現在皮膚科は7名のスタッフを擁し24時間365日皮膚科領域の救急疾患に対応しつつ、日々の診療を続けております。当院は35診療科を有する県下最大級の病院であり、様々な合併症を持たれた皮膚疾患の患者様を安心してご紹介をいただけるのも、当科の大きな特色と考えています。
通常の皮膚疾患に対応するのはもちろんですが、一般病院、開業医の諸先生方が治療に難渋する重症例、非典型例にも積極的に対応し、重症例に対しては入院加療をお勧めしています。
皮膚科がカバーする疾患は多岐にわたりますが、次のような疾患を数多く受け入れています。
腫瘍
悪性黒色腫をはじめ有棘細胞癌、基底細胞癌、乳房外パジェット病など皮膚悪性腫瘍に対し手術、化学療法、放射線療法を組み合わせベストな治療を提供しております。 特に予後の悪い疾患として有名な悪性黒色腫の治療の風景は免疫チェックポイント阻害薬の登場により一変したといっても過言ではありません。悪性黒色腫に対し免疫チェックポイント阻害薬を使用できるのは日本皮膚科学会認定の皮膚悪性腫瘍指導専門医もしくは日本臨床腫瘍学会認定のがん薬物療法専門医の在籍施設のみであり、皮膚悪性腫瘍指導専門医が在籍するのは当院を含め兵庫県下では4施設しかありません。
感染症
蜂窩織炎、壊死性筋膜炎などの重症細菌感染症、汎発性帯状疱疹など重症ウィルス性感染症などでは 積極的に入院していただき感染症科と連携し無駄のない薬剤選択を行っています。特に壊死性筋膜炎では早期の外科的介入を行い良好な成績を納めています。
炎症性疾患
尋常性乾癬は治らない皮膚科の疾患として有名でしたが、各種生物学的製剤(現在10種類が上梓されています)の導入により、難治例を見ることが極めて少なくなりました。高額の医療費がかかる点が難点ですが、乾癬に悩まされてきた患者QOLのアップに寄与すること大であり、乾癬に対する【攻めの治療】として有用であることは言を待ちません。
アレルギー性疾患
重症薬疹(TEN、スティーブンスジョンソン症候群など)に対しても様々な治療のオプションがあり、患者様と相談しつつ入院のうえ加療しております。また薬疹や食物アレルギー、蕁麻疹などに対し負荷試験を積極的に行い原因の追究に取り組んでいます。
潰瘍性疾患
末梢動脈疾患(PAD)についても循環器内科、形成外科、心臓血管外科、腎臓内科、糖尿病・内分泌内科とタイアップしフットケアチームとして対応しております。下腿潰瘍や褥瘡に関しても入院可能ですのでご相談ください。
自己免疫疾患
膠原病、水疱症、血管炎など難治性自己免疫疾患は入院、安静のうえステロイドの大量・長期投与、必要に応じ免疫抑制剤の併用や免疫グロブリン製薬の投与などが前提となります。総合内科、膠原病内科とタイアップし治療にとり組んでいます。重症円形脱毛症に対するステロイドパルス療法も必要応じて施行しております。
上記の疾患以外にも尋常性乾癬、尋常性白斑、難治性痒疹、円形脱毛症、アトピー性皮膚炎に対しては全身型ナローバンドUVBやエキシマライトによる加療を行っております。治療が必要な場合遠慮なくご相談ください。
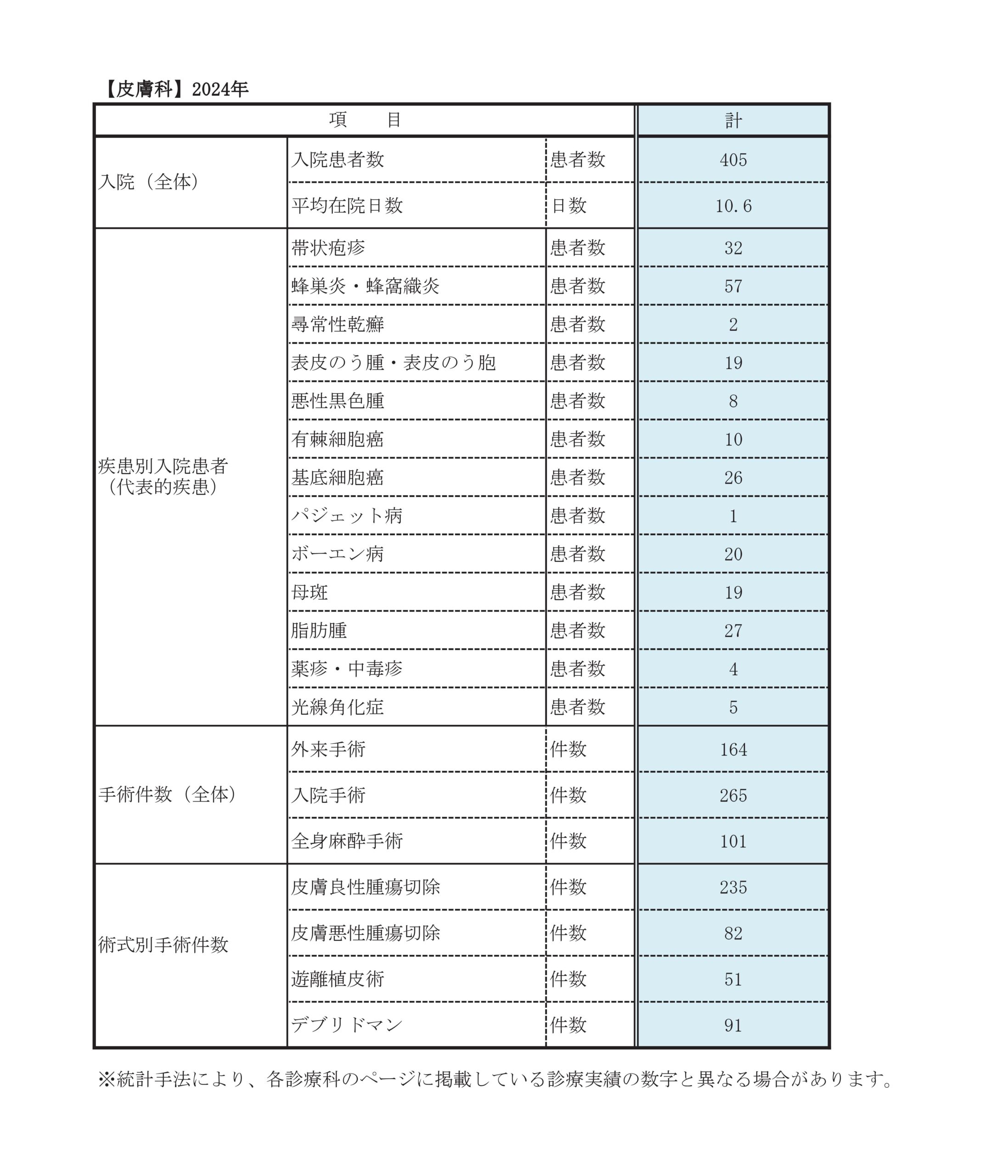
診療実績
診療科別統計
主な疾患・治療法
基本的には早期発見し拡大切除を行うことが肝要となります。当科では見張りリンパ節(センチネルリンパ節生検)をあらかじめRI法、体表エコーにて同定し、術前にパテントブルー、ICGによる色素法、蛍光法にて確認後 リンパ節の切除生検を行っています。それにより転移があればリンパ節廓清を行っていますが、場合により経過観察あるいは免疫チェックポイント阻害薬の投与を行っています。
切除不能例についてはまずBRAF遺伝子変異を確認します。変異陽性例は急速進行例についてはBRAF阻害薬+MEK阻害薬を投与し、変異陰性例や変異陽性例でも緩徐進行例はひとまず免疫チェックポイント阻害薬(抗PD-1抗体、抗CTLA4抗体)で経過を見るようにしています。この分野は次々と新しい薬剤が登場し治療のスタンダードがダイナミックに変化していますので常にup-to-dateな診療を心掛けています。
基底細胞癌、有棘細胞癌、付属器悪性腫瘍、乳房外Paget病、血管肉腫、悪性リンパ腫など、さまざまな悪性腫瘍が皮膚に生じます。ダーモスコピー所見、皮膚生検での病理組織学的診断とともに、疾患に応じて全身状態の評価を行い、手術および術後療法、経過観察の一連の治療をおこなっています。
最も多いとされる基底細胞癌は、リンパ節や他臓器に転移することは稀な皮膚悪性腫瘍ですが、顔面によくできる腫瘍です。最低3mmほど離して切除する必要があり、ある程度大きい場合には顔面に醜形を残さないように皮弁という、周囲の皮膚を回転させて閉創する手術をおこなっています。
その他、有棘細胞癌などの転移の可能性がある悪性腫瘍が診断された場合、CT, MRI, 疾患に応じてPET-CTを用いて腫瘍の深達度および他臓器転移の有無につき精査をおこない、病期応じた手術よび術後化学療法、放射線治療および、免疫チェックポイント阻害薬の投与をおこないます。
軽症の尋常性乾癬については従前通りステロイド外用剤やビタミンD3外用剤が治療の中心であることに変わりはありません。しかし治療抵抗例、広範囲に乾癬皮疹が拡大している例や関節症状を伴う場合は全身療法の適応になりうると考えます。 レチノイド、シクロスポリン、生物学的製剤などが使用薬剤候補ですが、それぞれに特色があります。患者様の全身状態、生活環境、許容できるコストなどに配慮しながら最適の薬剤をセレクトしております。特に生物学的製剤は現在10種類が上梓されており、特色が微妙に異なります。どの薬剤が最適か患者様に十分ICしながら治療法を決めてまいります。
アトピー性皮膚炎は、よくなったり悪くなったりを繰り返す、痒みを伴う湿疹を主病変とする疾患であり、患者さんの多くは気管支喘息やアレルギー性鼻炎・結膜炎などのアレルギー疾患の家族歴・既往歴があり、IgE抗体を産生しやすい素因を持つとされています。乳幼児期では食物アレルギーを合併することが多いですが、全年齢で認められる疾患であり、近年では高齢者のアトピー性皮膚炎が増加傾向にあります。
スキンケア、ステロイド外用剤、タクロリムス軟膏による加療がメインですが、2000年代に紫外線治療、2008年にシクロスポリン内服が適応となりました。
2018年に抗IL-4/13受容体モノクローナル抗体であるデュピルマブ(デュピクセント)が発売されたのを皮切りに、JAK阻害薬として2020年6月にデルゴシチニブ(コレクチム)軟膏が発売され、2020年12月にバリシチニブ(オルミエント錠)がアトピー性皮膚炎の治療に用いられるようになりました。現在、内服JAK阻害薬3剤が使用可能です。抗IL-13モノクローナル抗体であるトラロキヌマブ(アドトラーザ®)やレブリキズマブ(イブグリース®)も使用可能です。
今後も新たな分子標的薬が増えていくことが予想されますが、薬物治療のみではなく、日常生活での外用指導および悪化因子の検索、対応が必要な疾患であることには変わりありません。個々の生活状況を踏まえた上で、治療方法につき提案させていただきます。
典型的な症状としては、境界がはっきりとしたわずかに隆起した“膨疹”が生じます。強い痒みを伴うことが多く、数10分から数時間で消退します。食べ物や薬が原因の場合は、一旦消退したあと翌日に症状が出ることはまれですが、そうでない場合は翌日以降も膨疹の出没が続きます。一言で“じんま疹”といってもさまざまなタイプがあり、適切な病型診断とそれにもとづいた治療が必要になります。
刺激誘発型じんま疹(特定の刺激、負荷により誘発することができる蕁麻疹)の中には、食べ物や薬によるアレルギー性のじんま疹、ひっかいた部位に線状の膨疹ができる物理性じんま疹、体があたたまった際に小型の膨疹が生じるコリン性じんま疹、その他、アスピリンじんま疹などがあります。それぞれ詳細に話を聞くことによりある程度正確な診断が可能です。原因を避けられる場合にはその指導をおこない、そうでない場合には抗アレルギー剤の内服や、必要であればアドレナリン自己注射(エピペン)の処方をしています。
原因が特定できないじんま疹のうち、6週間以上出没を繰り返すものを“慢性じんま疹”と診断します。抗アレルギー剤の内服、H2受容体拮抗薬の内服でおさまらない場合、現在はオマリズマブ(ゾレア)の皮下注で加療を行うことが可能です。
従来の抗生剤内服・抗菌剤外用・アダパレン外用に加え最近過酸化ベンゾイルの使用が可能となり、さらに最近クリンダマイシンと過酸化ベンゾイルの合剤、ニューキノロン外用剤、アダパレンと過酸化ベンゾイルの合剤が次々と上梓されている状態です。様々な薬剤をどのように使い分けるか、ガイドラインに準拠しつつ状態に合わせ治療を進めてまいります。
臨床研究
| 当院における壊死性筋膜炎の臨床データおよび治療経過の検討 | |
|---|---|
| 当院でのアパルタミド投与46例の検討 | |
| 研究課題名 | 説明文(PDF) |