心臓病や高血圧、糖尿病、血が止まりにくくなるお薬を服用されるなど、一般の開業歯科医院では治療が困難な方の抜歯や麻酔処置を歯科医院からの紹介で行っています。地域の開業歯科医院と連携していますので、必ず紹介状をお持ちください。虫歯の治療や被せもの、差し歯、ブリッジ、入れ歯の治療、歯周病・インプラントなどの一般的歯科治療は行っておりません。
口腔外科的疾患の取り組み
顎口腔の炎症、顎嚢胞、口腔腫瘍、歯・口腔顎顔面外傷、顎変形症、顎関節疾患、唾液腺疾患、口腔粘膜疾患などの口腔外科的疾患に対して、標準的治療を高い水準で提供できるように努力しています。口腔がんとその他の口腔悪性腫瘍の治療は全て頭頸部外科に集約しており、頭頸部外科の要請時に共同で手術に参画し顎切除・顎骨再建を担当しています。
低侵襲治療への取り組み
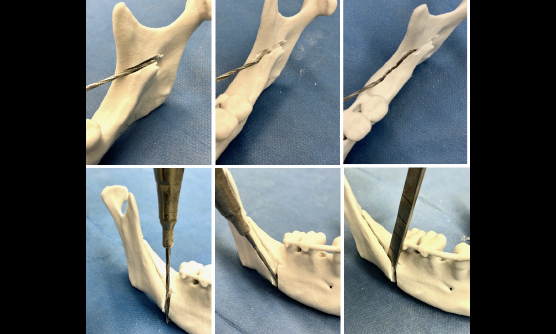
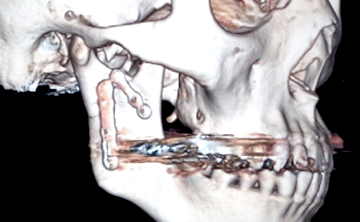
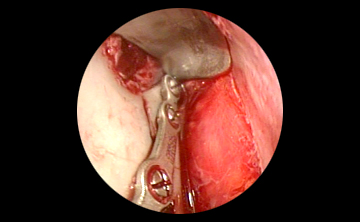
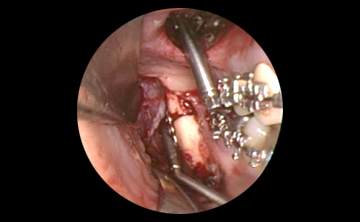
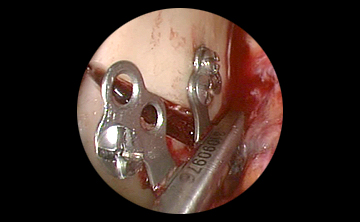
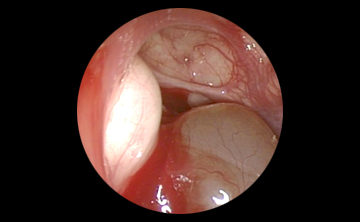
また当科では2003年頃よりいち早く内視鏡を取り入れた低侵襲口腔外科手術に取り組んでいます。下顎骨骨折で高頻度に合併する顎関節突起骨折に対して、口腔内から内視鏡支援下に整復固定を行う内視鏡支援下顎関節突起骨折観血的整復固定術は、顔面の皮膚切開を行うことなく骨折部分を固定するため傷跡を残しません。上下顎骨折手術では手術時に適切な咬合を確立し、術後の顎間固定(ワイヤーで上下の歯を縛って口が開かないようにする処置)を行わない治療を目指します。そのため患者さんは翌日から経口摂取が可能です。
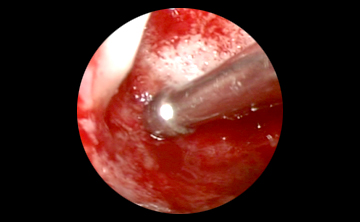
唾石症の治療では唾液腺内視鏡による唾石摘出術や口腔内切開による唾石摘出術に数多く取り組んでいます。ほとんどの場合で顎下腺摘出を回避できており、年間50例程の治療を行っています。唾石摘出術は入院全身麻酔で行いますが、入院期間は3泊4日です。
顎変形症の外科的矯正手術を数多く経験しています
歯列矯正治療のみでは改善できない骨格性不正咬合(顎変形症)の外科的矯正治療を矯正歯科専門医と連携して行っています。手術症例は年間120例以上です。上顎では主としてLe Fort I型骨切り術、下顎では下顎枝矢状分割術や下顎枝垂直骨切り術、オトガイ形成術を行います。手術の組み合わせに関わらず、入院期間は1週間程度で手術翌日から口を開けて食事が可能です。自己血輸血は不要です。また先天性疾患の高度顎変形症では顎骨に対する骨延長術や、形成外科と連携して骨格のみならず軟部組織の改善も目指しています。
2年間の初期研修医、3年間の専攻医制度を設けています
当科は日本口腔外科学会および日本口腔科学会の指定研修機関に認定されています。また病院歯科では全国でも数少ない5年間の口腔外科認定医を目指した研修医制度を設けています。毎年2名の初期研修医(2年制)と1名の専攻医(後期研修医3年制)を全国の優秀な人材から公募しており、毎年多くの歯科医学生の見学や歯科衛生士学生の実習も受け入れています。
口腔外科的疾患:標準的治療を高い水準で
〈医局員〉
歯科口腔外科医療を志す全国の大学歯学部出身者で構成されています。
〈内視鏡手術〉

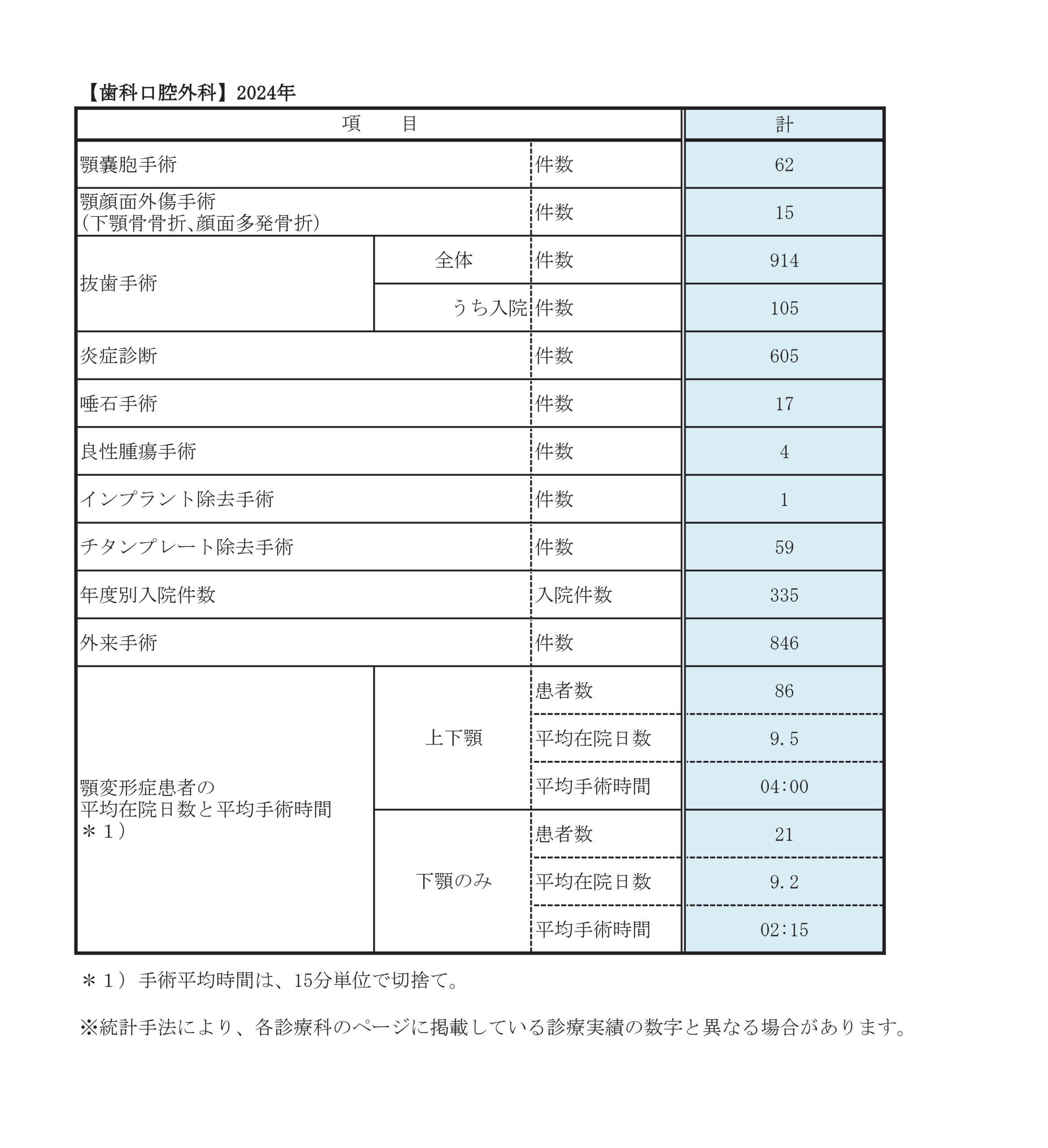
診療実績
歯科口腔外科 2021年度入院手術
| 歯槽骨外科手術(サイナスリフト・骨移植) | 1例 |
|---|---|
| 顎嚢胞手術 | 44例 |
| 顎変形症手術 | 147例 |
| 顎顔面外傷手術 | 11例 |
| 抜歯手術 | 38例 |
| 唾石摘出術 | 25例 |
| 良性腫瘍手術 | 4例 |
| インプラント手術 | 1例 |
| チタンプレート除去手術 | 67例 |
| 年度別入院件数 | 338例 |
| 外来手術 | 563例 |
顎変形症手術の内訳
| 例数 | |
| 上下顎手術 | 121例 |
|---|---|
| 下顎単独手術 | 26例 |
診療科別統計
主な疾患・治療法
顎変形症
歯列矯正治療とあごの骨を外科的に修正する手術を併用して治療することにより正しい噛み合わせを得ることが可能です。
なぜ手術を受けなければならないのですか?
歯の咬み合わせに不具合があることを不正咬合(ふせいこうごう)、なかでも歯の矯正治療のみで治すことができるものを歯性不正咬合(しせいふせいこうごう)といいます。一方、上顎・下顎の形や位置関係に問題があるものを、骨格性不正咬合(こっかくせいふせいこうごう)もしくは顎変形症(がくへんけいしょう)といいます。このような場合、骨格から問題があるために歯の矯正治療単独で治すことはできず、歯列矯正と顎骨の位置関係を修正する手術を併用することで正しい咬み合わせを得ることが可能となります。これを顎変形症に対する外科的矯正治療といいます。
外科的矯正治療は咬み合わせ改善のための治療ですから、美容・整形を主目的とした手術ではありません(そのため健康保険が適応されます)。したがって、不正咬合がみられない場合(単にエラが張っているなど)は、原則として治療の対象とはなりません。必ず矯正歯科医と歯科口腔外科医の協同治療が必要となります。
外科的矯正治療では顎の骨を動かすことになるため、顔を含めて様々な事が変わります。例えば受け口を改善するには下顎を後退させますので、口の中が狭くなったように感じられます。上顎の手術を行えば、鼻や上唇の形は当然変化しますし、鼻詰まりや鼻通りの低下を生じることもあります。メスを入れたところには傷跡や瘢痕が残り、剥離したところは癒着を起こします。咬み合わせの変化に始まり、痺れ、引きつれ感、各種の違和感、顔の動きや表情・形などの軟組織の変化、発音、咀嚼、呼吸、嚥下、顎関節の調子などなど全てが変わると言っても過言ではありません。これらは人それぞれに感じ方が異なり、ご自身以外にはなかなかわかってもらえません。また、術前に変化を正確に予測することもできませんし、術後にそれらを評価・実証する検査もありません。ほとんどの方はこれらの事象に徐々に適応され、しばらくの間は違和感や不自由があるものの咬み合わせをはじめとした多くの改善点を喜んでいただき、治療を受けて良かったと仰っていただくことが大多数です。しかしながら、一部(1%未満)で変化に適応できない方もおられます(事前には医療者側でも予測できません)。ただし、痺れをはじめとした感覚的な変化や見た目の変化など主観的な事は、原因を特定する検査・評価法や絶対に有効であると言える治療法もないため、一度手術を行なえば完全に元の状態に戻すことは不可能です。また、微細な審美的不満などは保険医療であるため、その改善のために再手術を行うことはできません。このようなことも事前に重々ご理解・ご了承いただいたうえで、治療を受けていただくことが肝要です。当科で手術を受けられた方に限らず、他医療機関での治療後に上記のような相談に来られる場合も少なくありませんが、それらの事象が生じてもなお咬み合わせの改善を望むお気持ちがご自身にないのであれば、外科的矯正治療を受けず歯科矯正治療のみにとどめるということも選択枝の一つとしてご自身で決めいただくことが大切です。
治療の流れは?
外科的矯正治療には大きく4つのステップがあります。標準的には全行程で3年程度を要します。
第1段階(術前矯正治療)
手術前に歯の並びや傾斜の修正、咬み合わせ平面の平坦化などを行い、手術後に安定するような咬み合わせを予め作ります。術前矯正治療は、平均1年半から2年程度を要します。
学校や仕事の都合で術前矯正が不十分な時期に手術を希望される方がおられますが、お勧めできません。外科的矯正治療は要件を満たし認可を受けた矯正歯科医院と当院との間では健康保険が適用されます。我が国の保険医療は標準的手法が確立された医療に適用されますので、逆に言うと標準とは異なる独自の手法は認められません(歯の裏側から行う見えない矯正を採用する、手術のみ先に行う、美容整容を目的とした手術、等)。
当科の初診時にはレントゲン、3次元CT、顎関節MRI検査などの予約を行います。
第2段階(入院手術)
術前矯正完了の目処がつけば、矯正歯科医より手術日程を決めてきて下さいと通知されます。その段階になれば、当院での手術日を相談することになります。当科の入院手術は、現状でおよそ1年以上の待機期間があります。ご希望の手術日程に添えない場合も多いのですが、ご容赦下さい。
入院のおよそ3か月前には全身麻酔のための術前検査一式(血液検査・尿検査・胸部レントゲン写真・心電図・顎顔面CTなど)を実施し、手術計画・手術リスクの詳細を再度説明するとともに、同意書をお渡しします。手術の前日に入院していただき、約10日間の入院となります。
なお、1年以上先の手術予定を組むことになりますので、外来診察医と手術担当医が変更となる可能性があります。
第3段階(術後矯正治療)
術後は3か月程度の矯正用ミニ輪ゴムによるリハビリ(後述)を行います。また、矯正歯科医により、歯並びの微調整を行ってもらいます。手術で骨接合用のチタンプレートを使用した場合、術後7-12か月程度経過した時点でプレート除去手術を行います。
第4段階(保定)
歯列矯正治療のワイヤーが除去され、歯並びの安定化を図るための保定装置を日中あるいは夜間のみ使用して、治療終了となります。
対象となる病気(顎変形症)とは?
受け口(下顎前突)や出っ歯(上顎前突)といった上・下の顎骨が大きすぎる場合や逆に小さすぎる場合(口唇口蓋裂による上顎後退や小下顎症)。顔や顎が曲がっている場合(顔面非対称、下顎非対称)や上・下の前歯が噛み合わず開いている場合(開咬症)等、多様なケースがあります。
手術方法はどのようなものですか?
手術は全身麻酔で行います。様々な顎変形に対して幾つかの手術方法がありますが、原則的に手術は口の中から行い、顔の皮膚を切ることはありません。ただし、多量の出血をきたし止血処置を要する場合や術後に気道閉塞をきたす可能性がある場合など緊急時にはその限りではなく、皮膚切開や気管切開を要することがあります(他施設において、術後の出血等が原因で気道閉塞を起こし、死亡または植物状態になった例が報告されています)。
以下に列挙します手術方法を組み合わせて、さまざまな変形に対応します。
まず、上顎に対する手術法について説明します。
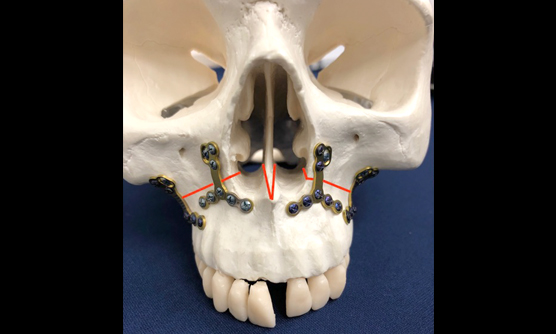
Le Fort I 型(ルフォー1型)骨切り術
上顎全体の移動を行う方法です。上唇の内側の歯肉を切開し、鼻の横くらいから水平に骨を切ります。歯がついた状態で上顎全体を動かせるようになりますので、正しい位置に移動させた後に骨接合用のプレートとネジでしっかりと固定します。当院では、上顎には生体吸収性プレートを主に使用しております。

上顎前方歯槽骨切り術
上顎の前歯部分にのみ問題がある場合に用いる方法です。手術は左右の第1小臼歯(4番目の歯)を抜歯し、その部分の歯槽骨を取り除き、左右の犬歯から犬歯までの6本の前歯を骨ごと切り離し、抜歯して骨を取り除いたスペースに移動させます。正しい位置へ移動後に骨片間をプレートとスクリューで固定し、さらに歯の裏側からオーダーメイドのプラスチック製口蓋床での固定も行います。口蓋床は1か月後に外来で除去します。
次に、下顎に対する手術法を説明します。
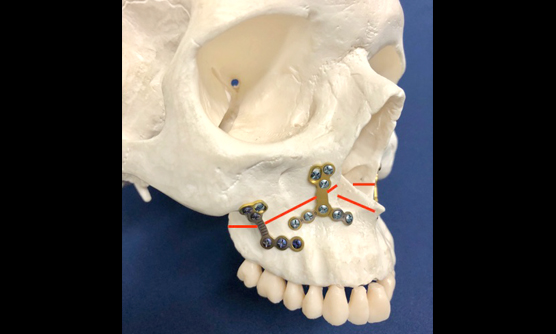
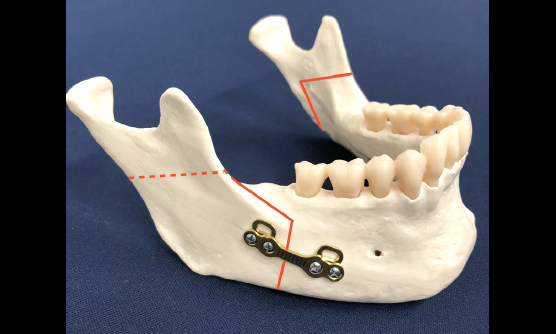
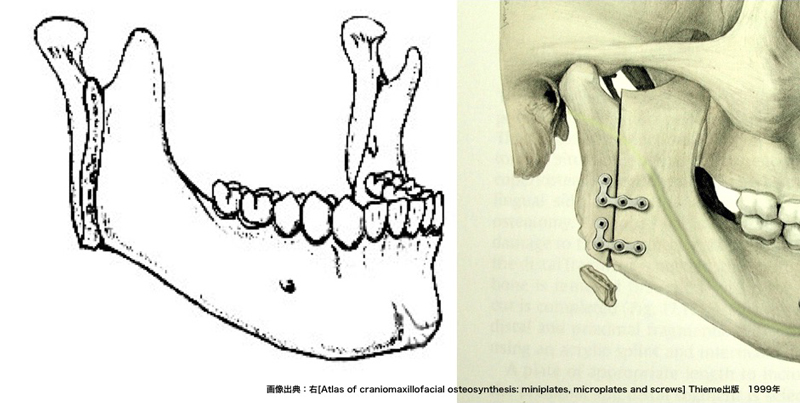
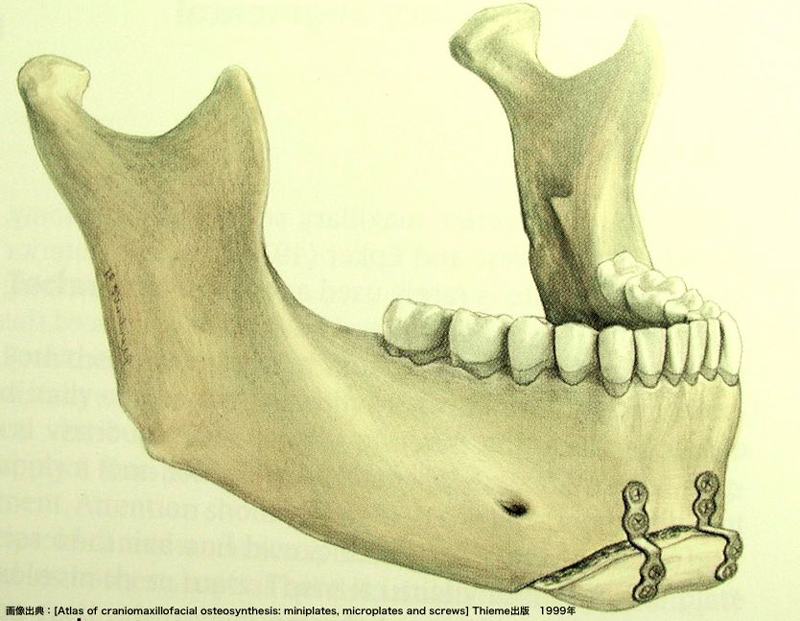
下顎枝矢状分割術(かがくししじょうぶんかつじゅつ)
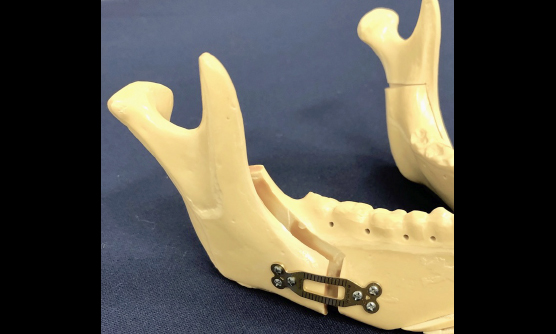
下顎全体を移動させる最も標準的な方法です。親知らずあたりの歯茎・頬粘膜を切開し、骨を内側と外側に分割します。左右両側の骨切り後、外側の顎関節が付いた骨を動かすことなく、歯の植わっている骨のみを正しく咬み合う位置へと移動させます。その後、プレートとスクリューで骨を固定します。
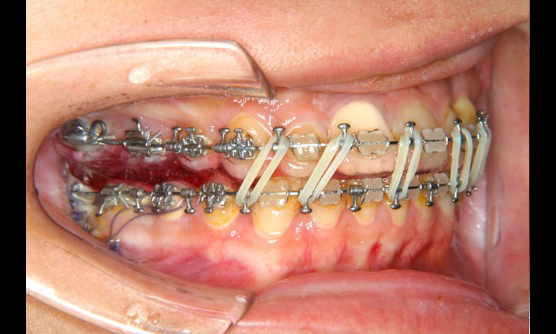
手術当日の顎間固定(上下の歯を細い針金でしばり付ける処置)は行わず、手術翌日から矯正用ミニ輪ゴムによるリハビリを開始します。この手術では親知らずを6か月前までに抜いておく必要があります。
当科では下顎の手術に際しては、咬むという大きな力がかかるためチタンプレートと吸収性プレートを症例によって使い分けています。チタンプレートは吸収性プレートのおよそ5倍の物理的強度を持っています。実際には、どれくらいの負荷が掛かるのかを手術中に判断し、プレートの選択を行います。チタンプレートを使用した場合、別途除去手術を行います。
なお、吸収性プレートは基本的に除去の必要はありませんが、稀に術後異物反応・感染をきたし、追加の手術・処置を要することがあります
下顎枝垂直骨切り術(かがくしすいちょくほねきりじゅつ)
同じく下顎全体を移動させる方法です。やはり親知らずあたりの歯茎・頬粘膜を切開し、顎関節前方の骨を上から下まで垂直に一直線に骨切りし、下顎を左右の関節部分と歯の植わっている部分に分離します。その後、歯の植わっている骨を正しく咬み合う位置へと移動させます。この方法では、分離した骨をプレートなどで固定しない場合が大半ですが、問題なく骨は癒合します。我が国のみならず世界的にも下顎の標準的手術は下顎枝矢状分割術であり、この垂直骨切り術はあまりポピュラーではありませんが、下顎の骨が薄く折れやすい場合などでは有用な方法です。手術当日から翌朝まで矯正用ミニ輪ゴムを用いて口を閉じた状態で安静を図ります。垂直骨切り術は、関節部分の骨が自由になるために顎の移動による顎関節への影響が少なく、顎関節症の患者さんや非対称の治療のように左右で移動量が大きく異なる場合に用いられることがあります。
下顎前方歯槽骨切り術
上顎前方歯槽骨切り術と同様のことを、下顎で行います。
オトガイ形成術
下唇の内側の歯茎を切開し、手術を行います。オトガイと呼ばれる下顎尖端部分の位置や形を修正します。この手術は咬み合わせには関係しませんが、他の手術法で顎の移動を行った後に顔面骨格のバランスを整えるため場合によって行うことがあります。人工物を入れる美容整形とは違ってご自身の骨を移動・修正して、プレートとスクリュー(チタンあるいは生体吸収性)で固定します。
オトガイ形成は、上顎や下顎の移動で咬み合わせを改善した後の顔貌を評価して、担当医が必要と判断すればプレート除去手術時に行います。初回手術後にオトガイ形成をすることで、全体のバランスをみながら微調整が可能となります。
ただし、オトガイ形成にも限界がありますので、手術後にご自分の望まれているような顔貌となるかは予測不能です。また、術野が神経孔(神経の出口)に近接するため、術後に違和感・知覚異常が後遺するリスクが高くなります。
顎骨延長術(がっこつえんちょうじゅつ)
あごの骨が小さい小下顎症の治療では、従来から先に述べた下顎枝矢状分割術を用いて下あごを前方に延ばしていました。しかしその方法ではあごの骨に付着する筋肉や皮膚、あごの骨の中を通る神経や血管が無理矢理引き延ばされ、前方への移動量に限界(およそ15ミリまで)がありました。また手術後にも皮膚や筋肉の引き戻す力で、せっかく移動させたあごの骨が何割か元の位置に戻ってしまうことさえありました。また口唇顎口蓋裂の患者さんの小さな上あごを前方に移動するために、従来からLe Fort I型骨切り術が行われていますが、しばしば過去の手術による瘢痕のために十分な移動が出来ないことがありました。顎骨延長術は延ばしたい骨の部分に骨切り線を入れ、そこに埋め込み式の骨延長器を装着します。手術後にその延長器を作動させ、1日1ミリ程度の極めてゆっくりとしたスピードで延長を開始します。骨と骨の間は日に日に隙間が空いてゆきますが、やがてそこには新しい骨が再生します。しかも骨だけでなく神経や血管といった組織までもが再生します。この方法を用いることで従来は治療が不可能であったトリチャーコリンズ症候群などの重度の顎変形症に対する治療が可能になりました。
手術はこれらの方法を組み合わせてさまざまな変形に対応します。
プレート除去手術
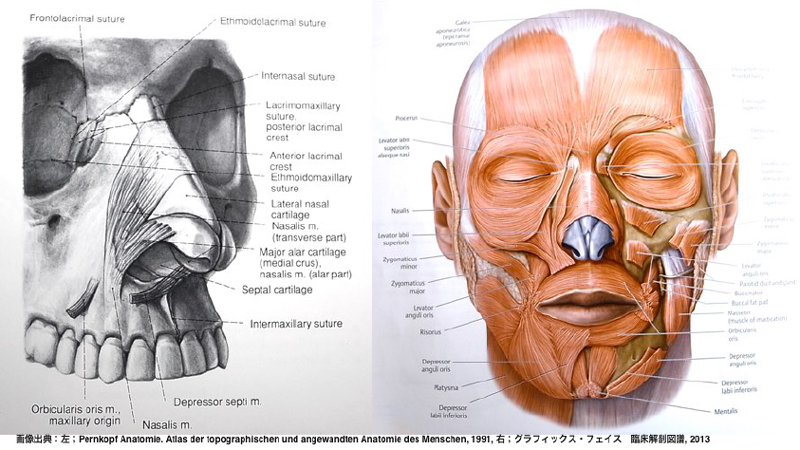
「上顎の手術後に鼻が変形しませんか?」という質問をよくお受けします。結論から言えば上顎の手術をする限り、微妙な鼻の形の変化は避けられないと言えます。鼻の形の変化とは、鼻翼(小鼻の部分)が横に拡がったり、鼻先が上を向いたり、鼻の穴の形が変わったり、ということを指すと思われます。手術後は上唇や鼻の周囲の頬などが術前の1.5–2倍程度の厚みに腫れ上がっていますので、それらが完全に引く術後4–6か月程度までは焦らず様子を見るべきです。それでも鼻の形が術後に違って見えるのには、大きく分けて二つの要因が考えられます。一つ目は、上顎の移動によって口元の形態が変化し、特に鼻と上唇の成す角度が変わることによって形や見え方が違ってくることが挙げられます。鼻は、上顎中央にぽっかり開いた洋梨型の穴の上に乗っかっている軟骨を芯にしたテントのようなものです。地面となる上顎が動けば、その上に乗っかるテントの傾きや形は当然ながら変化します。この変化は、上顎の移動距離が大きくなるほど目立ちやすくなります。
二つ目は、鼻全体の引き締まりが緩んでしまうことが原因ではないかと考えられます。地面の動きはさほどなくともテントを張っているロープが緩むと、テント本体の形も変わってしまうのと同じことです。笑うと小鼻が開くのと同時に、小鼻も口角も上方に引き上がります。これは表情筋(顔面筋ともいう)が動くためです。表情筋とは、顔面の骨から起こって顔面の皮膚に付着する筋肉のことを指します。顔には数多くの表情筋が存在し、特に鼻や口角の周辺には多くの表情筋が密集しています。もちろん鼻にも鼻筋という表情筋が付着しており、鼻翼の周囲には上唇鼻翼挙筋・上唇挙筋といった表情筋が上顎の骨から鼻・鼻翼の皮膚に付着しています。骨との付着部をアンカーにして皮膚を引っ張ることによって表情が生まれます。上顎の手術をする際には、骨を切るためにこれらの表情筋の付着を骨から剥がさなければなりません。プレート固定後に剥がされた表情筋をなるべく元の位置に戻すために、剥がされた左右の筋肉に糸を掛けてたぐり寄せておく必要があります。当科では左右共に2本の糸で牽引し固定しています。また鼻中隔と呼ばれる鼻の真ん中にある軟骨も、上顎の骨に再度固定します。さらに上唇裏側を正中部分でたぐり寄せるような縫合も行います。この3つの牽引縫合で鼻というテントの張りを回復させ、引き締めを図っています。しかしながらこのように細心の注意を払い手術を行っても、数%の方で術後に鼻の形を気にされることがあります。
大多数の方が気にされない程度ではあるものの上顎の手術後には鼻の変化・変形が必ず起こること、場合によっては鼻の容積が変化するため鼻詰まりや鼻通りの低下を生じることがあることを重々ご理解下さい。
手術のリスクはどのようなものがありますか?
次に手術のリスクを説明します。
1.手術中の多量出血のリスク
実際にはほとんど心配ないのですが、万が一大量の出血をきたした場合は止血処置を優先し、手術を中断のうえ後日に延期することがあります。
2.再手術の可能性があります
当科の場合、1.5%前後の確率です。術後異常出血に対する止血処置や矯正装置など迷入異物の除去を要する場合、顎関節の脱臼、手術中に見られなかった咬み合わせの不具合や術後の画像検査でないと判別不能な骨片の不具合などで再度整復固定が必要な場合、等。これらはほとんど入院中に生じますが、まれに退院後の術後感染や異常骨折、骨の癒合不全、プレート破折による不正な咬合の出現などでも再手術を要することがあります。
3.口唇、頬の皮膚・粘膜、歯肉や舌など、いずれかの部位に感覚の痺れが必ず出ます。骨の形や神経の走行、手術法の違いなどで、痺れが強く出る場所は人それぞれです。
通常、半年から1年程度で軽快することがほとんどですが、後遺症として知覚異常・麻痺が遺る方もおられます。40歳代、50歳代と年齢とともに回復は遅れる傾向にあります。
顔面神経麻痺(顔の表情を作る筋肉の運動障害)を生じ、後遺する可能性もわずかながらにあります。
4.顎関節症状
手術後に痛み、雑音、開口障害などの顎関節症状が出現・増悪する場合があります。関節症状を手術で完全にコントロールすることは、残念ながら不可能です。症状が発現した場合には、病態に応じた最善の対応を行います。
5.歯の損傷
骨切り部が歯の生えている部分と近い場合には、術後に歯髄壊死、歯根膜炎、歯根吸収、歯の破折などを生じる可能性があります。こうした症状が確認された場合、歯の修復治療、根管治療、抜歯等の処置が必要になることがあります。
6.術後感染の恐れ
歯にう蝕・感染病巣がある場合や口腔内を不潔にしていると、歯が原因で創部の感染を起こすことがあります。下顎の親知らずについては手術の6か月前までには抜歯が完了している必要があります。また、そもそも唾液中に細菌が存在しているため、口腔内の手術はどうしても術後細菌感染を起こす可能性あります。感染が生じた場合には、創の洗浄や固定したプレートの除去手術などを要することがあります。
7.顔の腫れ、頬や顎まわりのたるみ、上顎の手術を行った場合は鼻の形の微妙な変化が必ず出現します。上顎を動かすため、鼻を含めた何らかの見た目や表情の変化は避けることができません。咬み合わせの改善目的に必要な手術です。
顎の移動量・方向にもよりますが、手術後の腫れは1か月程度で見ず知らずの他人にはわからない程度に軽減していきます。ご自身や親しい方が気付く程度のむくんだ感じは、術後半年ほど持続するのが一般的です。
8.食事や会話の不自由はおよそ1か月程度
術後1か月程度で固い肉を引きちぎったりするようなこと以外は、ほぼ元の食事内容に戻せます。退院前には、電話での会話も可能なことがほとんどです。
9.術後の後戻り
移動した骨には筋肉などの軟組織が付着しているため、手術により軟組織の緊張が生じ、骨を元の位置に戻そうとする力が働きます。これによってしばしば後戻りが生じます。症例により後戻りの量は異なり、術後矯正治療により対処しますが、対処しきれない場合があります。
また、まれに顎関節の頭部分に進行性の形態変化・吸収を生じること(進行性下顎頭吸収)があり、それに伴い下顎の後退や前歯部の開咬(後戻り)を呈し、再手術を要することもあります。原因は解明されていませんが、もともと下顎頭が小さい症例や下顎後退症・開咬症の術後に生じる可能性が高いと報告されています。
これらのリスクを少しでも軽減するためにも、輪ゴム掛けのリハビリ(後述)が重要となります。
10.その他
外科的矯正治療は咬み合わせ改善のために顎の骨を動かす以上、美容手術ではないものの顔を含めて様々な事が変わります。受け口を改善するために下顎を後退させれば、口の中は狭く感じます。上顎の手術を行なえば鼻や上唇の形は当然変化しますし、鼻詰まりや鼻通りの低下を生じることもあります。咬み合わせに始まり、痺れ、引きつれ感、各種の違和感、顔の動きや表情・形、発音、咀嚼、呼吸、嚥下、顎関節の調子などなど全てが変わると言っても過言ではありません。これらは人それぞれ感じ方が異なり、ご自身以外の他人にはなかなかわかってもらえません。また、術前に変化を正確に予測することもできませんし、術後にそれらを評価・実証する方法もありません。ほとんどの方はこれらの事象に徐々に適応されますが、一部(1%未満)で変化に適応できない方もおられます(事前には医療者側でも予測できません)。ただし、痺れをはじめとした感覚的な変化や見た目の変化・不満など主観的な事は、原因を特定する検査や絶対に有効であると言える治療法もないため、一度手術を行えば完全に元の状態に戻すことは不可能です。また、微細な審美的不満などは保険医療であるため、その改善のために再手術を行うことはできません。このようなことも事前に重々ご理解・ご了承いただいたうえで、治療をお受け下さい。
以上の10項目を初診時に説明させていただいております。
また、すべて専門の麻酔科医による全身麻酔のもとで手術を行っています。以前は出血量が増えそうな上・下顎手術では、術前に800mlの自己血を貯血し準備を整え、手術後は気管内挿管のまま集中治療室(ICU)に一泊入室していました。現在では自己血貯血や術後の気管内挿管チューブの留置は行っておりませんが、安全のために手術当日夜は手術室に隣接するハイケアユニット(HCU)で経過観察を行う場合もあります。同様に鼻から入れる経鼻胃管留置による流動食注入もなく、術翌朝から経口摂取を行ってもらいます。また、2003年から治療方法を標準化するクリニカルパスを導入し、ご自身で治療経過を確認しながら安心して入院生活を送っていただけるように努めています。
入院中の療養生活は?
手術直後の数時間はベッド上で安静ですが、その後は徐々に起きて歩くことが可能です。術直後の痛みをご心配される方が多いのですが、実は痛みでお困りになる方は多くはありません。術直後は点滴薬や座薬等で、翌日からは一般的な内服の痛み止めで十分鎮痛可能なことがほとんどです。退院後は、鎮痛剤を必要としない方もおられます。
むしろ痛みよりも麻酔覚醒後の吐き気、手術後の鼻詰まり、鼻血の喉への垂れ込みなどがもっとも辛かった、、、という方が多いようです。麻酔後の吐き気は、一般に車酔いしやすい人に出やすいと言われていますが、吐き気止めの点滴も複数種類準備しておりますので、経過をみながら適宜対応していきます。また、下顎の創部は閉鎖されているため持続吸引ドレーンというチューブを留置し傷の中に貯まった血液を吸い出しますが、上顎は創部と鼻や喉が交通しているため傷口に貯まってくる血液がどうしても鼻から喉へと垂れ込んできます。この血液を飲み込んでしまうと徐々に胃の中に血の塊ができてさらなる吐き気の原因となりますので、あらかじめベッドの枕元に準備されている吸引器を用いて口や鼻からご自身で吸い出すことが大切です。吐き気に関しては、出る方・出ない方がはっきり分かれます。
鼻詰まりは、麻酔の経鼻挿管チューブの影響と手術そのものの腫れによって生じます。入院時に点鼻薬を処方いたしますので、適宜使用して下さい。アレルギー性鼻炎など元々鼻詰まりの持病がある方は、入院前に必ず耳鼻科医の診察を受けお薬などの処方を受けておいて下さい。また、上顎の手術を受けた方は、入院中は強く鼻をかまないで下さい。強く鼻をかみますと骨切り部より頬や目の下の皮下に空気が入り込み、気腫という強い腫れを生じてしまいます。2週間程度、強く鼻をかむのは控えて下さい。
手術によって骨格的な矯正がなされても、術後しばらくは顎周りの筋肉がいうことをきかないため、自力でいい位置まで咬むことができず半開きの状態となります。筋肉が馴染むまで、矯正ワイヤーに取り付けたフックに矯正用ミニ輪ゴムを掛けて、上下の顎を正しい咬み合わせ位置に誘導しながら口を閉じた状態で安静を図る必要があります。翌日以降に担当医からゴム掛けの指導がありますので、食事の際にはご自身で輪ゴムを取り外し、食後に歯磨きをしてから再度ご自身で装着していただきます。最初のうちはゴム掛けが難しく感じられますが、退院までに上手にできるようになれば問題ありません。食事は手術翌朝から流動食を開始し(鼻からのチューブ栄養などはありません)、2日目からは3分粥、それが食べられるようになれば5分粥へとアップしていきます。その他、化膿止めの点滴が術翌日まであります。術後2日目にはシャワー、洗髪も行っていただけます。
退院後の生活は?
通常、退院は手術後8日目が目安です。退院後の痛み止めは不要なことも多く、徐々に食べ物を普通食に戻していくことが可能です(おおよその目安は1か月)。また少しずつ口も開くようになり、噛む力も出てきます。退院後は、まず矯正歯科医の診察を受けて下さい。輪ゴムの掛け方も矯正医の指示に従って下さい。術後1か月もすれば、ゴムを掛けたままでもある程度口が開くようになります。
輪ゴム掛けのリハビリは、概ね3か月程度必要となります。このリハビリが極めて重要で、手術が上手くいってもゴム掛けを怠ると咬み合わせに不具合が遺ることがありますので、くれぐれも担当医師(矯正歯科、口腔外科)の指示に従って下さい。腕や脚を骨折して手術を受けた後、ギプスを巻いて安静を図る必要があることと同じです。また定期的に当院外来に受診していただき、術後6か月以降にレントゲンやCTを撮影し骨の位置や治り方を確認します。
退院後は経過にもよりますが、まだ腫れは残っているものの食事のことを除けば、学校や仕事などの日常生活を普通に送っていただくことが可能な場合がほとんどです。
健康保険が使えますか?
顎変形症は噛み合わせの異常という病気であるため、認可を受けた矯正歯科医院で「顎変形症」との診断を受け、さらに口腔外科で手術が必要と判断された場合、保険医療で矯正治療・手術を受けることが可能となります。矯正治療を自費で受けておられる患者さんは、入院手術に関しても自費治療となります。入院および手術の費用は手術の種類や数および入院日数によりますが、保険医療の対象になる場合は総医療費の3割を自己負担後、高額医療の対象となりますので後日還付があります。一方、自費診療に該当する場合は、下顎のみの手術でおよそ130-160万円、上下両方の手術では280-300万円程度の料金になります。また初診日の診察料から終了まで全ての外来診察料や血液検査・画像検査・お薬に至るまで、すべて自費診療になりますのでご了承下さい。矯正歯科治療を保険診療で行うためには、担当矯正歯科医が保険診療の指定(後述の付記参照)を受けている必要がありますので、詳しくは矯正担当歯科医師にお問い合わせ下さい。
なお、当科には矯正専門医が在籍していないため、近隣の矯正歯科専門医院との連携が必須となります。
付記:顎口腔機能診断算定が可能な指定機関
- 障害者自立支援法施行規則(平成十八年厚生労働省令第十九号)第三十六条第一号及び第二号に規定する医療について、障害者自立支援法(平成十七年法律第百二十三号)第五十四条第二項に規定する都道府県知事の指定を受けた医療機関(歯科矯正に関する医療を担当するものに限る)であること。
- 当該療養を行うにつき十分な専用施設を有していること。
- 当該療養につき顎離断などの手術を担当する別の保険医療機関との間の連携体制が整備されていること。
唾石症
顎下腺などの大唾液腺に生じる唾石症は、唾石が導管を閉塞し食事の際に反復して腫れと痛みを生じる疾患です。発生は圧倒的に顎下腺に多く、しかも顎下腺体から主導管への出口付近(移行部)に好発します。大きさは1ミリ程度のものから1cmを超えるものまで様々です。口腔底の浅い部分を走行する導管内唾石では主に口腔内切開により摘出され、深い部分や移行部、唾液腺体内の唾石では顎下部の皮膚切開による顎下腺摘出術が通常選択されています。唾液腺導管は口腔内への出口が直径0.5mm、内部の主導管でも直径1.5mm程度であり、腺体内部になりますと次々と分岐し1mm未満という細さになります。
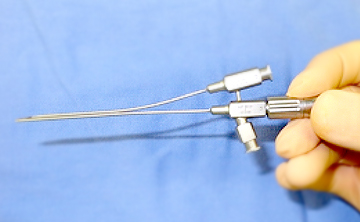
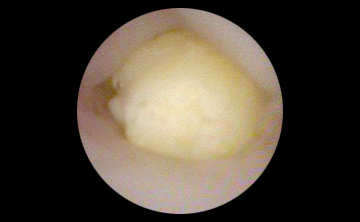
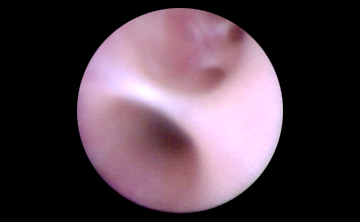
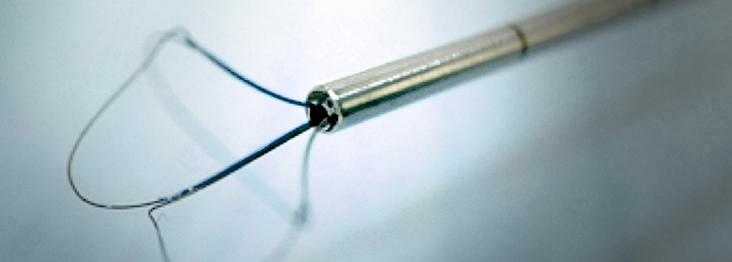
唾液腺内視鏡による唾石摘出術は、直径1.6mmもしくは2.5mmの内視鏡を口腔内の唾液腺管開口部を拡大しながら挿入し、内視鏡内部から唾石把持鉗子を伸展させ唾石を掴み取ってくる方法です。
適応となる唾石症
唾石の直径がおよそ5mm以下、腺体より手前の導管内に存在する場合です。
上記以外の大きな唾石あるいは唾液腺体内部に存在する場合は、内視鏡単独での摘出は不可能ですが、口腔内の小切開(2cm程度)で内視鏡補助や細心の注意を払って触診しながら摘出します。内視鏡単独での摘出が不可能な唾石のほとんどが口腔内切開法で摘出可能であり、顎下腺摘出が回避できております。入院期間は3泊4日です。
内視鏡支援下の治療法
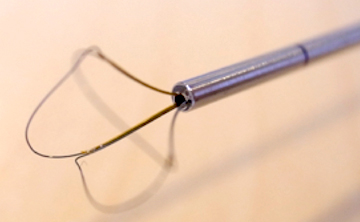
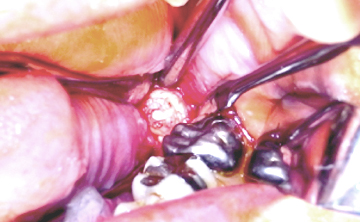
下顎骨関節突起の骨折は従来顎間固定のみの非観血的整復治療が多く、仮に手術となっても耳前部、耳介下部あるいは顎下部皮膚切開で行われました。この方法は骨折部の整復は容易になりますが、顔面に瘢痕を遺し顔面神経麻痺を生じる可能性がありました。内視鏡支援下手術は口腔内切開で顎関節突起を整復固定する方法です。この方法はドイツで開発され実用化されましたが、わずかながら耳前部の皮膚切開を加え、小さな穴を開けて器具を貫通させて治療していました。当科では独自の工夫で現在では皮膚切開を行わない完全口腔内手術を実践しています。
手術適応になるのは、顎関節突起の基底部分もしくは下頸部分で、上頸部分や関節頭は手術適応にはなりません。
先天性顎骨低形成の骨延長手術では、通常の後天性の疾患とは異なり、術野が狭く形態的にも手術の難易度が上がります。内視鏡支援下の骨切り、骨延長器装着、骨接合プレート装着が可能となり、より安全で確実な手術を行っています。
下顎骨および上顎骨に生じた歯原性腫瘍などの摘出においても、内視鏡を使用することにより、肉眼では見えない部分が見えるようになり、かつ局所の視野が拡大されることによって腫瘍の取り残しが無くなり、再発率が下がります。また神経損傷のリスクが低減されます。
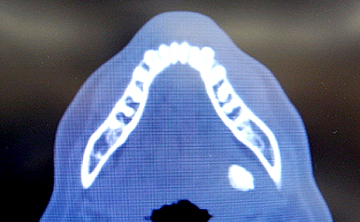
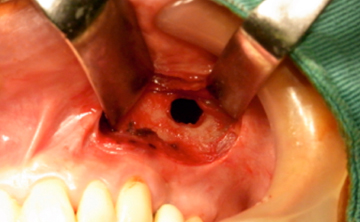
歯やインプラントなどの上顎洞内迷入異物の摘出は、口の中から歯肉を1〜2cm切開し、上顎洞壁に開けた直径5mm程度の小さな穴から摘出することが可能です。
内視鏡を使用すれば、少し離れた場所から小さな窓を開けるだけで摘出できるため、その後の歯やインプラント治療に支障をきたしません。
下あごの非常に深い位置に埋伏した親知らずの抜歯にも内視鏡を応用しています。通常であれば絶対に直視できない場所ですが、奥歯の内側の歯肉から内視鏡で見ながら皮膚を切ることなく抜歯しています。
臨床研究
歯科口腔外科に受診中の患者さんへ 臨床研究の実施に関するお知らせ
現在歯科口腔外科では、下記の臨床研究を実施しております。
この研究では、患者さんの日常診療で得られたデータ(情報)を利用させていただきます。
ご自身のデータがこの研究に利用されることについて、異議がある場合は、情報の利用や他の研究機関への提供をいつでも停止することができます。研究の計画や内容などについて詳しくお知りになりたい方、ご自身のデータがこの研究で利用されることについて異議のある方、その他ご質問がある方は、以下の「問い合わせ先」へご連絡ください。
| 研究課題名 | 当院責任者 | 説明文 (PDF) |
| BSSOにおける近位骨片の位置変化および術後安定性の三次元的評価 | 山本信祐 | |
|---|---|---|
| Le Fort I 骨切り術による上顎の移動量と鼻唇部の軟組織変化に関する3次元的評価 | 山本信祐 | |
| Le Fort I osteotomyにおけるCAD/CAMスプリントの適応と限界 | 山本信祐 | |
| 両側下顎骨関節突起骨折を伴う下顎骨正中部骨折における下顎幅径の術後安定性に関する検討 | 前田圭吾 | |
| u-HA/PLLAを用いた上顎骨形成術の術後安定性に対する3次元的評価 | 山本信祐 | |
| 顎矯正手術後の悪心・嘔吐の予防に対するグラニセトロンおよびオンダンセトロンの有用性 | 前田圭吾 |
| 当院における連絡先 | 神戸市立医療センター中央市民病院 歯科口腔外科部長 谷池 直樹 〒650-0046 神戸市中央区港島中町4-6 TEL:078-302-4321, FAX:078-302-2487 |
|---|