糖尿病内分泌内科の外来での予約患者数は糖尿病患者約3800人・内分泌内科約1700人で、1日平均患者数は約100人です。また年間糖尿病約160人・内分泌約200人の患者さんが入院されています。
糖尿病の教育・治療のためにはチーム医療が大切であり、医師・看護師・管理栄養士・薬剤師・検査技師によるカンファレンスを行い、情報を共有し総合的に糖尿病教育・治療を行っています。理学療法士も糖尿病教室などの教育に携わっています。また、進展した糖尿病で問題となる合併症については、他の科と連携して精密検査及び治療にあたっています。糖尿病性腎症で進行した腎不全では腎臓内科と、虚血性心疾患の評価・治療では循環器内科と、糖尿病性網膜症の評価・治療では神戸アイセンター病院と密に連絡をとっています。妊娠糖尿病症例・糖尿病合併妊娠症例も産科と協力して加療しています。糖尿病専門医は常勤4人で、糖尿病療養指導士も看護師、薬剤師、管理栄養士、理学療法士・検査技師と多彩な職種におよんでいます。
内分泌疾患は希少疾患も多く非常に専門性の高い領域です。当科には内分泌代謝専門医が2名在籍しており、正確な診断と治療を行うように努めています。下垂体疾患の多くは厚生労働省より指定難病に認定されており、当科ではその診断と治療について対応可能です。甲状腺疾患ではバセドウ病に対する放射性ヨウ素内用療法(アイソトープ治療)や甲状腺眼症の治療も行なっています。高血圧症は5〜15%が原発性アルドステロン症という内分泌疾患が原因と言われており、日本内分泌学会のガイドラインに従って適切な高血圧治療につなげています。最近では癌に対する免疫治療を行なった際に甲状腺や下垂体の機能異常を発症される患者さんが増えており、担当の診療科と共同で診療を行なっています。
内分泌臓器の腫瘍は外科的治療が必要になることが多く、関連の診療科と協力して診療にあたっています。特に甲状腺癌においては、穿刺吸引細胞診での診断、手術時の周術期管理、放射性ヨード治療、術後ホルモン補充療法、分子標的薬治療などを、頭頸部外科・腫瘍内科と連携して診断から治療までを一貫して行っています。当院には、全国的に数が少ない「甲状腺癌の放射性ヨード治療室」を2室有しており、他院で手術を受けた患者さんも積極的に紹介を受け、治療を行っています。
神経内分泌腫瘍の放射性同位元素(ルテチウム177)を用いたペプチド受容体放射性核種療法が2021年より国内でも可能となりました。当科でも同治療も開始しており、良好な成績を得ています。
当科では病診連携を積極的に行っており、地域医療機関からの紹介を多数受け入れています。一方、状態が安定した患者さんには地域医療機関(診療所)に今後の治療を依頼しています。その場合も、必要に応じて地域医療機関からの紹介により当院で治療を行います。
他院で治療中の方が当院他科で入院される場合も連携して血糖コントロールや内分泌疾患の管理を行っています。
医師、看護師(病棟・外来)、管理栄養士、薬剤師、検査技師、理学療法士

〈甲状腺癌チーム〉
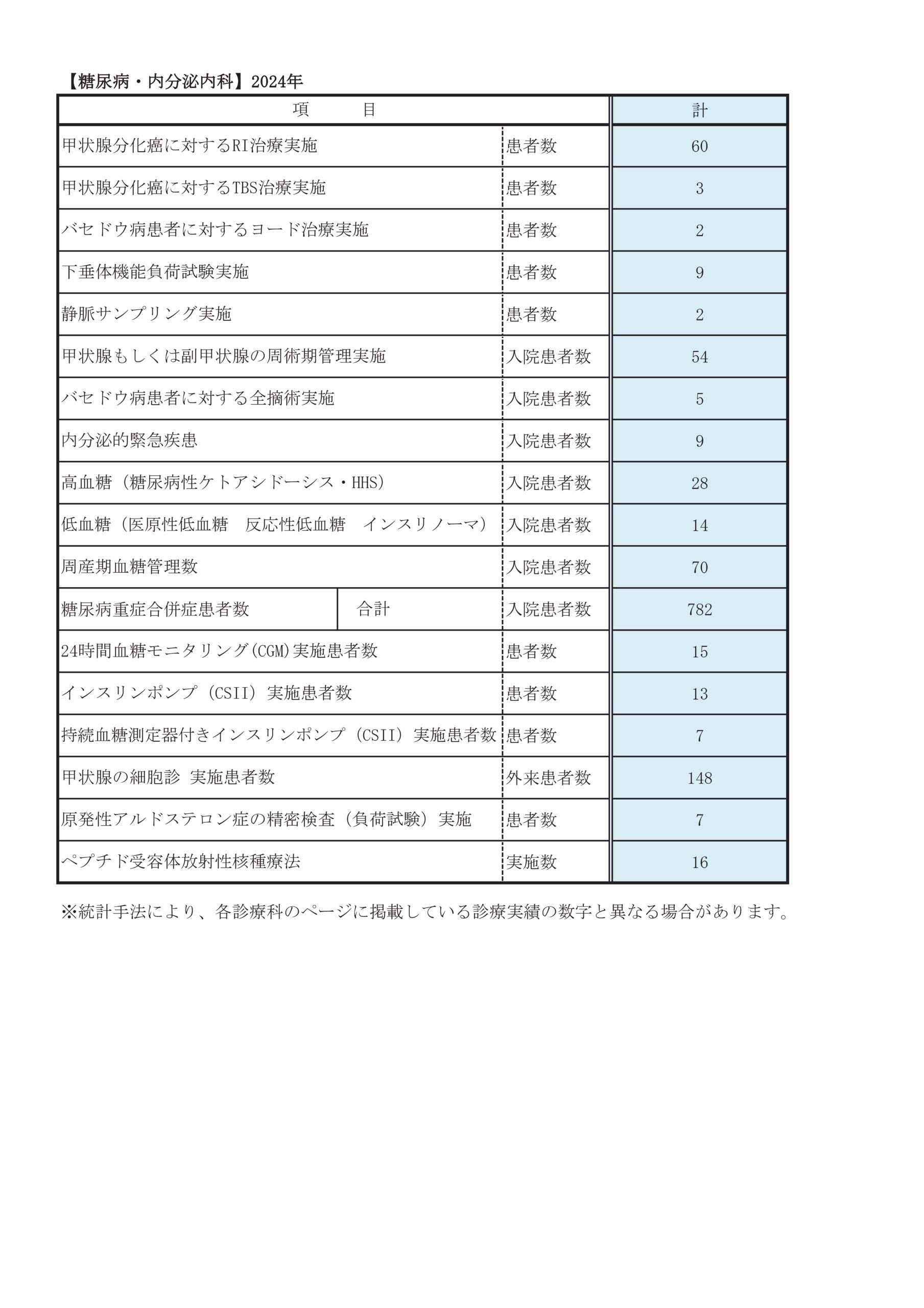
診療実績
重症低血糖昏睡
毎年増加し、年間50名の救急入院があります。インスリン・SU剤・高齢者・腎機能低下がキーワードであり、当科では重症低血糖を起こしにくい薬の選択と患者指導を徹底的に行うと共に危険性について注意喚起を広く行っています。
1型糖尿病
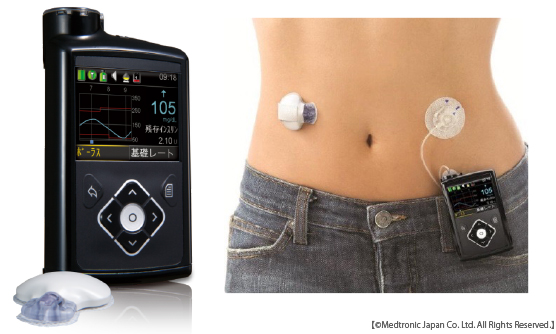
約100人の1型糖尿病成人患者さんが通院されています。1型糖尿病の治療は2型糖尿病とは大きく異なり、患者さん個々の生活にあわせた治療が必要です。
持続血糖測定器(CGM)とインスリンポンプ(CSII,SAP)
新しい医療機器も導入し、糖尿病治療現場での有効な活用をはかっています。
甲状腺分化癌に対する放射性ヨウ素内用療法
| 2018年度 | 2019年度 | 2020年度 | 2021年度 | 2022年度 | 2023年度 | 2024年度 | |
|---|---|---|---|---|---|---|---|
| 放射性ヨウ素内用療法総数(人) | 85 | 96 | 84 | 90 | 63 | 53 | 73 |
| 当院手術例(人) | 25 | 29 | 28 | 26 | 12 | 11 | 21 |
| 他院手術例(人) | 60 | 67 | 56 | 64 | 51 | 42 | 52 |
原発性アルドステロン症
| 2018年度 | 2019年度 | 2020年度 | 2021年度 | 2022年度 | 2023年度 | 2024年度 | |
|---|---|---|---|---|---|---|---|
| 原発性アルドステロン症負荷試験入院(人) | 19 | 26 | 15 | 7 | 5 | 6 | 9 |
| 副腎静脈サンプリング検査(件) | 5 | 9 | 11 | 0 | 0 | 0 | 2 |
ペプチド受容体放射性核種療法
| 2021年度 | 2022年度 | 2023年度 | 2024年度 | |
|---|---|---|---|---|
| 延べ人数 | 2 | 18 | 16 | 15 |
診療科別統計
主な疾患・治療法
患者様向け情報提供サイト「インスリンポンプ.jp」
「インスリンポンプ.jp」はこちら2型糖尿病は、インスリン分泌が残っている状態で、生活習慣の乱れなどが原因で糖尿病になっているものですが、健康な人よりもインスリン分泌は低下しているとされています。食事療法、運動療法で血糖が改善しない場合は薬物療法を追加します。
糖尿病ではないのに妊娠中に血糖が高くなる病態で一般の糖尿病より厳しい診断基準となっています。胎児への影響を考えて血糖のコントロールにはインスリン注射を用います。多くの場合は出産後正常にもどりますが、将来糖尿病になりやすいとされています。産科と協力して血糖管理しています。
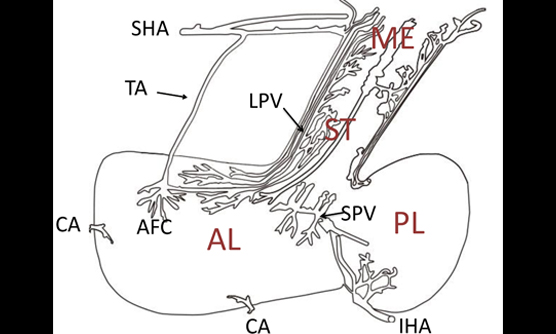
主な内分泌臓器には、視床下部、下垂体、甲状腺、副甲状腺、膵臓、副腎、卵巣、精巣などがあります。これらの臓器からは、さまざまな働きを持つ物質(ホルモン)が血液中に分泌され、全身の臓器に作用して体の恒常性を維持しています。
内分泌疾患は大きく分けて、ホルモンが過剰に分泌されている状態(機能亢進)、ホルモンが不足している状態(機能低下)、内分泌臓器に腫瘍が発生している状態に分けられます。これらの疾患の中には、他の疾患と症状が似ているため区別が難しい場合もあり、正確な診断と適切な治療が重要となります。 正確な診断のために、安静や絶食などの状態での血液検査、数日間の入院による薬剤投与後の血液検査などが必要となることがあります。さらに、超音波検査、CT、MRI、シンチグラフィなどの画像検査や静脈サンプリングなどを行って、病変の性質や部位を詳細に調べます。
バセドウ病は、甲状腺を刺激する自己抗体が作られることで発症します。この影響で、甲状腺が腫れたり、甲状腺ホルモンが過剰に作られたりします。女性に多い病気で、場合によっては目が飛び出して見える症状が出ることもあります。
甲状腺ホルモンが過剰に作られると、食欲があるのに体重が減る、汗をかきやすくなる、微熱が続く、心臓がドキドキする、動くと息切れがする、手が震える、下痢をするなどの症状が出ることがあります。
治療にはいくつかの方法があります。ひとつは、抗甲状腺薬という飲み薬を使用する方法です。この薬には副作用が出ることがあるため、注意深く経過を観察しながら治療を進めます。通常、数年以上薬を服用する必要があります。もうひとつは、放射線ヨウ素治療(アイソトープ治療)という方法です。この治療では、放射性ヨウ素(I-131)を内服し、甲状腺細胞を破壊します。ただし、この治療を受けた場合、多くの場合でその後、甲状腺ホルモンを補う薬が必要となります。また、手術で治療する方法もあります。これは、甲状腺が大きく腫れている場合や抗甲状腺薬が使用できない場合に行われます。手術で甲状腺を全て取り除くため、術後には甲状腺ホルモンを補う薬が必要となります。
橋本病は、甲状腺に慢性的な炎症が起きる病気です。この病気では、甲状腺が腫大し、一部の人で甲状腺ホルモンの分泌が減少することがあります。甲状腺ホルモンの分泌が減少すると、体にさまざまな不調が現れる場合があります。たとえば、むくみが生じたり、寒さに弱くなったり、便秘になりやすくなったりすることがあります。甲状腺ホルモンの分泌が減少している場合には、甲状腺ホルモン補充療法(ホルモンを補う治療)を行います。
また、ヨウ素を摂りすぎると、甲状腺ホルモンの分泌がさらに悪くなることがあります。ヨウ素は昆布などの海藻に多く含まれているため、これらの食品を摂りすぎないよう注意が必要です。
良性と判断された場合には、定期的に診察や検査で経過を観察します。一方で、悪性の可能性がある場合は、手術で甲状腺を取り除きます。甲状腺がんの手術後には、放射性ヨウ素(I-131)を用いた治療が行なわれることもあります。また、病気の進行が速い場合には、新しいタイプの抗がん剤である「分子標的薬」を用いた治療を腫瘍内科と協力して行うこともあります。
甲状腺がんの治療法の一つとして、甲状腺を全摘出した後に「放射性ヨウ素(I-131)内用療法」を行うことがあります。この治療法は、世界中で古くから行われてきた安全性と有効性が確立された方法です。
転移がある場合は、この治療を半年から1年ごとに繰り返し行います(治療)。一方、転移がない場合でも手術後にこの治療を受けることで、残存する正常な甲状腺細胞を破壊して経過観察を簡略化したり(アブレーション)、わずかに残っている癌細胞を破壊して再発を予防したり(補助療法)します。
I-131は甲状腺の性質を持つ細胞だけに取り込まれ、ベータ線という放射線を放出して細胞を破壊します。この放射線は1~2ミリ程度の範囲にしか届かないため、周囲の臓器に与える影響は最小限に抑えられます。主な副作用としては嘔気や味覚障害などがありますが、通常1週間程度で回復します。
治療は、I-131の入った小さいカプセルを服用するだけです。ただし、治療にはいくつかの準備が必要です。まず、甲状腺を全摘出していること、次に甲状腺ホルモン剤を中止すること、そしてヨウ素を含む食事を控えることが必要です。甲状腺ホルモン剤を中止すると、むくみや便秘、食欲の低下といった症状が現れることがあります。また、治療後しばらくの間は体外に放射線が放出されるため、数日間、隔離された治療室で過ごしていただきます。当院の治療室は6階にあり、窓から外の景色が見える環境です。全国的に治療室の数は限られていますが、当院には2部屋あり、年間約100名の治療が可能です。当院では治療の確実性を高めるため、11日間の入院期間を設けています。
当院では、他院で手術を受けられた患者さんも放射性ヨウ素内用療法を多数実施しています。治療をご希望の場合は、担当医師にご相談の上、当院の地域医療連携センターを通じて内分泌内科の外来予約をお取りください。
下垂体腫瘍の中には、ホルモンを過剰に分泌するものがあります。このような腫瘍が原因で、特定の病気が引き起こされることがあります。たとえば、成長ホルモンの過剰分泌によって「先端巨大症」が、副腎皮質刺激ホルモンの過剰分泌によって「クッシング病」が、プロラクチンの過剰分泌によって「プロラクチノーマ」という病気が生じます。これらの治療には、脳神経外科との連携で腫瘍を除去する手術のほか、薬物治療や放射線治療も用いられます。また、ホルモンを分泌しない腫瘍であっても、腫瘍が大きくなると視野の狭窄などの症状を引き起こすことがあり、その場合も手術が必要です。
一方で、下垂体が障害を受けるとホルモンが十分に分泌されなくなる場合があります。たとえば、副腎皮質刺激ホルモンが不足すると、疲労感や食欲不振が生じることがあります。成長ホルモンの不足では、疲労感や体脂肪の増加がみられることがあります。また、性腺刺激ホルモンが不足すると不妊や月経が止まることがあり、抗利尿ホルモンが不足すると多尿が生じることがあります。しかし、適切なホルモン補充療法を行うことで、これらの症状は改善し、通常の日常生活を送ることが可能です。
副腎は、左右の腎臓の上に位置する小さな三角形の臓器です。副腎からは、血圧や代謝を調整するコルチゾール、アルドステロン、カテコラミンなどのホルモンが分泌されています。
副腎腫瘍の中には、ホルモンを過剰に分泌するものがあります。このような腫瘍が原因で、特定の病気が引き起こされることがあります。たとえば、 コルチゾールが過剰に分泌される「クッシング症候群」では、高血圧、糖尿病、顔が丸くなる、お腹まわりの肥満、皮膚が薄くなり傷つきやすくなるといった症状が見られます。アルドステロンが過剰に分泌される「原発性アルドステロン症」では、高血圧や血液中のカリウムの減少が見られます。カテコラミンが過剰に分泌される「褐色細胞腫」では、高血圧、動悸、大量の汗、頭痛などの症状が発作的に現れることがあります。
これらの病気を診断し、治療方針を決めるためには、詳細な検査が必要です。検査には、ホルモンの働きを調べる機能検査、CTやシンチグラフィなどの画像検査、さらに副腎静脈サンプリング検査などがあります。これらの検査を基に、手術が必要かどうかを判断します。手術が必要と判断された場合は、泌尿器科へ紹介します。
また、最近ではCT検査などで、症状がなくても偶然副腎に腫瘍が見つかるケースが増えています。これらの多くは良性ですが、腫瘍が大きい場合やホルモンが過剰に分泌されている場合には、手術が勧められることがあります。
原発性アルドステロン症は、副腎からアルドステロンというホルモンが過剰に分泌されることで発症する病気です。この病気では、高血圧や血液中のカリウム濃度の低下が見られます。最近の研究から、高血圧患者の約5~15%がこの病気に起因すると考えられています。
原発性アルドステロン症は、通常の高血圧と比較して、心筋梗塞、心肥大、心不全、不整脈、脳卒中、腎不全といった合併症のリスクが高いとされています。しかし、適切な診断と治療を受けることで、これらの合併症を予防することが可能です。
この病気には主に2つのタイプがあります。一つは、副腎にアルドステロンを過剰に産生する腫瘍ができる場合(アルドステロン産生腺腫)で、通常は片側の副腎に発生します。もう一つは、副腎の細胞が増殖することで起こる場合(過形成)で、両方の副腎に異常がみられることが多いです。
診断には、まず血液検査でレニン活性とアルドステロン濃度を測定します。この検査で異常が認められた場合、確定診断のために機能確認検査を行います。機能確認検査では、薬を使用したり生理食塩水を点滴したりして、ホルモン分泌量を調べます。当院では、これらの検査を正確に行うために、2泊3日の入院で実施しています。
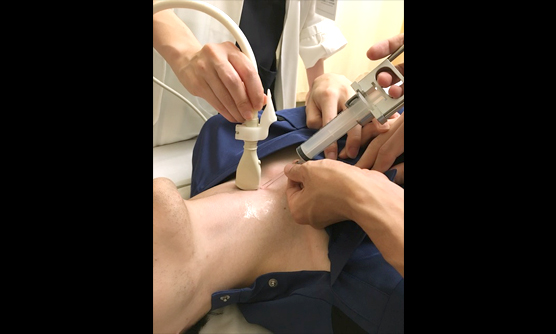
原発性アルドステロン症と診断された場合、問題がある副腎の部位を特定するための検査(副腎静脈サンプリング)を行うことがあります。この検査では、足の付け根から細い管を挿入し、左右の副腎から採血を行います。当院では、この検査も2泊3日の入院で実施しています。
検査の結果、片側の副腎だけに異常がある場合は、泌尿器科に依頼し、異常のある副腎を摘出します(入院期間は約1週間です)。一方、両側の副腎に異常がある場合は、アルドステロンの作用を抑える内服薬による治療を行います。
副甲状腺は、甲状腺の裏側にある非常に小さい臓器で、通常4つ存在します。この臓器は、副甲状腺ホルモンを分泌し、体内のカルシウム量を調節する重要な役割を担っています。
原発性副甲状腺機能亢進症は、副甲状腺に腫瘍ができ、副甲状腺ホルモンが過剰に分泌される病気です。その結果、血液中のカルシウム濃度が異常に高くなり、骨がもろくなったり(骨粗鬆症)や尿路結石ができたりといった症状が現れることがあります。この病気の治療には腫瘍を摘出する手術が一般的ですが、症状が軽い場合は経過観察が選択されることもあります。診断には、ホルモン検査や画像検査が用いられます。
一方、副甲状腺ホルモンが不足すると、血液中のカルシウム濃度が低下し、手足のしびれや筋肉のこわばりなどの症状が生じることがあります。この場合、治療としてビタミンDやカルシウム製剤が投与されます
膵臓は、お腹の奥、胃の裏側にある臓器です。膵臓には、消化を助ける消化液を分泌する役割(外分泌)と血液中にホルモンを分泌する役割(内分泌)があります。特に内分泌では、血糖値を下げるインスリンや血糖値を上げるグルカゴンといったホルモンを分泌し、体内の糖代謝を調節しています。
インスリンを過剰に分泌する腫瘍(インスリノーマ)ができると低血糖を引き起こすことがあります。この病気の診断には、絶食試験や選択的動脈内カルシウム注入試験が用いられます。治療方法としては、手術による腫瘍の摘出が一般的です。
神経内分泌腫瘍は、ホルモンを分泌する神経内分泌細胞から発生する腫瘍で、体内の様々な臓器、特に膵臓、消化管、肺に多く見られます。神経内分泌腫瘍に対する薬物療法は選択肢が限られており、特に手術で治療できない場合には治療法が限られることが課題となっています。しかし、欧米で使用されてきた放射性同位元素(ルテチウム177)を用いたペプチド受容体放射性核種療法(PRRT)が、2021年に日本でも承認され、新たな治療法として注目されています。
PRRTは、腫瘍に存在する「ソマトスタチン受容体」に結合する薬剤を注射し、体内で放射線を照射して腫瘍を治療する方法です。この治療法は国際的な臨床試験で効果が確認されており、治療効果に期待が寄せられています。
当院では、この治療を2泊3日の入院で行っており、8週間ごとに4回繰り返します。治療を開始する前には、腫瘍にソマトスタチン受容体が存在するかどうかを確認するため、オクトレオスキャンという検査が必要です。
他の病院で治療中の方でPRRTを希望される場合は、担当医師とご相談の上、当院の地域医療連携センターを通じて内分泌内科外来の予約をお取りください。
甲状腺眼症は、バセドウ病や橋本病といった甲状腺の病気に関連して起こる目の病気です。この病気では、目の奥の組織に炎症が起こり、目が突出して見える、物が二重に見える、視力が低下するなどの症状が現れ、日常生活に大きな支障をきたすことがあります。
甲状腺眼症の原因は、TSH受容体に対する自己免疫反応が関与していると考えられています。また、遺伝的な体質や喫煙などの生活習慣も、発症に影響を与えることがわかっています。
治療方法は症状の重さや進行具合によって異なります。症状が軽い場合は、定期的に様子を見ながら、目薬や局所注射などで症状を和らげる治療を行います。症状の重い場合には、ステロイドの点滴治療や放射線治療を行い、炎症を抑え症状の悪化を防ぎます。また、炎症が治まった後には、目の手術を行って、見た目や視力の改善を目指すこともあります。
2024年に「テプロツムマブ」という新しい薬が承認されました。この薬は、目の奥の炎症を抑え、眼球突出を改善する効果があります。従来のステロイド治療では1か月程度の入院が必要でしたが、この薬は3週間ごとに計8回の点滴を外来で行うだけで済むため、患者さんの負担軽減が期待されています。ただし、副作用として聴覚障害や血糖値の上昇が報告されており、注意深い管理のもとで投与する必要があります。
患者様向け情報提供サイト「甲状腺眼症.jp」
甲状腺眼症.jpはこちら https://www.kojosen-gansho.jp
低ホスファターゼ症(HPP)は、稀な遺伝性の代謝性骨疾患です。この病気は、ALPLという遺伝子の変異により、体内でアルカリホスファターゼ(ALP)という酵素が十分に働かなくなることが原因で起こります。小児期までに診断されることが多いですが、大人になってから見つかる場合もあります。
成人期のHPPでは、骨折や偽骨折、骨や関節の痛み、筋肉の痛みや筋力低下などの症状が現れ、日常生活に支障をきたすことがあります。これらの症状は他の病気と似ているため、診断が難しい場合も少なくありません。
診断の際には、血液検査で血清ALP値が低下していることが重要な手がかりとなります。さらに、尿検査でホスホエタノールアミンという物質が増えていることを確認したり、遺伝子検査を行ったりすることで確定診断が可能です。
治療には、ALP酵素補充療法(アスホターゼ アルファ)が用いられます。この治療により、HPPの症状が緩和され、生活の質の向上が期待されます。
患者様向け情報提供サイト「HPPガイド」
HPPガイドはこちら https://hpp-life.jp
臨床研究
糖尿病内分泌内科に受診中の患者さんへ 臨床研究の実施に関するお知らせ
現在糖尿病内分泌内科では、下記の臨床研究を実施しております。
研究では、患者さんの日常診療で得られたデータ(情報)を利用させていただきます。ご自身のデータが研究に利用されることについて、異議がある場合は、情報の利用や他の研究機関への提供をいつでも停止することができます。研究の計画や内容などについて詳しくお知りになりたい方、ご自身のデータが研究で利用されることについて異議のある方、その他ご質問がある方は、「問い合わせ先」へご連絡ください。
| 低アルカリフォスファターゼ血症の検出頻度とその臨床的特徴 | 籏谷雄二 | |
| チロシンキナーゼ阻害薬投与中に発症する原発性副腎不全の臨床的特徴 | 籏谷雄二 | |
| 難治性の稀少癌(甲状腺未分化癌、肺小細胞癌、脳神経膠腫など)患者におけるVHH抗体を用いたバイオマーカー探索研究 | 籏谷雄二 | |
| 神経内分泌腫瘍における177Lu-DOTATATEの集積と治療効果の検討 | 藤本寛太 | |
| 研究課題名 | 研究責任者 (問い合わせ先) |
説明文 (PDF) |
|---|
お知らせ
糖尿病教室 WEB上で医師・コメディカルからの情報発信を行っております。
糖尿病教室