断・治療に関する研究 | 大嶋野歩 | |
| 食道胃接合部癌の適切な口側切離に関する国際共同研究 | 近藤正人 | |
| 進行横行結腸がんに対する結腸部分切除術の有用性に関するランダム化第Ⅲ相試験 | 大嶋野歩 | |
| 80歳以上の高齢鼠径ヘルニア患者に対する至適手術治療の検討 | 成田匡大 | |
| 京都大学外科関連多施設における胃癌手術レジストリ | 近藤正人 | |
| 胃癌に対するロボット支援手術と腹腔鏡下手術の中長期成績に関する多機関共同後ろ向きコホート研究 | 近藤正人 | |
| 閉塞性大腸癌に対するステント留置後の術前化学療法の安全性と有効性に関する多機関共同試験(SUCCEED study) | 大嶋野歩 | |
| 大腸癌根治術後の異時性再発巣切除を施行した症例における再々発形式の考察 | 大嶋野歩 | |
| 外科的切除を施行した大腸癌腹膜播種における周術期化学療法の有効性の検討 | 大嶋野歩 | |
| 胃癌根治術後の栄養状態の変化と予後に関する多機関共同研究 | 近藤正人 | |
| 閉鎖孔ヘルニアの病態及び治療法と予後についての全国調査研究 | 成田匡大 | |
| 当院における胆嚢癌・胆嚢癌疑診例における術前診断の精度と問題点 | 鳥口寛 | |
| 偶発胆嚢癌に対する多機関共同後ろ向きコホート研究 | 成田匡大 | |
| 胃癌c onversion surgery における低侵襲手術の意義 | 松田正太郎 | |
| 切除不能局所進行膵癌に対するConversion Surgery の新規化学療法導入後治療成績の再検討 | 鳥口寛 | |
| 当院におけるロボット支援下尾側膵切除:導入から現在までの工夫と変遷 | 鳥口寛 | |
| 当院における80歳以上の高齢者に対する肝細胞癌の外科治療の現状と問題点 | 鳥口寛 | |
| 腹腔鏡下肝切除時のグリソン鞘一括処理におけるsurgical staple line reinforcementの使用経験 | 鳥口寛 | |
| 京都大学外科関連施設における大腸癌手術治療成績の検討 | 橋田裕毅 | |
| 当院における切除可能大腸癌肝転移に対する治療成績の現状と課題 | 鳥口寛 | |
| 細胆管細胞癌の臨床病理学的特徴とその臨床的意義 | 北村好史 | |
| 当院における高難度の腹腔鏡下肝切除術は患者に対して有益か | 鳥口寛 | |
| 市中病院におけるロボット支援下結腸切除術の導入と短期成績 | 橋田裕毅 | |
| 若手外科医に対する施設横断型腹腔鏡下鼠径ヘルニア根治術指導の有用性の検証 | 小山達也 | |
| 当院における虫垂の悪性腫瘍性病変の検討 | 松田正太郎 | |
| 直腸DST 吻合における縫合不全ゼロを目指した試み | 橋田裕毅 | |
| 大腸神経内分泌腫瘍に対する治療成績 | 橋田裕毅 | |
| TNM分類から見た虫垂悪性腫瘍性の検討 | 橋田裕毅 | |
| 地方市中病院でのロボット支援下直腸手術の導入と短期成績からみた術者教育 | 橋田裕毅 | |
| 当院における胆嚢癌に対する腹腔鏡下手術の現状と問題点 | 鳥口寛 | |
| 腹腔洗浄細胞診陽性膵癌に対し切除の是非を明らかにするための比較研究 | 北村好史 | |
| 当院における切除可能膵癌に対する術前化学療法の現状と成績について | 木原康樹 | |
| 直腸切除術のDST再建における体腔内補強縫合による縫合不全防止の取り組み | 橋田裕毅 | |
| 反回神経麻痺ゼロを目指したロボット支援下食道手術の工夫 | 小林裕之 | |
| 内視鏡外科手術の多施設データベース構築 | 橋田裕毅 | |
| Bismuth III・IV型 肝門部領域胆管癌手術における根治性と安全性を担保した術前評価 | 北村好史 | |
| ロボット支援下手術は食道癌の術後合併症を減らしたか | 小林裕之 | |
| 当院の腹腔鏡下結腸切除術における体腔内吻合の成績 | 金田優也 | |
| 再発低リスク大腸癌に対するレスインテンシブサーベイランスの単群検証的試験 | 橋田裕毅 | |
| 単一施設における直腸癌に対するTNTの臨床成績 | 橋田裕毅 | |
| 高齢者胃癌に対する術式選択や周術期管理の工夫 | 近藤正人 | |
| 高齢者における大腸癌術後補助化学療法の有効性と忍容性 | 橋田裕毅 | |
| StageII 、III直腸癌に対する術後補助化学療法の進行度ステージ別の有効性に関する後ろ向き探索的な統合解析 | 橋田裕毅 | |
| 大腸癌術後補助化学療法における有害事象と予後の関連 | 橋田裕毅 | |
| 当院における食道癌に対する胸腔鏡下手術と縦隔鏡下手術の現状 | 小林裕之 | |
| 妊娠中の急性虫垂炎に対する腹腔鏡下虫垂切除術 | 橋田裕毅 | |
| 十二指腸乳頭部癌術後無再発生存期間を短縮させる臨床病理学的因子の解析:多機関共同後方視的コホート研究 | 北村好史 | |
| 高齢者における胃空腸バイパス術の成績に関する後ろ向き研究 | 貝原 聡 | |
| 内視鏡外科手術の多施設データベース構築 | 橋田裕毅 | |
| 肝臓移植後肝癌再発高危険群の全国実態調査 | 貝原 聡 | |
| 一般社団法人 National Clinical Database (NCD)における手術・治療情報データベース事業 | 貝原 聡 | |
| 黄色肉芽腫性胆嚢炎と胆嚢癌の鑑別としての術前因子の検討 | 貝原 聡 | |
| 一般市中病院におけるロボット胃切除術導入後の成績と経過 | 近藤正人 | |
| 直腸癌に対する腹腔鏡下直腸手術におけるDST吻合での補強縫合の有用性 Intracorporeal Reinforcing Sutures Reduce Anastomotic Leakage in Double-Stapling Anastomosis for Laparoscopic Rectal Surgery |
橋田裕毅 | |
| 腹腔鏡下直腸切除術のDST再建における補強縫合による縫合不全防止 | 橋田裕毅 | |
| GIST(Gastrointestinal Stromal Tumor)の悪性度、薬剤耐性に関 する多施設共同研究 |
近藤正人 | |
| 腹腔鏡下直腸切除における縫合不全対策としての補強縫合の有用性 | 橋田裕毅 | |
| ロボット支援下胃切除術導入の安全性に関する研究 | 近藤正人 | |
| 再発高リスク消化管間質腫瘍に対する完全切除後の治療に関する研究(STAR ReGISTry)の追跡調査 | 近藤正人 | |
| 腹膜播種に対するCRS/HIPECの意義に関する多施設共同研究 | 貝原 聡 | |
| 残胃癌に対する低侵襲手術の有用性、妥当性の検討 | 貝原 聡 | |
| RAS遺伝子変異の有無から見た適切な大腸癌肝転移切除術 | 岩城謙太郎 | |
| 直腸脱に対する腹腔鏡下直腸固定術(Wells 変法) | 橋田裕毅 | |
| 非機能性膵神経内分泌腫瘍に対する術式の再考 | 神部宏幸 | |
| グルカゴン静脈注射による延長胃管は食道癌術後縫合不全を減少させるか? | 河原林卓馬 | |
| 膵癌に対する術前EUSは腫瘍径評価に有用か | 喜多亮介 | |
| 食道癌再建時における術中グルカゴン投与の有用性 | 喜多亮介 | |
| 2型糖尿病患者に対する消化器悪性腫瘍手術において術前血糖コントロールが術後成績に及ぼす影響に関する多施設共同後ろ向き観察研究 | 近藤正人 | |
| 市中病院におけるロボット支援下直腸手術の導入と短期成績 | 橋田裕毅 | |
| 脾弯曲部結腸癌に対する内側アプローチを中心とした腹腔鏡下左側結腸切除術 | 橋田裕毅 | |
| 超高齢者大腸癌に対する腹腔鏡手術の有用性 | 橋田裕毅 | |
| 2型糖尿病を有する胃癌患者に対する幽門側胃切除術後の消化管再建法の糖尿病経過への影響に関する多施設共同後ろ向き観察研究 | 近藤正人 | |
| 超高齢者大腸癌に対する腹腔鏡下大腸手術の有用性 | 橋田裕毅 | |
| 京都大学外科関連多施設における胃癌手術レジストリ | 小林裕之 | |
| RAS遺伝子変異の大腸癌肝転移切除後肝局所再発への影響 | 岩城謙太郎 | |
| 京都大学外科関連施設における大腸癌手術治療成績の検討 | 橋田裕毅 | |
| 膵全摘後中長期成績の検討 | 岩城謙太郎 | |
| 直腸癌に対するロボット支援下手術の定型化 | 橋田裕毅 | |
| 内視鏡外科手術の多施設データベース構築 | 橋田裕毅 | |
| 抗血栓薬(抗血小板薬・抗凝固薬)服用患者における消化器外科手術の安全性の検証 | 瓜生原健嗣 | |
| ロボット支援下直腸切除術の導入と初期治療成績 | 橋田裕毅 | |
| 切除可能膵癌の範疇で術前補助療法を要しない症例とは? 手術先行施設における後ろ向き検討 | 北村好史 | |
| 絞扼性イレウスに対する腹腔鏡下手術の適応とその限界 | 神部宏幸 | |
| 十二指腸癌外科的切除症例の臨床病理学的因子と予後に関する研究(多施設共同観察研究) | 北村好史 | |
| 市中病院におけるロボット胃癌手術の導入と成績 | 近藤正人 | |
| 大腸癌切除可能肝限局転移例に対する術前XELOX+ベバシズマブ(BV)療法の第Ⅱ相臨床試験 | ||
| 胃切除後の異時性多発癌の実態に関するアンケート | ||
| 京都大学外科関連多施設における胃癌手術レジストリ | ||
| 腹腔鏡下胃全摘術における食道空腸吻合法に関する多施設共同後ろ向き観察研究 | ||
| GISTの悪性度、薬剤耐性に関する多施設共同研究 | ||
| 当院におけるロボット支援胃がん手術の成績E | ||
| 腹腔鏡下直腸切除における縫合不全対策としての補強縫合の有用性 | ||
| 肝硬変合併肝細胞癌に対する腹腔鏡手術の有効性 | ||
| 病態からみた直腸脱に対する腹腔鏡手術の有効性 | 橋田裕毅 | |
| 大腸癌肝転移に対する治療戦略(腫瘍内科と共同、観察研究) | ||
| 高度進行胃癌に対する術前化学療法の効果(腫瘍内科と共同、観察研究) | ||
| StageIB胃癌に対する腹腔鏡下手術(観察研究) | ||
| 人工肛門創管理プロトコールの有効性(観察研究) | ||
| 膵体尾部切除における断端処理(観察研究) | ||
| 胆嚢癌切除プロトコールと成績(観察研究) | ||
| 直腸側方廓清の適応(観察研究) | ||
| 進行直腸癌に対する術前化学療法(腫瘍内科と共同、観察研究) | ||
| 穿孔性虫垂炎に対する待機的虫垂切除の適応と成績(観察研究) | ||
| 胃癌術後の栄養状態評価(観察研究) | ||
| 腹腔鏡下肝切除術の安全性の検証(多施設共同観察研究) | ||
| 高齢胃がん患者における胃切除後の予後予測ノモグラムの開発(多施設共同観察研究) |
学会発表・論文実績
学会発表・論文実績
- 橋田裕毅,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本素子,北村好史, 近藤正人,瓜生原健嗣,小林裕之,貝原 聡:大腸神経内分泌腫瘍の治療成績.第 15 回日本消化管学会,佐賀, 2019.2.1-3
- 橋田裕毅:傍ストーマヘルニア治療における腹腔鏡手術.第 36 回日本ストーマ排泄リハビリテーション学会, 大阪,2019.2.22-23
- 水本素子,占野尚人,貝原聡:当院における噴門部粘膜下腫瘍に対する腹腔鏡内視鏡合同手術.第 91 回日 本胃癌学会,沼津,2019.2.27-3.1
- 小林裕之,近藤正人,喜多亮介,増井秀行,橋田裕毅,松原孝明,塩川桂一,岩城謙太郎,神部宏幸,水野 良祐,水本素子,瓜生原健嗣,北村好司,貝原 聡:市中病院におけるロボット支援下食道手術の導入.第 119 回日本外科学会,大阪,2019.4.18-20
- 橋田裕毅,水野良祐,神部宏幸,岩城謙太郎,塩川桂一,水本素子,北村好史,近藤正人,小林裕之,瓜生 原健嗣,細谷亮,貝原聡:腹腔鏡下直腸切除術の DST 再建における補強縫合による縫合不全防止.第 119 回日本外科学会,大阪,2019.4.18-20
- 神部宏幸,北村好史,岩城謙太郎,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本素子,近藤 正人,橋田裕毅,小林裕之,瓜生原健嗣,貝原聡:膵頭十二指腸切除症例における術前胆道ドレナージの効 果と術後合併症への影響.第 119 回日本外科学会,大阪,2019.4.18-20
- 岩城謙太郎,貝原 聡,神部宏幸,水野良祐,塩川桂一,水本素子,北村好史,近藤正人,橋田裕毅,小林裕之, 瓜生原健嗣:肝硬変合併肝細胞癌に対する腹腔鏡手術の有効性.第 119 回日本外科学会,大阪,2019.4.18-20
- 北村好史,貝原 聡,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本 素子,北村好史,近藤正人,瓜生原健嗣,小林裕之,橋田裕毅,細谷 亮:肝門部領域癌における胆道造影 下 CT fusion 画像による定型化した simulation と成績.第 119 回日本外科学会,大阪,2019.4.18-20
- 塩川桂一,瓜生原健嗣,岩城謙太郎,水野良祐,神部宏幸,松原孝明,喜多亮介,増井秀行,水本素子,近 藤正人,橋田裕毅,小林裕之,貝原 聡,細谷 亮:当院における下部消化管穿孔奨励の治療成績と予後予 測因子の検討.第 119 回日本外科学会,大阪,2019.4.18-20
- 岩城謙太郎,貝原 聡,北村好史:The impact of laparoscopic surgery for hepatocellular carcinoma with liver cirrhosis.ILLS 2019 Tokyo,東京,2019.5.9-11
- 神部宏幸,北村好史,塩川桂一,松原孝明,瓜生原健嗣:早期診断により腸管切除を免れた S 状結腸間膜窩ヘル ニアの一例.第 17 回日本ヘルニア学会,四日市,2019.5.24-25
- 小林裕之,近藤正人,喜多亮介,増井秀行,松原孝明,塩川桂一,岩城謙太郎,神部宏幸,水野良祐,貝原 聡: 当院でのロボット支援下食道手術の導入と課題.第 73 回日本食道学会,福岡,2019.6.6-7
- Masato Kondo, Satoshi Kaihara:Introduction and results as a safe operative procedure for robotic gastrectomy. EAES 2019, Sevilla, 2019.6.12-15
- Ryosuke Mizuno, Masato Kondo, Hiroyuki Kanbe, Kentaro .Iwaki, Keiishi Shiokawa, Takaaki Matsubara, Hideyuki Masui, Ryosuke Kita, Motoko Mizumoto, Koji Kitamura, Hiroki Hashida, Hiroyuki Kobayashi, Kenji Uryuhara, Satoshi Kaihara, Ryo Hosotani:Comparison of standard IPOM and IPOM plus in our hospital. EAES 2019, Sevilla, 2019.6.12-15
- 貝原 聡,北村好史、瓜生原健嗣、塩川桂一、橋田裕毅、岩城謙太郎:Central Sectionectomy for Hilar Cholangiocarcinoma; Application of the Hanging Method in Parenchymal Dissection.第 31 回肝胆膵外科学会,高松, 2019.6.13-15
- 岩城謙太郎,貝原 聡、増井秀行、北村好史、瓜生原健嗣:A novel preoperative remnant liver functional evaluation using 99mTcGSA-SPECT and KICG for safe hepatectomy.第 31 回肝胆膵外科学会,高松,2019.6.13-15
- 北村好史,貝原 聡、岩城謙太郎、瓜生原健嗣:Importance of regional lymph node dissection for pancreatobiliary subtype of ampullary carcinoma. Investigation of recurrent sites after curative resection.第 31 回肝胆膵外科学会,高松, 2019.6.13-15
- 貝原 聡,北村好史,瓜生原健嗣,岩城謙太郎,神部宏幸,水野良佑,塩川桂一,松原孝明,喜多亮介,増井秀明: 細管切除術における手術手技.第 74 回日本消化器外科学会,東京,2019.7.17-19
- 小林裕之,近藤正人,喜多亮介,増井秀行,松原孝明,塩川桂一,岩城謙太郎,神部宏幸,水野良祐,貝原 聡: 当院でのロボット支援下食道手術の導入と課題.第 74 回日本消化器外科学会,東京,2019.7.17-19
- Hiroyuki Kambe, Koji Kitamura, Ryosuke Mizuno, Kentaro Iwaki, Keiichi Shiokawa, Takaaki Matsubara, Hideyuki Masui, Ryosuke Kita, Motoko Mizumoto, Masato Kondo, Hiroyuki Kobayashi, Hiroki Hashida, Kenji Uryuhara, Satoshi Kaihara:Clinical investigation of resected primary duodenal carcinoma. 第 74 回 日 本 消 化 器 外 科 学 会, 東 京, 2019.7.17-19
- Motoko Mizumoto, Ryosuke Mizuno, Hiroyuki Kanbe, Kentaro Iwaki, Keiichi Shiokawa, Takaaki Matsubara, Hideyuki Masui, Ryosuke Kita, Satoshi Kaihara, Ryo Hosotani:Clinical experience of primary small bowel cancer in our hospital. 第 74 回日本消化器外科学会,東京,2019.7.17-19
- Ryosuke Mizuno, Masato Kondo, Takuma Kawarabayashi, Tokihiko Sumi, Hiroyuki Kanbe, Kentaro .Iwaki, Keiishi Shiokawa, Motoko Mizumoto, Koji Kitamura, Hiroki Hashida, Hiroyuki Kobayashi, Kenji Uryuhara, Satoshi Kaihara, Ryo Hosotani”:Emergency operation for diverticulitis from the view of pre-operative CT imaging.第 74 回日本消化器外科 学会,東京,2019.7.17-19
- 近藤正人,岩城謙太郎,水野良祐,神部宏幸,塩川桂一 ,水本素子,北村好史,小林裕之,橋田裕毅,貝原 聡: 一般市中病院におけるロボット消化管手術の導入と成績.第 74 回日本消化器外科学会,東京,2019.7.17-19
- 橋田裕毅,岩城謙太郎,神部宏幸,水野良祐,水本素子,北村好史,近藤正人,瓜生原健嗣,小林裕之,貝原 聡: 病態から見た直腸脱に対する腹腔鏡手術.第 74 回日本消化器外科学会,東京,2019.7.17-19
- 塩川桂一,瓜生原健嗣,岩城謙太郎,水野良祐,神部宏幸,松原孝明,喜多亮介,増井秀行,水本素子,近藤正人, 橋田裕毅,小林裕之,貝原 聡:T2 胆嚢癌に対する当院治療プロトコールの検討.第 74 回日本消化器外科学会,東京, 2019.7.17-19
- 岩城謙太郎,貝原 聡,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本素子,北村好史, 近藤正人,橋田裕毅,小林裕之,瓜生原健嗣:The replaced RHA preserving technique for the plexus of pancreatic head dissection.第 74 回日本消化器外科学会,東京,2019.7.17-19
- 北村好史,貝原 聡,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,瓜生原健嗣: Preoperative 3D-CT fusion image aim for R0 resection in hilar cholangiocarcinoma.第 74 回日本消化器外科学会,東京, 2019.7.17-19
- 瓜生原健嗣,貝原 聡:当院における高齢肝移植後患者フォローの現状と課題.第 55 回日本移植学会,広島, 2019.10.10-12
- 橋田裕毅,近藤正人,水本素子,小林裕之,貝原 聡:横行結腸癌に対する内側アプローチを中心とした腹 腔鏡手術の定型化.第 74 回日本大腸肛門病学会,東京,2019.10.11-12
- 橋田裕毅,水野良祐,神部宏幸,塩川桂一,水本素子,近藤正人,小林裕之,貝原 聡:超高齢者の大腸癌 に対する腹腔鏡手術の検討.第 57 回日本癌治療学会,福岡,2019.10.24-26
- Hiroyuki Kobayashi, Masato Kondo, Ryosuke Kita, Hideyuki Masui, Takaaki Matsubara, Keiichi Shiokawa, Kentaro Iwaki, Hiroyuki Kanbe, Ryosuke Mizuno, Satoshi Kaihara:Impact of Intravenous Injection of Glucagon on Anastomotic Leakage in Esophagectomy. ACS 2019, San Francisco, 2019.10.27-31
- Koji Kitamura, Satoshi Kaihara, Kentaro Iwaki, Hiroyuki Kanbe, Ryosuke Mizuno, Keiichi Shiokawa, Kenji Uryuhara, Hiroyuki Kobayashi:Usefulness of three-dimensional computed tomography simulation for safe laparoscopic liver anatomical resection. ACS 2019, San Francisco, 2019.10.27-31
- 近藤正人,小林裕之,河原林卓馬,鷲見季彦,神部宏幸,岩城謙太郎,水野良祐,塩川桂一,貝原 聡:よ り簡便で強固な吻合のために 組織補強材付きの自動縫合器を用いて.第 49 回胃外科術後障害研究会,鹿 児島,2019.10.31-11.1
- 河原林卓馬,北村好史,鷲見季彦,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,水本素子,近藤正人,橋 田裕毅,小林裕之,瓜生原健嗣,貝原 聡:膵頭十二指腸切除後長期を経て発症した膵放線菌症の一例.第 81 回臨床外科学会総会,高知,2019.11.14-16
- 鷲見季彦,貝原 聡,河原林卓馬,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,水本素子,北村好史,近藤正人, 橋田裕毅,小林裕之,瓜生原健嗣:切除不能膵頭部癌に対して、Conversion surgery を行い完全切除し得た一例.第 81 回臨床外科学会総会,高知,2019.11.14-16
- 小林裕之,近藤正人,塩川桂一,岩城謙太郎,神部宏幸,水野良祐,河原林卓馬,鷲見季彦,水本素子,橋 田裕毅,貝原 聡:神経モニタリングの経験から辿りついた反回神経麻痺のない上縦隔郭清手技.第 32 回 日本内視鏡外科学会,横浜,2019.12.5-7
- 水本素子,河原林卓馬,鷲見季彦,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,北村好史,近藤正人,橋 田裕毅,小林裕之,瓜生原健嗣,貝原 聡:当院における噴門 LECS の治療成績.第 32 回日本内視鏡外科学会, 横浜,2019.12.5-7
- 神部宏幸,北村好史,河原林卓馬,鷲見季彦,岩城謙太郎,水野良祐,塩川桂一,水本素子,近藤正人,橋 田裕毅,小林裕之,瓜生原健嗣,貝原 聡:絞扼性イレウスに対する腹腔鏡下手術の適応とその限界.第 32 回日本内視鏡外科学会,横浜,2019.12.5-7
- 橋田裕毅,近藤正人,小林裕之,河原林卓馬,鷲見季彦,岩城謙太郎,神部宏幸,水野良祐,北村好史,水本 素子,瓜生原健嗣,貝原 聡:ロボット支援下直腸手術の導入と早期成績.第 32 回日本内視鏡外科学会,横浜, 2019.12.5-7
- 岩城謙太郎,近藤正人,河原林卓馬,鷲見季彦,神部宏幸,水野良祐,水本素子,北村好史,橋田裕毅,小 林裕之,瓜生原健嗣,貝原 聡:高齢者に対する腹腔鏡下胃切除術の合併症頻度は高いが中期成績は良好で ある.第 32 回日本内視鏡外科学会,横浜,2019.12.5-7
- 水野良祐,橋田裕毅,河原林卓馬,鷲見季彦,岩城謙太郎,神部宏幸,塩川桂一,水本素子,北村好史,近 藤正人,小林裕之,瓜生原健嗣,貝原 聡:腹腔鏡下直腸 DST 吻合における縫合不全予防への取り組み. 第 32 回日本内視鏡外科学会,横浜,2019.12.5-8
- 鷲見季彦,瓜生原健嗣,河原林卓馬,神部宏幸,水野良祐,水本素子,北村好史,近藤正人,橋田裕毅,小 林裕之,瓜生原健嗣,貝原 聡:当院における腹腔鏡下鼠径ヘルニア修復術(TAPP 法)の治療成績と合併症. 第 32 回日本内視鏡外科学会,横浜,2019.12.5-7
- 近藤正人,河原林卓馬,鷲見季彦,岩城謙太郎,神部宏幸,水野良祐,水本素子,北村好史,瓜生原健嗣, 小林裕之,橋田裕毅,貝原 聡:市中病院におけるロボット胃癌手術の導入と成績.第 32 回日本内視鏡外 科学会,横浜,2019.12.5-7
- 北村好史,貝原 聡,河原林卓馬,鷲見季彦,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,水本素子,近 藤正人,瓜生原健嗣,小林裕之,橋田裕毅,細谷 亮:” 腹腔鏡下肝 S7,S8 腫瘍切除における画像支援の活 用と手術手技 “.第 32 回日本内視鏡外科学会,横浜,2019.12.5-7
- Masato Kondo, Hironaga Satake, Motoko Mizumoto, Takanori Watanabe, Norimitsu Tanaka, Kenro Hirata, Hiroaki Tanioka, Yoshihiro Okita, Takahisa Kyogoku, Mitsutoshi Tatsumi, Koreatsu Matoba, Shinichi Adachi, Satoshi Kaihara, Hisateru Yasui, Akihito Tsuji:Multicenter phase Ⅱ study of neoadjuvant chemotherapy with S-1 and oxaliplatin for locally advanced gastric cancer (Neo G-SOX P Ⅱ ). ASCO-GI 2020, San Francisco, 2020.1.23-25
- 橋田裕毅,鷲見季彦、河原林卓馬、水野良祐、神部宏幸、岩城謙太郎、塩川桂一、水本素子、近藤正 人、小林裕之、貝原 聡:超高齢者大腸癌に対する腹腔鏡手術の有用性.第 16 回日本消化管学会,姫路, 2020.2.7-8
- 小林裕之,喜多亮介,増井秀行,北野翔一,熊田有希子,松原孝明,塩川桂一,瓜生原健嗣,橋田裕毅,近 藤正人,北村好史,水本素子,貝原 聡,細谷 亮:胸腔鏡下食道癌手術における安全な上縦隔郭清手技の 工夫.第 118 回日本外科学会総会,東京,2018.4.5-
- 橋田裕毅,塩川桂一,松原孝明,熊田有希子,北野翔一,増井秀行,喜多亮介,水本素子,北村好史,近藤 正人,小林裕之,瓜生原健嗣,細谷 亮,貝原 聡:クローン病に対する抗 TNF-a 抗体の有用性と手術加療. 第 118 回日本外科学会総会,東京,2018.4.5-7
- 近藤正人,塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,北村好史,水本素子,瓜生 原健嗣,橋田裕毅,小林裕之,貝原 聡,細谷 亮:高度進行胃癌に対する審査腹腔鏡と術前化学療法の成 績.第 118 回日本外科学会総会,東京,2018.4.5-7
- 水本素子,塩川桂一,松原孝明,熊田有希子,北野翔一,増井秀行,喜多亮介,北村好史,近藤正人,橋田 裕毅,小林裕之,瓜生原健嗣,貝原 聡,細谷 亮:当院における腹腔鏡下胃切除術の再建法による術後障 害の検討.第 118 回日本外科学会総会,東京,2018.4.5-7
- 喜多亮介,塩川桂一,松原孝明,熊田有希子,北野翔一,増井秀行,水本素子,北村好史,近藤正人,小林 裕之,瓜生原健嗣,橋田裕毅,貝原 聡,細谷 亮:腹腔鏡下系統的肝切除の導入~開腹手術と遜色ない質 を保つために~.第 118 回日本外科学会総会,東京,2018.4.5-7
- 北野翔一,塩川桂一,松原孝明,熊田有希子,北野翔一,増井秀行,喜多亮介,貝原 聡,細谷 亮:当院 における TaTME による下部直腸癌手術の短期治療成績.第 118 回日本外科学会総会,東京,2018.4.5-7
- 熊田有希子,近藤正人,塩川桂一,松原孝明,北野翔一,喜多亮介,増井秀行,水本素子,北村好史,貝原 聡, 細谷 亮:胃切除患者における Oral nutrition supplementation の取り組み.第 118 回日本外科学会総会,東京, 2018.4.5-7
- 塩川桂一,瓜生原健嗣,松原孝明,北野翔一,喜多亮介,増井秀行,水本素子,北村好史,近藤正人,橋田裕毅, 小林裕之,貝原 聡,細谷 亮:Comparative analysis of surgical strategy for acute cholecystitis.第 118 回日本 外科学会総会,東京,2018.4.5-7
- 水野良祐,橋田裕毅,岩城謙太郎,神部宏幸,塩川桂一,松原孝明,増井秀行,喜多亮介,水本素子,北村 好史,近藤正人,小林裕之,瓜生原健嗣,貝原 聡,細谷 亮:局所進行直腸癌に対する術前化学療法の有 効性.第 118 回日本外科学会総会,東京,2018.4.5-7
- 鷲見季彦,北野翔一,瓜生原健嗣,貝原 聡,小林裕之,橋田裕毅,近藤正人,北村好史,水本素子,喜多亮介, 増井秀行:当院における閉鎖孔ヘルニア嵌頓症例の検討.第 118 回日本外科学会総会,東京,2018.4.5-7
- 高橋駿太,小林裕之,喜多亮介,増井秀行,北野翔一,熊田有希子,松原孝明,塩川桂一,瓜生原健嗣,橋 田裕毅,近藤正人,北村好史,水本素子,貝原 聡,細谷 亮:術前診断に難渋した小腸粘膜下動脈瘤の一 例.第 118 回日本外科学会総会,東京,2018.4.5-7
- Kobayashi H, Kondo M, Mizumoto M, Kita R, Masui H, Kitano S, Kumata Y, Matsubara T, Shiokawa K, Uryuhara K, Hashida H, Kitamura K, Hosotani R, Kaihara S: Mesenterization and Intra-Operative Neural Monitoring to Reduce the Recurrent Laryngeal Nerve Paralysis after Thoracoscopic esophagectomy in Prone Position. SAGES,Seattle, 2018.4.11-14
- 岩城謙太郎,八木真太郎,森田智視,山本 玄,政野裕紀,福光 剣,長井和之,伊藤孝司,吉澤 淳,加 茂直子,秦浩一郎,田浦康二朗,岡島英明,海道利実,上本伸二:生体肝移植術後の多量腹水に関する危険 因子解析.第 36 回日本肝移植研究会,東京,2018.5.25-26
- Kaihara S, Kitamura K, Uryuuhara K: Tape Guided Parenchymal Dissection Applying Hanging Method for Safe and Secure Anatomical Hepatectomy.JGSSLS2018, Graz, 2018.5.26-27
- Kitamura K, Kaihara S, Uryuuhara K: 3D-CT simulation and laparoscopic procedure for safe anatomical liver resection.JGSSLS2018, Graz, 2018.5.26-27
- Kaihara S, Kitamura K, Uryuhara K, Kita R, Masui H, Hashida H, Hosotani R: Strategies on the treatment of colorectal liver metastasis. The 30th Meeting of Japanese Society of Hepato-Biliary-Pancreatic Surgery, Yokohama,2018.6.7-9
- Kitamura K, Kaihara S, Kita R, Masui H, Uryuhara K, Hashida H, Hosotani R: Our procedure and results for anatomical liver resection less than segmentectomy based on the Glissonean branches. The 30th Meeting of Japanese Society of Hepato-Biliary-Pancreatic Surgery, Yokohama, 2018.6.7-9
- Kita R, Kaihara S, Masui H, Kitamura K, Uryuuhara K, Hosotani R: Evaluation of the safety and validity of hepatectomy for elderly people. The 30th Meeting of Japanese Society of Hepato-Biliary-Pancreatic Surgery, Yokohama, 2018.6.7-9
- Masui H, Kaihara S, Shiokawa K, Matsubara H, Kita R, Mizumoto M, Kitamura K, Kondo M, Hashida H, Kobayashi H, Uryuuhara K, Hosotani R: Evaluation of the new guidelines of IPMN- from the viewpoint of surgical validity-. The 30th Meeting of Japanese Society of Hepato-Biliary-Pancreatic Surgery, Yokohama, 2018.6.7-9
- Iwaki K, Yagi S, Iida T, Masano Y, Tajima T, Okumura S, Yamamoto G, Kamo N, Kaido T, Uemoto S: Case report of extensive isolated spontaneous celiac trunk dissection after liver transplantation. The 30th Meeting of Japanese Society of Hepato-Biliary-Pancreatic Surgery, Yokohama, 2018.6.7-9
- 小林裕之,近藤正人,水本素子,瓜生原健嗣,塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増 井秀行,北村好史,橋田裕毅,貝原 聡,細谷 亮:特発性食道破裂に対して胸腔鏡下穿孔部縫合・縦隔ド レナージ術を施行した 1 例.第 72 回日本食道学会,宇都宮,2018.6.28-29
- 貝原 聡,細谷 亮:膵全摘後中長期成績の検討.第 49 回日本膵臓学会,和歌山,2018.6.29-30
- 塩川桂一,瓜生原健嗣:当院における閉鎖孔ヘルニア嵌頓症例の検討.第 16 回日本ヘルニア学会,札幌, 2018.6.29-30
- 瓜生原健嗣:当院における鼠径ヘルニア手術指導の現状.第 16 回日本ヘルニア学会,札幌,2018.6.29-30
- 貝原 聡,北村好史,瓜生原健嗣,塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,細 谷 亮:アシアロシンチと CT を Fusion させた 3D 画像解析による機能的残肝予備能評価の有効性の検討. 第 73 回日本消化器外科学会,鹿児島,2018.7.11-13
- 小林裕之,喜多亮介,増井秀行,北野翔一,熊田有希子,松原孝明,塩川桂一,近藤正人,貝原 聡,細谷 亮: 合併症ゼロを目指した食道癌の胸腔鏡下縦隔アプローチ.第 73 回日本消化器外科学会,鹿児島,2018.7.11-13
- 橋田裕毅,塩川桂一,松原孝明,喜多亮介,増井秀行,水本素子,近藤正人,小林裕之,細谷 亮,貝原 聡: TaTME による下部直腸手術の短期成績と有用性.第 73 回日本消化器外科学会,鹿児島,2018.7.11-13
- 近藤正人,塩川桂一,松原孝明,熊田有希子,北野翔一,増井秀行,喜多亮介,橋田裕毅,小林裕之,貝原 聡,細谷 亮:完全内側アプローチを主体とした進行横行結腸癌に対する CME を意識した腹腔鏡手術.第 73 回日本消化器外科学会,鹿児島,2018.7.11-13
- 北村好史,貝原 聡,塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,水本素子,瓜生 原健嗣:Our procedure of superior mesenteric artery surrounding dissection for pancreatic head cancer.第 73 回日 本消化器外科学会,鹿児島,2018.7.11-13
- 水本素子,占野尚人,北村好史,近藤正人,橋田裕毅,小林裕之,瓜生原健嗣,貝原 聡,細谷 亮: Transformed laparoscopic endoscopic cooperative surgery for gastric submucosal tumor.第 73 回日本消化器外科学 会,鹿児島,2018.7.11-13
- 北野翔一,近藤正人,塩川桂一,松原孝明,熊田有希子,水本素子,小林裕之,貝原 聡,細谷 亮:ESD 後追加切除症例の対する臨床病理学的特徴に関する検討.第 73 回日本消化器外科学会,鹿児島,2018.7.11-13
- 熊田有希子,貝原 聡,塩川桂一,松原孝明,北野翔一,増井秀行,喜多亮介,水本素子,北村好史,近藤 正人,細谷 亮:80 歳以上の高齢者における肝切除術の手術成績、長期予後の検討.第 73 回日本消化器外 科学会,鹿児島,2018.7.11-13
- Kita R, Kaihara S, Masui H, Kitamura K, Uryuuhara K, Hosotani R:Strategy for pancreaticojejunostomy ~ reducing the pancreatic fistula ~ . The 73rd General Meeting of the Japanese Society of Gastroenterological Surgery, Kagoshima, 2018.7.11-13
- Masui H, Uryuuhara K, Shiokawa K, Matsubara T, Kumata Y, Kitano S, Kita R, Mizumoto M, Kaihara S, Hosotani R: Standardization of distal pancreatectomy for prevention of pancreatic fistula. The 73rd General Meeting of the Japanese Society of Gastroenterological Surgery, Kagoshima, 2018.7.11-13
- 塩川桂一,小林裕之,岩城謙太郎,神部宏幸,松原孝明,増井秀行,喜多亮介,水本素子,北村好史,近藤正人, 橋田裕毅,瓜生原健嗣,貝原 聡,細谷 亮:当院における大腸癌イレウスに対する治療戦略.第 73 回日 本消化器外科学会,鹿児島,2018.7.11-13
- 水野良祐,橋田裕毅,岩城謙太郎,神部宏幸,塩川桂一,松原孝明,増井秀行,喜多亮介,水本素子,北村好史, 近藤正人,小林裕之,瓜生原健嗣,貝原 聡,細谷 亮:Standardization of laparoscopic abdominal incisional hernia repair.第 73 回日本消化器外科学会,鹿児島,2018.7.11-13
- Kobayashi H, Kondo M, Mizumoto M, Kita R, Masui H, Kitano S, Kumata Y, Matsubara T, Shiokawa K, Kaihara S, Hosotani R: Mesentery-oriented Lymph Nodes Dissection and Intra-operative Neural Monitoring to Reduce the Postoperative Recurrent Laryngeal Nerve Paralysis in Esophagectomy. ISDE, Vienna, 2018.9.16-19
- Masui H, Kobayashi H, Kondo M, Kaihara S, Hosotani R: laparoscopic trans-hiatal repair for Boerhaave’s syndrome: A case report. ISDE, Vienna, 2018.9.16-19
- 水本素子,加藤紀子,土井諒也,佐野亜紀子,長谷川美和,貝原 聡:術前減圧処置を要する奨励へのパス 適応の安全性についての検討.クリニカルパス学会,函館,2018.10.12-13
- Kondo M: Introduction and results as a safe operative procedure for robotic gastrectomy. Asian summit on robotic surgery, Singapore, 2018.10.18-21
- 橋田裕毅,塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,近藤 正人,小林裕之,瓜生原健嗣,細谷 亮,貝原 聡:超高齢者大腸癌に対する腹腔鏡手術の検討.第 16 回 日本消化器外科学会大会,神戸,2018.11.1-11.4
- 橋田裕毅,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本素子,北村好史, 近藤正人,小林裕之,瓜生原健嗣,貝原 聡:超高齢者大腸癌に対する腹腔鏡手術の有用性.第 73 回日本 大腸肛門病学会学術集会,東京,2018.11.9-11.10
- Hashida H: Laparoscopic Repair with Sandwich Technique for Parastomal Hernia. ELSA, Kuala Lumpur, 2018.11.15-17
- Mizumoto M, Shimeno N, Hashida H, Kaihara S: Evaluation of laparoscopic and endoscopic cooperative surgery for gastric submucosal tumor of cardia. ELSA, Kuala Lumpur, 2018.11.15-17
- 水野良祐,北村好史,岩城謙太郎,神部宏幸,塩川桂一,松原孝明,増井秀行,喜多亮介,水本素子,近藤 正人,小林裕之,瓜生原健嗣,橋田裕毅,貝原 聡,細谷 亮:当院における NOMI(非閉塞性腸間膜虚血) 症例の検討.第 46 回救急医学会,横浜,2018.11.19-20
- 岩城謙太郎,貝原 聡,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本素子,北村 好史,近藤正人,小林裕之,瓜生原健嗣:肝細胞癌との鑑別が困難であった巨大肝細胞腺腫の 2 切除例.第 80 回日本臨床外科学会,東京,2018.11.22-24
- 神部宏幸,貝原 聡,岩城謙太郎,水野良祐,塩川桂一,松原孝明,増井秀行,喜多亮介,北村好史,近藤正人, 小林裕之,瓜生原健嗣,橋田裕毅:膵腺扁平上皮癌と膀胱癌の同時性重複癌の 1 例.第 80 回日本臨床外科学会, 東京,2018.11.22-24
- 小林裕之,近藤正人,水本素子,喜多亮介,増井秀行,松原孝明,塩川桂一,岩城謙太郎,神部宏幸,水 野良祐,瓜生原健嗣,橋田裕毅,北村好史,貝原 聡:胸腔鏡下食道癌における Mesentery-oriented lymph nodes dissection.第 31 回内視鏡外科学会,福岡,2018.12.6-8
- 橋田裕毅,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本素子,北村 好史,近藤正人,瓜生原健嗣,小林裕之,貝原 聡:脾弯曲部結腸に対する 4 方向アプローチによる腹腔鏡 下左側結腸切除術.第 31 回内視鏡外科学会,福岡,2018.12.6-8
- 近藤正人,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,増井秀行,喜多亮介,貝原 聡:膵良 性、境界悪性疾患に対する腹腔鏡での機能温存を重視した尾側膵切除術.第 31 回内視鏡外科学会,福岡, 2018.12.6-8
- 北村好史,貝原 聡,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本 素子,近藤正人,瓜生原健嗣,小林裕之,橋田裕強,細谷 亮:当院における腹腔鏡下肝部分切除術の治療 成績.第 31 回内視鏡外科学会,福岡,2018.12.6-8
- 水本素子,水野良祐,神部宏幸,岩城謙太郎,塩川桂一,松原孝明,増井秀行,喜多亮介,北村好史,近藤 正人,橋田裕毅,小林裕之,瓜生原健嗣,貝原 聡,細谷 亮:当院における胃粘膜下腫瘍に対する手術法 の選択.第 31 回内視鏡外科学会,福岡,2018.12.6-8
- 喜多亮介,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,増井秀行,水本素子,北村好史,近藤 正人,小林裕之,瓜生原健嗣,橋田裕毅,貝原 聡,細谷 亮:下部直腸癌に対する TaTME 導入後の短期 成績.第 31 回内視鏡外科学会,福岡,2018.12.6-8
- 増井秀行,橋田裕毅,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,水本素子,北村好史, 近藤正人,瓜生原健嗣,小林裕之,貝原 聡,細谷 亮:下行結腸進行癌に対する内視鏡手術.第 31 回内 視鏡外科学会,福岡,2018.12.6-8
- 塩川桂一,近藤正人,岩城謙太郎,神部宏幸,水野良祐,松原孝明,喜多亮介,水本素子,北村好史,橋田裕毅, 瓜生原健嗣,小林裕之,貝原 聡,細谷 亮:当院における大腸癌イレウス減圧方法の検討.第 31 回内視 鏡外科学会,福岡,2018.12.6-8
- 岩城謙太郎,近藤正人,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本素子,北村 好史,小林裕之,瓜生原健嗣,貝原 聡:Complicated appendicitis に対する内視鏡手術.第 31 回内視鏡外科 学会,福岡,2018.12.6-8
- 神部宏幸,橋田裕毅,岩城謙太郎,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,貝原 聡:腹腔 鏡下腹壁ヘルニア修復術の新しい流れ.第 31 回内視鏡外科学会,福岡,2018.12.6-8
- 水野良祐,瓜生原健嗣,岩城謙太郎,神部宏幸,塩川桂一,松原孝明,増井秀行,喜多亮介,水本素子,北 村好史,近藤正人,小林裕之,橋田裕毅,貝原 聡,細谷 亮:鼠径部解剖を重要視した TAPP/TEPP の術 式選択と成績.第 31 回内視鏡外科学会,福岡,2018.12.6-8
- 橋田裕毅,岩城謙太郎,神部宏幸,水野良祐,塩川桂一,松原孝明,喜多亮介,増井秀行,水本素子,北村 好史,近藤正人,瓜生原健嗣,小林裕之,貝原 聡:大腸神経内分泌腫瘍の治療成績.第 15 回日本消化管 学会,佐賀,2019.2.1-03
- 橋田裕毅:傍ストーマヘルニア治療における腹腔鏡手術.第 36 回日本ストーマ排泄リハビリテーション学会, 大阪,2019.2.22-23
- Kaihara S,Iwamura S,Matsubara T,Kumata Y,Kitano S,Kita R,Masui H,Mizumoto M,Uryuhara K: Preoperative assessment of remnant liver function in major hepatectomy after portal vein embolization using 99mTc-GSA scintigraphy / 3D-CT fused imaging.AHPBA(米国肝胆膵),Miami,2017.3.29-4.2
- 近藤正人,水本素子,岩村宣亜,喜多亮介,増井秀行,北野翔一,熊田有希子,松原孝明,貝原 聡,細谷 亮:グルカゴン静注胃管延長による食道癌術後縫合不全対策.第 117 回外科学会,横浜,2017.4.27-29
- 松原孝明,大森彩加,熊田有希子,北野翔一,増井秀行,喜多亮介,岩村宣亜,水本素子,近藤正人,小林 裕之,細谷 亮,貝原 聡:市中病院における腹腔鏡下大腸手術の教育の取り組み.第 117 回外科学会,横 浜,2017.4.27-29
- 貝原 聡,塩川桂一,松原孝明,熊田有希子,北野翔一,喜多亮介,増井秀行,水本素子,近藤正人,瓜生 原健嗣,小林裕之,橋田裕毅,細谷 亮:門脈浸潤を伴う膵頭部通常型膵癌切除における門脈合併切除成績. 第 117 回外科学会,横浜,2017.4.27-29
- 占野尚人,松原孝明,熊田有希子,北野翔一,増井秀行,喜多亮介,北村好史,近藤正人,橋田裕毅,小林 裕之,瓜生原健嗣,貝原 聡,細谷 亮:当院における腹腔鏡内視鏡合同手術.第 117 回外科学会,横浜, 2017.4.27-29
- 貝原 聡,塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,近藤 正人,橋田裕毅,小林裕之,瓜生原健嗣,細谷 亮:膵頭十二指腸切除術における術前状態の術中 / 術後に 与える影響の検討.第 117 回外科学会,横浜,2017.4.27-29
- 松原孝明,北野翔一,熊田有希子,喜多亮介,水本素子,北村好史,近藤正人,橋田裕毅,小林裕之,瓜生 原健嗣,貝原 聡,細谷 亮:大腸癌肝転移切除後の治療戦略~術後補助化学療法~.第 117 回外科学会, 横浜,2017.4.27-29
- 近藤正人,塩川桂一,松原孝明,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,橋田裕毅,瓜生 原健嗣,小林裕之,貝原 聡,細谷 亮:術前 SOX 療法を施行した局所進行胃癌手術症例についての検討. 第 117 回外科学会,横浜,2017.4.27-29- 144 -
- 橋田裕毅,塩川桂一,松原孝明,北野翔一,喜多亮介,増井秀行,水本素子,北村好史,近藤正人,瓜生原 健嗣,小林裕之,貝原 聡,細谷 亮:大腸内分泌腫瘍に対する当院の外科治療成績.第 117 回外科学会, 横浜,2017.4.27-29
- 近藤正人,塩川桂一,北野翔一,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,瓜生原健嗣,橋 田裕毅,小林裕之,貝原 聡,細谷 亮:当院における膿瘍形成性虫垂炎に対する Interval appendectomy の 取り組み.第 117 回外科学会,横浜,2017.4.27-29
- 松原孝明,熊田有希子,北野翔一,増井秀行,喜多亮介,岩村宣亜,水本素子,北村好史,近藤正人,橋田 裕毅,小林裕之,瓜生原健嗣,貝原 聡,細谷 亮:卵巣と膵臓に同時に腫瘍が見つかり原発巣特定に苦慮 し診断的切除手術まで行った 1 例.第 117 回外科学会,横浜,2017.4.27-29
- Uryuhara K,Kitamura K,Iwamura S,Kita R,Masui H,Hashida H,Hosotani R:Hepatectomy for Large HCC - strategies and technical tips for secure operation -.第 29 回肝胆膵外科学会,横浜,2017.6.7-10
- Kaihara S,Kita R,Masui H,Uryuhara K,Hashida H,Hosotani R:Reliable and safe procedure of anatomical resection of segment VIII for HCC.第 29 回肝胆膵外科学会,横浜,2017.6.7-10
- Kaihara S,Masui H,Kitamura K,Hosotani R:Evaluation of treatment outcome to incidental gallbladder cancer. 第 29 回肝胆膵外科学会,横浜,2017.6.7-10
- Kaihara S:Pancreatic neuroendocrine tumors:A single institution’s experience with surgically treated patients. 第 29 回肝胆膵外科学会,横浜,2017.6.7-10
- 瓜生原健嗣,塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,近 藤正人,橋田裕毅,小林裕之,貝原 聡,細谷 亮:鼠径部ヘルニア嵌頓症例に対する治療戦略.第 15 回 日本ヘルニア学会,東京,2017.6.2-3
- Satake H,Tanioka H,Miyake Y,Yoshioka S,Watanabe T,Matsuura M,Kyogoku T,Inukai M,Kotake T,Okita Y, Hatachi Y,Yasui H,Kotaka M,Kato T,Kaihara S,Tsuji A:Hepatectomy followed by adjuvant chemotherapy with capacitabine plus oxaliplatin for three months for colorectal cancer liver metastases:A multi-center phase 2 study.2017 ASCO Annual Meeting,Chicago,2017.6.2-6
- Kaihara S,Kondo M:Therapeutic strategy for acute appendicitis with an appendicular abscess or mass.EAES 2017,Frankfurt,2017.6.14-17
- Kita R,Masui H:Liver Parenchymal Dissection with Pre-coagulation Dissection Technique for Laparoscopic Hepatectomy.EAES 2017,Frankfurt,2017.6.14-17
- Kaihara S:A safe technique for laparoscopic distal pancreatectomy with spleen preservation.EAES 2017, Frankfurt,2017.6.14-17
- 水本素子,近藤正人,瓜生原健嗣,塩川圭一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,北 村好史,貝原 聡,細谷 亮:食道間膜腸間膜化と Intra-operative Nerve Monitoring による胸腔鏡下食道切除 の定型化.第 71 回日本食道学会,軽井沢,2017.6.15-16
- 増井秀行,喜多亮介,近藤正人,小林裕之,貝原 聡,細谷 亮:手術治療を行った食道穿孔及び特発性食 道破裂症例の検討.第 71 回日本食道学会,軽井沢,2017.6.15-16
- 小林裕之,水本素子,貝原 聡,細谷 亮:術前栄養免疫状態と術後合併症の関連についての検討.第 71 回日本食道学会,軽井沢,2017.6.15-16
- 貝原 聡,塩川桂一,松原孝明,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,近藤正人,橋田 裕毅,瓜生原健嗣,小林裕之,細谷 亮:腫瘍破裂による腹痛を契機に発見された SPN の 1 例.第 48 回日 本膵臓学会,京都,2017.7.14-15
- 水本素子,岩村宣亜,喜多亮介,増井秀行,北野翔一,熊田有希子,大森彩加,松原孝明,貝原 聡: Intra-operative Nerve Monitoring による食道癌術後反回神経麻痺の予防効果.第 72 回消化器外科学会,金沢,2017.7.20-22
- 貝原 聡,大森彩加,松原孝明,熊田有希子,北野翔一,喜多亮介,増井秀行,岩村宣亜,細谷 亮:右葉 系肝切除における 99mTc-GSA シンチグラフィーと VINCENT 融合画像による肝予備能評価.第 72 回消化 器外科学会,金沢,2017.7.20-22
- 瓜生原健嗣,北村好史,松原孝明,熊田有希子,北野翔一,喜多亮介,増井秀行,岩村宣亜,細谷 亮: Treatment Strategies for Colorectal Liver Metastasis:The Analysis of Risk Factor and the Management.第 72 回消 化器外科学会,金沢,2017.7.20-22
- 松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,岩村宣亜,貝原 聡,細谷 亮:救急と外科医が 協力する急性汎発性腹膜炎手術患者の術後管理.第 72 回消化器外科学会,金沢,2017.7.20-22
- 貝原 聡,塩川桂一,松原孝明,北野翔一,熊田有希子,増井秀行,水本素子,北村好史,近藤正人,橋 田裕毅,瓜生原健嗣,小林裕之,細谷 亮:切除可能膵癌に対する術前治療戦略.第 72 回消化器外科学会, 金沢,2017.7.20-22
- 橋田裕毅,松原孝明,北野翔一,熊田有希子,喜多亮介,水本素子,北村好史,近藤正人,小林裕之,瓜生 原健嗣,貝原 聡,細谷 亮:A clinical study of surgical resection for patients over 80 years of age with colorectal cancer.第 72 回消化器外科学会,金沢,2017.7.20-22
- 貝原 聡,塩川桂一,松原孝明,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,近藤正人,橋田 裕毅,瓜生原健嗣,小林裕之,細谷 亮:The strategies for the reduction of the bile leakage after the hepatectomy in our hospital.第 72 回消化器外科学会,金沢,2017.7.20-22
- 小林裕之,大森彩加,北野翔一,熊田有希子,喜多亮介,増井秀行,細谷 亮,貝原 聡:当院における大 腸癌イレウス患者治療戦略の検討.第 72 回消化器外科学会,金沢,2017.7.20-22
- 塩川桂一,松原孝明,熊田有希子,北野翔一,増井秀行,喜多亮介,水本素子,北村好史,近藤正人,橋田 裕毅,小林裕之,瓜生原健嗣,貝原 聡,細谷 亮:汚染手術における創部 SSI 撲滅に向けて.第 72 回消 化器外科学会,金沢,2017.7.20-22
- 貝原 聡:当院における生体肝移植ドナーの術後長期フォローの実際.第 53 回日本移植学会,旭川, 2017.9.7-9
- 占野尚人,猪熊哲朗,貝原 聡:当院における Delle を伴う内腔発育型胃粘膜下腫瘍に対する腹腔鏡内視鏡 合同手術.第 107 回日本消化器病学会近畿支部例会,大阪,2017.9.23
- 松原孝明,熊田有希子,北野翔一,増井秀行,喜多亮介,水本素子,北村好史,近藤正人,小林裕之,瓜生 原健嗣,細谷 亮,貝原 聡:大腸神経内分泌腫瘍に対する外科治療の限界と展望.第 15 回日本消化器外 科学会大会,福岡,2017.10.12-15
- 橋田裕毅,松原孝明,北野翔一,熊田有希子,喜多亮介,水本素子,北村好史,近藤正人,小林裕之,瓜生 原健嗣,貝原 聡,細谷 亮:当院における左側大腸癌イレウスに対する治療戦略.第 15 回日本消化器外 科学会大会,福岡,2017.10.12-15
- 水本素子,大森彩加,松原孝明,北野翔一,喜多亮介,増井秀行,岩村宣亜,貝原 聡,細谷 亮:当院に おける消化管 GIST の再発因子の検討.第 15 回日本消化器外科学会大会,福岡,2017.10.12-15
- Kondo M,Mizumoto M,Kita R,Masui H,Kitano S,Kumata Y,Matsubara T,Shiokawa K,Kaihara S,Hosotani R: Prevention of Recurrent Laryngeal Nerve Paralysis after Esophagectomy by Intra-operative Nerve Monitoring.ACS, San Diego,2017.10.22-26
- 塩川桂一,松原孝明,北野翔一,熊田有希子,増井秀行,喜多亮介,貝原 聡,細谷 亮:腹腔鏡手術にお ける電気メスの安全な使用法.胃癌術後障害研究会,東京,2017.11.3-4
- 近藤正人,塩川桂一,松原孝明,北野翔一,喜多亮介,増井秀行,水本素子,北村好史,瓜生原健嗣,小林 裕之,橋田裕毅,貝原 聡,細谷 亮:胃術後患者における Oral nutrition supplementation の取り組み.胃癌 術後障害研究会,東京,2017.11.3-4
- 喜多亮介,塩川桂一,小林裕之,細谷 亮,貝原 聡:直腸肛門部悪性黒色腫に対して腹腔鏡下腹会陰式直 腸切断術(TAMIS-APR)を行った 1 例.第 72 回大腸肛門病学会,福岡,2017.11.10-11
- Shiokawa K,Matsubara T,Kumata Y,Kitano S,Kita R,Masui H,Mizumoto M,Kondo M,Kobayashi H, Hosotani R, Kaihara S:Laparoscopic Posterior Rectopexy for Complete Rectal Prolapse.ACRES2017,Taipei, 2017.11.24-26
- Kaihara S:Complete intrathoracic reconstruction for lower esophageal cancer under the prone position. ACRES2017,Taipei,2017.11.24-26
- Shimeno N,Shiokawa K,Matsubara T,Kumata Y,Kitano S,Masui H,Kita R,Kondo M,Hashida H,Kaihara S: Laparoscopic endoscopic cooperative surgery for gastric submucosal tumor.ACRES2017,Taipei,2017.11.24-26
- 塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,近藤正人,橋田 裕毅,瓜生原健嗣,小林裕之,細谷 亮:当院における腹腔鏡下系統的肝切除導入と成績.第 30 回日本内 視鏡外科学会,京都,2017.12.7-9
- 近藤正人,水本素子,喜多亮介,増井秀行,北野翔一,熊田有希子,松原孝明,塩川圭一,瓜生原健嗣,橋 田裕穀,北村好史,貝原 聡,細谷 亮:反回神経麻痺のない食道癌上縦隔郭清手技の工夫.第 30 回日本 内視鏡外科学会,京都,2017.12.7-9
- 塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,近藤正人,瓜生 原健嗣,小林裕之,細谷 亮,貝原 聡:傍ストーマヘルニアに対する腹腔鏡下修復術.第 30 回日本内視 鏡外科学会,京都,2017.12.7-9
- 喜多亮介,増井秀行,北野翔一,熊田有希子,水本素子,北村好史,小林裕之,瓜生原健嗣,橋田裕毅,貝 原 聡,細谷 亮:進行横行結腸癌に対する完全内側アプローチを基本とした挟みうち D3 郭清.第 30 回 日本内視鏡外科学会,京都,2017.12.7-9
- 貝原 聡,塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,水本素子,近藤正人,瓜生 原健嗣,小林裕之,橋田裕毅,細谷 亮:当院での腹腔鏡下系統的肝切除における画像支援活用法.第 30 回日本内視鏡外科学会,京都,2017.12.7-9
- 塩川桂一,松原孝明,熊田有希子,北野翔一,増井秀行,喜多亮介,北村好史,近藤正人,橋田裕毅,小林 裕之,瓜生原健嗣,貝原 聡,細谷 亮:当院における胃粘膜下腫瘍に対する腹腔鏡内視鏡合同手術の工夫. 第 30 回日本内視鏡外科学会,京都,2017.12.7-9
- 北村好史,塩川桂一,松原孝明,北野翔一,熊田有希子,増井秀行,水本素子,近藤正人,橋田裕毅,瓜生 原健嗣,小林裕之,貝原 聡,細谷 亮:大腸癌肝転移同時切除症例の短期成績に関する検討.第 30 回日 本内視鏡外科学会,京都,2017.12.7-9
- 貝原 聡,塩川桂一,松原孝明,北野翔一,熊田有希子,喜多亮介,水本素子,北村好史,近藤正人,小林裕之, 橋田裕毅,瓜生原健嗣,細谷 亮:腹腔鏡下肝切除術における Difficulty scoring system の有用性についての検 討.第 30 回日本内視鏡外科学会,京都,2017.12.7-9
- 橋田裕毅,塩川桂一,松原孝明,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,近藤正人,瓜生 原健嗣,小林裕之,貝原 聡,細谷 亮:妊娠中の急性虫垂炎に対して腹腔鏡下虫垂切除術を施行した 9 例. 第 30 回日本内視鏡外科学会,京都,2017.12.7-9
- 橋田裕毅,塩川桂一,松原孝明,北野翔一,喜多亮介,増井秀行,水本素子,北村好史,近藤正人,瓜生原健嗣, 小林裕之,貝原 聡,細谷 亮:当院の腹腔鏡下直腸後方固定の手術成績.第 30 回日本内視鏡外科学会,京都, 2017.12.7-9
- 瓜生原健嗣,小林裕之,橋田裕毅,近藤正人,北村好史,水本素子,喜多亮介,増井秀行,北野翔一,熊田 有希子,塩川桂一,細谷 亮,貝原 聡:鼠径部および閉鎖孔ヘルニア嵌頓緊急手術症例の術式選択の検討. 第 30 回日本内視鏡外科学会,京都,2017.12.7-9
- 瓜生原健嗣,松原孝明,北野翔一,熊田有希子,喜多亮介,増井秀行,水本素子,北村好史,近藤正人,橋 田裕毅,小林裕之,貝原 聡,細谷 亮:当院における急性胆嚢炎に対する術式および治療法選択の検討. 第 30 回日本内視鏡外科学会,京都,2017.12.7-9
- 水本素子:当院における腹腔鏡下幽門側胃切除術の再建法による術後障害の比較.第90回日本胃癌学会,横浜, 2018.3.7-9
- 近藤正人:Neoadjuvant chemotherapy using G-SOX for locally advanced gastric cancer.第90回日本胃癌学会,横浜, 2018.3.7-9
- 貝原 聡,他:当院における肝外胆管癌手術の現状と対策.第116回日本外科学会,大阪,2016.4.14-16
- 瓜生原健嗣,他:当院における肝移植後C型肝炎再発に対する治療状況と新たな抗ウイルス薬使用経験.第 116回日本外科学会,大阪,2016.4.14-16
- 小林裕之,他:食道癌左上縦隔リンパ節郭清時のNIM-response systemの有用性.第116回日本外科学会,大 阪,2016.4.14-16
- 橋田裕毅,他:クローン病に対する手術加療と周術期抗TNF-α抗体治療.第116回日本外科学会,大阪, 2016.4.14-16
- 小森淳二,他:幹細胞移植による肝臓・臓器創世へのチャレンジ.第116回日本外科学会,大阪, 2016.4.14-16
- 近藤正人,他:局所進行胃癌に対する術前SOX療法.第116回日本外科学会,大阪,2016.4.14-16
- 水本素子,他:Delleを伴う胃粘膜下腫瘍に対する腹腔鏡内視鏡合同手術の工夫.第116回日本外科学会,大 阪,2016.4.14-16
- 阪本裕亮,他:当院におけるT2胆嚢癌についての術式の検討.第116回日本外科学会,大阪,2016.4.14-16
- 喜多亮介,他:創部管理プロトコールの有用性の検討.第116回日本外科学会,大阪,2016.4.14-16
- 増井秀行,他:高齢者に対する肝切徐の治療成績.第116回日本外科学会,大阪,2016.4.14-16
- 北野翔一,他:当院における膵消化管吻合の工夫と成績.第116回日本外科学会,大阪,2016.4.14-16
- 熊田有希子,他:当院における悪性大腸閉塞に対する大腸ステントSEMSの留置成績.第116回日本外科学 会,大阪,2016.4.14-16
- Kaihara S,et al: Treatment strategy for large HCC. 28th JHPBA annual meeting,Osaka,2016.6.4 - 6
- Iwamura S,et al: Pancreatoduodenectomy with portal vein resection for locally advanced pancreatic head cancer. 28th JHPBA annual meeting,Osaka,2016.6.4 - 6
- Kita R,et al: Evaluation of clinical outcome of our procedure in biliary reconstruction. 28th JHPBA annual meeting, Osaka,2016.6.4 - 6
- Masui H,et al: Standardization of distal pancreatectomy for prevention of pancreatic fistula. 28th JHPBA annual meeting,Osaka,2016.6.4 - 6
- 瓜生原健嗣,他:当院におけるBlumgart変法による膵空腸吻合の検討.第28回日本肝胆膵外科学会,大阪, 2016.6.4 - 6
- 橋田裕毅,他:完全直腸脱に対する腹腔鏡下直腸固定術の手技と有用性.第18回日本女性骨盤底医学会,北 九州,2016.6.11-12
- Kobayashi H,et al: Prevention of Recurrent Laryngeal Nerve Paralysis after Esophagectomy using NIM-Response System. EAES 2016,Amsterdam,2016.6.15-18
- Mizumoto M,et al: A new method of laparoscopic endoscopic cooperative surgery for gastric submucosal tumor. EAES 2016,Amsterdam,2016.6.15-18
- 小林裕之,他:食道癌術後栄養のための胃管瘻作成の工夫と治療成績.第70回日本食道学会,東京, 2016.7.4 - 6
- 貝原 聡,他:Our strategies to achieve safety in major hepatectomy.第71回日本消化器外科学会,徳島, 2016.7.14-16
- 小森淳二,他:同所性肝細胞シート移植による臓器再生.第71回日本消化器外科学会,徳島,2016.7.14-16
- 橋田裕毅,他:傍ストーマヘルニアに対するSandwich法による腹腔鏡下修復術.第71回日本消化器外科学 会,徳島,2016.7.14-16
- 瓜生原健嗣,他:当院における生体肝移植後長期フォロー患者の問題点.第71回日本消化器外科学会,徳島, 2016.7.14-16
- 水本素子,他:当院における十二指腸腫瘍に対する腹腔鏡内視鏡合同手術の経験.第71回日本消化器外科学 会,徳島,2016.7.14-16
- 木下裕光,他:当院における80才以上大腸大腸癌手術症例の検討.第71回日本消化器外科学会,徳島, 2016.7.14-16
- 熊田有希子,他:80歳以上の高齢者における肝切除術の手術成績,長期予後の検討.第71回日本消化器外科 学会,徳島,2016.7.14-16
- 喜多亮介,他:透析患者に対する外科手術について.第71回日本消化器外科学会,徳島,2016.7.14-16
- 阪本裕亮,他:直腸癌手術における縫合不全症例の検討と対策.第71回日本消化器外科学会,徳島, 2016.7.14-16
- 北野翔一,他:当院における膵頭十二指腸切除術後の膵液瘻低減に向けた工夫.第71回日本消化器外科学 会,徳島,2016.7.14-16
- 大森彩加,他:早期直腸癌に合併した微少NET G2の1切除例.第71回日本消化器外科学会,徳島, 2016.7.14-16
- Kaihara S,et al: Long term follow up after surgical resection for pancreas cancer smaller than 2cm in diameter. The 20th meeting of IAP,Sendai,2016.8.4 - 7
- Iwamura S,et al: Management of locally advanced pancreatic cancer adjacent to the celiac axis. The 20th meeting of IAP,Sendai,2016.8.4 - 7
- Kita R,et al: Our Strategy for pancreaticojejunostomy. The 20th meeting of IAP,Sendai,2016.8.4 - 7
- Kondo M,et al: Complete laparoscopic spleen-preserving distal pancreatectomy without splenic vessels ligation. ACS 2016,Washington DC,2016.10.16-20
- Kumata M,et al: The Sandwich Method for Parastomal Hernia. ACS 2016,Washington DC,2016.10.16-20 ― 152 ―
- 橋田裕毅,他:多発転移を伴う切除不能横行結腸癌に対する化学療法CR後の原発巣再発を切除した1例. 第54回日本癌治療学会,横浜,2016.10.20-22
- 近藤正人,他:腹腔鏡胃癌手術における郭清の定型化と要点.胃癌術後障害研究会,米子,2016.10.27-28
- 増井秀行,他:80歳以上の高齢者胃癌手術症例の検討.胃癌術後障害研究会,米子,2016.10.27-28
- 熊田有希子,他:The Sandwich Method for Parastomal Hernia.第14回日本ヘルニア学会,東京,2016.10.28-29
- 大森彩加,他:The usefulness of preoperative ultrasound scan to detect contralateral groin hernia.第14回日本ヘル ニア学会,東京,2016.10.28-29
- 松原孝明,他:当院における腹腔鏡下腹壁瘢痕ヘルニア修復術手術術式の検討.第14回日本ヘルニア学会, 東京,2016.10.28-29
- Hashida H,et al: Infliximab therapy and surgical intervention for Crohn’s disease. APDW 2016,Kobe,2016.11. 2 - 5
- Kaihara S,et al: Liver parenchymal dissection with pre-coagulation dissection technique for laparoscopic hepatectomy. ELSA 2016,Shuzo,2016.11. 9 -12
- Masui H,et al:Introduction of Laparoscopic Liver Resection in our hospital. ELSA 2016,Shuzo,2016.11. 9 -12
- 北村好史:術前に診断できなかった異物誤飲による小腸穿孔(症例報告).第44回日本救急医学会,東京, 2016.11.17-18
- 橋田裕毅:下部消化管穿孔に対する緊急人工肛門造設後のSSI予防の取り組み.第71回日本大腸肛門病学会, 伊勢,2016.11.18-19
- 岩本宣亜:当科における腹腔鏡下系統的肝切除の導入に向けた取り組み-外側区域切除におけるグリソン個 別先行処理法-.第10回肝臓内視鏡外科研究会,東京,2016.11.23
- 増井秀行:当院における高難度部腫瘍へのアプローチ~市中病院における取り組み~.第10回肝臓内視鏡外 科研究会,東京,2016.11.23
- 近藤正人:胃癌手術の術野展開を応用した腹腔鏡下尾側膵切除術.第8回膵臓内視鏡外科研究会,東京, 2016.11.23
- 大森彩加:腫瘍進展により膵の著明な腫大を認めたIPMCの1切除例.第78回臨床外科学会,東京, 2016.11.24-26
- 松原孝明:消化管出血をきたし,腹腔鏡下胃局所切除術を施行した胃glomus腫瘍の1例.第78回臨床外科学 会,東京,2016.11.24-26
- 水本素子:腹腔鏡下大腸切除術に対するクリニカルパスを用いた検討.第17回日本クリニカルパス学会学術 集会,金沢,2016.11.24-26
- 貝原 聡,他:出血しない肝実質切離法:ソフト凝固によるpre-coagulation dissection technique.第29回内視 鏡外科学会,横浜,2016.12. 8 -10
- 小林裕之,他:腸管膜化とIntra-Operative Nerve Monitoringによる食道癌術後反回神経麻痺の予防.第29回内 視鏡外科学会,横浜,2016.12. 8 -10
- 橋田裕毅,他:脾弯曲部結腸癌に対する内側アプローチを中心とした腹腔鏡下左側結腸切除術.第29回内視 鏡外科学会,横浜,2016.12. 8 -10
- 近藤正人,他:一般市中病院における幽門側胃切除術の定型化 布石と本番,場の置き換え.第29回内視鏡 外科学会,横浜,2016.12. 8 -10
- 近藤正人,他:腫瘍と脈管,脾臓との位置関係から術式選択を行う機能温存尾側膵切除術の定型化.第29回 内視鏡外科学会,横浜,2016.12. 8 -10
- 北村好史,他:当科での腹腔鏡下肝外側区域切除におけるGlisson処理法の手技改新~適応拡大にむけての 段階的な工夫.第29回内視鏡外科学会,横浜,2016.12. 8 -10
- 水本素子,他:当院における腹腔鏡下胃全摘術のLinear staplerを用いた吻合法.第29回内視鏡外科学会,横 浜,2016.12. 8 -10
- 岩村宣亜,他:腹腔鏡下尾側膵切除における術野展開の工夫 腹腔鏡下膵体尾部切除における胃のテーピン グは必要か?第29回内視鏡外科学会,横浜,2016.12. 8 -10
- 増井秀行,他:市中病院における腹腔鏡下肝切徐術の試み.第29回内視鏡外科学会,横浜,2016.12. 8 -10
- 喜多亮介,他:左側進行結腸癌に対する内側アプローチによる手術手技の定型化.第29回内視鏡外科学会, 横浜,2016.12. 8 -10
- 北野翔一,他:当院における腹腔鏡補助下右側結腸切除術の出血量低減にむけた工夫.第29回内視鏡外科学 会,横浜,2016.12. 8 -10
- 熊田有希子,他:腹腔鏡下胃切除術における止血手技~出血を広げない,ドライな視野を保つための工夫. 第29回内視鏡外科学会,横浜,2016.12. 8 -10
- 大森彩加,他:当院におけるTAPPと鼠径部切開法の実際.第29回内視鏡外科学会,横浜,2016.12. 8 -10
- 松原孝明,他:腹腔鏡下腹壁瘢痕ヘルニア修復術の定型化にむけての取り組み.第29回内視鏡外科学会,横 浜,2016.12. 8 -10
- 橋田裕毅,他:傍ストーマヘルニアに腹腔鏡下修復術.第34回日本ストーマ排泄リハビリテーション学会, 名古屋,2017.2.17-18 70.近藤正人,他:局所進行胃癌に対する術前SOX療法の治療成績.第89回日本胃癌学会,広島,2017.3.8 - 9
- Kondo M,Kita R,Masui H,Sakamoto Y,Kinoshita H,Komori J,Uryuhara K,Kobayashi H,Hashida H, Kaihara S,Hosotani R:Total Medial Approach for Complete Mesoscopic Excision of Advanced Transverse Colon Cancer How to Approach Easily Ensuring Oncological Safety.SAGES2015,Nashville,2015. 4. 15-20
- Kinoshita H,Kondo M,Kita R,Masui H,Sakamoto Y,Okada K,Yamamoto T,Miki A,Yagi S,Uryuhara K,Kobayashi H,Hashida H,Kaihara S,Hosotani R:Thoracoscopic intrathoracic esophagogastric anastomosis following minimally invasive esophagectomy for the patient after total laryngectomy,report of a case.SAGES2015,Nashville,2015. 4. 15-20
- 小林裕之,近藤正人,岡田和幸,山本健人,木下裕光,阪本裕亮,喜多亮介,増井秀行,瓜生原健嗣,橋田 裕穀,八木真太郎,三木 明,細谷 亮,貝原 聡:腹臥位胸腔鏡下食道切除術における左上縦隔郭清の定 型化.第116回外科学会,名古屋,2015. 4. 16-18
- 瓜生原健嗣,増井秀行,喜多亮介,阪本裕亮,木下裕光,山本健人,岡田和幸,三木 明,近藤正人,八木 眞太郎,橋田裕毅,小林裕之,貝原 聡,細谷 亮:当院における腹部外傷治療の実際-救急部主導の協動 的かつ協調的診療体制.第116回外科学会,名古屋,2015. 4. 16-18
- 橋田裕毅,喜多亮介,増井秀行,阪本裕亮,木下裕光,岡田和幸,山本健人,三木 明,近藤正人,瓜生原 健嗣,小林裕之,貝原 聡,細谷 亮:完全直腸脱に対する腹腔鏡下後方固定術-術式と骨盤臓器機能から 診た検討-.第116回外科学会,名古屋,2015. 4. 16-18
- 八木真太郎,貝原 聡,喜多亮介,阪本裕亮,木下裕光,岡田和幸,山本健人,三木 明,近藤正人,小森 淳二,瓜生原健嗣,橋田裕毅,小林裕之,細谷 亮:局所進行膵癌に対するR0をめざした手術手技.第116回 外科学会,名古屋,2015. 4. 16-18
- 岡田和幸,近藤正人,北野翔一,熊田有希子,喜多亮介,増井秀行,阪本裕亮,岩村宣亜,水本素子,小森 淳二,瓜生原健嗣,橋田裕毅,小林裕之,貝原 聡,細谷 亮:食道胃接合部癌に対する手術手技.第116回 外科学会,名古屋,2015. 4. 16-18
- 山本健人,近藤正人,北野翔一,熊田有希子,喜多亮介,増井秀行,阪本裕亮,岩村宣亜,水本素子,小森 淳二,瓜生原健嗣,橋田裕毅,小林裕之,貝原 聡,細谷 亮:腹腔鏡下幽門側胃切除術の治療成績と術前 診断.第116回外科学会,名古屋,2015. 4. 16-18
- 喜多亮介,八木真太郎,増井秀行,木下裕光,阪本裕亮,岡田和幸,山本健人,三木 明,近藤正人,瓜生原 健嗣,小林裕之,橋田裕毅,貝原 聡,細谷 亮:切除可能膵癌の成績.第116回外科学会,名古屋,2015. 4. 16-18
- 増井秀行,貝原 聡,喜多亮介,阪本裕亮,木下裕光,岡田和幸,山本健人,三木 明,近藤正人,小森淳二, 瓜生原健嗣,橋田裕毅,小林裕之,細谷 亮:99mTc-GSA-SPECTとKICGに基づく肝切除術式決定法の安全 性.第116回外科学会,名古屋,2015. 4. 16-18
- 登 祐哉,橋田裕毅,喜多亮介,増井秀行,阪本裕亮,木下裕光,岡田和幸,山本健人,三木 明,近藤正人, 瓜生原健嗣,小林裕之,貝原 聡,細谷 亮:外傷性十二指腸損傷の一例.第116回外科学会,名古屋,2015. 4. 16-18
- 水本素子,岡部 寛,田中英治,角田 茂,久森重夫,村上克宏,坂井義治:審査腹腔鏡による進行胃癌に 対する病期診断法の有用性についての検討.第116回外科学会,名古屋,2015. 4. 16-18
- 岩村宣亜,飯田 拓,寺嶋宏明,松原弘侑,後藤 徹,井上善景,吉冨摩美,内田洋一朗,上田修吾,金澤 旭宣:膵頭部領域腫瘍に対する術前胆道ドレナージと周術期合併症との関連性.第116回外科学会,名古屋, 2015. 4. 16-18
- 増井秀行,瓜生原健嗣,喜多亮介,阪本裕亮,木下裕光,岡田和幸,山本健人,三木 明,近藤正人,小森 淳二,瓜生原健嗣,橋田裕毅,小林裕之,貝原 聡,細谷 亮:抗凝固・抗血小板薬内服症例に対する腹腔 鏡下鼠径ヘルニア修復術の治療方針.第13回日本ヘルニア学会,名古屋,2015. 5. 22-23
- 瓜生原健嗣,貝原 聡,増井秀行,喜多亮介,阪本裕亮,木下裕光,岡田和幸,山本健人,三木 明,近藤 正人,小森淳二,橋田裕毅,小林裕之,細谷 亮:当院におけるアルコール性肝硬変に対する生体肝移植の 実際.第33回肝移植研究会,神戸,2015. 5. 28-29
- 小森淳二:異所性肝細胞移植による生体内肝組織・臓器創世.第22回肝細胞研究会,米子,2015. 6. 4-5
- Uryuhara K,Masui H,Kita R,Sakamoto Y,Kinoshita H,Yamamoto T,Okada K,Miki A,Kondo M, Komori J,Hashida H,Kobayashi H,Kaihara S,Hosotani R:Analysis of secondary resection for incidental gallbladder cancer.第27回肝胆膵外科学会,東京,2015. 6. 11-13
- Kinoshita H,Kaihara S,Kitano S,Kumata Y,Kita R,Masui H,Sakamoto Y,Iwamura S,Mizumoto M, Kondo M,Komori J,Uryuhara K,Kobayashi H,Hashida H,Hosotani R:Current status of central hepatectomy in our hospital.第27回肝胆膵外科学会,東京,2015. 6. 11-13
- Sakamoto Y,Kaihara S,Kita R,Masui H,Kinoshita H,Okada K,Yamamoto T,Miki A,Kondo M, Komori J,Uryuhara K,Kobayashi H,Hashida H,Hosotani R:Feasibility of standardization of distal pancreatectomy for prevention of pancreatic fistula.第27回肝胆膵外科学会,東京,2015. 6. 11-13
- Komori J,Uryuhara K,Hashida H,Kaihara S,Hosotani R:A strategy for the leakage from pancreaticojejunostomy in soft pancreas cases using the modified Blumgart method.第27回肝胆膵外科学 会,東京,2015. 6. 11-13
- Kaihara S,Yagi S,Hashida H,Uryuhara K,Hosotani R:Treatment strategy for multiple liver metastasis from colo-rectal cancer.第27回肝胆膵外科学会,東京,2015. 6. 11-13
- 山本健人,小林裕之,近藤正人,北野翔一,熊田有希子,喜多亮介,増井秀行,阪本裕亮,岩村宣亜,水本 素子,小森淳二,瓜生原健嗣,橋田裕毅,小林裕之,貝原 聡,細谷 亮:急性胆嚢炎に対する腹腔鏡下胆 嚢摘出術の検討.第27回肝胆膵外科学会,東京,2015. 6. 11-13
- 岩村宣亜,飯田 拓,寺嶋宏明,松原弘侑,後藤 徹,井上善景,吉冨摩美,内田洋一朗,上田修吾,金澤 旭宣:膵頭部領域腫瘍に対する術前胆道ドレナージと周術期合併症への影響.第27回肝胆膵外科学会,東京, 2015. 6. 11-13
- 瓜生原健嗣,繁平清美,佐久間美佐緒,水本美也子,平田智香,奥貞 智,片山悌代,石田美智子:医師業 務に対する入院前検査センターの補助的役割に関する現状と課題.第17回医療マネジメント学会,大阪, 2015. 6. 12-13
- 阪本裕亮,貝原 聡,喜多亮介,増井秀行,木下裕光,岡田和幸,山本健人,三木 明,近藤正人,小森淳二, 瓜生原健嗣,橋田裕毅,小林裕之,細谷 亮:術前放射線化学療法後に腹腔動脈合併尾側膵切除を行いR0をなし得た局所進行膵癌の1例.第46回日本膵臓学会,名古屋,2015. 6. 19-20
- 木下裕光,近藤正人,北野翔一,熊田有希子,喜多亮介,増井秀行,阪本裕亮,岩村宣亜,水本素子,小森 淳二,瓜生原健嗣,橋田裕毅,小林裕之,貝原 聡,細谷 亮:当院における腹腔鏡下膵体尾部切除術の導 入と成績.第46回日本膵臓学会,名古屋,2015. 6. 19-20
- Komori J,Fontes P,Lagasse E:Liver tissue engineering in swine lymph nodes by cell transplantation. ISCCR2015 ,Stockholm,2015. 6. 24-27
- 小林裕之,近藤正人,岡田和幸,山本健人,木下裕光,阪本裕亮,喜多亮介,増井秀行,細谷 亮,貝原 聡: 喉頭切除後の胸部食道癌に対する胸腔鏡下食道切除・胸腔内吻合.第69回日本食道学会,横浜,2015. 7. 2-3
- 近藤正人,喜多亮介,増井秀行,木下裕光,阪本裕亮,瓜生原健嗣,橋田裕毅,小林裕之,貝原 聡,細谷 亮:食道癌におけるDCFを用いた術前化学療法.第69回日本食道学会,横浜,2015. 7. 2-3
- 貝原 聡,岡田和幸,喜多亮介,木下裕光,阪本裕亮,山本健人,小森淳二,瓜生原健嗣,細谷 亮:肝切 除安全性向上に向けた工夫と術式定型化の試み.第70回日本消化器外科学会,浜松,2015. 7. 15-17
- 小林裕之,近藤正人,岡田和幸,山本健人,木下裕光,阪本裕亮,喜多亮介,増井秀行,細谷 亮,貝原 聡: 胸骨上縁切除を併用した胸腔鏡下食道亜全摘.第70回日本消化器外科学会,浜松,2015. 7. 15-17
- 橋田裕毅,喜多亮介,増井秀行,木下裕光,阪本裕亮,三木 明,近藤正人,小林裕之,細谷 亮,貝原 聡: クローン病に対する周術期抗TNF-α抗体治療の検討.第70回日本消化器外科学会,浜松,2015. 7. 15-17
- 小森淳二,喜多亮介,増井秀行,阪本裕亮,木下裕光,岩村宣亜,水本素子,近藤正人,瓜生原健嗣,橋田 裕毅,小林裕之,貝原 聡,細谷 亮:当院におけるBorderline resectable膵癌の治療戦略.第70回日本消化 器外科学会,浜松,2015. 7. 15-17
- 近藤正人,増井秀行,喜多亮介,阪本裕亮,木下裕光,山本健人,岡田和幸,橋田裕毅,貝原 聡,細谷 亮: Laparoscopic Complete Mesocolic Excision through Total Medial Approach for Advanced Colon Cancer.第 70回日本消化器外科学会,浜松,2015. 7. 15-17
- 水本素子,岡部 寛,田中英治,角田 茂,平井健次郎,塩田哲也,坂井義治:腹腔鏡下胃全摘術における Linear Staplerを用いた再建法.第70回日本消化器外科学会,浜松,2015. 7. 15-17
- 三木 明,小森淳二,喜多亮介,増井秀行,阪本裕亮,木下裕光,岩村宣亜,水本素子,近藤正人,瓜生原 健嗣,橋田裕毅,小林裕之,貝原 聡,細谷 亮:胃外科領域における手術手技の工夫.第70回日本消化器 外科学会,浜松,2015. 7. 15-17
- 岡田和幸,三木 明,小森淳二,喜多亮介,増井秀行,阪本裕亮,木下裕光,岩村宣亜,水本素子,近藤正人, 瓜生原健嗣,橋田裕毅,小林裕之,貝原 聡,細谷 亮:内視鏡腹腔鏡併用手術治療の工夫、注意点.第70 回日本消化器外科学会,浜松,2015. 7. 15-17
- 山本健人,橋田裕毅,喜多亮介,増井秀行,木下裕光,阪本裕亮,岡田和幸,近藤正人,細谷 亮,貝原 聡: 内側アプローチを主体とした「はさみうち郭清」による安全かつ至適な腹腔鏡下横行結腸切除術.第70回日 本消化器外科学会,浜松,2015. 7. 15-17
- Kinoshita H,Miki A,Kita R,Masui H,Sakamoto Y,Kaihara S,Hosotani R:Current status of No.13 lymph node dissection in our hospital.第70回日本消化器外科学会,浜松,2015. 7. 15-17
- 喜多亮介,小森淳二,北野翔一,熊田有希子,増井秀行,木下裕光,阪本裕亮,水本素子,近藤正人,瓜生原 健嗣,小林裕之,橋田裕毅,貝原 聡,細谷 亮:Our Strategy for pancreaticojejunostomy.第70回日本消 化器外科学会,浜松,2015. 7. 15-17
- 増井秀行,貝原 聡,喜多亮介,阪本裕亮,木下裕光,岡田和幸,山本健人,三木 明,近藤正人,小森淳二, 瓜生原健嗣,橋田裕毅,小林裕之,細谷 亮:Monopolar電極を用いたラジオ波前凝固法による肝実質切離の 有用性の検討.第70回日本消化器外科学会,浜松,2015. 7. 15-17
- 大森彩加,橋田裕毅,喜多亮介,増井秀行,木下裕光,阪本裕亮,岡田和幸,近藤正人,細谷 亮,貝原 聡: 骨形成性大腸癌の1例.第70回日本消化器外科学会,浜松,2015. 7. 15-17
- 岩村宣亜,金澤旭宣,松原弘侑,後藤 徹,井上善景,吉冨摩美,飯田 拓,上田修吾,寺嶋宏明:当科に おける大腸癌イレウスに対する治療戦略~Self-Expanding Metal Stent:SEMS導入前後での短期成績の推 移~.第70回日本消化器外科学会,浜松,2015. 7. 15-17
- 岩村宣亜,内田洋一朗,寺嶋宏明,後藤 徹:頻回の局所治療後に門脈腫瘍栓の急速進展を来した肝細胞癌 の1例~手術の妥当性と適切な残肝再発の制御法とは~.第51回日本肝癌研究会,神戸,2015. 7. 23-24
- Mizumoto M,Tsunoda S,Tanaka E,Hirai K,Shiota T,Sakai Y:Esophagojejunostomy using linear stapler in laparoscopic total gastrectomy.World Congress of Surgery,Thailand,2015. 8. 22-27
- Mizumoto M,Shinohara H,Okabe H,Tsunoda S,Hisamori S,Kaihara S,Sakai Y:The usefulness of staging laparoscopy for advanced gastric cancer.ELSA2015,Daegu,Korea,2015. 9. 2-5
- Uryuhara K,Kaihara S:Successful protocol with rituximab in adult living donor liver transplantation across ABO barrier.European Society for Organ Transplantation(ESOT),Brussels,Belgium,2015. 9. 13-16
- 木下裕光,近藤正人:腹腔鏡補助下幽門側胃切除における郭清手技.京都臨床外科セミナー,京都,2015. 9. 26
- 瓜生原健嗣,貝原 聡,上田浩之:生体肝移植後に十二指腸潰瘍が肝動脈に穿破して出血性ショックとなり IVRと手術で救命しえた一例.第51回日本移植学会,熊本,2015. 10. 1-3
- Kobayashi H,Kondo M,Kaihara S:Lifting Technique in the Thoracoscopic Esophagectomy Makes Lymphadenectomy Along the Left Recurrent Laryngeal Nerve Easier.ACS2015,Chicago,2015. 10. 4-8
- Kondo M,Hashida H,Kaihara S:Total Medial Approach with Pincers Movement for Laparoscopic Complete Mesocolic Excision of Advanced Transverse Colon Cancer.ACS2015,Chicago,2015. 10. 4-8
- Masui H,Kaihara S:Usefulness of remnant liver function using 99m-Tc SPECT CT to estimate the future liver function after hepatectomy.ACS2015,Chicago,2015. 10. 4-8
- 増井秀行,瓜生原健嗣,喜多亮介,阪本裕亮,木下裕光,岡田和幸,山本健人,三木 明,近藤正人,小森 淳二,橋田裕毅,小林裕之,貝原 聡,細谷 亮:副胆嚢管の1例.第13回日本消化器外科学会,東京,2015. 10. 8-11
- Sakamoto Y,Kondo M,Yamamoto T,Kinoshita H,Kita R,Masui H,Komori J,Hashida H,Kobayashi H,Uryuhara K,Kaihara S,Hosotani R:Efficacy of a Modified Fletcher classification for Gastrointestinal Stromal Tumors.ACG2015,Waikiki,2015. 10. 16-21
- Kinoshita H,Sakamoto Y,Kaihara S,Hosotani R:Clinical Outcomes for Interval Appendectomy in the Treatment of Acute Appendicitis with an appendiceal abscess or mass.ACG2015,Waikiki,2015. 10. 16-21
- Kita R,Hashida H,Kaihara S,Hosotani R:Clinical Outcome of Colonic Neuroendocrine Neoplasms. ACG2015,Waikiki,2015. 10. 16-21
- 熊田有希子,近藤正人,北野翔一,喜多亮介,増井秀行,木下裕光,阪本裕亮,岩村宣亜,貝原 聡,細谷 亮:糞石症例を含めたInterval appendectomyの適応とその成績.第43回救急医学会,東京,2015. 10. 21-23
- 橋田裕毅,北野翔一,熊田有希子,増井秀行,喜多亮介,木下裕光,阪本裕亮,岩本宣亜,水本素子,小森 淳二,近藤正人,瓜生原健嗣,小林裕之,細谷 亮,貝原 聡:大腸神経内分泌腫瘍に対する外科治療の現 状と展望.第53回癌治療学会,京都,2015. 10. 29-31
- 北野翔一,橋田裕毅,熊田有希子,喜多亮介,増井秀行,阪本裕亮,木下裕光,岩本宣亜,水本素子,近藤 正人,小森淳二,瓜生原健嗣,小林裕之,貝原 聡,細谷 亮:Trastuzumab+XP療法を施行したHER2陽性 進行胃癌に対してadjuvant surgeryを行った1例.第53回癌治療学会,京都,2015. 10. 29-31
- Hashida H,Kumata Y,Kitano S,Masui H,Kita R,Sakamoto Y,Kinoshita H,Iwamura S,Kondo M, Hosotani R,Kaihara S:Standardization of laparoscopic Left Colectomy by 4 Directional approach to Mobilize Splenic Flexure.10th ISLCRS,Singapore,2015. 11. 5-6
- Hashida H,Kumata Y,Kitano S,Masui H,Kita R,Sakamoto Y,Kinoshita H,Iwamura S,Mizumoto M, Kondo M,Kobayashi H,Hosotani R,Kaihara S:Laparoscopic Rectopexy for Rectal prolapse and Pelvic Organ Dysfunction.10th ISLCRS,Singapore,2015. 11. 5-6
- 阪本裕亮,近藤正人,北野翔一,熊田有希子,喜多亮介,増井秀行,木下裕光,岩本宣亜,水本素子,小森 淳二,瓜生原健嗣,小林裕之,橋田裕毅,貝原 聡,細谷 亮:当院における腹腔鏡下幽門側胃切除と幽門 保存胃切除における栄養障害への影響.第45回胃外科・術後障害研究会,新潟,2015. 11. 7
- 近藤正人,北野翔一,熊田有希子,増井秀行,喜多亮介,阪本裕亮,木下裕光,岩本宣亜,貝原 聡,細谷 亮:腹腔鏡胃切除術の郭清操作における電気メスの有用性.第45回胃外科・術後障害研究会,新潟,2015. 11. 7
- 橋田裕毅,石黒めぐみ,滝口伸浩,尾嶋 仁,杉原健一:高齢者に対する結腸癌術後補助化学療法:ACTS-CC trial年齢別解析.第70回大腸肛門病学会,名古屋,2015. 11. 13-14
- 岩村宣亜,貝原 聡:出血しない肝実質切離法:ソフト凝固によるpre-coagulation dissection technique.第 9回肝臓内視鏡外科研究会,福岡,2015. 11. 25
- 橋田裕毅,北野翔一,熊田有希子,増井秀行,喜多亮介,阪本裕亮,木下裕光,岩本宣亜,水本素子,近藤 正人,小森淳二,瓜生原健嗣,小林裕之,細谷 亮,貝原 聡:腹腔鏡下直腸切除術における吻合部補強縫 合の縫合不全防止効果の検討.第77回臨床外科学会,福岡,2015. 11. 26-28
- 北野翔一,貝原 聡,熊田有希子,喜多亮介,増井秀行,阪本裕亮,木下裕光,岩本宣亜,水本素子,近藤 正人,小森淳二,瓜生原健嗣,小林裕之,橋田裕毅,細谷 亮:緊急手術を施行した鼠径部ヘルニア嵌頓の 2例.第77回臨床外科学会,福岡,2015. 11. 26-28
- 熊田有希子,小林裕之,北野翔一,喜多亮介,増井秀行,木下裕光,阪本裕亮,岩村宣亜,貝原 聡,細谷 亮:胆嚢悪性リンパ腫の1例.第77回臨床外科学会,福岡,2015. 11. 26-28
- 木下裕光,近藤正人:膿瘍・腫瘤形成性虫垂炎に対するInterval Appendectomyの有用性の検討.平成27度京 都大学外科冬期研究会,京都,2015. 12. 5
- 貝原 聡,瓜生原健嗣,小森淳二,岩村宣亜,北野翔一,熊田有希子,喜多亮介,増井秀行,木下裕光,阪本 裕亮,水本素子,近藤正人,小林裕之,橋田裕毅,細谷 亮:出血しない肝実質切離法:ソフト凝固による pre-coagulation dissection technique.第28回内視鏡外科学会,大阪,2015. 12. 10-12
- 小林裕之,近藤正人,岩村宣亜,木下裕光,阪本裕亮,喜多亮介,北野翔一,熊田有希子,橋田裕穀,小森 淳二,水本素子,貝原 聡,細谷 亮:食道栄養血管から考える左上縦隔郭清手技.第28回内視鏡外科学会, 大阪,2015. 12. 10-12
- 橋田裕毅,近藤正人,北野翔一,熊田有希子,喜多亮介,増井秀行,阪本裕亮,木下裕光,岩本宣亜,水本 素子,小森淳二,瓜生原健嗣,小林裕之,細谷 亮,貝原 聡:横行結腸癌に対する内側アプローチを中心 とした腹腔鏡手術の定型化.第28回内視鏡外科学会,大阪,2015. 12. 10-12
- 近藤正人,北野翔一,熊田有希子,増井秀行,喜多亮介,木下裕光,阪本裕亮,水本素子,小森淳二,瓜生原 健嗣,小林裕之,橋田裕毅,貝原 聡,細谷 亮:D2郭清につながる胃切除郭清時の展開 研修医でも安全確 実に.第28回内視鏡外科学会,大阪,2015. 12. 10-12
- 水本素子,近藤正人,木下裕光,岩村宣亜,小森淳二,橋田裕毅,小林裕之,貝原 聡,細谷 亮:当院に おける胃粘膜下腫瘍に対する腹腔鏡下手術・腹腔鏡内視鏡合同手術の経験.第28回内視鏡外科学会,大阪, 2015. 12. 10-12
- 岩村宣亜,貝原 聡,北野翔一,熊田有希子,増井秀行,喜多亮介,木下裕光,阪本裕亮,水本素子,小森 淳二,瓜生原健嗣,小林裕之,橋田裕毅,細谷 亮:当科における腹腔鏡下肝部分切除術への取り組み~安 全・確実な切離を目指して~.第28回内視鏡外科学会,大阪,2015. 12. 10-12
- 木下裕光,北野翔一,熊田有希子,喜多亮介,増井秀行,阪本裕亮,岩本宣亜,水本素子,近藤正人,小森 淳二,瓜生原健嗣,小林裕之,橋田裕毅,貝原 聡,細谷 亮:専攻医による腹腔鏡下胃切除術におけるリ ンパ節郭清の難しさ.第28回内視鏡外科学会,大阪,2015. 12. 10-12
- 阪本裕亮,近藤正人,北野翔一,熊田有希子,喜多亮介,増井秀行,木下裕光,岩本宣亜,水本素子,小森 淳二,瓜生原健嗣,小林裕之,橋田裕毅,貝原 聡,細谷 亮:腹腔鏡下膵体尾部切除の定型化の工夫.第 28回内視鏡外科学会,大阪,2015. 12. 10-12
- 喜多亮介,橋田裕毅,北野翔一,熊田有希子,増井秀行,木下裕光,阪本裕亮,水本素子,近藤正人,小森 淳二,瓜生原健嗣,小林裕之,貝原 聡,細谷 亮:腹腔鏡補助下右側結腸切除術における203番リンパ節郭 清.第28回内視鏡外科学会,大阪,2015. 12. 10-12
- 北野翔一,瓜生原健嗣,熊田有希子,喜多亮介,増井秀行,阪本裕亮,木下裕光,岩本宣亜,水本素子,近藤 正人,小森淳二,小林裕之,橋田裕毅,貝原 聡,細谷 亮:当院における腹腔鏡下ヘルニア修復術(TAPP) の標準化に対する取り組み.第28回内視鏡外科学会,大阪,2015. 12. 10-12
- 熊田有希子,小林裕之,北野翔一,喜多亮介,増井秀行,木下裕光,阪本裕亮,岩村宣亜,貝原 聡,細谷 亮:急性胆嚢炎に対する腹腔鏡下胆嚢摘出術の当院における現状 TG13の妥当性.第28回内視鏡外科学会, 大阪,2015. 12. 10-12
- 近藤正人,増井秀行,喜多亮介,阪本裕亮,木下裕光,岩本宣亜,熊田有希子,北野翔一,貝原 聡,細谷 亮:腹腔鏡での機能温存を追求した膵体尾部切除術.膵臓内視鏡外科研究会,京都,2015. 12. 13
- 阪本裕亮,近藤正人,北野翔一,熊田有希子,喜多亮介,増井秀行,木下裕光,岩本宣亜,水本素子,小森 淳二,瓜生原健嗣,小林裕之,橋田裕毅,貝原 聡,細谷 亮:腹腔鏡下膵体尾部切除術における膵液瘻予 防に対する取り組み.膵臓内視鏡外科研究会,京都,2015. 12. 13
- 岩村宣亜,貝原 聡:Pancreatoduodenectomy with portal vein resection for locally advanced pancreatic head cancer.第13回兵庫手術手技ビデオカンファレンス,神戸,2016. 1. 23
- 橋田裕毅,貝原 聡,近藤正人,三木 明,小森淳二,瓜生原健嗣,小林裕之,細谷 亮:当院における大 腸癌手術の現状.第15回神戸市東灘区医師会病診連携学術集談会,神戸,2016. 2. 21
- 橋田裕毅,熊田有希子,北野翔一,喜多亮介,増井秀行,木下裕光,阪本裕亮,岩本宣亜,水本素子,近藤 正人,小森淳二,瓜生原健嗣,小林裕之,細谷 亮,貝原 聡:大腸神経内分泌腫瘍に対する治療の現状と 展望.第12回日本消化管学会,東京,2016. 2. 26-27
- Kaihara S,Iwamura S,Kumata Y,Kitano S,Masui H,Kita R,Sakamoto Y,Kinoshita H,Mizumoto M, Kondo M,Komori J,Uryuhara K,Kobayashi H,Hashida H,Hosotani R:Parenchymal dissection technique in laparoscopic hepatectomy.SAGES2016,Boston,2016. 3. 16-19
- Iwamura S,Kaihara S,Kumata Y,Kitano S,Masui H,Kita R,Sakamoto Y,Kinoshita H,Mizumoto M, Kondo M,Komori J,Uryuhara K,Kobayashi H,Hashida H,Hosotani R:Management of laparoscopic partial hepatectomy for cranial and dorsal lesions in our department.SAGES2016,Boston,2016. 3. 16-19
- 水本素子,近藤正人,木下裕光,岩村宣亜,小森淳二,橋田裕毅,小林裕之,貝原 聡,細谷 亮:Delleを 伴うGISTに対する腹腔鏡内視鏡合同手術の工夫.第86回日本胃癌学会,東京,2016. 3. 17-19
- Resection strategy for colorectal liver metastasis focusing on intrahepatic vessels and resection margins. Iwaki K, Kaihara S, Kitamura K, Uryuhara K. Surg Today. 2021 Mar 6.
- 空腸漿膜パッチおよび十二指腸憩室化にて救命しえた広範な外傷性十二指腸損傷の1例 近藤正人(神戸市立医療センター中央市民病院 外科), 貝原聡.日本救急医学会雑 誌 (0915-924X)32巻2号 Page116-119(2021.02)
- Usefulness and Cost-effectiveness of Interval appendectomy for Complicated Appendicitis. Ryosuke Kita, Hiroki Hashida, Daisuke Yamashita, Hiromitsu Kinoshita, Masato Kondo, Satoshi Kaihara. Journal of Surgery 2021; 9(3): 109-113
- A case report of intersigmoid hernia treated using laparoscopic surgery. Hiroyuki Kambe, Koji Kitamura, Satoshi Kaihara. Int J Surg Case Rep. 2021 Apr;81:105822.
- Resection strategy for colorectal liver metastasis focusing on intrahepatic vessels and resection margins. Kentaro Iwaki, Satoshi Kaihara, Koji Kitamura, Kenji Uryuhara .Surg Today. 2021 Mar 6. doi: 10.1007/s00595-021-02254-0.
- QOL assessment after palliative surgery for malignant bowel obstruction caused by peritoneal dissemination of gastric cancer: a prospective multicenter observational study. Yuichi Ito , Kazumasa Fujitani , Kentaro Sakamaki , Masahiko Ando , Ryohei Kawabata , Yutaka Tanizawa , Takaki Yoshikawa , Takanobu Yamada , Motohiro Hirao 8, Makoto Yamada , Jun Hihara , Ryoji Fukushima , Yasuhiro Choda , Yasuhiro Kodera , Shin Teshima, Hisashi Shinohara, Masato Kondo. Gastric Cancer. 2021 Mar 31. doi: 10.1007/s10120-021-01179-4. Online ahead of print
- 虫垂炎手術 膿瘍形成性虫垂炎に対する待機的腹腔鏡下虫垂切除術.水野 良祐, 貝原 聡:手術(0037-4423)75巻4号 Page417-423(2021.04)
- Cause of recurrent laryngeal nerve paralysis following esophageal cancer surgery and preventive surgical technique along the left recurrent laryngeal nerve. Kobayashi, H., Kondo, M., Kita, R., Hashida, H., Shiokawa, K., Iwaki, K., Kambe, H., Mizuno, R., Kawarabayashi, T., Sumi, T., Kaihara, S., Hosotani, R. Mini-invasive Surg 30 (4) 2020
- Survival analysis of a prospective multicenter observational study on surgical palliation among patients receiving treatment for malignant gastric outlet obstruction caused by incurable advanced gastric cancer. Terashima M, Fujitani K, Ando M, Sakamaki K, Kawabata R, Ito Y, Yoshikawa T, Kondo M, Kodera Y, Kaji M, Oka Y, Imamura H, Kawada J, Takagane A, Shimada H, Tanizawa Y, Yamanaka T, Morita S, Ninomiya M, Yoshida K. Gastric Cancer. 2021 Jan;24(1):224-231.
- Changes in the sexual function of male patients with rectal cancer over a 2-year period from diagnosis to 24-month follow-up: A prospective, multicenter, cohort study. Sakamoto T, Hida K, Hoshino N, Yamaguchi T, Manaka D, Yamada M, Kadokawa Y, Yamanokuchi S, Kondo M, Kanazawa A, Abe H, Okada T, Morita S, Sakai Y.J Surg Oncol. 2020 Dec;122(8):1647-1654.
- 傍ストーマヘルニアの診断と治療.橋田裕毅.消化器外科43巻7号 Page1151-1160(2020.06)
- Laparoscopic Surgery for Colorectal Cancer in Super-Elderly Patients: A Single-Center Analysis. Hashida H, Mizuno R, Iwaki K, Kanbe H, Sumi T, Kawarabayashi T, Kondo M, Kobayashi H, Kaihara S. Surg Laparosc Endosc Percutan Tech. 2020 Nov 23;31(3):337-341.
- Laparoscopic Colectomy for Splenic Flexure Cancer Approached from Four Directions. Hashida H, Kondo M, Kita R, Kitamura K, Uryuhara K, Kobayashi H, Kaihara S. J Laparoendosc Adv Surg Tech A. 2020 Nov 23. doi: 10.1089/lap.2020.0709. Online ahead of print.
- Internal hernia of the stomach associated with colostomy after laparoscopic surgery for rectal cancer: a case report. Hashida H, Kita R, Kondo M, Mizuno R, Kobayashi H, Kaihara S. Surg Case Rep. 2020 Dec; 6: 127.
- Diaphragm disease associated with nonsteroidal anti-inflammatory drugs mimicking intestinal tumor: A case report. Mori A, Hashida H, Kitamura K, Matsui J, Mizuno R, Tanigawa Y, Izumi A, Ishida S, Yamashita D, Yamaguchi T, Kaihara S. Int J Surg Case Rep. 2020;76:121-124.
- Analysis of the Outcome of Laparoscopic Repair for Parastomal Hernia Using the Sandwich Technique. Hiroki Hashida, Yukiko Kumata, Masato Kondo, Hiroyuki Kobayashi, Satoshi Kaihara. Indian Journal of Surgery. 83, pages542–546 (2021) Published: 27 May 2020
- Complete Response of Locally Advanced Gastric Cancer with Pancreatic Invasion and Gastric Outlet Obstruction after Neoadjuvant Chemotherapy with S-1 and Oxaliplatin. Kondo M, Nishino S, Yamashita D, Kaihara S. Case Rep Oncol. 2020 Jun 24;13(2):716-720. doi: 10.1159/000507983. eCollection 2020 May-Aug.
- Conversion to complete resection with mFOLFOX6 with bevacizumab or cetuximab based on K-RAS status for unresectable colorectal liver metastasis (BECK study): Long-term results of survival. Okuno M, Hatano E, Toda R, Nishino H, Nakamura K, Ishii T, Seo S, Taura K, Yasuchika K, Yazawa T, Zaima M, Kanazawa A, Terajima H, Kaihara S, Adachi Y, Inoue N, Furumoto K, Manaka D, Tokuka A, Furuyama H, Doi K, Hirose T, Horimatsu T, Hasegawa S, Matsumoto S, Sakai Y, Uemoto S. J Hepatobiliary Pancreat Sci. 2020 Aug;27(8):496-509. doi: 10.1002/jhbp.747. Epub 2020 Jun 9.
- Successful Treatment of a Mixed Neuroendocrine-Nonneuroendocrine Neoplasm of the Colon with Metastases to the Thyroid Gland and Liver. Kanazawa Y, Kikuchi M, Imai Y, Katakami N, Kaihara S, Shinohara S. Case Rep Otolaryngol. 2020 Feb 13;2020:5927610. doi: 10.1155/2020/5927610. eCollection 2020.
- 下部消化管穿孔の手術.塩川 桂一, 貝原 聡:消化器外科(0387-2645)43巻5号 Page664-668(2020.04)
- Transperineal abdominoperineal resection for anorectal melanoma: A case report.Hiroki Hashida, Masato Kondo, Daisuke Yamashita, Shigeo Hara, Ryosuke Mizuno, Motoko Mizumoto, Hiroyuki Kobayashi, Satoshi Kaihara. Int J Surg Case Rep 61:214-217,2019
- Usefulness of laparoscopic posterior rectopexy for complete rectal prolapse: A cohort study.Hiroki Hashida, Masato Sato, Yukiko Kumata, Motoko Mizumoto, Masato Kondo, Hiroyuki Kobayashi, Takehito Yamamoto, Hiroaki Terajima, Satoshi Kaihara. Int J Surg 72:109-114,2019
- Hepatic Anisakiasis Mimicking Metastatic Liver Tumour.Ryosuke Kita, Hiroki Hashida, Kenji Uryuhara, Satoshi Kaihara. Int J Surg Case Rep 60:209-212,2019
- Chronic rejection after intestinal transplantation: A systematic review of experimental models.Koji Kitamura, Bettina M Buchholz, Kareem Abu-Elmagd, Joerg C Kalff, Nico Schafer, Martin W von Websky. Transplant Rev (Orlando) 33:173-181,2019
- 当院で経験したラジオ波焼灼術後横隔膜ヘルニア の2例.増井秀行,瓜生原健嗣,喜多亮介,近藤正人,貝原聡.日本ヘルニア学会誌 5:17-25,2019
- 膿瘍形成性虫垂炎を併発した盲腸癌に対して腹腔鏡手術を施行した1例.増井秀行,小林裕之,瓜生原健嗣,貝原聡,細谷亮.外科 81:155-161,2019
- Observational study of first-line chemotherapy including cetuximab in patients with metastatic colorectal cancer: CORAL trial. Muro K, Itabashi M, Hashida H, Masuishi T, Bando H, Denda T, Yamanaka T, Ohashi Y, Sugihara K. Jpn J Clin Oncol. 2019 Apr 1;49(4):339-346.
- Linear or circular stapler? A propensity score-matched, multicenter analysis of intracorporeal esophagojejunostomy following totally laparoscopic total gastrectomy. Murakami K, Obama K, Tsunoda S, Hisamori S, Nishigori T, Hida K, Kanaya S, Satoh S, Manaka D, Yamamoto M, Kadokawa Y, Itami A, Okabe H, Hata H, Tanaka E, Yamashita Y, Kondo M, Hosogi H, Hoshino N, Tanaka S, Sakai Y. Surg Endosc. 2020 Dec;34(12):5265-5273.
- Safety and effectiveness of FOLFOXIRI plus molecular target drug therapy for metastatic colorectal cancer: A multicenter retrospective study.Ogata T, Satake H, Ogata M, Hatachi Y, Maruoka H, Yamashita D, Hashida H, Hamada M, Yasui H. Oncotarget. 2019 Feb 1;10(10):1070-1084.
- 当院における腫瘤形成性虫垂炎に対するinterval appendectomyプロトコルの有用性の検討.木下裕光,近藤正人,山本健人,貝原聡. 日本内視鏡外科学会雑誌 (1344-6703)24巻3号 Page206-213(2019.05)
- ALPlat criterion for the resection of hepatocellular carcinoma based on a predictive model of posthepatectomy liver failure. Yamamoto G, Taura K, Ikai I, Fujikawa T, Nishitai R, Kaihara S, Zaima M, Terajima H, Yoshimura T, Koyama Y, Tanabe K, Nishio T, Okuda Y, Ikeno Y, Yoshino K, Fukuyama K, Seo S, Hatano E, Uemoto S. Surgery. 2020 Feb;167(2):410-416. doi: 10.1016/j.surg.2019.09.021. Epub 2019 Nov 11.
- 妊婦の虫垂炎に対する腹腔鏡下虫垂切除術.熊田有希子,貝原 聡,細谷 亮.手術 72:1241-1247,2018
- Prevalence and risk factors of hepatitis B virus reactivation in patients with solid tumors with resolved HBV infection. Kotake T, Satake H, Okita Y, Hatachi Y, Hamada M, Omiya M, Yasui H, Hashida T, Kaihara S, Inokuma T, Tsuji A.Asia Pac J Clin Oncol. 15: 63-68, 2018
- Technique and surgical outcomes of mesenterization and intra-operative neural monitoring to reduce recurrent laryngeal nerve paralysis after thoracoscopic esophagectomy: A cohort study. Kobayashi H, Kondo M, Mizumoto M, Hashida H, Kaihara S, Hosotani R. Int J Surg. 56: 301-306, 2018
- Laparoscopic appendectomy during the third trimester: Case presentation and literature review. Iwamura S, Hashida H, Yoh T, Kitano S, Mizumoto M, Kitamura K, Kondo M, Kobayashi H, Kaihara S, Hosotani R. Asian J Endosc Surg. 11: 413-416, 2018
- Updated 5-year survival and exploratory T x N subset analyses of ACTS-CC trial: a randomized controlled trial of S-1 versus tegafur-uracil/leucovorin as adjuvant chemotherapy for stage III colon cancer. Kusumoto T, Ishiguro M, Nakatani E, Yoshida M, Inoue T, Nakamoto Y, Shiomi A, Takagane A, Sunami E, Shinozaki H, Takii Y, Maeda A, Ojima H, Hashida H, Mukaiya M, Yokoyama T, Nakamura M, Munemoto Y, Sugihara K. ESMO Open. 3: e000428, 2018
- 食道・胃の鏡視下手術 腹腔鏡下大網充填術.近藤正人.消化器外科. 41巻5号 Page576-582(2018.04)
- 直腸脱の治療.橋田裕毅. 消化器外科41巻8号 Page1201-1210(2018.07)
- A Case of Cecal Cancer with Heterotopic Ossification. Ayaka Omori, Hiroki Hashida, Satoshi Kaihara. J Med Cases. 2018;9(5):131-134
- Fistula Formation Secondary to Mucinous Appendiceal Adenocarcinoma May Be Related to a Favorable Prognosis: A Case Report and Literature Review. Yokode M, Ikeda E, Matsui Y, Iwamura S, Mikami S, Kobayashi H, Imai Y, Kaihara S, Yamashita Y. Intern Med. 2018 Oct 15;57(20):2945-2949. doi: 10.2169/internalmedicine.0694-17. Epub 2018 Jun 6.
- Clinical factors that affect the outcomes after anatomical versus non-anatomical resection for hepatocellular carcinoma. Yamamoto T, Yagi S, Uryuhara K, Kaihara S, Hosotani R. Surg Today. 2017 Feb;47(2):193-201.
- Phase I Study of Neoadjuvant Chemotherapy with Capecitabine and Oxaliplatin for Locally Advanced Gastric Cancer. Satake H, Kondo M, Mizumoto M, Kotake T, Okita Y, Ogata T, Hatachi Y, Yasui H, Miki A, Imai Y, Ichikawa C, Murotani K, Kotaka M, Kato T, Kaihara S, Tsuji A. Anticancer Res. 2017 Jul;37(7):3703-3710.
- Phase I study of neoadjuvant chemotherapy with S-1 and oxaliplatin for locally advanced gastric cancer (Neo G-SOX PI). Satake H, Miki A, Kondo M, Kotake T, Okita Y, Hatachi Y, Yasui H, Imai Y, Ichikawa C, Murotani K, Hashida H, Kobayashi H, Kotaka M, Kato T, Kaihara S, Tsuji A. ESMO Open. 2017 Mar 9;2(1):e000130.
- A Complete Response Case in a Patient with Multiple Lung Metastases of Rectal Cancer Treated with Bevacizumab plus XELIRI Therapy. Hashida H, Satake H, Kaihara S. Case Rep Oncol. 2017 Jan 17;10(1):81-85.
- 完全直腸脱に対する腹腔鏡下直腸固定術の手技と有用性.橋田裕毅, 熊田有希子, 水本素子, 塩川桂一, 松原孝明, 北野 翔一, 喜多亮介, 増井秀行, 北村好史, 近藤正人, 瓜生原健嗣, 小林裕之, 細谷亮, 貝原聡.日本女性骨盤底医学会誌 (2187-5669)14巻1号 Page84-87(2017.12)
- 妊娠32週目に発症した切迫早産を伴った急性虫垂炎に対して腹腔鏡下虫垂切除術を施行した1例.岩村宣亜, 橋田裕毅, 水本素子, 細谷亮, 貝原聡.日本内視鏡外科学会雑誌 (1344-6703)22巻4号 Page539-544(2017.07)
- Significance of Proper Graft Selection in Adult Living-Donor Liver Transplant Recipients with Preoperative Deteriorated Condition. Iida T, Masuda K, Matsuyama T, Harada S, Nakamura T, Koshino K, Suzuki T, Nobori S, Ushogome H, Ito T, Sakamoto S, Uryuhara K, Okajima H, Kaihara S, Uemoto S, Yoshimura N. Ann Transplant. 2017 Sep 8;22:541-549. doi: 10.12659/aot.904575.
- Biliary Pneumonia due to the Presence of a Bronchobiliary Fistula. Matsumoto T, Otsuka K, Kaihara S, Tomii K. Intern Med. 2017;56(11):1451-1452. doi: 10.2169/internalmedicine.56.8066. Epub 2017 Jun 1.
- Prospective registry for laparoscopic liver resection. Fuji H, Hatano E, Seo S, Arimoto A, Okabe M, Fujikawa T, Nishitai R, Ishii T, Kaihara S, Matsushita T, Oike F, Ichimiya M, Ohta S, Yamanaka K, Taura K, Yasuchika K, Uemoto S. Asian J Endosc Surg. 2017 May;10(2):173-178. doi: 10.1111/ases.12351. Epub 2016 Dec 14.
- 肝切除術. 貝原 聡:消化器外科(0387-2645)40巻4号 Page433-440(2017.04)
- 術中に診断し得た重複胆嚢管の1症例.増井秀行.手術 70:701-706,2016
- Axillobifemoral Bypass for Aortitis Syndrome in a Living-Donor Liver Transplant Patient. Fukunaga N, Uryuhara K, Koyama T. Ann Vasc Dis. 2016;9(2):114-6.
- 造影USが診断に有用であった虫垂粘液癌の一例.南 佳織,荒木直子,岩崎信弘,杤尾人司,鄭 浩柄,杉之下与志樹,橋田裕毅,簑輪和士,今井幸弘,猪熊 哲朗.超音波医学 43:367,201
- Long-term survival after resection of pancreatic cancer:A single-center retrospective analysis.Yamamoto T,Yagi S,Kinoshita H,Sakamoto Y,Okada K,Uryuhara K,Morimoto T,Kaihara S,Hosotani R. World J Gastroenterol 21:262-268,2015
- Comparison between anatomical subsegmentectomy and non-anatomical partial resection for hepatocellular carcinoma located within a single subsegment:a single-center retrospective analysis.Yamamoto T,Yagi S,Kita R,Masui H,Kinoshita H,Sakamoto Y,Okada K,Miki A,Kondo M,Hashida H,Kobayashi H,Uryuhara K,Kaihara S,Hosotani R. Hepatogastroenterology 62:363-367,2015
- Prediction of mortality in patients with colorectal perforation based on routinely available parameters:a retrospective study.Yamamoto T,Kita R,Masui H,Kinoshita H,Sakamoto Y,Okada K,Komori J,Miki A,Uryuhara K, Kobayashi H,Hashida H,Kaihara S,Hosotani R. World J Emerg Surg 10:24, 2015
- The preventive surgical site infection bundle in patients with colorectal perforation.Yamamoto T,Morimoto T,Kita R,Masui H,Kinoshita H,Sakamoto Y,Okada K,Komori J,Miki A, Kondo M,Uryuhara K,Kobayashi H,Hashida H,Kaihara S,Hosotani R. BMC Surg 15:128,2015
- 消化管間葉系腫 瘍の術後再発危険因子とmodified Fletcher分類によるリスク分類の有用性の検討.山本健人,三木 明,岡田和幸,市川千宙,松岡亮介,上原慶一郎,貝原 聡,細谷 亮. 日本消化器外科学会雑誌 48:473-480,2015
当院での研修を考える若手医師へ
当院での外科後期研修を目指す人たちへ
当院は外科専門研修プログラム(プログラム名『兵庫京大外科専門研修プログラム』)の基幹病院です。ここでは『兵庫京大外科専門研修プログラム』についても含め、当院での消化器外科研修の特徴につき説明します。
兵庫京大外科研修プログラムについて
①プログラムの特色
幅広い環境を有する教育施設群
神戸市立医療センター中央市民病院(以下、中央市民病院)を基幹病院とし、兵庫県内の有数の高度急性期病院と救命救急センターを有する7病院(県立尼崎総合医療センター、姫路医療センター、西神戸医療センター、神鋼記念病院、公立豊岡病院、神戸市立医療センター西市民病院、赤穂市民病院)を連携施設として配置する地域医療に配慮した病院群を形成しています。
屈指の手術数
グループ全体で高難度手術を含む年間約1万2000件の手術(内視鏡手術年間約5000件)を行っており、数多くの手術を経験するとともに外科疾患の理解を深めるには極めて恵まれた環境にあります。
専門性の高い指導陣
専門研修指導医数は80名で、消化器外科・心臓血管外科・呼吸器外科・小児外科・乳腺外科のみならず肝胆膵外科高度技能指導医、内視鏡外科技術認定医など専門性の高い指導医陣を配しています。
②採用について
『兵庫京大外科研修プログラム』の採用定員は17名/年です(3年で計51名)。サブスペシャリティーごとの採用定員は設定しておりません。採用は書類審査と面接が行われ決定します。このグループの病院での研修を希望される方は、『兵庫京大外科研修プログラム』に採用されて配属となりますので各病院での採用は行われません。
③研修病院、研修期間
主な研修を行うメイン施設を設定し、そこで少なくとも連続した2年間の外科専門研修を行います。残りの1年の内、半年の基幹病院(中央市民病院)での研修は必須ですが、希望によりさらに半年のメイン施設以外の連携施設での研修も可能です。またこの3年間の中で希望のサブスペシャリティー以外の科目(例えば消化器外科希望であれば、それ以外の心臓・呼吸器・小児・乳腺の各外科)も経験に応じてローテートし専門医に必要な症例数を経験します。
メイン施設の選択は研修医師の希望が最優先されますが、各病院の状況を考慮した上で最終的にはプログラム管理委員会にて決定されます。
④外科専門研修終了後の進路
『兵庫京大外科研修プログラム』終了後は、研修終了医師の希望にて自由に選択が可能です。もし京大系列でのキャリアパスを考えられる場合は、京都大学外科交流センター(消化器外科、乳腺外科)、京都大学呼吸器外科、京都大学心臓血管外科との連携と情報共有を行い、研修終了後も手厚いサポート体制を整えています。またそれ以外にがんセンター、循環器病センター、こども病院などの専門疾患病院での勤務も可能です。現在の神戸市立医療センター中央市民病院外科を例にすると、3年の研修期間が終了した人の約80%が京大系列のキャリアパスを選択されておりますが、残りはそれ以外の様々な進路を選択されています。
ダブルボードを目指す専攻医を対象としたカリキュラム制での採用【NEW!】
新専門医制度において、初めに救急領域の専門研修を修了し、二つ目の基盤領域専門医として外科専門医を取得(ダブルボード)を目指す専攻医の採用も行っています。
ダブルボードとしてのカリキュラム制での専攻医の採用は、プログラム制と同様に書類審査と面接にて決定します。また救急科領域の専門研修開始後2年間のうちに外科学会に入会し、外科領域における専門研修を行う意思を所定の書式で明示された場合は、個別審査の上で研修期間が1年短縮できる場合があります。
詳細は外科学会HPの「新専門医制度におけるダブルボードによる専門研修について」を参照ください。
神戸市立医療センター中央市民病院外科での研修について
それではここからは神戸市立医療センター中央市民病院消化器外科での研修内容について述べていきます。
①臨床現場でのトレーニング
当院での外科研修は、他の病院と比べ実際の手術に携わる割合が非常に高いのが特徴です。具体的には数多くの癌の手術を中心とした定期手術に加え、緊急手術も積極的に行うことで、年間約1100-1200件の手術数を維持しています(症例の詳細は『手術統計』の項を参照ください)。これら手術はスタッフ医師と後期研修医が必ずペアになって担当となり、術前診断と評価、手術、術後管理、手術記録の整理、などマンツーマンに直接指導を受けられる体制をとっています。また手術手技の習熟度を測る指標として独自に開発した手術手技評価システムを採用しており、それに基づいて指導を行います。一方、外科手術と周術期以外の研修は当院では十分に行う体制はありません。例えば、癌の患者さんが不幸にして再発した場合は、化学療法は腫瘍内科が行います。また癌末期の患者さんは緩和ケア部門が担当となります。このように当院の外科は手術とその周術期に特化したトレーニングとなりますので、化学療法や緩和ケアなど当院で不足する分野はローテーション病院で研修を受けることになります。
スタッフの厳しい指導の下で若手医師には積極的に手術を執刀してもらうことにより多くの経験を積んでもらう方針としております。具体的には研修1年目は、まずは胆摘、ヘルニア、開腹手術が中心となり手術の基本手技を習得します。また後半は徐々に悪性疾患の担当医となる機会が増えてきます。2年目になると、消化管の手術の担当となる場合が増え、これら疾患の執刀をする機会が増加します。また肝胆膵疾患も段階を経たのちに担当となり、症例に応じ自ら執刀する機会も増えてきます。これら指導は必ずペアとなるスタッフ医師が責任をもって指導しますが、腹腔鏡手術は内視鏡技術認定医が、肝胆膵手術は肝胆膵外科高度技術指導医・認定医が指導を行う体制をとっています。
他に、救急疾患も数多く経験が可能です。月に約4回の当直時に入院となった外科疾患患者は主治医となり、手術が必要な場合は担当のスタッフの指導のもとで執刀医となり治療にあたります。 これらの臨床経験を積むことにより、外科専門医、消化器外科専門医の必要症例数は容易に達成できます。
②ロボット手術の執刀が可能です【NEW!】
消化器外科領域では、後期研修医はロボット手術は執刀ができない状況でした。しかし2022年にその条件は大幅に緩和され、後期研修医でも一定の条件下でロボット手術が可能となりました。
しかし実際は、手術支援ロボットは非常に高価で複数台の保有は困難であり、よってロボット手術の施設での手術症例数には大きな制限がるがゆえに後期研修が執刀する機会は非常に限られています。さらに後期研修医が執刀できる条件として、その臓器のロボット手術プロクターが常勤医として勤務していることが必須でこの条件を満たす末津は限られています。またロボット手術の上達にはトレーニングがとても重要で、通常は実機に付属するシュミレーターでのトレーニングとしている施設が多いです。しかしその場合臨床で使用している以外の時間しか使用できないため夜間や早朝の練習にならざるを得ず、常に手術室に出向いての練習が必要です。しかし当院は上記の問題に関していち早く様々な対応を取っており、ロボット手術の臨床応用のみならず若手への教育に力を入れてきました。
1)当院は手術支援ロボットを3台有しています。
他の施設に比べロボット手術を数多く行うことが可能で、2023年より後期研修医もロボット手術の執刀を行っています
2)消化器外科でロボット手術が行える臓器すべてにプロクターが常勤しています。
後期研修医は全ての臓器(食道、胃、大腸、直腸、肝臓、膵臓)のロボット手術が執刀可能です。
3)ロボット手術の研修の費用は後期研修医個人の負担なく資格が取得できます。
4)ロボット手術練習機器があります。
当院の外科系Labには、ロボット手術のトレーニングシュミレーター:ロボティックメンターが設置してありますので、後期研修医は手術室に行くことなくDry Labにて好きな時間に好きなだけロボット手術のトレーニングが可能です。
このように、当院の消化器外科では後期研修医がいち早くロボット手術の執刀を行うことが出来るような環境が整っているのは特筆すべき点と言えます。
③Off Siteトレーニング環境が整っています
実際の臨床だけでなく、Dry Labや手術ビデオの編集・クリニックを行うことにより、off siteでのトレーニングも行っております。具体的には複数の外科系診療科共同でDry Labを使用しており、24時間好きな時間に練習が可能な環境が整っています。また手術ビデオは外科医局で一括管理・保存し、いつでも以前の手術ビデオを閲覧することが可能です。また若手医師が編集した手術ビデオをもとにdiscussionをおこなう場としての『ビデオクリニック』を毎月開催しており、これによって手術時のみならずビデオ編集を通じ自分の行った手術のreviewを行い、指導を受け得る環境を整えています。
④積極的に学術活動に参加しています
臨床では解明すべき課題が、いまだ数多くあります。これらを解決する手段の一つとして臨床研究があり、我々も積極的に臨床研究に参加したり独自のプロジェクトを立ち上げています。それぞれのプロジェクトはスタッフ医師に加え必ず後期研修医が担当となり、これらを通じて、論理的な物事の考え方を習得し、文献を読むことによりさらに知識が深まります。また当院で経験した疾患のデータをまとめ解析することにより、新たな知見が得られる可能性もあります。その意味でデータベース管理は非常に重要で、臨床研究と同様にスタッフと若手医師がペアで責任者となります。
そしてこれら研究の発表の場として学会発表に積極的に参加しています。発表内容も初めは症例報告ですが、やがてはデータを解析したまとめの発表が中心となり、スタッフのみならず後期研修医も全国規模学会の上級演題での発表を行ってきました。また海外の学会は、海外の医療を肌で感じるのみならず日本の医療の現状を見つめなおす良い機会と考え、積極的に参加しています。国内の全国規模学会での発表4回、海外の学会での発表は当院在籍中に1回、をスタッフ・後期研修医を問わず各人の目標としており、毎年70題前後の演題を国内外の学会(地方会は除く)で採用され発表を行っています。
⑤働き方改革に向けてのライフワークバランスを考慮した診療体系【NEW】
2024年度より医師の時間外労働上限を年間960時間(月80時間)以下とする、いわゆる「医師の働き方改革」が実施されました。しかし我が国の良質な医療提供体制は、「病院勤務医の献身的な努力」があって成り立っており、とくに外科系は若手医師の労働力に支えられてきました。しかしこのようなライフワークバランスを軽視した労働環境があるがために近年外科志望の医師が減少しており、大きな問題となっております。
当院はいち早くこの問題を重要視しており、今まで様々な改革を行ってきました。その具体例を列記すると、
- 入院患者対応は、主治医制ではなくチーム制をとっています。
- 当直入りの日は、原則15時からの勤務です。また当直明けは必ず翌日12時までに帰宅できる環境を整えています。
- 土日祝日は専攻医当番制としており、3回に1回の出務です。
- 手術は10時、18時に次の当番医と交代し長時間労働を避ける工夫を取っています(緊急手術のみが対象で定期手術は含まれません)。
一方で時間外労働が認められなければ十分な研修ができないという意見もありますが、勤務に余裕を持たせることで通常の勤務内に研修ができるような体制や環境つくりをとるように工夫しています。このように非常にメリハリの利いた研修を行うのも当院の大きな特徴といえます。
最後に
当院での外科研修は、外科手術・周術期に特化した専門的なトレーニングを受けるとこが可能です。またその他にも、専門資格を持ったスタッフによるマンツーマン指導、後期研修医によるロボット手術が可能、Off Siteでの自主的な研修システムの構築、積極的な学術活動、ライフワークバランスを考慮したメリハリの利いた研修、を特徴としています。3年間の研修期間は非常に忙しいですが、各学年2人、3年で計6人の後期研修医はお互い刺激しつつも助け合いながら楽しく研修をしています。
当院での臨床研修に興味を持たれた方、何か質問がある方、は外科部長:貝原(skaihara@kcho.jp)までご連絡ください。そしてぜひ当院の外科研修を見学していただければと思います。
文責:外科部長 貝原聡
お知らせ
医師、医師を目指す方向け当科のご紹介
※本コンテンツは、医師の方を対象とし、当医療機関についての理解を深めていただけるよう作成しているものであり、一般の方を対象とする宣伝・広告等を目的としたものではありません。 はじめまして、神戸市立医療センター中央市民病院 外科・移植外科部長の貝原 聡(かいはら さとし)です。
当科は地域の基幹病院として、胆石症、鼠経ヘルニアなどの良性疾患から、胃癌、大腸癌、肝癌などの悪性疾患まであらゆる消化器疾患に対応しております。また救急疾患については24時間365日対応しております。スタッフ8名と専攻医7名を有し、消化器外科、救急外科、移植外科と幅広い領域において、一般外科、上部消化管外科、下部消化管外科、肝胆膵外科のエキスパートを揃えて診療し、各診療科との連携も迅速かつ強固であり、集約的に治療を行えることも当院の大きな強みとなっています。
大腸癌の国内年間罹患数は、現在15万人を超えており、その治療機会は増加してきています。本日は大腸癌に対しての外科治療と抗癌剤治療について、当院での取り組みの一部をご紹介いたします。大腸の低侵襲手術については、外科医長の橋田 裕毅(はしだ ひろき)が、肝転移に対する手術加療については、外科医長の北村 好史(きたむら こうじ)が、化学化学療法については、腫瘍内科部長の安井 久晃(やすい ひさてる)が担当いたします。
貝原 聡
院長補佐
外科・移植外科 部長
大腸癌に対する低侵襲手術適応範囲の広さと術後合併症の成績に強み
外科・移植外科 医長
橋田 裕毅(はしだ ひろき)
専門分野
消化器外科、大腸外科、内視鏡外科
学会専門医・認定医
日本外科学会専門医・指導医
日本消化器外科学会専門医・指導医
内視鏡外科学会技術認定医 など
大腸癌に対しての当外科の最大の特徴は、低侵襲アプローチと腫瘍学的アプローチの両立を目指しているところです。従来から腹腔鏡手術を積極的に取り入れており、その件数は増加してきており、9割近くになります。
低侵襲で質の高い手術を提供できるように取り組んでおり、また、高齢者や肥満者も腹腔鏡手術の適応外とはせず、開腹手術既往者も癒着に注意して腹腔鏡手術を行っています。全身状態(心・肺・肝・腎機能など)不良者でも全身麻酔が可能であれば適応とし、さらに巨大腫瘍、他臓器浸潤などの一部以外も腹腔鏡手術の適応とし、日本内視鏡外科学会技術認定医を中心として実施しています。当院では、この10年で2000例近くの大腸癌手術を施行しています。
術後合併症基準のClavien-Dindo分類Grade IV以上の合併症は1%以下で極めて低率であり、安定した成績を残しています。術後平均在院日数では7.3日でありました。
直腸癌ではほぼ全例でロボット手術を実施 根治性と予後の向上
ロボット手術の執刀は、ロボット手術術者認定を受けた医師が行っています。直腸癌に対するロボット支援手術は従来の腹腔鏡手術の利点をさらに向上させることができると考えられていて、現在、直腸癌ほぼ全例でロボット手術を実施しています。
ロボットは多関節の鉗子を持ち、従来の腹腔鏡手術では難易度の高い骨盤底の操作も、複雑で細やかな手術手技が可能となり、直腸癌に対する根治性の向上が期待できます。
Firefly イメージングシステムにより、リアルタイムに近赤外線ならびに可視光による組織の評価が可能で、縫合不全の対策になり、また下腹神経や骨盤内臓神経を温存することにより、術後の排尿・性機能の保持や早期の回復が期待され、後遺症の少ない低侵襲手術が可能となります。
またロボット手術では、狭い骨盤内であってもロボットの特性を十分発揮することで、骨盤奥深くまで操作ができることから、肛門温存が可能となり、永久人工肛門を回避することが出来ます。
ステージ4でも根治を目指す集学的治療
外科・移植外科 医長
北村 好史(きたむら こうじ)
専門分野
消化器外科、肝胆膵外科、救急外科
学会専門医・認定医
日本消化器科学会専門医・指導医
日本肝胆膵外科学会高度技術専門医
日本救急医学会救急科専門医 など
転移再発大腸癌であるステージ4において、大腸外科医、肝臓外科医、腫瘍内科医など多方面からのアプローチにより根治を目指しています。
当外科では毎年20件程度の転移性肝腫瘍に対する手術を行っております。過去の実績をもとに、肝切除の適応を決めています。
腫瘍個数4個以上または腫瘍サイズ5cm以上の肝転移を切除可能境界域肝転移と定義し、これら切除可能境界域肝転移を持つ症例に対してはまず術前化学療法を行ってから切除を行うという方針にしています。
再発した患者さんでも約半数は肝臓だけの再発であり、切除可能であれば再発部位に対しても積極的に切除を繰り返すことで、予後の改善・治癒が見込めます。
肝転移に対しては外科切除を積極的に実施
その件数は増加してきており、腹腔鏡手術での切除も急増しています。肝切除術はその解剖学的な特徴から高難易度のことが少なくありません。肝胆膵外科高度技能専門医を中心に、根治切除を目指しています。従来行われてきた開腹手術に比べて腹腔鏡手術は術後の回復が早く整容性の面だけではなく、出血量も少ないなどのメリットはありますが、腫瘍の位置や大きさによっては腹腔鏡下でできる手術は制限されます。現在では約8割の肝切除を腹腔鏡下で行っています。
切除困難な症例に対しては化学療法を併用
肝予備能が、限界よりも小さい場合は切除不能と判断せざるを得ませんが、化学療法により腫瘍が小さくなることで切除が可能となることがあります。手術前に門脈塞栓により残肝を増加させる処置や、手術を2回に分けて切除する方法(2期的肝切除)を選択することで、切除困難とされる肝腫瘍も切除できる症例があります。
術前に撮影された画像を元に3D画像を構築することで切除範囲や術式を設定し、手術の難易度や残る予定肝容量を推測することができ、過不足のない最適な術式を決定します。
また術中にICG蛍光イメージングを用いて、腫瘍の描出や切除する肝領域をリアルタイムに描出させて肝切除のナビゲーションとして活用し、より質の高い安全な手術を提供しています。
肝被膜下にある小病変は、術中超音波では描出が難しいことがあり、ICG蛍光イメージングを用いて腫瘍を同定しています。
日進月歩の化学療法
腫瘍内科 部長
安井 久晃(やすい ひさてる)
専門分野
固形がんの薬物療法、サポーティブケア(支持療法)、がんゲノム医療
学会専門医・認定医
日本内科学会 認定内科医・指導医
日本臨床腫瘍学会 がん薬物療法専門医・指導医 など
①肝転移切除後の補助化学療法
当院が中心となって行った多施設共同臨床試験では、肝切除後に補助化学療法を加えることにより、良好な結果が得られています。肝転移の治癒切除後の補助化学療法として、カペシタビンを1サイクル、カペシタビン+オキサリプラチン(CAPOX)を4サイクル投与し、5年間の無再発生存率と全生存率はそれぞれ65.2%、87.2%であり、最も多かったグレード3以上の毒性は、好中球減少でした(29%)¹⁾。肝切除後の化学療法は副作用が強く出るとされていますが、腫瘍内科でのマネージメントにて、十分な治療が継続され、良好な生存率が得られています。
1)Satake, et al. The Oncologist 2021;25:1–8
CAPOXによる3ヶ月間の補助化学療法は忍容性があり、肝転移治癒切除における有望な戦略のひとつと考えられます。そのうえで今後は遺伝子の特徴による個別化医療を進めていく必要があると考えています。
②切除不能肝転移に対する術前化学療法
分子標的薬の導入により、一見切除不能に見える多発肝転移であっても、化学療法で腫瘍縮小が得られれば切除可能となるケースがあります。腫瘍細胞のバイオマーカー(RAS/BRAF遺伝子変異、マイクロサテライト不安定性、UGT1A1遺伝子多型)を検査した上で、最適な化学療法レジメンを選択し、腫瘍内科医がしっかり治療を行います。初回治療であれば60~70%程度の奏効が得られ、根治切除が可能となる割合も20~30%程期待できます。治療効果は6~8週毎に評価し、外科と連携を取りながら、適切な手術のタイミングを検討します。
最近は、免疫チェックポイント阻害薬を用いた新規治療(治験)など、効果が期待できる新しい治療選択肢が増えています。2次治療以降であっても、腫瘍縮小により切除が可能となる可能性もあります。
大腸癌は、ステージ4であっても根治切除ができれば治癒につながる可能性があるため、切除の可能性を諦めず、外科と腫瘍内科がタッグを組んで最善の治療ストラテジーをご提示いたします。
外科、腫瘍内科へのご紹介方法と診療フロー
当科への紹介には当院ホームページに記載されているFAX予約もしくはWeb予約をご利用ください。Web予約ではこちらから専用のIDとパスワードを配布しますので、そこから専用のサイトにアクセスして、空いている枠へ直接予約が可能となっています。 新患外来は、すべての曜日で9~11時の予約が可能です。当院受診後は治療方針が決まり次第ご連絡を差し上げます。通常手術日の1日前に入院していただき、通常術後1週前後で退院となります。患者の希望によりご紹介いただいた先生へ地域連携を通じて紹介させていただいています。
当院への患者紹介方法の詳細はコチラ先生方へのメッセージ
大腸癌では、高度進行癌であっても、手術、化学療法を含めた集学的治療により、長期予後が期待できるようになってきました。また高齢であるからという理由で手術を躊躇されることもありますが、当院では低侵襲手術により、80歳以上、場合によっては90歳以上でも安全に手術を行ってきた実績があります。手術の適応が不確定でも構いませんのでまずはご紹介ください。どのような症例でも対応させていただきます。
腫瘍内科での治療が必要であれば、院内紹介をいたします。私たちのモットーは、市民病院の外科として質の高い医療を提供していくことです。病診連携、病病連携を充実させ、地域の先生方に、当院の医療機能を利用していただくことが重要であり、今後もより緊密な連携を宜しくお願い致します。