脳卒中の治療はタイミングを逸さない素早い初期対応、外科的対処と二次予防に向けた専門的な内科的原因精査が必須です。当科はコメディカルを含めた豊富なマンパワーを背景に脳神経内科とともに総合脳卒中センターとしてチーム医療を実践することで、「脳卒中になっても困らない町 神戸」を目指して24時間365日外科・内科単科では実現しえない質が高く専門的な脳卒中診療を実現しています。

脳神経外科領域の血管内治療は日進月歩で新しいデバイスが出てくる世界です。国際的なレベルで血管内治療の時代の最先端を走る当科のノウハウを駆使して外科的治療が困難な血管障害性疾患に対し「切らない治療」を実践しています。もちろん腫瘍性疾患もその道のエキスパートがあなたの病気に対して適切な対処法を親身に提案します。

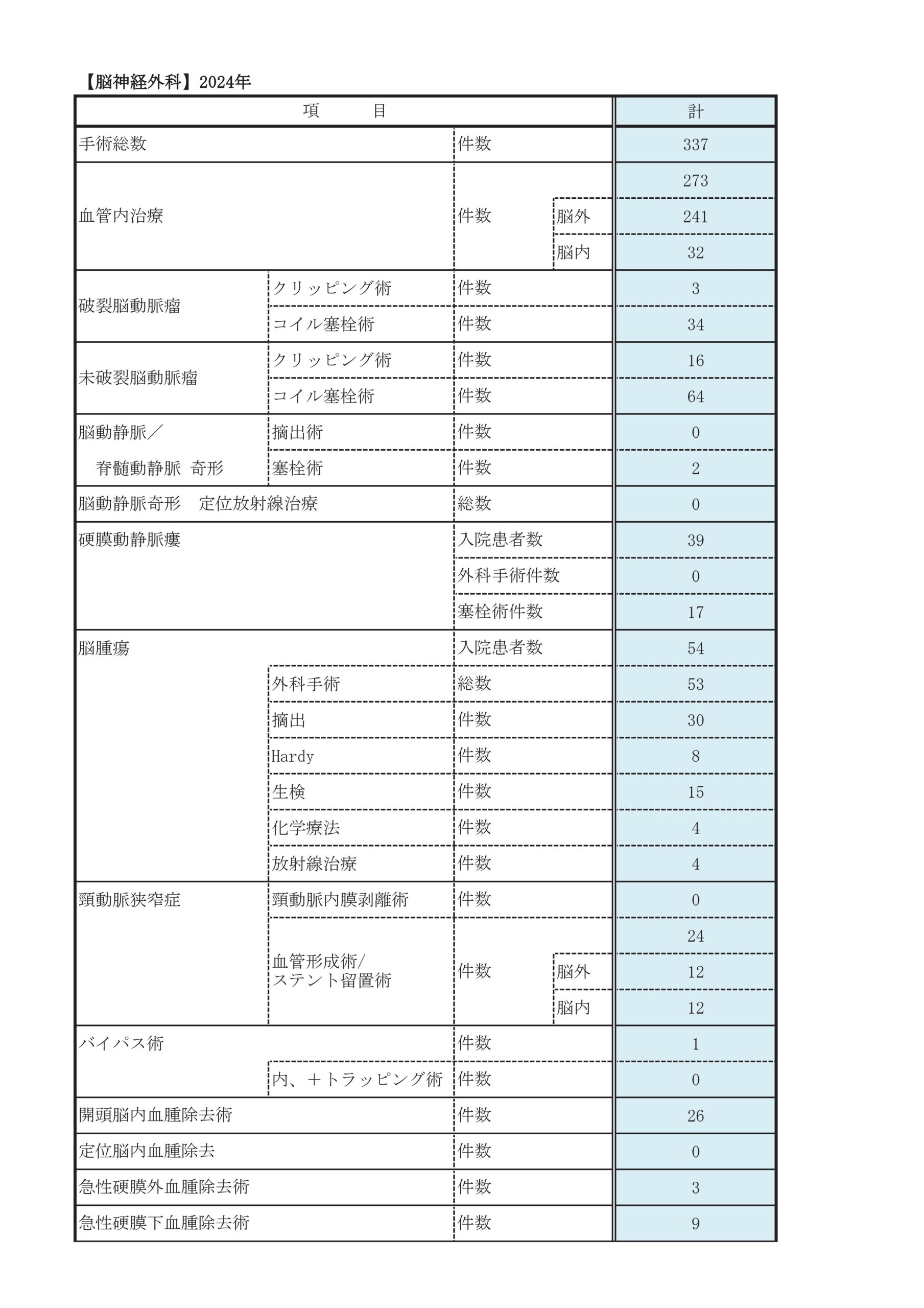
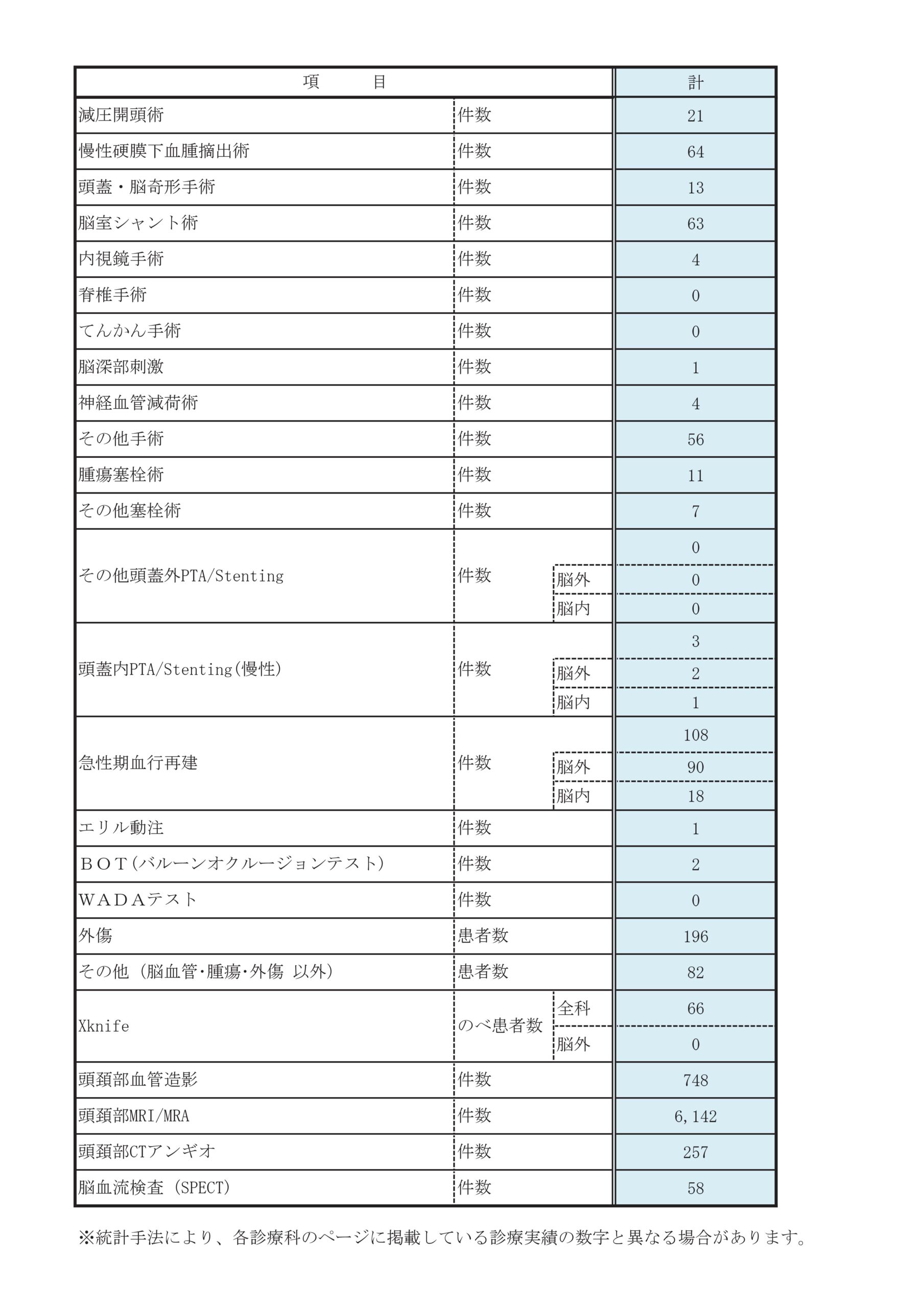
診療実績
診療科別統計
主な疾患・治療法
脳血管障害
- 当院は24時間365日、すべての脳卒中患者さんを断らずに受け入れています。
- 最先端のハイブリッド手術室が24時間使用可能です。
- 脳神経専用の血管撮影室を3室使用しています。
- 脳神経外科学会専門医9名、脳卒中学会専門医8名、脳血管内治療学会専門医8名(うち指導医4名)、脳卒中の外科学会技術認定医4名(うち指導医1名)が在籍しています。
脳卒中とは
脳卒中とは、脳の血管が詰まったり、あるいは破れて出血したりして、脳の一部の機能が失われる状態です。大きく分けて、脳梗塞、脳出血、くも膜下出血があります。病態や大きさ、部位などによって治療方針は異なりますが、いずれも早期の診断、早期の治療が必要です。
当院では救急部の医師の協力を得て、24時間365日断らない医療を実践しています。神戸市内の救急隊との直通電話「脳卒中ホットライン」を用いて、搬送の時点から治療までを脳卒中専門医が直接診療を行い、短時間で滞りなく行っています。さらに休日・夜間でも常に二人以上の脳卒中専門医師が常に勤務しており、いかなる時でも迅速に診断・治療を行う態勢を整えています。また脳神経内科とも密に連携を取り、薬剤の選択や調整など、脳卒中の再発予防にむけて適切な全身管理を行っています。
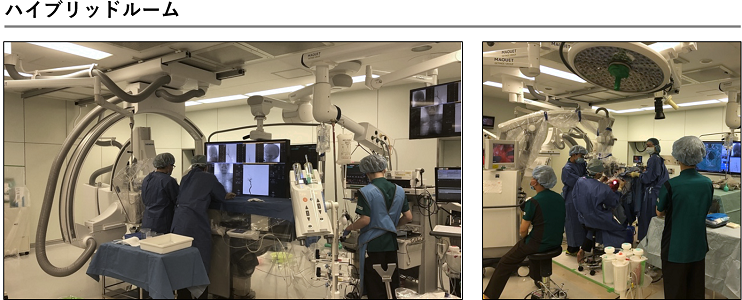
当院では3室の血管撮影室があり、近年急速に進歩を遂げている血管内治療を迅速に行うことができます。また、血管内治療および開頭術をいずれも行うことができるハイブリッド手術室が24時間使用可能で、麻酔科による全身管理のもとで安全に診断、治療を行うことができます。
急性脳梗塞(脳主幹動脈閉塞症)
- 不整脈などでできた血栓により脳血管が閉塞する病気。
- 治療はカテーテル治療とtPAの投与。
- 予後を決めるのは、いかに早く治療するか。
主に不整脈が原因でできる血栓(血のかたまり)が原因となり、脳の太い血管が急性に閉塞する病気です。脳梗塞の中でも最も重篤になり後遺症が残りやすく、tPA(血栓を溶かす薬剤)の点滴や、カテーテル治療による血栓の除去が必要になります。
この病気の予後は、発症からどれだけ早くtPAの投与とカテーテル治療を行うことができるかにかかっています。当院では、24時間365日2人の脳卒中医が勤務し、11人のカテーテル治療専門医がほぼ毎日当直する体制をとることで、救急搬送到着直後から患者さんの診療を救急部と一緒に行っています。
閉塞した血管が再開通するまでの時間が5分延長するごとに、100人に1人の自立が妨げられるといわれており、世界の推奨では患者さんが病院に到着してから60分でのカテーテル治療開始が勧められています。当院では、脳卒中センターと救急部の協力のもと、患者さんが来院されてから半数以上の方が約50分以内(2023年実績)でカテーテル治療を受けており、神戸市内どこから搬送されても最も早く治療をうけていただける体制を自負しています。
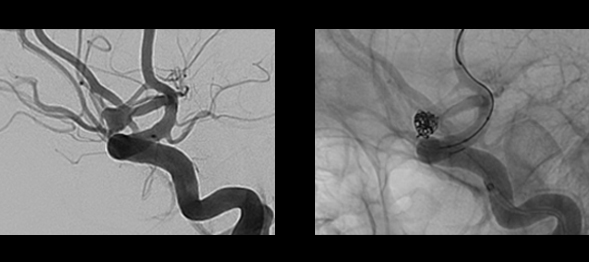
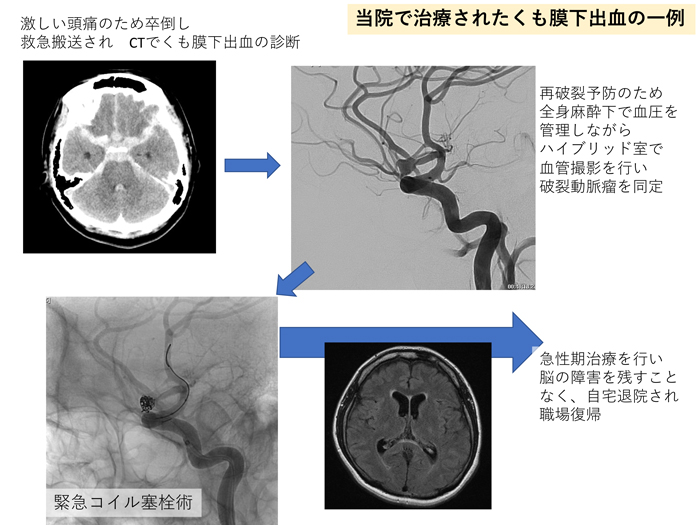
くも膜下出血
- 突然の激しい頭痛や意識障害・嘔吐で発症します。
- 再破裂した場合、救命率は下がるため、再破裂を防ぐための治療が必要です。
- 血管内治療と開頭クリッピング術の治療を最適に選択する必要があります。
- 当院ではハイブリッド手術室を使用して間断の無い治療が可能です。
くも膜下出血とは、頭蓋内のくも膜下というところに突然出血が起こります。多くの場合、原因は脳動脈瘤の破裂によります。くも膜下出血を発症した場合、約1/3は死亡し、約1/3は重度から中等度の後遺症が残り、残りの1/3は治療の末、社会復帰します。たとえ死亡せず病院にたどり着いたとしても、再破裂した場合には社会復帰する率はさらに下がります。再破裂を防ぐための治療が必要です。
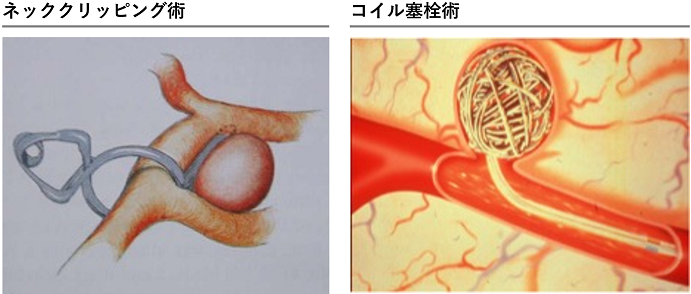
治療法には、血管内治療と開頭クリッピング術の2種類があります。動脈瘤の部位や形状、大きさに基づき、救急診療の現場で、最適な治療戦略を柔軟に組んで対応していく必要があります。当院は日本脳神経外科学会認定専門医10名、日本脳神経血管内治療学会認定専門医9名(うち日本脳神経血管内治療学会認定指導医4名)が医師スタッフとして働いており、ほぼ365日24時間 各専門医が院内に勤務しており、くも膜下出血の治療に携わることが可能です。
当院では出血性脳卒中症例に対し、このハイブリッド手術室を使用できるため、診断から治療まで間断の無い治療が可能となっています。
術後も集中治療医と共に術後管理を行い、継続的な全身管理とケアを行なっていくことで、くも膜下出血に続発する脳血管攣縮と水頭症に備えます。
重篤かつ予後不良な疾患ではあるものの、これら体制により、総じて良好な治療成績をおさめています。
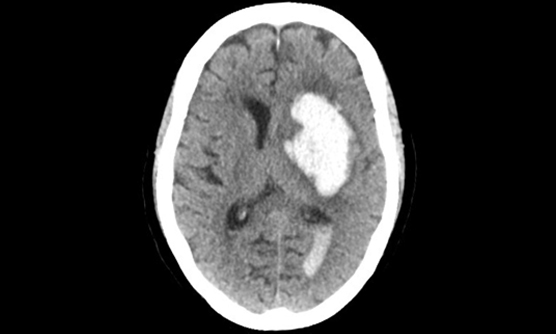
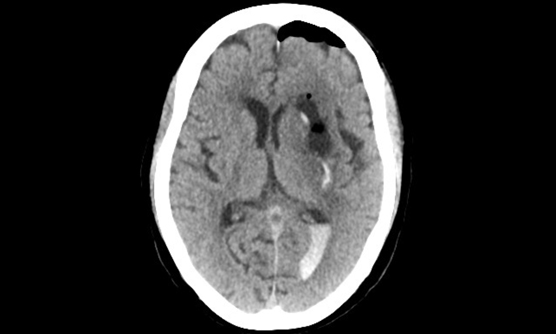
脳出血
- 突然の意識障害や頭痛、半身麻痺などで発症し、早期発見・治療開始が重要です。
- 脳神経外科・脳神経内科共同の脳卒中診療体制(24時間365日複数の脳卒中医師常駐、複数症例同時対応可能)を整えています。
- 出血増大による症状の増悪を回避することが大事であり、時に救命のための手術が必要となることがあります。
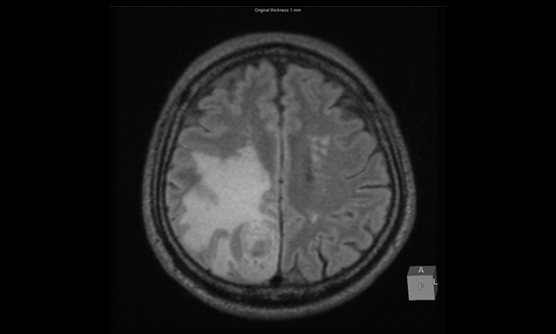
脳の細い血管が破れ、脳内に出血を起こすことで、突然、意識障害や頭痛、嘔気、半身麻痺などが生じます。ひとたび発症した場合は、早期の発見・専門病院での治療開始が望まれます。脳出血の治療は、血圧管理を中心とした出血増大の予防と、早期のリハビリテーションが重要ですが、出血量が多く、脳への圧迫が強くなって命が危機に瀕すると判断される場合には救命のための手術が必要になります。
脳出血の原因は、高血圧によるものが多くを占めますが、それ以外に脳動静脈奇形、もやもや病、脳腫瘍など、決して見逃してはいけない疾患が背景に隠れている場合があります。当院はハイブリット手術室(CT撮影・カテーテル検査・血管内治療・直達手術を同時に行うことができる手術室)を有しており、早急な検査・原因の同定を行い、治療につなげることができる脳神経外科・脳神経内科共同の脳卒中診療体制(24時間365日、複数脳卒中医師常駐、複数症例同時対応可能)を整えており、いつでも最適な治療を行うことが可能です。
また適応症例に対しては、脳卒中ケアユニット(SCU)で発症後早期から、積極的なリハビリテーションを行います。重大な脳出血では、後遺症が残ることが多く、時に致命的にもなり得ますが、一人でも多くの方が身体の機能や正常な生活を営むための能力を戻し、家庭・社会復帰ができるよう、治療に取り組んでおります。
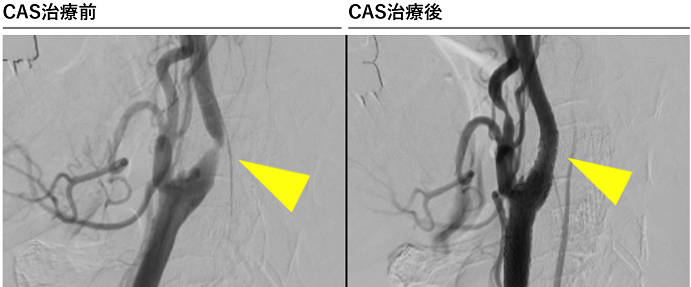
- 頚動脈が頚部で狭くなることにより、脳梗塞の原因となります。
- カテーテルを使った切らない治療が可能で、これまで約1000件以上の実績があります。
- 必要に応じて外科治療も行っており、患者さんに応じた最適な治療を行います。
頚動脈狭窄症とは
頚動脈狭窄症とは、心臓から脳につながる頚動脈が狭くなる病気です。高血圧症などの生活習慣病による動脈硬化により発症し、脳梗塞の原因となることがあります。
治療は外科治療によって動脈硬化の部分を取り除く手術(頚動脈内膜剥離術)と、カテーテルを使って狭窄している部分を拡張させ、ステントと呼ばれる金属製の筒を血管に留置する治療(頚動脈ステント留置術)があります。
当院では特に頚動脈ステント留置術に積極的に取り組んでおり、殆どの患者さんでカテーテル治療が可能です。治療は脳神経内科と合同で行っており、経頭蓋ドップラー(TCD)など、様々なモニターを使用して安全に治療を行うことに努めています。
当院で日本にこの治療が導入された約20年前からの経験があり、現在まで約1000件以上の治療の実績があります。
頚動脈ステント留置術は造影剤を使用するため、一般的には腎臓の機能が悪化している方には行われないことが多いですが、当院では造影剤の使用量を極力抑えた方法も行うことが可能です。
- 脳の血管にできたこぶで、多くは無症状ですが、破れるとくも膜下出血になります。
- 治療法は、血管内治療と開頭手術の2種類があり、患者さんに応じた最善の治療を選択することが必要です。
- 2023年度の治療実績は、82件(手術14件・血管内治療68件)です。
未破裂脳動脈瘤とは
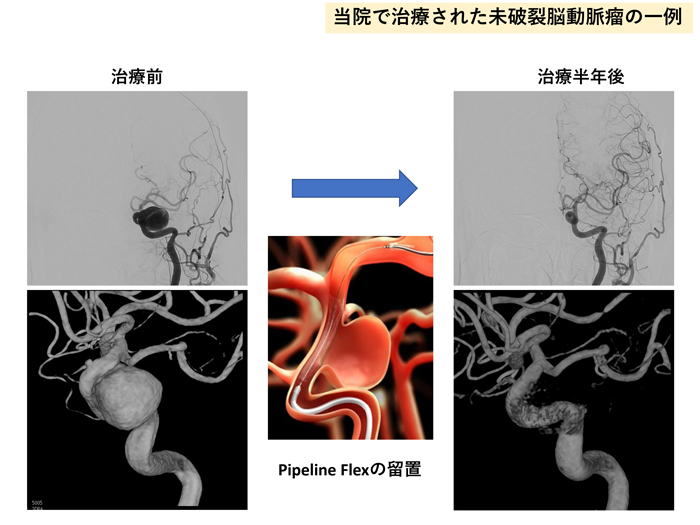
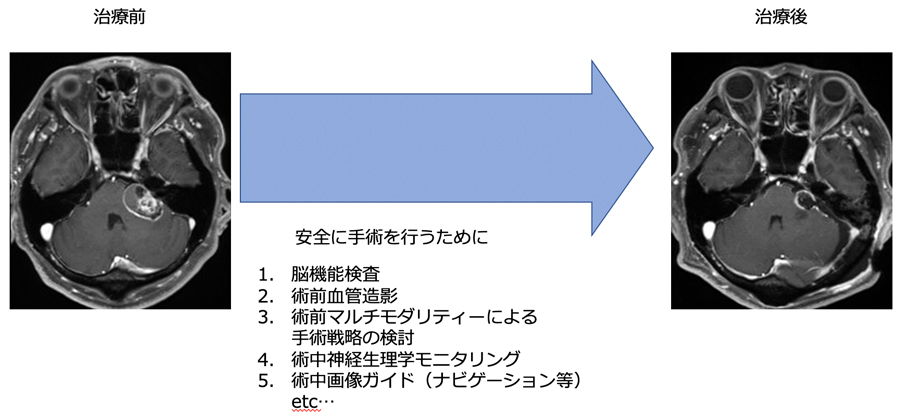
未破裂脳動脈瘤は、部位・大きさ・形状や患者さんの状態に応じて、治療の是非が検討されます。治療方法には、開頭クリッピング術と血管内治療の2種類があります。当院では、どちらの専門家も擁しており、精密検査の結果を踏まえ、最善の治療方法を選択することが可能です。
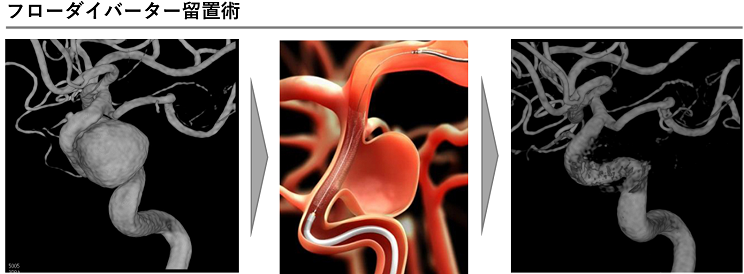
血管内治療は2001年以降、約2300例の経験があり、コイルやステントなど殆どの最新のデバイスの使用が可能で、さらに安全性と根治性を追求した治療を行っています。また従来は治療が難しかった巨大脳動脈瘤に対しても、フローダイバーターステントを用いた治療を行なっており、良好な治療成績をおさめています。
開頭クリッピング術は、最新のハイブリッド手術室で行います。これまで術後に行なっていた血管撮影を手術中に行うことで、患者さんの負担軽減を図っています。神経誘発電位モニタリング(術中神経評価)・術中ICG蛍光血管撮影も標準的に行っていますので、より安全なクリッピング術が可能です。
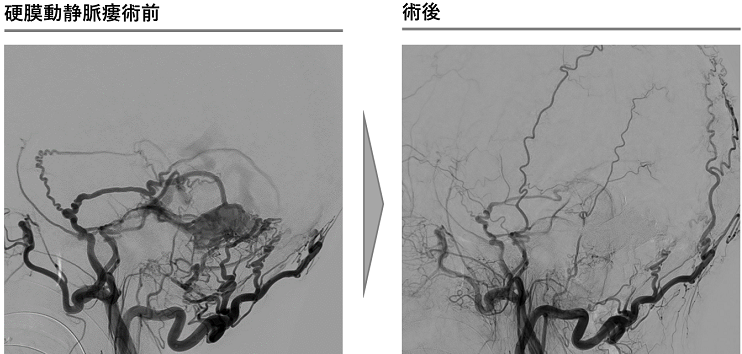
- 硬膜という脳を包む膜の血管に異常な連絡ができる病気で耳鳴り、眼の症状、痙攣や麻痺などの多彩な症状をきたしたり、脳出血を発症します。
- 部位によって開頭手術とカテーテル治療を使い分け治療を行います。
- 当院は液体塞栓物質(OnyxやNBCA)を用いた治療が可能な施設です。
硬膜動静脈瘻とは、頭蓋骨や脊椎骨の内側にある硬膜(脳や脊髄を包む膜)上の動脈と静脈との間に異常な連絡(動静脈短絡)が形成され、血液の逆流をきたす病気です。
症状は、その発生部位や血流量にもよりますが、拍動性の耳鳴り、眼球突出、眼球結膜充血、物が2重に見える複視、脳への血流の逆流をきたせば麻痺や言語障害、痙攣、意識障害や認知症状などがおこり、ひどい場合には脳に出血することがあります。
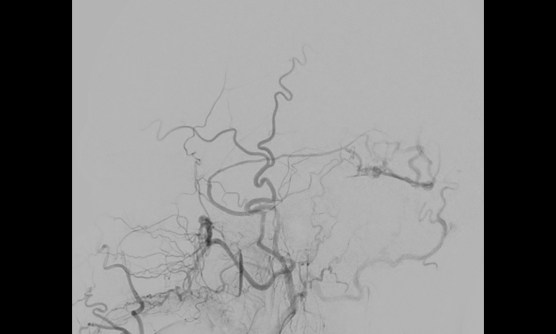
MRIや脳血管撮影により診断し、開頭手術とカテーテル治療のどちらが適切か判断し治療を行います。カテーテル治療では金属製のコイルや液体塞栓物質(NBCA、Onyx等)で異常血管の閉塞を目指します。当院は液体塞栓物質による豊富な治療経験があります。
また当院には血管撮影装置を常設した手術室であるハイブリッド手術室があり、手術とカテーテル治療の複合治療も行えるため、より安全で高度な治療が可能です。
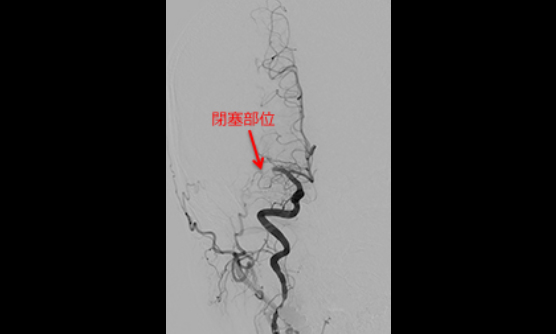
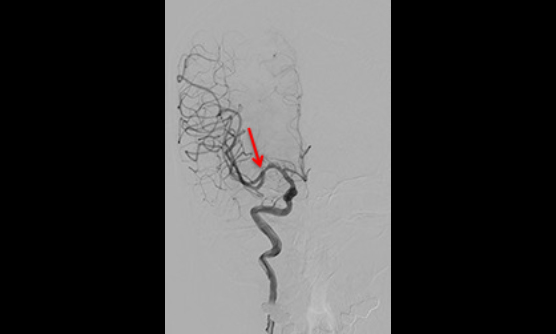
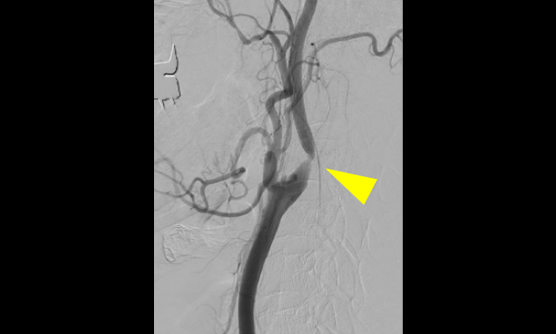
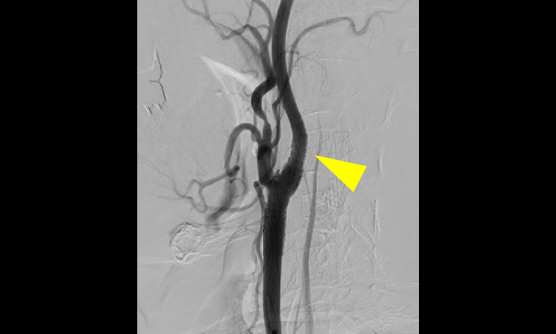
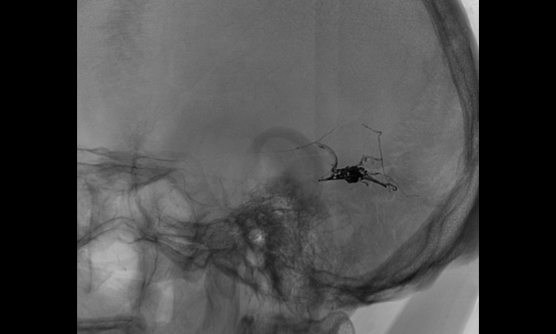
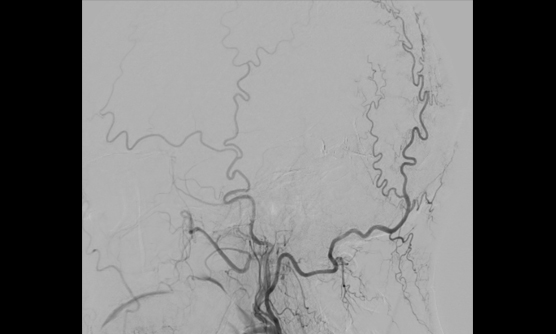
硬膜動静瘻に対するONYXでの治療例
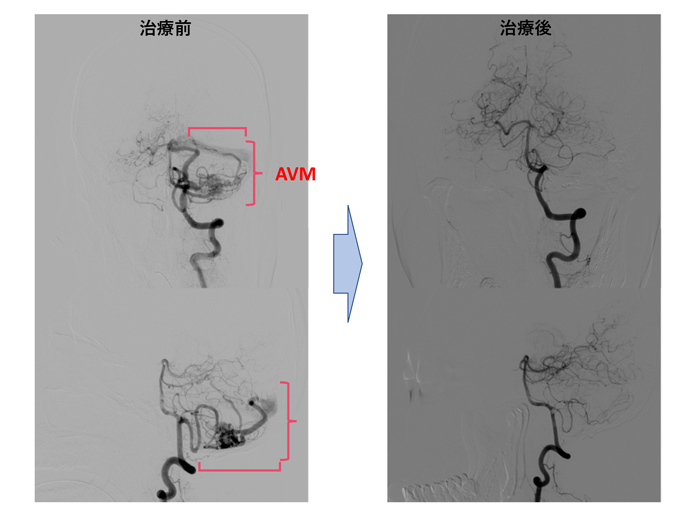
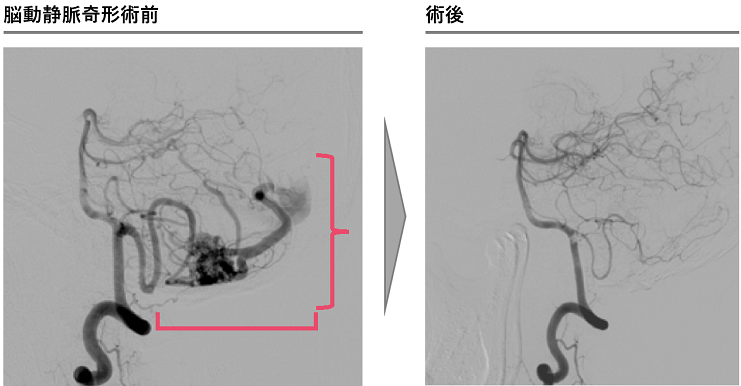
- 脳内に異常な血管塊(ナイダス)があり、動静脈が直接吻合する病気で、くも膜下出血や脳出血、痙攣の原因となります。
- 治療には開頭手術、血管内治療、放射線治療があり、それらを組み合わせて行います。当院では全ての治療方法の実施が可能です。
- 当科では術者指定のあるONYX(血管内治療で用いる液体塞栓物質)が使用可能で、国内トップクラスの使用実績があります。
脳動静脈奇形(脳AVM)は、異常な血管塊(ナイダス)を介して動静脈間が直接つながっている病気です。多くは脳表に位置しますが、脳内のどこでも発生します。出血やけいれんを契機に発見されることが一般的です。
年間発見率は1.1-1.4人/10万人で、破裂の発生頻度は脳動脈瘤によるものと比べて1/10程度とされていますが、AVM個々の年間出血率は2-3%程度と脳動脈瘤に比べると若干高いと言われています。
血管内治療は、手術摘出前の治療として重要で、手術中の出血を大幅に軽減し、より安全な手術を可能にします。特に液体塞栓物質ONYXについては、薬事承認当初より当院は認定施設となっており、国内での治療実績をリードしています。また、当院では脳神経外科専用のハイブリッド手術室を完備しているため、手術と血管内治療/検査が同時に可能であり、脳AVM治療でもその有用性が発揮されます。
放射線治療は、摘出困難例や手術を希望されない方で行なっており、当院の放射線治療科と密に連携しながら治療を行っています。
- 動脈の壁が内部で裂けて、突然の痛みで発症します。症状がなく画像検査で偶然発見されることもあります。
- 脳梗塞やくも膜下出血を発症することがあります。
- 治療には薬物による対症療法と血管内治療があり、適切な診断が必要です。
動脈は内膜、中膜、外膜の三層構造で形成されておりますが、その膜間で血管が裂けることを動脈解離と言います。外傷性や特発性(原因がはっきりしないこと)が多く、椎骨動脈と内頚動脈の解離がほとんどです。MRIや造影CTで診断可能なことが多く、精密検査が必要な場合は脳血管撮影検査を行います。
日本人に多い椎骨動脈解離のほとんどは頭痛や後頚部痛で発症します。無症状なこともあり、非出血性では内服加療のみで保存的に経過を見ることがほとんどですが、一部の症例では外科的介入(主に血管内治療)が必要となります。
発症直後から外科的治療が必要な場合は、主にくも膜下出血を発症している例で、破裂脳動脈瘤に準じた治療が行われます。
時間が経ってから外科的治療が必要になるのは、抗血小板薬による保存的治療が行われたにも関わらず脳梗塞を繰り返す例や、動脈解離によって発生した動脈瘤が大きいもしくは拡大する例などで、やはり脳動脈瘤に準じた治療が行われます。
症例ごとに適切な対応が異なるため、発症した際は早期に病院を受診し、専門的な診断を行う必要があります。
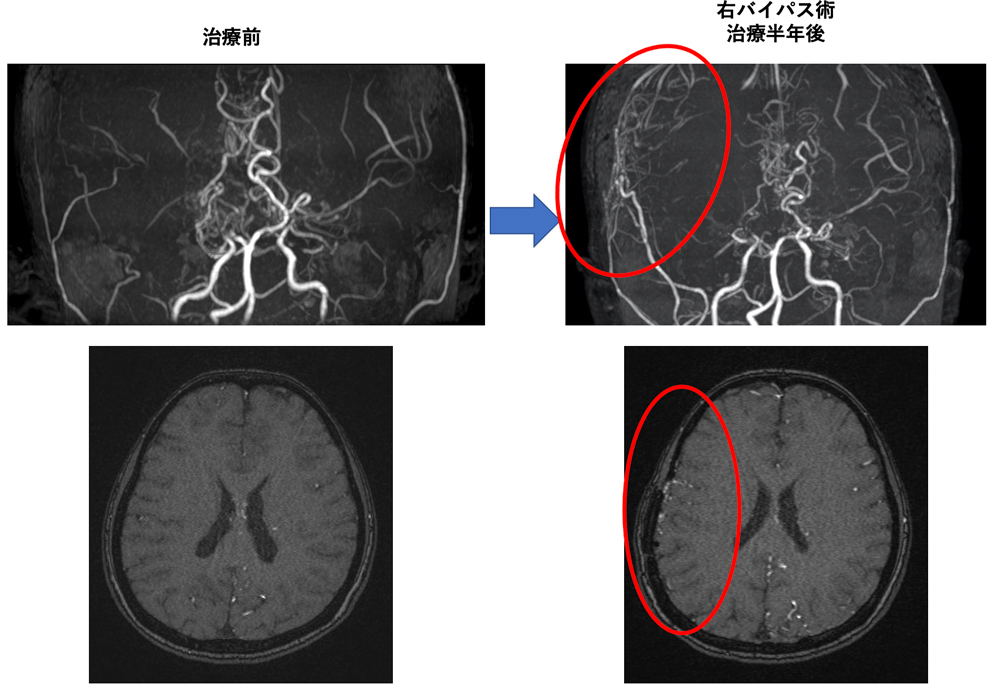
- 脳の太い血管が狭窄し、細い血管で脳が栄養される病気です。
- 脳梗塞、脳出血いずれの原因にもなります。
- 血管吻合術などによって症状の進行を抑えることができます。
もやもや病は脳の血管が狭窄し、発達した多数の細い血管のみで脳が栄養される疾患です。脳の血流を補うために、「もやもや」とした新しい血管が作られるため、もやもや病と名付けられました。脳の血流が不足し脳梗塞を起こしたり、もやもやとした弱い血管が破れて脳出血を起こしたりします。小児期だけでなく、成人になってから発症することもあります。日本で発見された、日本人に多い病気であり、厚生労働省で難病に指定されています。原因は不明ですが10%程度は家族内発症が見られ、最近では関連した遺伝子異常も判明してきました。
診断はMRIなどで行いますが、詳細な脳血管および血液の流れを把握するためには脳血管造影検査(カテーテル検査)が有効です。また頭部CT、脳血流シンチグラフィ(SPECT)など、もやもや病の状態を評価するために必要な検査も全て施行することが可能で、適切な治療方針を立てることができます。
再発予防の為にはバイパス手術(頭皮の血管を脳の血管につなぐ手術)が必要となることがありますが、治療内容は脳梗塞、脳出血の程度により異なり、薬物治療やリハビリテーション加療を優先するべき場合もあります。当院では脳神経内科、麻酔科、リハビリテーション科などと協力し、一人一人に適切な治療、術後管理、リハビリテーションを行って症状が改善するように努めています。
機能疾患
- 血管が脳神経(三叉神経、顔面神経)を圧迫することでそれぞれ顔面の激痛、痙攣を引き起こす病気です。
- 内科的治療の効果が乏しい場合も多く、手術により神経に対する圧迫を解除します。
- 聴力低下等の合併症予防のため当院では全例で様々な術中モニタリングを行っています。
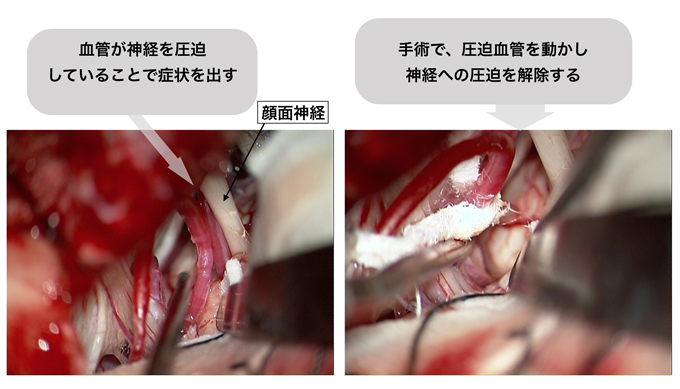
三叉神経痛は顔面の感覚を司る三叉神経を、顔面痙攣は顔面の運動を司る顔面神経を、主に血管が圧迫することで顔面の激痛、または痙攣を来す病気です。
対症療法として三叉神経痛に対しては抗てんかん薬を始めとした薬物治療、顔面痙攣に対してはボトックス注射があり当院神経内科でも積極的に施行しています。
薬物での治療が困難な場合、手術を行います。原因となる血管を神経から剥離し、テフロンなどを用いて圧迫をなくす手術です。手術により起こりうる合併症として聴力低下が心配されます。当院では聴力の術中モニタリング(ABR)を全例で行っており、これまでの手術では殆ど聴力の低下はおこっていません。また顔面痙攣の手術中は、圧迫による異常な電気信号の消失を確認する(AMR)ことで、手術中に顔面痙攣の消失を確認しています。
微小血管減圧術とは
- 脳深部刺激療法は、進行期パーキンソン病の運動症状を改善します。
- 特に薬物療法によるコントロールが困難となった症例では、ADL(日常生活動作)およびQOL(生活の質)を改善します。
- 脳深部刺激療法後には、抗パーキンソン病薬の減量が可能です。
- 脳深部刺激療法は、パーキンソン病以外にも、本態性振戦および一部の全身性ジストニア[註1]も有効です。
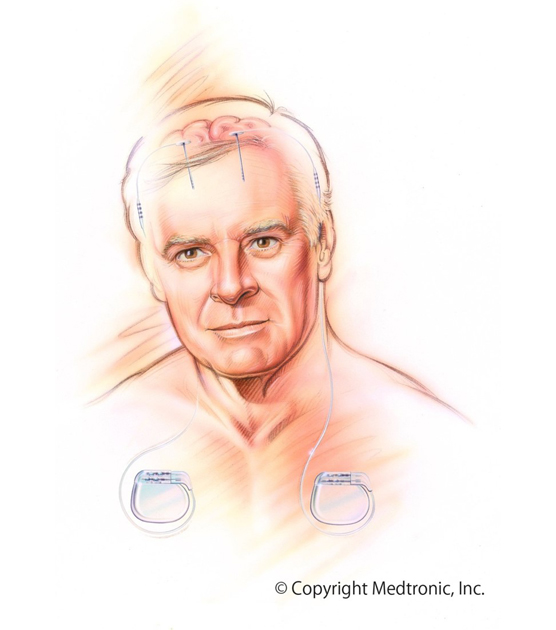
パーキンソン病の患者さんに対する、脳深部刺激療法(Deep Brain Stimulation:DBS)は、本邦で2000年4月に保険収載され、これまでに全国で約1万人の患者さんがこの手術を受けています。
パーキンソン病とは、振戦(ふるえ)、動作の緩慢、筋肉の固縮、姿勢保持障害を主な症状とする病気です。日本での有病率は、人口1000人あたり1人と言われ、全国で15万人の患者さんがいると推計されています。パーキンソン病では中脳黒質にあるドパミン産生細胞が減少していくことにより、大脳皮質と基底核の連絡回路にアンバランスが生じ、運動制御がうまくできなくなることで、上記のような症状が出ることが判っています。残念ながら、現在でも根治的な治療は確立しておらず、薬剤治療を行って症状を緩和するようにしていますが、ドパミン産生細胞の枯渇に伴い経時的に進行して重症になっていく病気です。このような進行期のパーキンソン病に対し、視床下核に対するDBSは、運動症状を改善することができ、特に薬物療法によるコントロールが困難となった症例では、日常生活動作(Activities of Daily Living:ADL)と生活の質(Quality of Life:QOL)を明らかに改善することが知られています。Wearing off[註2]やディスキネジア[註3]のあるパーキンソン病患者さんにも効果が期待できます。
具体的な手術方法を簡単に紹介します。頭皮に小さい切開を設け頭蓋骨に小さい穴を開けたのち、脳深部に電極を挿入していき、神経細胞の活動電位をはかりながら最適の刺激留置部位を検討します。電極留置予定部位を試験刺激して、神経学的診察を行いパーキンソン病の症状の改善の程度と、副作用が出ていないかを確認しながら、刺激位置を決めて電極を留置し、それを胸部に埋伏した刺激装置に接続します。
DBSは脳神経外科が単独でできる治療ではなく、術前、術中、術後を通じ、パーキンソン病に精通した神経内科医と、生理機能を担当する臨床検査技師、診療放射線技師、麻酔科医、手術部スタッフなどとの連携によって成し遂げられる手術です。多職種のプロフェッショナルで構成される当院では本療法を行うことが可能です。
パーキンソン病の患者さん達のQOLが向上し、より良い生活を維持することに貢献したいと思っています。
Wearing off[註2]やディスキネジア[註3]があるなどの場合には、主治医の先生に相談のうえ、脳神経外科と神経内科の専門の外来を受診してください。
註1 ジストニアとは、筋肉の緊張の異常によって様々な不随意運動や肢位、姿勢の異常が生じる状態のことで、筋緊張を調節している大脳基底核という部分の働きの異常によっておこると考えられています。
註2 Wearing offとは、抗パーキンソン薬の効果継続時間が短縮し症状が変動する状態です。
註3 ジスキネジアとは、自分の意思とは関係なく体が動いてしまう不随意運動の総称。特に四肢が勝手に動くことが多く、自分で止めることができないので長時間続くと疲れてしまいます。抗パーキンソン薬の副作用で起こります。
脳腫瘍
- 脳脊髄の中にある神経膠細胞(グリア細胞)からできる腫瘍です。
- 摘出手術に加えて放射線治療や化学療法など複合(集学)的に治療を行います。
- 摘出手術時には神経機能の術中モニタリングやナビゲーションシステムを用いた安全かつ十分な摘出を行います。
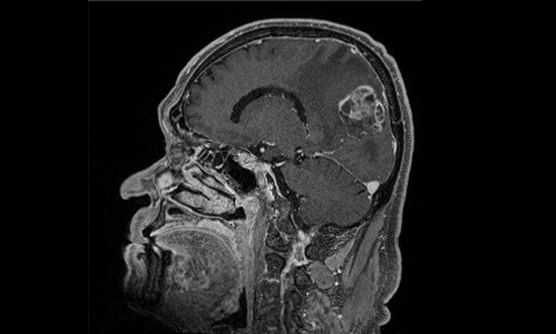
神経膠腫(グリオーマ)は、脳脊髄の中にある細胞からできるできもの(脳原発腫瘍)の中では最も多く、およそ2割を占めているといわれています。神経細胞と神経細胞の間に存在する神経膠細胞(グリア細胞)が由来と考えられています。
上述の通り、神経細胞の間に存在する細胞が腫瘍となったもののため、脳脊髄の中を染み渡るように増大(浸潤)している上、大切な機能を果たす脳神経の近くに存在することも多く、外科的手術だけでは根治することは困難です。
悪性度の高いグリオーマでは、脳脊髄の機能を温存した可能な限りの摘出手術の上で、手術周囲を含めた放射線治療とテモゾロミドという飲み薬(もしくは注射薬)を用いた複合(集学)的な治療が標準的に行われます。
当科でも上記標準治療に合わせて、腫瘍の部位が手術中に確認できる製剤(5-ALA)や画像支援(ナビゲーション)・脳機能の評価(モニタリング)を利用しつつ、腫瘍を摘出した跡に留置する薬剤(Gliadel)、特殊な電場を発生させる装置(Novo TTF)を頭部に装着し腫瘍細胞の分裂を抑えるという治療も、場合によって用いています。
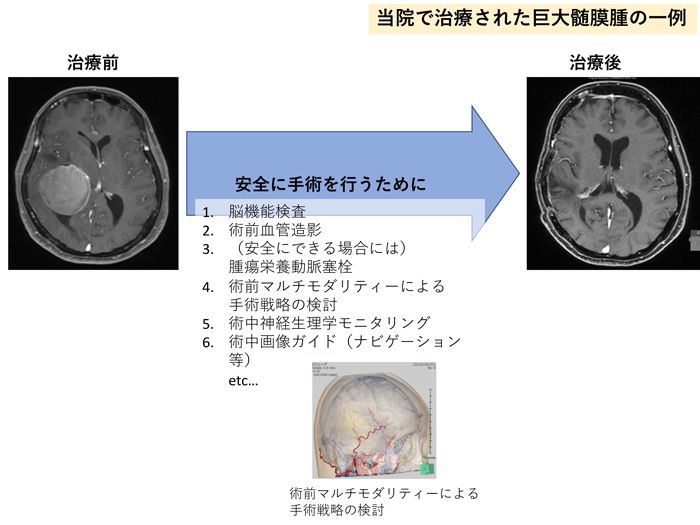
- 脳を包んでいる髄膜という膜から発生する腫瘍。悪性の経過を辿るのは2〜5%で、大部分は良性腫瘍です。
- 脳が圧迫され神経症状がある場合や、脳浮腫を伴う場合には治療が検討されます。
- 術前の塞栓術やモニタリングを併用することで、より安全な手術を行っています。
髄膜腫は、脳を包む髄膜から発生する腫瘍で、大部分が良性腫瘍です。これは、増殖速度が遅かったり、転移や浸潤しないという意味です。しかし、頭蓋骨という閉じた空間のため、転移や浸潤をしなくても、脳が圧迫をされたり、周囲に浮腫を伴い症状を呈する場合があります。その場合には、手術が検討されます。
当院では、術中神経誘発電位モニタリングを併用し、手術に際して神経学的後遺症を起こしにくくしているほか、術前評価で安全に塞栓できると判断される症例に対しては、術前に経動脈的腫瘍塞栓術を行い手術に伴う出血を最小限に留めるように務めています。
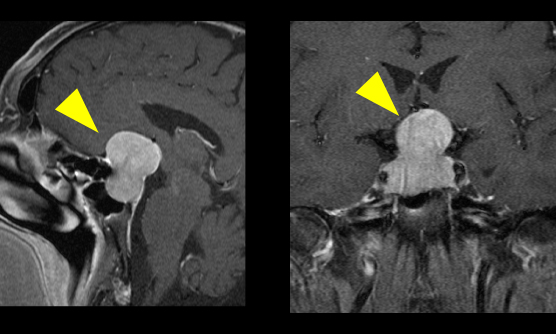
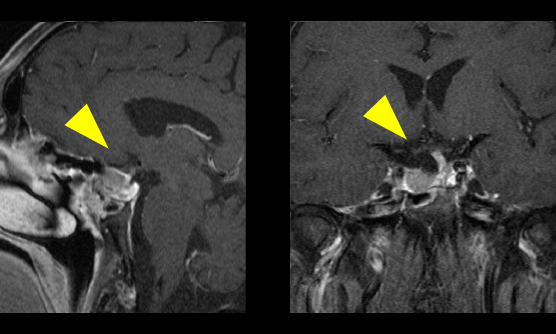
- ホルモンの低下や過剰による症状、視力・視野障害で発症します。
- 鼻から内視鏡を使用しての手術をしています。
- 各種のモニターを使用しながら安全な手術を心掛けています。
- 内分泌内科と連携して術前、術後の治療を行います。
下垂体腫瘍とは
下垂体とは、脳の中心部にあり、体の様々な機能を整える各種のホルモンを分泌する臓器です。下垂体周辺にできる腫瘍としては、主に下垂体腺腫、頭蓋咽頭腫、ラトケ嚢胞があります。
下垂体腺腫とは、下垂体そのものから発生する腫瘍です。増大すると、すぐ上方にある視神経を圧迫し、視力障害や視野障害をきたすことがあります。また腫瘍の種類によっては、ホルモンを過剰に分泌するものや、逆にホルモンが不足して症状が出現するものもあります。
一部の腫瘍は薬剤で治療可能なこともありますが、薬剤で治療が困難な場合には手術による治療が一般的で、鼻の穴から内視鏡を使用して腫瘍の摘出を行います。手術の際には視力のモニターや、腫瘍の位置を正確に把握するためのニューロナビゲーションシステムを使用して手術を行います。
術前、術後のホルモン管理はホルモンの専門家である内分泌内科の協力を得て慎重に行っています。当院には内分泌代謝科専門医3名が在籍しています。
ラトケ嚢胞も下垂体周辺に存在し、中に液体が貯留している病気です。通常無治療で経過を見ることが多いですが、視野障害などが出現した際には手術が必要です。
頭蓋咽頭腫も同じように下垂体周辺から発生する腫瘍ですが、腫瘍の部位や広がりによっては開頭術が必要になります
- 神経鞘腫とは神経を取り巻く細胞から発生するできもの(腫瘍)で、基本的には良性で耳鳴りや聴力低下、めまいなどで発症します。
- 腫瘍の大きさなどに応じて手術や放射線治療があり、いずれも当院で実施が可能です。
- 手術は術中モニタリング下で安全に行うことが可能です。
聴神経は蝸牛神経(聴力をつかさどる神経)と前庭神経(体のバランスを取る神経)からなります。聴神経腫瘍はほとんどが前庭神経鞘腫と呼ばれ、前庭神経から発生しています。神経鞘腫とは神経を取り巻くシュワン細胞という細胞から発生し、脳の神経では他に三叉神経(顔の感覚をつかさどる神経)、顔面神経(顔を動かす神経)などからも発生することがあります。
腫瘍がある側の耳鳴りや聴力低下、めまいなどで脳の検査をしたところ見つかることが多いです。ただ周辺には顔面神経や脳幹・小脳という部位があり、さらに大きくなると顔面神経麻痺や歩行障害・意識障害に至ることがあります。神経を取り巻く細胞から発生しており周辺に脳の大事な部位もあるため、症状や腫瘍の大きさで慎重に治療方針を検討する必要があります。
症状がほぼなく偶然見つかった小さな腫瘍では定期的に経過観察をすることもあります。少し大きくなり(3cm以下)軽い症状を認める方には、放射線治療科と協議を行い手術による摘出または定位放射線治療が検討されます。さらに大きくなり(3cmを超える)症状が強い(脳幹への圧迫など)場合には、手術が必要となります。当科では手術の時には残存している(温存すべき)神経機能(聴力・顔面の運動・嚥下機能・眼球運動など)を専門のスタッフの協力の下、術中に評価(モニタリング)しながら、安全な範囲で摘出します。
脊髄
- 脊柱管狭窄症や椎間板ヘルニアのような骨や軟骨の病気と、脊髄腫瘍、脊髄血管障害があります。
- 症状をきたすような脊髄腫瘍には、外科的手術を行います。
- 脊髄血管障害に対しては、患者さんにあわせたカテーテル治療や外科的手術を行います。
脊椎・脊髄疾患とは
脊髄の病気には脊柱菅狭窄症や、椎間板ヘルニアなどがありますが、数は少ないものの、脊髄に血管奇形や硬膜動静脈瘻といった疾患が発見されることがあります。出血して頭痛や背部痛で発症するものや、静脈がうっ滞して症状が出現するものなど、多彩な症状を呈します。複雑な構造の病変も多くみられますが、カテーテルによる血管内治療や手術治療など、個々の病変に最適な治療方針を検討して治療を行います。当院ではハイブリッド手術室を使用して、術中にカテーテル検査を併用した治療が可能です。
また手のしびれなどを契機として、脊髄の腫瘍が発見されることがあります。神経鞘腫や髄膜腫、上衣腫など、様々な種類の腫瘍がありますが、一般的には手術による治療を行います。
臨床研究
| 研究課題名 | 説明文(PDF) |
| 未破裂大型脳動脈瘤の治療変還と成績 | |
|---|---|
| 多施設コホートを利用した血栓回収療法に関する後ろ向き登録調査 | |
| 硬膜動静脈瘻に対するMMAを用いた経動脈的塞栓術 | |
| 多機関コホートを利用したくも膜下出血出血の治療成績と合併症の検討 | |
| 患者の機能生命予後を念頭にした、破裂脳動脈瘤に対する血管内治療と直達術の治療選択 | |
| Medium Vessel Occlusionに対する機械的血栓回収療法の結果にDevice選択が与える影響 | |
| Tigertrieverを用いた機械的血栓回収療法の効果と安全性に関する多施設共同登録研究 Treatment of Acute Ischemic Stroke using Generable Stent Retriever (TIGER Registry in Japan) |
|
| 活動性悪性腫瘍合併脳梗塞に対する血管内再開通療法の多施設共同後ろ向き観察研究 (The Endovascular Stroke thrombectomy for Patients with active Oncologic lllness aiming at Recovery [ESPOIR] Registry) | |
| 脳梗塞中血管閉塞例に対する小口径吸引カテーテルの治療効果を評価する研究 | |
| AIを用いた脳動脈瘤部位診断システムの読影試験を目的とした多機関共同研究 | |
| 硬膜動静脈瘻の病変位置と治療法の選択の関連性 | |
| 頭部外傷の患者背景、治療介入、臨床転機の関係についての後ろ向きコホート研究 | |
| Protection device変更に伴う治療成績の検討 | |
| Medium Vessel Occlusionに対する機械的血栓回収療法の結果にDevice選択が与える影響の研究 | |
| 未破裂脳動脈瘤の再治療に関する後方視的研究 | |
| 破裂脳動脈瘤に対する血管内治療後再発の検討 | |
| 脳動静脈奇形に対する集学的治療の長期成績 | |
| パーキンソン病細胞移植手術における MRI 画像による移植針刺入経路の決定法 | |
| 大型・巨大部分血栓化動脈瘤に対する母血管閉塞とフローダイバーター留置術の治療成績の比較 | |
| 脳主幹動脈閉塞の再開通療法に使用するダイレーターの安全性と有効性に関する研究 付随研究(後方視的観察研究) | |
| Envi-SRステントレトリーバーを用いた機械的血栓回収療法の効果と安全性に関する多施設共同登録研究 Mechanical thrombectomy using Envi-SR for acute ischemic stroke. Initial Experience in Japan (Envi-SR registry in Japan) |
|
| 成人pial arteriovenous fistulaの特徴に関する全国調査(多施設共同後ろ向き研究による実態調査) | |
| 脳動脈瘤に対するFlow Diverter治療の予後予測のためのマルチモーダルAIモデルの構築と治療戦略最適化 | |
| 多機関脳動脈瘤患者コホートを使用したAI に基づく脳動脈瘤診断、増大予測システムの検証研究 | |
| 一般社団法人日本脳神経外科学会データベース研究事業(Japan NeurosurgicalDatabase:JND) | PDF 別紙 |
| Transdural blood supplyを有する脳動静脈奇形の臨床症状、血管構築、治療成績の検討:多施設共同研究 | |
| 頭蓋内動脈の蛇行紡錘形動脈瘤(dolichoectasia)の病態形成及びその臨床像に関する研究 | |
| 内視鏡下脳内血腫除去術の血腫除去率に関連する因子の検討 | |
| 未破裂脳動脈瘤根治術の長期成績 | |
| VertebroBasilar Dolichoectasia の自然歴および外科的治療の成績に関する多機関共同前向き登録研究 (VERtebrobasilar DolIchoectasia Prospective Registry) VERDI study | |
| 脳卒中を含む循環器病対策の評価指標に基づく急性期医療体制の構築に関する研究(Close The Gap-Stroke J-ASPECT Study) | |
| グリオーマにおける化学療法感受性の遺伝子指標の検索とそれに基づくテーラーメード治療法の開発 | |
| 日本人脳出血患者における適切な超急性期降圧療法の探求:SAMURAI-ICH研究とATACH2試験の個別データ統合解析 | |
| Carotid webの頻度と外科的治療の安全性、有効性に関する後方視的多機関共同研究 | |
| 京都大学および関連施設における膠芽腫症例に関する後方視的解析 | |
| 睡眠中発症もしくは発症時刻不明脳梗塞に対するアルテプラーゼ静注血栓溶解療法試験の個別データ統合解析 Evaluation of unknown Onset Stroke thrombolysis trials(EOS) | |
| 脳血流解析ソフトの精度検証と精度向上に関する研究 | |
| レセプト等情報を用いた脳卒中、脳神経外科医療疫学調査 J-ASPECT study(Nationwide survey of Acute Stroke care capacity for Proper dEsignation of Comprehensive stroke cenTer in Japan) | |
| フローダイバーターの有効性と安全性に関する全国悉皆調査 | |
| 発症時刻不明脳梗塞に対する静注血栓溶解療法の多施設共同観察研究(THAWS 2) | |
| 急性期脳卒中症例の諸因子と転帰との関連についての調査研究 | |
| 脳卒中研究者新ネットワークを活用した脳・心血管疾患における抗血栓療法の実態と安全性の解明 The Second Bleeding with Antithrombotic Therapy Study BAT2 |
|
| 適正使用指針第3版に基づく血管内再開通療法の安全性に関する調査研究 | |
| 脳血管内治療の長期成績に関する多施設共同登録研究 | |
| 脳腫瘍全国統計調査と解析 (臓器がん登録調査) |
お知らせ
医師、医師を目指す方向け当科のご紹介
※本コンテンツは、医師の方を対象とし、当医療機関についての理解を深めていただけるよう作成しているものであり、一般の方を対象とする宣伝・広告等を目的としたものではありません。
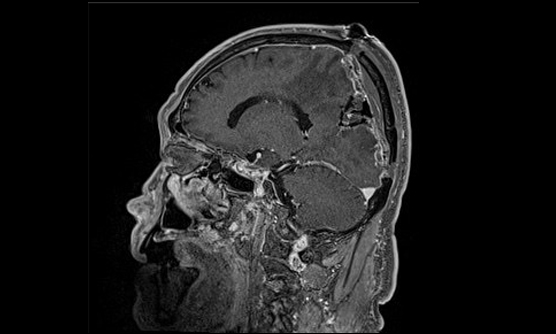
はじめまして、神戸市立医療センター中央市民病院 脳神経外科の太田剛史(おおたつよし)と申します。2022年4月に坂井信幸の後任の脳神経外科部長に就任しました。当院は、神戸市民の命と健康を守る「最後の砦」を唱い、救急医療と高度医療を提供しています。当科は、脳血管障害、脳腫瘍、頭部外傷を中心に脳神経疾患のほぼすべての病態の治療に対応しています。2つの手術室と2つのカテーテル治療室を併用し、9名の脳神経外科専門医を含む19名の脳神経外科医が、脳神経内科医とともに、24時間365日同時に多数の外科的治療と血管内治療が可能な体制を整えており、「脳卒中になっても困らない街」「最新・最善の脳神経外科医療を目指して」をスローガンに、患者さんの安全を第一に日々研鑽を積んでいます。
私たちは、それぞれの医師が外科的手術と血管内治療という2つの異なる治療方法を行うことができる二刀流脳神経外科医であることをモットーに、内科治療を含めたベストの治療方法を患者さんに提供しています。以下に、脳動脈瘤治療を中心に、私たちが行っている脳血管障害の医療の一部をご紹介いたします。
太田 剛史
脳神経外科 部長
くも膜下出血を見逃さないために
脳動脈瘤には、すでにくも膜下出血をきたしている破裂脳動脈瘤と、破裂していない未破裂脳動脈瘤、ふたつの病態があります。くも膜下出血は脳卒中の中でも致死率が高く、見逃すと再出血を繰り返して命を落とすことが多いため、見逃すことのできない病気です。
「突然、頭を殴られたような」激しい頭痛と吐き気嘔吐は、意識障害を伴わない比較的軽症のくも膜下出血の典型的な症状です。頭部CTで診断がつく緊急性の高い疾患ですので、いつでも遠慮なくご紹介ください。また動脈瘤の部位によりますが、時に破裂直前に「まぶたが挙がらない」「ものが二重に見える」と訴えることがありますので、このような症状があった際にもすぐに詳しい検査が必要です。
くも膜下出血(破裂脳動脈瘤)の治療
くも膜下出血(破裂脳動脈瘤)の治療には、ネッククリッピングといって開頭手術で脳動脈瘤の中への血流の流入を防ぐ治療方法と、コイル塞栓術といってプラチナ製形状記憶合金でできた、非常に細く、柔らかいコイルを脳動脈瘤の中に充填するカテーテル治療(コイル塞栓術)があります。
近年、治療の中心はカテーテル治療になりつつありますが、両者にはそれぞれ長所と短所があるため、どちらの治療を行うかの判断は治療成功の重要な要素です。
常に患者さんに応じた最適な治療選択が可能な診療体制
当院は、ふたつの異なる治療を熟知し、いずれの治療も行える二刀流脳神経外科医がほぼ常駐していますので、それぞれの患者さんに最適な治療を24時間365日提供することが可能です。また最新の血管撮影装置を併設した脳神経外科専用手術室(ハイブリッドルーム)で治療を行います。開頭手術とカテーテル治療のどちらを行う場合も診断後に直ちに治療できますので、くも膜下出血という重症疾患を発症した患者さんの移動を最小限に減らすことが可能であり、患者さんの負担を軽減し、より良好な予後につなげることができます。
未破裂脳動脈瘤の治療成績は機器の進歩とともに向上
未破裂脳動脈瘤の治療の目的は、将来の破裂を予防するために行う治療と増大することで周囲の脳症状をきたした症候を治す治療があります。
カテーテル治療に使用する新しい機器はどんどん進歩していて、全国調査では脳動脈瘤の半数以上にカテーテル治療が行われています。近年、最も治療件数を増やしてきたのがフローダイバーターステント留置術です。これは、動脈瘤の中にコイルを入れずに、動脈瘤が発生した血管内にフローダイバーターステントという細かい網の金属の筒を留置することで、動脈瘤を閉塞させてしまう治療です。
少しずつ治療可能な病院が増えてきてはいますが、当院では2011年からこの治療を開始して多様の経験を蓄積しており、いくつか種類があるフローダイバーターステントの全ての使用が可能です。当初は10mm以上の大きさの大型動脈瘤を対象としていましたが、現在は5mm以上の中型動脈瘤に対しても使用が承認されており、未破裂脳動脈瘤の治療を行う際には必須の治療選択になりつつあります。
また、フローダイバーターステント以外にも、これまで血管内治療では難しかった分岐部型脳動脈瘤に対する新しい機器として、動脈瘤内に留置する細かな網目状の袋型のデバイスであるW-EBなど、全国でもまだ限られた施設でしか使用できない機器による治療も当院では行っています。
カテーテル治療の治療成績は、機器の進歩とともに歩んできているものであり、最新の治療による最善の治療が当院では可能です。未破裂脳動脈瘤が発見されて悩まれている患者さんがいらっしゃいましたら、是非当院へご紹介ください。開頭手術、経過観察も含めたベストな治療方針を提供させていただきます。
頚動脈狭窄症の治療は安全かつ低侵襲に
頚部頚動脈狭窄症とは、頚部に位置する内頚動脈起始部から総頚動脈分岐部にかけての動脈硬化性狭窄病変のことです。狭窄が進行したり、一度脳梗塞(塞栓症)をきたすと、内科的治療だけではその後の脳梗塞発症のリスクが高くなり、介入的治療が必要となります。
介入的治療としては、頚部を切開して動脈を露出して動脈内の動脈硬化(プラーク)を切除する頚動脈内膜剥離術(CEA)と、カテーテル治療によるステント留置術(CAS)があります。このふたつの治療は、以前から比較試験が何度も行われてきましたが、近年の研究ではCASとCEAの安全性は同等ですので、患者さんに対する侵襲度の低いCASが国内では2倍以上行われるようになってきています。
当院ではすでに90%以上の症例をCASで治療していますが、脳動脈瘤に対する治療と同じように、CASとCEAそれぞれに長所短所があり、私たち二刀流脳神経外科医は患者さんの状態に合わせて最善の治療方法を選択しています。脳ドックで発見されるような無症候の頚動脈狭窄症も含めて、専門的判断が必要と思われましたら、いつでもご紹介ください。
高難度な脳動静脈奇形や硬膜動静脈瘻もお任せください
脳動静脈奇形は、脳の動脈と静脈が毛細血管を介さずに直接つながっていることで、脳出血やてんかん発作をきたす疾患です。年間出血率は約2%と考えられていますが、一度出血をきたすと一定の期間は破裂率が高くなるといわれています。
治療方針としては、開頭摘出術、カテーテル治療、放射線照射の3つの治療方法を組み合わせて根治を目指すか、とくに治療難易度の高い症例などは経過観察を行うことになります。
根治を目指す際には、開頭手術や放射線治療を単独で行う場合と、それぞれとカテーテル治療を組み合わせて行うことが多く、とくに開頭摘出術の術前にカテーテル治療を行う場合には、前述した両方の治療が可能なハイブリッドルームで治療を行います。手術のことを熟知した二刀流脳神経外科医がカテーテル治療を行うことで、より効果的なカテーテル治療を可能とし、開頭手術の安全性もより高まります。脳神経外科疾患の中で最も難易度が高いといわれる脳動静脈奇形を指摘された患者さんがいらっしゃいましたら、ぜひご紹介いただければと思います。
硬膜動静脈瘻は、脳を包んでいる硬膜を栄養する血管と脳の静脈洞や静脈に連絡ができて耳鳴りや眼の充血を来したり、進行すると脳出血や脳梗塞の原因となる特殊な疾患です。開頭手術や放射線治療を行うこともありますが、治療の多くはカテーテル治療です。詳細な血管診断を基に、綿密な治療計画を立てて行いますので、経験豊富な当科に是非ご紹介いただければと思います。
先生方へのメッセージ
私たち神戸市立医療センター中央市民病院の脳神経外科医は、外科手術と血管内治療を行うことができる二刀流脳神経外科医であることをモットーにしており、ご紹介した病気に加え、急に脳動脈が閉塞した急性脳梗塞に対する血栓回収療法にも脳神経内科、救急部、そしてメディカルスタッフの協力を得て積極的に取り組んでおり、到着から治療開始までの時間が平均40分以下と国内有数の実績を達成しています。「脳卒中になっても困らない街」を実現するためにこれからの精進を続けますので、今後とも何卒宜しくご指導賜りますようお願い申し上げます。
当院への患者紹介方法の詳細はコチラ