地域医療支援病院の使命のもと、あらゆる呼吸器疾患の急性期とくに重症難治例・希少疾患等に対して24時間365日対応し、病診病病連携を通じて地域全体の医療に貢献することをモットーとしています。診療内容はエビデンスに基づく最新の診断治療を展開することを基本としつつ、常に問題意識を忘れずそれらを解決すべく治験、臨床試験にも多く参画し、学会発表、論文執筆などを通じて常に若い医師たちが高いモチベーションを維持できる場となるよう努力しています。市民の皆様から呼吸器疾患でもっとも頼りになる病院としてご評価いただけるよう、安全かつ先進的な医療を今後も継続してまいります。
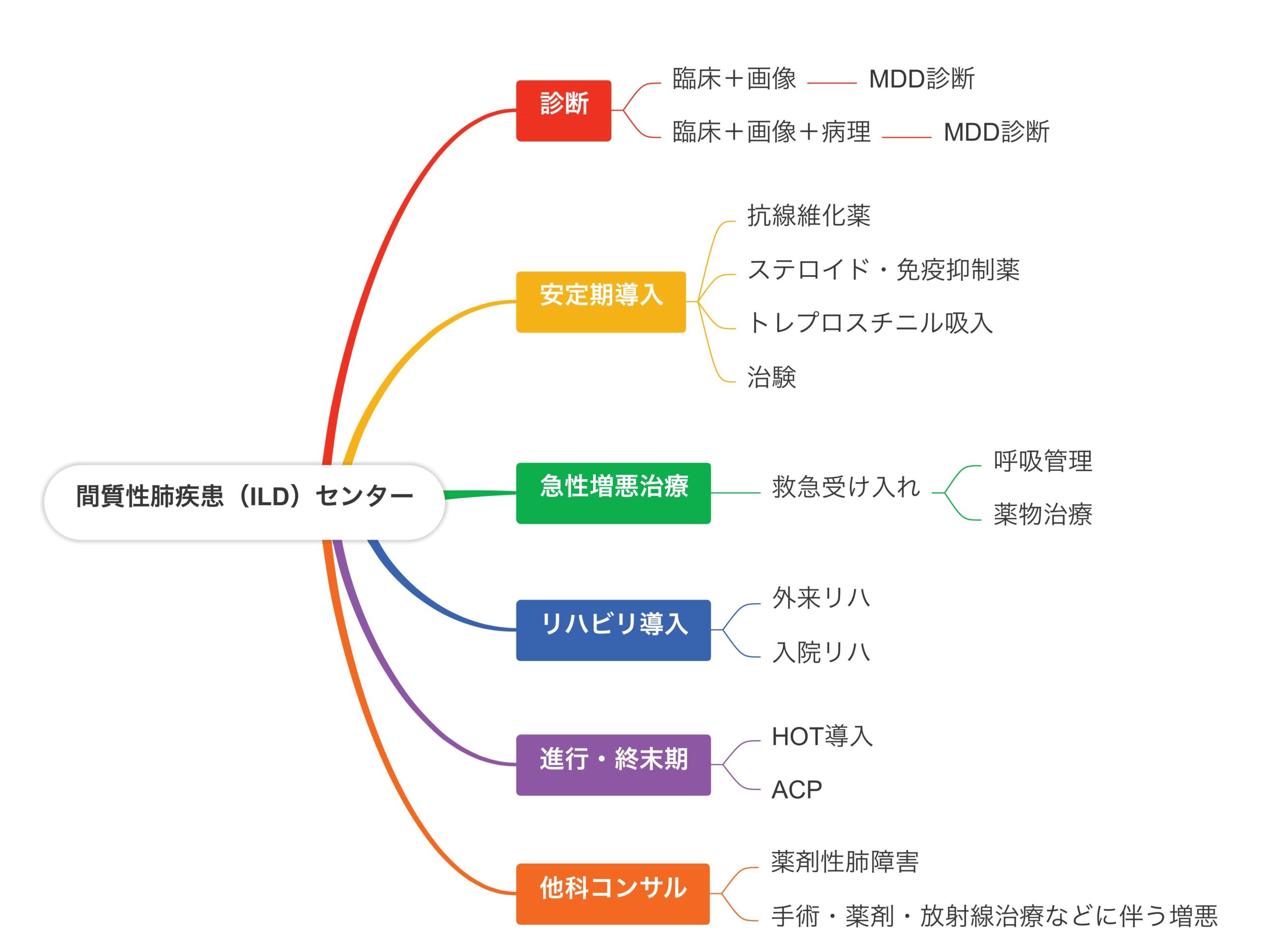
間質性肺疾患センター(ILDセンター)開設について(2024年4月より)
間質性肺疾患は難病でもある特発性間質性肺炎から、膠原病に伴うもの、粉塵や喫煙、各種抗原吸入に伴うもの、薬剤に起因するもの、コロナのような感染症に伴うもの、他の疾患や治療に合併するものなどがあり、その予後は治癒するものもあれば進行性に線維化が進み呼吸不全に至るもの、突然致死的な急性増悪を起こすものなど多種多様です。診断には診療に習熟した施設で行う専門的な検査や合議が必要で、治療には種々の薬物やリハビリテーション、呼吸管理などの専門的知識と多職種の関わりが求められます。また進行性の病態においては、生涯にわたっての支援や教育、緩和ケアも欠かせません。
当院においてはこれまで呼吸器内科の一分野として、関西圏でも有数の患者さんの診療に関わってきましたが、今回さらに一層ILDの認知度を向上させ、より多くの患者さんに適切な治療とケアを届けられるように専門のセンターを立ち上げました。未診断でよくわからない画像で対応に困る患者さん、急速に呼吸不全が進行する患者さん、次第にADLが低下して対応に苦慮する患者さん、がんや膠原病の治療中に発症してきた患者さんなどなど、院内外を問わずあらゆるILD患者さんのサポートを行なっていきたいと考えています。
主な対象疾患と診療の流れ
肺癌という病気について
肺癌とは肺に発生する癌の総称です。気管・気管支・肺胞の正常細胞が本来の機能を失い、無秩序に増殖することで肺癌は発生します。しかも癌細胞は局所にとどまらず血流やリンパの流れに乗って多臓器に広がり同様に増殖します。これを転移といいます。肺癌は急激な増殖能力と転移能を兼ね備えているため、悪性度が高く予後の悪い病気といえます。
わが国の肺癌死亡数は1960年代から男女とも一貫して増加しており、男性では部類別悪性新生物死亡率が1993年に胃癌を抜いて第1位に、女性でも第3位となり増加し続けています。
症状
大きさや場所によって様々な症状が出現します。咳や血痰といった症状を呈することもありますが、かなり大きくなっても無症状であることが多いです。
ほかに胸背部痛や喘鳴(ゼ―ゼー音)、息切れ、声がかすれる、顔面や首のむくみなどが症状として出やすいです。また一般的な癌の症状として、疲れやすい、食欲低下、体重減少や発熱が持続するといった症状も現れます。
肺癌の診断
①気管支鏡検査
肺癌の正確な病理組織診断を得るため、極細径気管支鏡検査や気管支腔内超音波検査、クライオ生検も行い診断を行います。
②超音波ガイド下生検
超音波ガイド下に経皮的に生検を行います。皮下に近い病変の場合に行います。
③CTガイド下生検
CTスキャンを撮影しながら、病変部を確認し経皮的に生検を行います。気管支検査では到達困難な病変に対して行っています。
④胸腔鏡下肺生検
当院呼吸器外科と連携し、上記検査では診断が困難な場合に行われます。
上記の組織学的検査に加えて、レントゲン検査、CTスキャン、MRI、骨シンチグラフィ、PET/CTなどの画像診断も行い病期(癌の進行度)診断を行います。
組織型による分類
扁平上皮癌、腺癌、大細胞癌、神経内分泌癌の4つの組織型に分類されます。治療方針の決定上このうち非小細胞肺癌(扁平上皮癌、腺癌、大細胞癌)と小細胞肺癌(神経内分泌癌)の2つに分類することが多いです。
個別化治療の時代
近年肺癌治療は遺伝子変異に基づく治療に変わり、対象となる患者さんには腫瘍の遺伝子検査を行い一人一人に合った治療を検討していきます。それにあたり当院では国内の他施設と協力した遺伝子検査を行い最先端の治療方針を検討する場合もあります。
病期分類
StageⅠ⇒局所癌、StageⅡ、StageⅢ⇒局所進行肺癌、StageⅣ⇒遠隔転移を伴う進行肺癌
肺癌の治療
肺癌の治療には大きく分けて手術療法、放射線療法、化学療法とに分かれます。また近年ではがん免疫療法が肺癌で適応となり、がん免疫療法も行っております。どの治療においても関西圏で屈指の症例数を誇っております
①手術療法
当院では呼吸器外科を中心として定型的手術は胸腔鏡を用いた低侵襲手術を行い、腫瘍の進展具合により、肺全摘出術、葉切除術、区域切除術、スリーブ切除術を行っております。
②放射線療法
放射線を照射することにより腫瘍病変部の局所制御を行います。骨転移病変や脳転移病変に対しても放射線療法を行っております。
③化学療法
抗がん剤による治療です。当院では最新のデータに基づいて抗がん剤を選択しております。対象となる患者さんには腫瘍の遺伝子検査を行い、適応のある患者さんにおいては分子標的治療薬(オシメルチニブ、アレクチニブなど)を用いて治療も行います。
④免疫療法
2015年12月に本邦において適応となり、期待が持てる薬剤であります。しかしながらこれまでの薬剤と異なった全身への副作用も報告されており、総合病院としての強みを生かし他科連携を行い安全に治療を行えるように努力しております。
肺癌治療は病期分類、組織型、遺伝子変異によって大きく分かれます。下記はあくまで参考です
①非小細胞癌
Ⅰ期、Ⅱ期、Ⅲ期の場合は、根治を目標とした手術療法、放射線療法、化学療法もしくはそれらを組み合わせた集学的治療がなされます。手術の前後や放射線療法後に、免疫療法を追加することもあります。
Ⅳ期:全身化学療法、放射線療法、免疫療法を行います。より長くより元気になる治療を目標とし、最大限の支持療法を行いながら治療を行います。
②小細胞肺癌
小細胞肺癌はLDタイプ(限局型)とEDタイプ(進展型)に分かれます。LDタイプの場合はⅠ期の場合は手術療法と化学療法を行います。それ以外は化学放射線療法を行います。EDタイプにおいては全身化学療法の適応となります。
チーム医療、他科連携の時代
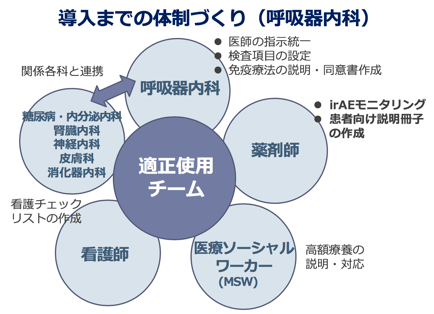
近年肺癌化学療法では日々進歩する治療、多様化する副作用、診断を含めて他科多職種による診療が不可欠となっています。当院では医師、看護師、薬剤師からなる肺癌化学療法チームを設定し、治療についても助言や相談を行い治療行っています。
また肺癌は治療中の救急受診が最も多い部類の癌腫といわれており、当院の24時間365日提供する救急医療により急に起こる治療中の合併症や毒性対応について癌治療を行う病院にて行うことができるという安心した医療を提供します。
1)間質性肺炎とはどんな病気?
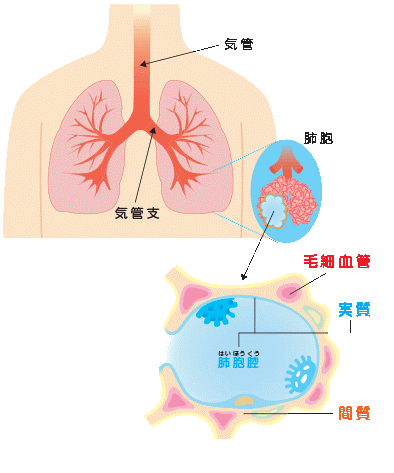
肺の「間質」とは何でしょうか?
肺は、空気の入った小さな袋である「肺胞」が多数集まってできています。「間質」は肺胞と肺胞の間の領域のことで、外側の壁の部分に相当します。これに対して、肺胞の中の部分は、肺の実質と呼ばれます。
通常の肺炎と間質性肺炎は、どう違うのでしょうか?
一般的に「肺炎」と呼ばれる疾患は、感染症が原因のことが多く、肺胞の中(実質)で細菌が増殖して炎症が起こります。これに対して、肺胞の壁(間質)に肺炎の主体があるものを総称して、間質性肺炎と呼んでいます。つまり「間質性肺炎」とは、肺炎が生じている場所に基づいて区別した呼称で、一口に間質性肺炎と言っ
ても、その原因や病気の経過は様々です。
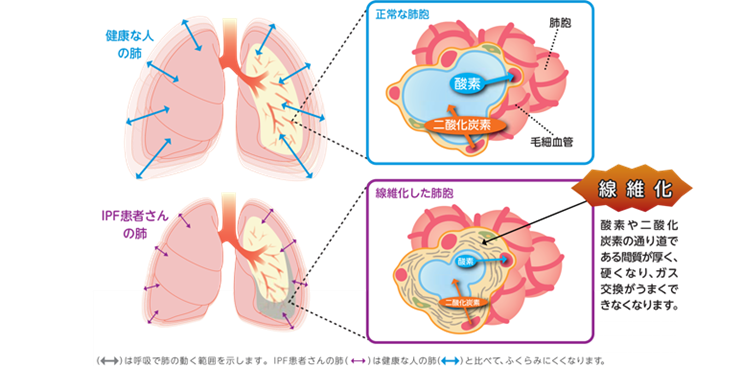
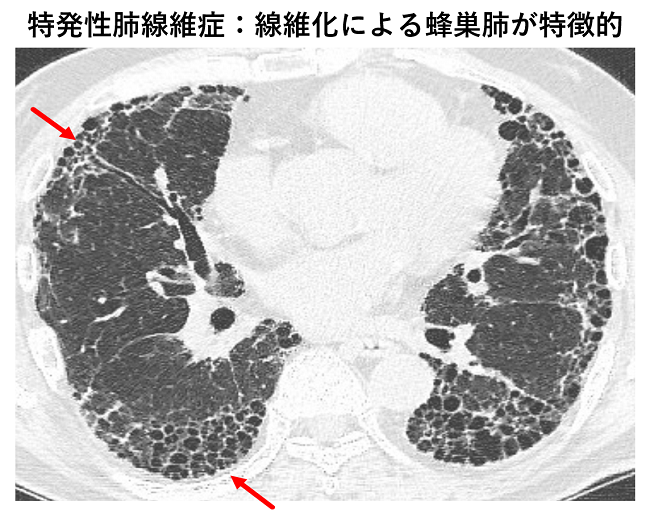
間質性肺炎が長期にわたって続くと、組織を修復しようというという働きにより、間質が分厚く硬くなる「線維化」が起こってきます。間質に線維化がおこると、肺が固くなるため十分に拡張・することができず、肺活量が低下して息切れが生じます。また、正常なガス交換が妨げられ、少しの動作でも体内の酸素濃度が下がりやすくなります。
間質性肺炎の症状はどのようなものがありますか?
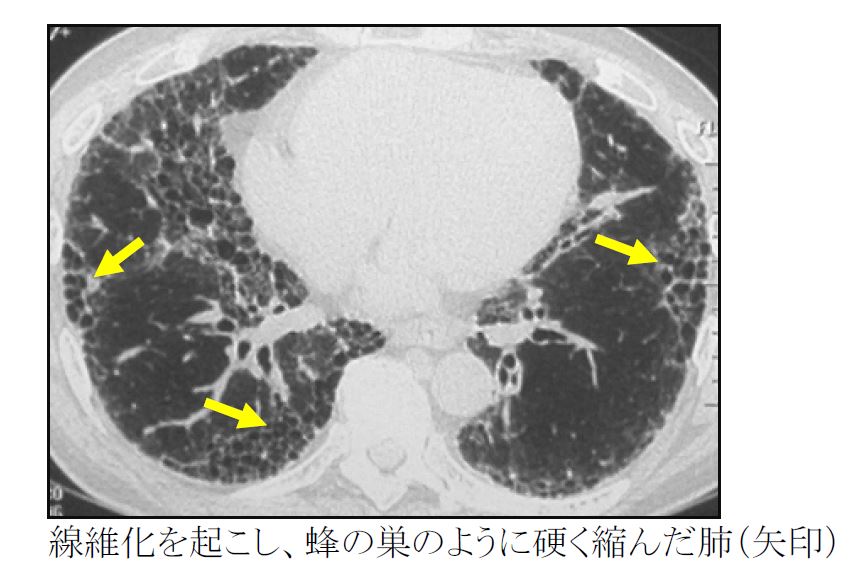
咳・息切れが主な症状です。経過が早いものは発熱を伴うことが多くなります。経過の長いものは線維化を起こして本来スポンジのように軟らかい肺が硬く縮み、肺活量が低下します。
間質性肺炎の経過はどのようなものでしょうか?
間質性肺炎は種類ごとに進行の速度・様式が大きく異なります。また同じ診断名(例えば特発性肺線維症)であっても患者さんごとにその経過は大きく異なります。緩やかに呼吸機能が低下する人もいれば、急速に進行するタイプの人もいます。数日から1ヶ月程度の短い期間に呼吸状態が急激に悪化する、急性増悪と言われる状態を繰り返し起こす人もいます。
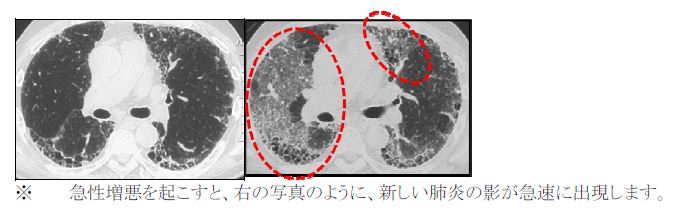
間質性肺炎の急性増悪とは何でしょうか?
間質性肺炎は肺の間質に炎症や線維化がおこり、徐々に呼吸機能の低下が進行する疾患群です。ところが時々、慢性的な進行の範囲をこえて急激な悪化が生じることがあり、これを急性増悪とよびます。具体的には、数日から1ヶ月以内の経過で急速に肺に新しい陰影が出現し、呼吸不全(必要な酸素を取り込むことができない状態)に至る状態です。特発性肺線維症の患者さんでは年間5-15%の確率で急性増悪を起こすとされています。
急性増悪の原因は特定できないことも多いですが、感染症・全身麻酔の手術・新しい薬の投与(抗がん剤など)などの後に急性増悪が起こる場合があります。サプリメントや漢方薬で急性増悪を起こすこともあり、間質性肺炎の患者さんが何か新しく薬やサプリメントを始める際には担当医に相談することをお勧めします。
間質性肺炎の急性増悪が起きた場合、急速に呼吸不全(必要な酸素を取り込めない状態)が進行します。確立された治療法はなく、死亡率も高い重篤な病態です。治療にはステロイドや免疫抑制剤というタイプの薬を用います。人工呼吸器などの呼吸のサポートも必要になる場合があります。また急性増悪から回復できても在宅酸素療法が必要になるなど、呼吸機能に後遺症を残すこともあります。
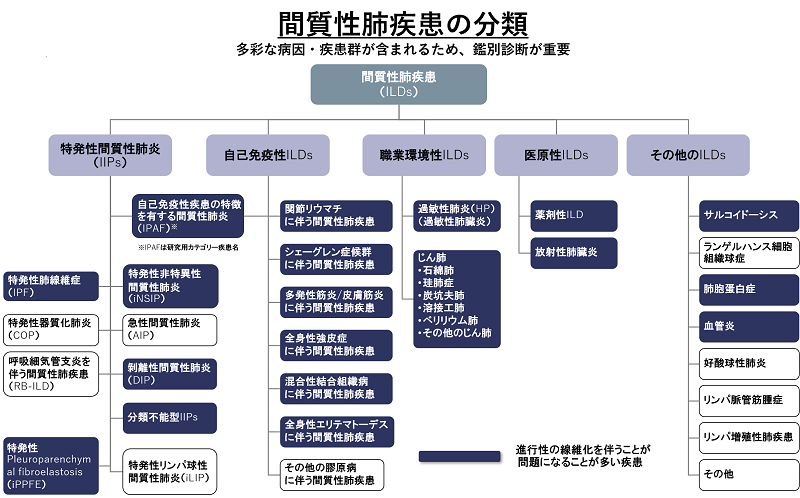
2) 間質性肺炎はどのように分類されていますか?
原因が特定できたもの
- 過敏性肺炎
さまざまな有機物質の吸入によって起こる間質性肺炎です。住居・加湿器・空調・飼料などについたカビや、羽毛布団やダウン製品など鳥由来の粉塵などが原因となります。 - 塵肺
さまざまな無機物質の吸入によって起こる間質性肺炎です。岩石に含まれる硅酸化合物の吸入によって起こる珪肺、石綿吸入によって起こる石綿肺などが代表です。 - 膠原病に伴う間質性肺炎
関節リウマチ、強皮症、皮膚筋炎、多発筋炎、シェーグレン症候群、血管炎などに伴って間質性肺炎を起こすことがあります。 - 放射線治療後に起こる放射線肺炎
- 薬剤服用による薬剤性肺炎
- ウイルスや一部の真菌などによって生じる感染症としての間質性肺炎
原因が特定できないもの=特発性間質性肺炎(特発性とは医学用語で原因不明という意味です)
- 慢性線維化型
✓特発性肺線維症(IPF):もっとも多いタイプです
✓特発性非特異性間質性肺炎(NSIP) - 喫煙関連
✓剥離性間質性肺炎(DIP)
✓ 呼吸細気管支炎関連性間質性肺疾患(RB-ILD) - 急性・亜急性
✓特発性器質化肺炎(COP)
✓急性間質性肺炎(AIP) - 稀なもの
✓特発性胸膜肺実質線維弾性症(PPFE)
✓特発性リンパ球間質性肺炎(LIP)
3)間質性肺炎はどのように診断するのですか?
医療機関を受診するきっかけ
間質性肺炎が見つかる状況としては、空咳や息切れのため近くの医院を受診し、胸部写真で異常を指摘される場合が多いです。全く無症状の方が定期検診で異常を指摘されて、医療機関を受診することもあります。間質性肺炎が疑われた場合には、専門的な診断・治療が可能な医療機関を受診することが大切です。
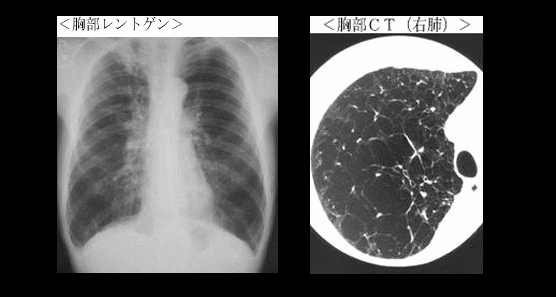
画像検査
通常のCTよりも精密な肺画像を撮影できる高分解能CT(HRCT)によって、間質性肺炎の性状について詳しく解析します。これにより、間質性肺炎の原因・タイプ・治療などについて情報を得ることができます。CT検査は間質性肺炎の診断だけでなく、疾患の進行・治療効果の判定・合併する肺癌を見つける上でも役に立ちます。
血液検査
KL-6やSP-Dなど間質性肺炎で上昇するマーカーを測定し、診断や治療効果の判定に役立てます。自己抗体が上昇していれば自己免疫疾患が原因で発症する間質性肺炎の可能性が高い、など原因についての情報が得られることもあります(自己抗体:通常の抗体は外部から侵入した異物の除去に作用するのですが、自己抗体は自分の体の一部を異物として誤って攻撃してしまい、間質性肺炎の原因となることがあります)
呼吸機能検査
間質性肺炎にかかると肺活量やガスの交換能力が低下します。これらのことをスパイロメトリーとよばれる機械を用いて測定します。治療の効果を判定する目的でも行われます。
6分間歩行検査
間質性肺炎の心肺機能への影響を評価するために行います。6分間に歩くことのできる距離から運動持久力を評価します。検査はパルスオキシメーターを装着しながら行いますので、運動により血液の酸素飽和度がどれだけ変化するかも評価できます。
細胞や組織を採取する検査(気管支鏡検査、肺生検)
気管支肺胞洗浄
気管支鏡を用いて肺胞を生理食塩水で洗浄し、洗浄液を回収する検査です。回収した液体に含まれる成分や細胞の種類から病気の種類を推定します。
鉗子生検
気管支鏡から小さな鉗子を入れて、肺の末梢の組織を採取する検査です。採取できる組織が小さいため、慢性型の間質性肺炎での診断能力は限定されます。
凍結生検(クライオバイオプシー)
気管支鏡から専用の検査器具を入れて、先端周囲を凍結させて肺の末梢の組織を採取する新しい方法で、間質性肺炎の診断手技として普及しつつあります。採取できる組織の量と質が従来の鉗子生検よりも優れており、当科でも積極的に行っています。2泊3日の入院で行います。
胸腔鏡下肺生検
体表に小さな穴をあけ、胸腔鏡とよばれる内視鏡を用いて、肺の外側から肺の組織を採取します。大きな組織が得られるため情報量も多いですが、手術と同様に全身麻酔で行う必要があります。
間質性肺炎の診断は、上記の検査を組み合わせて行います。病気のタイプにより必要な検査が異なりますので担当医とよく相談して検査を進めましょう。
4)間質性肺炎はどのように治療するのですか?
治療目標
間質性肺炎の治療の考え方は、どのタイプの間質性肺炎かによって大きく変わります。例えば、最も多いタイプの特発性肺線維症(IPF)では、線維化で硬くなった肺は元に戻らないことが多く、今後の病気の進行を抑えるのが現実的な目標となります。一方で自己免疫による膠原病や吸入による過敏性肺炎では、原因を取り除いたり炎症を抑えたりすることで、ある程度回復が期待できる場合もあります。治療を始める前に、診断に必要な検査を十分に行い、適切な治療方針を設定することが大切です。
原因を取り除く
原因が分かっている間質性肺炎では、原因をできるだけ取り除くことから始めます。薬剤が原因の場合は、該当する薬剤を中止します。羽毛やカビなど環境中のアレルゲンが原因の間質性肺炎(過敏性肺炎)では、原因物質を除去・回避しましょう。
薬物療法
間質性肺炎の治療薬は、①肺の線維化を抑える薬(抗線維化薬)と②炎症を抑える薬(ステロイド、免疫抑制剤)に分けられます。
- 抗線維化薬
線維化が中心のタイプの間質性肺炎に対して用いられます。現在、特発性肺線維症(IPF)の治療薬として、2種類の抗線維化薬が認可されています。ピルフェニドン(ピレスパ®︎、ピルフェニドン®︎)とニンテダニブ(オフェブ®︎)は、いずれも肺活量の低下速度を約半分にすることが証明されています。また、間質性肺炎の急性増悪の抑制も期待できます。さらに2020年以降、標準的な治療を行っていても線維化が進行する間質性肺炎に対しては、そのタイプにかかわらずニンテダニブ(オフェブ®︎)が使用できるようになり、治療薬の選択肢が広がりました。 - ステロイド、免疫抑制剤
いずれも炎症を抑える薬で、炎症が強いタイプの間質性肺炎に対して用いられます。長期間の使用が必要な場合は、ステロイドと免疫抑制剤を併用することもあります。代表的な対象疾患は、自己免疫疾患(膠原病)に伴う間質性肺炎です。いずれの薬も自身の免疫力を低下させるため、内服中は細菌やウイルスの感染症に注意が必要です。間質性肺炎の急性増悪に対しては大量のステロイドを投与し、肺に起きている炎症を強力に抑える治療を行います。
その他の治療
咳や息切れなどによる生活への影響をできるだけ抑えるためには、間質性肺炎そのものの治療だけでなく、運動や栄養などに気をつかって全身的なコンディションを整えることが大切です。
- 運動療法
息切れは、「肺の力」「心臓の力」「筋肉の力」の3つの力の足し算で起こります。肺の力が落ちている時こそ、より一層の身体機能の維持・向上を図るため、適切な身体活動を継続して行うことが大切になります。自宅でできる運動としては、歩行が中心となります。呼吸に負担をかけない動き方も覚えましょう。 - 栄養療法
息切れがあると、呼吸のために通常よりも多くのエネルギーをとします。食欲が落ちてやせてしまい、より一層息切れが強くなる悪循環に注意が必要です。「高カロリー」「高たんぱく」を意識し、食事内容にも十分に配慮しましょう。 - 酸素療法
呼吸機能の低下により、肺で十分な酸素が取り込めなくなった場合に行います。自宅に酸素濃縮機を設置して、空気中の酸素を濃縮して鼻から吸入します。携帯用のボンベを持ち運び、外出することも可能です。携帯性に優れた液体酸素やポータブル型酸素濃縮器など、いくつかのタイプがありますので、病状と生活スタイルに合わせて選びましょう。 - 肺移植
薬物療法を行っても病状が進行する場合、移植の適応となることがあります。肺移植には脳死ドナーから提供を受ける脳死肺移植と、健康な人から提供を受ける生体肺移植があります。肺移植の適応にはいくつかの条件がありますので、詳細については主治医にお尋ねください。 - 治験
治験とは、「治療薬の候補」を健康な人や患者さんに使用して、効果や安全性などを確認する目的で行われるものです。薬は治験の結果に基づいて国の承認を得ることで、初めて多くの患者さんに使用できるようになります。間質性肺炎についても、今なお多くの薬が開発されており、当院も間質性肺炎の治療成績の向上のため、積極的に治験を実施しています。詳細については、担当医や治験コーディネーターにお尋ねください。
5) もしもの時の話し合いを始める(アドバンス・ケア・プランニング)
万が一、病気が進行した場合の対応や療養について、事前に考えておくことを「アドバンス・ケア・プランニング」と言います。間質性肺炎が進むと、息切れなどで生活に支障がでることも考えられますが、将来どのような治療・ケアを受けたいか、「大切にしていること」「してほしくないこと」など、考えておられることがあれば、どうぞ医療スタッフやご家族にお伝えください。私たちも患者さんのお気持ちに寄り添ってサポートしていきたいと考えています。
6)間質性肺炎の治療で利用できる医療制度には、どのようなものがありますか?
難病医療費助成制度
国が定める「指定難病」のうち、症状が一定程度以上または高額な医療費を長期に支払っている場合、難病に関係する医療費が助成され、自己負担が軽減される制度です。間質性肺炎の全てが対象となるわけではなく、特発性肺線維症(IPF)、もしくは肺生検で診断されたIPF以外の特発性間質性肺炎が、難病(特定疾患)に指定されています。
高額療養費制度
難病医療費助成制度の対象とならない方は、加入されている健康保険(医療保険)によって医療費の自己負担が軽減される制度があります。同一月(1日~月末まで)にかかった医療費のうち、自己負担限度額を超えた分が免除もしくは払い戻されます。自己負担限度額は加入している健康保険、世帯収入により異なります。
介護保険制度
介護や日常生活の支援を希望し、市区町村に介護や支援が必要と認定された方が利用できる制度です。サービスにかかる費用の1~3割の自己負担で介護サービスが利用できます。対象となる方は、「65歳以上で介護や支援が必要と認定された人」、「40~64歳で16種類の特定疾病(初老期認知症、脳血管障害、ガンなど)により介護や支援が必要と認定された人」です。
身体障害者手帳
身体障害者福祉法に定める身体状況の方が、申請により取得できます。障害にも様々あり、在宅酸素を導入する際に呼吸機能障害の対象となる場合があります。ご自身が対象となるかは、医師へご確認ください。等級によっては医療費助成を受けることもでき、内容はお住まいの市区町村により異なります。
日常生活用具給付事業(パルスオキシメーター購入費の助成)
障害者の日常生活の利便をはかるための用具の購入費を支給する事業です。内容はお住まいの市区町村により異なります。神戸市では、呼吸機能障害3級以上の方が、パルスオキシメーターの購入費の支給を受けることができます。必ず購入する前に申請しなければなりませんので、ご注意ください。
7) 間質性肺炎サポートチーム
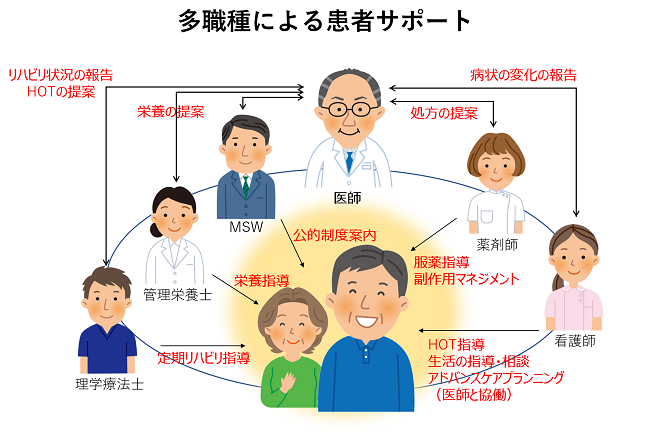
当院では診断・治療に難渋するこれらの疾患に対して、医師、看護師、薬剤師、理学療法士、栄養士、ソーシャルワーカーなどの多職種が、それぞれの専門的アプローチを連携して行い、患者さんの治療導入や日常生活の維持、生活の質向上を目指して取り組んでいます。具体的には医師による病気の診断や治療法の説明、看護師による日常生活指導や在宅酸素療法の支援、薬剤師によるきめ細かい服薬指導、副作用管理、理学療法士によるリハビリテーション、栄養士による栄養指導、ソーシャルワーカーによる社会資源の有効利用などです。これらの理解を深めるために「間質性肺炎ハンドブック」をお渡ししています。また病気が進行して緩和ケアが必要な患者さんのための「呼吸不全の緩和ケア」という冊子もお渡しします。
参考のためにご希望の方は下記よりダウンロードください。(著作権は保有していますので、許可なく他への転載はご遠慮ください。)
「間質性肺炎ハンドブック」のダウンロードはこちら 「間質性肺炎とどう付き合うか」のダウンロードはこちら「息が苦しい」や「息ができない」と呼吸不全とは同じではありません。「息」という字は、「自らの心」と書きますが、心臓の病気や精神的な問題でも息が苦しくなることがあります。逆に、息が苦しくなくても呼吸不全のことがあります。人に限らず全ての動物は、酸素がないと生きていけませんが、呼吸不全とは、動脈血中の酸素濃度の低下、つまり体内に酸素が不足していることであり、医学的には、「空気吸入時の動脈血ガス分圧が60Torr以下の場合」と定義されています。動脈血ガス分圧というのは動脈からの採血をしなければ測れませんが、パルスオキシメータという装置を使えば、指に光をあてるだけで動脈血の酸素化レベル(動脈血酸素飽和度 SpO2)をリアルタイムに測定でき、動脈血ガス分圧を簡単に推定することができます。SpO2で90%以下が、大体、動脈血ガス分圧での60Torr以下に相当しますので呼吸不全であるといえます。パルスオキシメータは連続記録も可能で、小型、軽量のものが普及しており、病院などでは呼吸管理のため様々なところで使用されています。
呼吸不全はどうしておこる?
呼吸は、気道および肺によって空気中の酸素を体内にとり込み、炭酸ガスを体外に排出する作業ですので、気道に障害があって空気が肺に到達しにくくなったり、肺の病気で酸素が血液内にとけ込みにくくなった時に呼吸不全になります。しかし、気道や肺に異常がなくても、神経の病気で呼吸筋の力が低下したり、胸郭変形があって肺が十分に膨らまなかったり、あるいは薬物で脳の呼吸中枢の働きが弱くなった場合などでも呼吸不全はおこります。
呼吸不全にはどのようなタイプがある?
I型呼吸不全とⅡ型呼吸不全
呼吸不全は、不要な炭酸ガスが体内に貯まらないタイプ(Ⅰ型呼吸不全)と貯まるタイプ(Ⅱ型呼吸不全)の2種に分けられます。Ⅰ型呼吸不全は肺不全型とも呼ばれ、喘息発作、肺線維症、肺塞栓症などがあります。Ⅱ型呼吸不全は、換気不全型とも呼ばれ、進行した肺気腫、肺結核後遺症、胸郭変形、薬物による呼吸抑制などがあります。
急性呼吸不全と慢性呼吸不全
呼吸不全の状態が1ケ月以上続く場合を慢性呼吸不全、そうでない場合を急性呼吸不全として分けています。慢性呼吸不全の患者さんは長期にわたって呼吸不全の治療が必要で、しばしば急性増悪といって、いろいろな原因で呼吸不全の悪化をきたすことがあります。肺気腫、結核後遺症、肺線維症、気管支拡張症、胸郭変形などが慢性呼吸不全の原因になります。一方、急性呼吸不全は慢性化することはまれで急性期をのりこえれば、それ以後、呼吸不全の治療は通常必要ありません。肺炎、喘息発作、薬物中毒、肺塞栓症などは急性呼吸不全の原因となります。
呼吸不全の評価は?
動脈血ガス分圧やパルスオキシメータで動脈血酸素飽和度(SpO2)を測ればその時点での呼吸不全の程度はわかりますが、呼吸不全の患者さんでは、呼吸不全のためにどれくらい行動が制限されているかということを示す指標に、Hugh-Jones(ヒュー・ジョーンズ)の分類という次の5段階に分ける方法があります。
| Hugh-Jones (ヒュー・ジョーンズ)の分類 |
|---|
| Ⅰ度 | 正常 |
|---|---|
| Ⅱ度 | 同年齢の健常者と同様に歩行はできるが、階段や坂は健常者なみに登れない。 |
| Ⅲ度 | 平地でも健常者同様に歩行はできないが、自分のペースなら1.6km(1マイル)以上歩ける。 |
| Ⅳ度 | 休みながらでなければ50m以上歩けない。 |
| Ⅴ度 | 会話、衣服の着脱にも息切れがする。息切れのため外出が出来ない。 |
また、肺機能検査や、6分間歩行試験(6分間で平地をどれくらい歩けるか)などによって呼吸不全の程度を評価することもあります。
呼吸不全の治療は?
体内に酸素が不足しているわけですから、どのようなタイプの呼吸不全であっても、酸素を体内に補う治療が最優先されます。
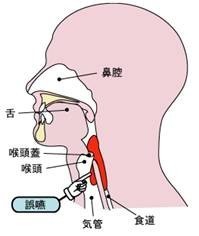
気道確保
痰、血液、異物などによって窒息状態にある場合は、酸素を補うルートを確保するため、まず吸引によって、それらをのどから除去しますが、うまく除去できない場合や、重症の呼吸不全の患者さんには、気管チューブという管を鼻や口から気管内に挿入します。
酸素療法
通常は鼻、あるいは口からカニューレやマスクで酸素を吸入させますが、必要な酸素の流量は原因疾患や呼吸不全の程度によって異なります。急性呼吸不全では、最初から高流量(3-4L/分)で良いのですが、慢性呼吸不全では、炭酸ガスが体内に貯まるII型呼吸不全の場合、高流量ではさらに換気が弱くなってしまうことがあるので、通常、低流量(3L/分以下)から始めます。自分で息が楽に吸えない患者さんや重症の呼吸不全の患者さんに対しては、口や鼻から、あるいは気管チューブから酸素を押し流す、いわゆる人工呼吸を行います。
人工呼吸
人工呼吸の方法は応急処置としては患者さんの口や鼻に呼気を吹き込む方法がありますが、病院では、通常、気管チューブを人工呼吸器につないで、器械によって酸素を気管に押しこみます。ただし、気管チューブの挿入は非常に苦痛を伴うので、最近では、管のかわりに鼻マスクや鼻口マスクを使って人工呼吸を行う方法(非侵襲性換気療法)が広く行われるようになってきました。
薬物療法
酸素療法や人工呼吸はあくまで不足した酸素を補っているに過ぎませんから、呼吸不全の患者さんに対しては、酸素療法と同時に、肺炎に対する抗生剤、喘息に対するステロイドホルモンや気管支拡張剤など、原因となっている病気の治療も必要です。
在宅酸素療法とは?
わが国で最も普及している在宅療法の1つで、現在、10万人以上の慢性呼吸不全の患者さんが、この治療を受けておられます。社会保険の適用を受けたのは1985年で、それ以前は、酸素吸入が必要なために長期の入院をしいられる患者さんがたくさんいました。現在、この治療の適応基準は、安静時の動脈血ガス分圧が55Torr以下(パルスオキシメータのSpO2では88%以下)あるいは、60Torr以下でも、運動時や睡眠時に著しく下がる人とされています。
また、その他に、肺高血圧症やチアノーゼ型心疾患の患者さんも適応とされています。肺気腫、肺結核後遺症、肺せんい症、気管支拡張症などの慢性呼吸不全の患者さんが、多くこの治療を受けておられますが、最近では、肺癌の患者さんも増えてきています。酸素供給方法は、空気中の酸素を濃縮する据え置き型の器械が多く使われていますが、この場合、通常、携帯用には酸素ボンベを使用します。他に、専用の容器に詰めた液体酸素を使用する場合もありますが、詰め替えや器械の設置場所の問題などで濃縮器ほどは普及しておりません。在宅酸素療法を始めると、どうしても行動範囲がせまくなってしまいがちですが、実際には旅行することも可能で、酸素供給を行っている業者が宿泊先に酸素濃縮器や酸素ボンベを届けてくれますし、在宅酸素療法をうけている患者さん同士の会も各地にあります。ただし、在宅酸素療法を始められたら、必ず定期的にかかりつけの医師の診察を受けて、呼吸状態のチェックをしておくことが大事です。
在宅人工呼吸療法とは?
在宅人工呼吸療法は、炭酸ガスが体内に貯まるⅡ型の慢性呼吸不全の患者さんに対して、気管切開口を通して人工呼吸を行う方法と、専用の鼻マスク、もしくは鼻口マスクを通して人工呼吸を行う方法とがあります。前者の気管切開口からの人工呼吸は、主に、神経疾患のために呼吸筋の力が極端に弱くなった患者さんに対して行われています。一方、後者の、専用のマスクを使う人工呼吸は、胸郭変形、結核後遺症、肺気腫などの慢性呼吸不全の患者さんに対して、在宅酸素療法と併用して夜間のみに行われる場合が多く、方法が簡便なこともあり、ここ数年、急速に患者数がふえています。
急性増悪の予防は?
慢性呼吸不全は、しばしば、入院が必要となるような急性増悪をきたすことがありますが、その原因としては、風邪やそれに引き続いておこる気道感染が最も多いといわれます。これを完全に予防することは困難ですが、日頃からうがい、歯みがき、手洗いなど清潔に心がけるとともに、バランスのとれた食事、十分な睡眠、適度の運動などにより抵抗力をつけることが重要です。また、インフルエンザワクチンや肺炎球菌ワクチンの接種も予防につながりますので、医師と相談されたらよいと思います。その他の原因としては、慢性的に酸素が不足していると、肺高血圧から慢性心不全(肺性心)をきたしている場合があり、この心不全が悪化しても急性増悪となります。過度の運動や疲労で酸素が不足した状態を長くつづけていたり、水分の摂りすぎなどが原因でおこることが多く、足のすねの部分がむくんできたり、まぶたが腫れぼったくなったりします。肺性心のある患者さんでは「水分・塩分の摂取量を控えて、利尿剤を服用する、また体動時には酸素吸入量を上げ、過度の運動を避ける」などといったことも悪化の予防になります。
はじめに…
「睡眠時無呼吸症候群」という言葉を聞いたことがある方は多いでしょう。2003年2月に山陽新幹線での居眠り運転事件で有名になり、よく新聞やテレビでもとりあげられています。実は、眠気だけでなく高血圧や心疾患など、身近な病気に密接に絡んでいます。睡眠時無呼吸はとてもありふれた病気で、50歳以上の男性の約2割・女性の1割に、治療対象となる睡眠時無呼吸があると推定されています。以下の内容をご覧になって、心当たりがある方は、一度医療機関を受診されてみてはいかがでしょう。
睡眠時無呼吸症とは
睡眠時無呼吸の大部分は、睡眠中に呼吸が止まったり(無呼吸)、呼吸が止まりかけたりする(低呼吸)、「閉塞性睡眠時無呼吸」です。自覚症状としては、睡眠時のいびき、熟睡できた感覚がない、睡眠の途中で目が覚める、起床時の頭痛、昼間の眠気、集中力の低下などがあります。本人には自覚がなく、睡眠時に呼吸が止まっていることに家族が気づく場合もしばしばあります。睡眠時無呼吸は、仕事や日常生活の支障となったり、交通事故の原因となったりするだけでなく、高血圧・不整脈・脳出血・心筋梗塞など様々な合併症を引き起こします。重症であれば無治療で寿命も短くなることがわかっており、積極的な治療をお勧めします。
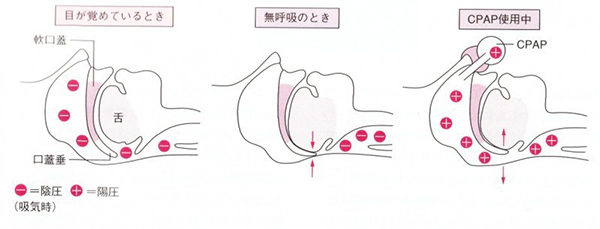
睡眠時無呼吸の原因
閉塞性睡眠時無呼吸は、多くの場合空気の通り道である気道が、部分的あるいは完全に閉塞してしまうことにより起こります(図1参照)。肥満のある人や、首が短くて太い人、あごが小さい人は特に気道が狭い傾向にあり、睡眠時無呼吸になりやすいことが知られています。睡眠時無呼吸が最も多いのは肥満の中高年男性で、メタボリック症候群の方では約半数に閉塞性睡眠時無呼吸症候群の合併が見られます。
睡眠時無呼吸の診断
原則的に一泊入院して、睡眠中の脳波、酸素濃度や胸郭の動き、脈拍、鼻や口からの気流などを計測し(この検査をポリソムノグラフィーといいます)、データを解析して睡眠中の無呼吸、低呼吸の回数を調べます。ご自宅でできる簡易型のポリソムノグラフィーもあります。
睡眠時無呼吸の治療
血圧や糖尿病などその他の生活習慣病の改善のためにも、肥満がある場合はまず減量に取り組みましょう。ただし、減量のみでは無呼吸は十分に改善しない場合も多く、一定以上の無呼吸がある場合は、無呼吸そのものの治療が勧められます。また、アルコールや睡眠薬・抗不安薬は咽頭の筋肉の緊張をゆるめるために気道の閉塞を悪化させるの
経鼻的持続陽圧呼吸療法装置(CPAPといいます)(図1、2参照)
一定の圧力を加えた空気を鼻から送り込むことにより、気道の閉塞を取り除く装置で、閉塞性睡眠時無呼吸の治療の第一選択と考えられています。ポリソムノグラフィーで計測した睡眠1時間あたりの無呼吸低呼吸が20回以上(簡易型では40回以上)で保険適用となります。
口腔内装置(マウスピース)(図3参照)
上下の歯間に固定して、上気道閉塞の原因の一つである下あごの沈下を防ぐ装置です。歯科医師に作成してもらいます。主に軽度から中等症の閉塞性睡眠時無呼吸の患者さんに効果があります。
手術
肥満がなく気道閉塞の主な原因が扁桃腺の肥大やアデノイドであれば、手術が良い適応となりますが、対象となるのは主に小児の睡眠時無呼吸です。
最後に…
以下の症状がある方は睡眠時無呼吸の疑いがあるので、一度医療機関を受診してみることをおすすめします。特に肥満・高血圧・糖尿病などの生活習慣病や、心臓・血管のご病気をお持ちの方は、注意が必要です。
- いびきがひどいといわれる。時に息が止まっている。
- 十分に睡眠をとっているはずなのに、昼間に眠たくなる。
- 夜間によく目覚めてしまう。息がつまる感じがある。
COPDはChronic(慢性)、Obstructive(閉塞性)、Pulmonary(肺)、Disease(疾患)の頭文字で、喫煙による炎症で肺胞の壁破壊や気管支の狭窄により慢性的に咳、痰、息切れを引き起こす病気です。
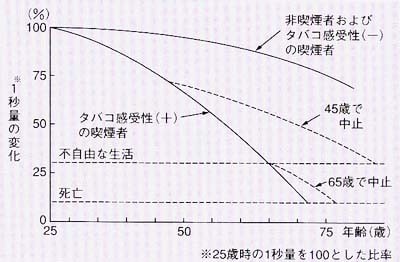
COPDの原因
以前は大気汚染もCOPDの原因でしたが現在の先進国ではほとんどの原因は喫煙にあります。喫煙歴がない人はほとんどCOPDになりませんので喫煙がCOPDの原因であることはたしかですが、喫煙者全員がvの原因になるわけでなく、喫煙者の約15%程度がCOPDに進展しますが、残りの85%の喫煙者はCOPDにはなりません。そのため喫煙以外にたばこの感受性(肺気腫になりやすさ)の要素かあると考えられています。しかし現在でも肺気腫になる人とならない人の違いはわかっておらず、また予測することもできません。COPDにならないためにはタバコから離れて生活することしかありません。ある予測では45歳までに喫煙をやめればCOPDにならずにすむが65歳以降に喫煙をやめてももはやCOPDは避けられないと報告しています。またCOPDになった人も早急に喫煙をやめないとCOPDは進行していきます。COPDと診断されて最も重要なことは直ちに禁煙することなのです。
COPDの症状
咳、痰などの症状から始まり、徐々に動いた時の息切れ(特に階段昇降時)を呈し、やがて軽度の日常動作でも呼吸困難を起こすようになります。重症化すると、呼吸に多大のエネルギーを使うため痩せ、筋委縮、体力低下が起きて寝たきりになりかねません。
COPDの診断
COPDの治療
禁煙
すでに肺や気道の傷んだ部分を回復する方法はありません。これ以上進行しないように直ちに禁煙することが先決です。喫煙したまま投薬等を受けても悪化はさけられないからです。禁煙外来では禁煙補助薬(ニコチン禁断症状を軽くする)を使用して医師の指導のもと禁煙を行うことができます。
薬物療法
禁煙した上で気管支拡張薬(抗コリン剤、長時間作動型β2刺激剤)の吸入を行うのがもっとも有効な治療法です。また重症例や増悪を繰り返す例では、吸入ステロイドを併用します。現在では、長時間作動型の抗コリン薬、β2刺激剤、吸入ステロイド、またそれらの合剤が複数市販されており、個々の患者さんに適した吸入薬が選択されます。これらの吸入には即効性はなく、しんどい時ではなく毎日定期的に吸入することが大切です。耐えられる運動量を上昇させ(つまり息切れしてできなかったことができるようになる。)、生活の質を改善させますが、予後(あと何年生きれるかという期間)は延長しないと考えられています。
その他、去痰薬や、重症時にはステロイド薬を使用します。
酸素療法
進行した場合、不足した酸素を補うために在宅酸素療法(家に酸素の機械を設置して家庭内や運動時に酸素を吸う治療)が必要です。在宅酸素療法は予後延長効果が認められています。血液中に二酸化炭素がたまるとマスク型の人工呼吸器が必要となることもあります。
リハビリテーション
呼吸不全に加え、COPDは全身の炎症をもつ疾患でもあり、その結果筋肉量の減少や栄養障害をきたします。下肢筋力強化や呼吸リハビリテーションなどの運動療法は薬物療法に上乗せ効果を持ちます。また体重減少は呼吸不全への進行や死亡のリスクが高いとされており、やせを防ぐ栄養療法が重要です。
急性増悪
COPDの方には急性増悪といって肺炎、気管支炎を引き起こすのをきっかけとして危機的な状態の悪化を招くことがあり、重症の人ほど頻度が高いことが知られています。息切れが急速に進行する場合などにはこの可能性があります。ほとんどの場合、入院治療が必要で致死率も高い状態といえます。去痰薬やマクロライド系抗生物質、ワクチン(インフルエンザ、肺炎球菌)などが増悪予防に効果があるとされています。
COPDの予後
息切れ感出現後の5年生存率(5年後に何%生きているかという指標)は約70%、10年生存率は40%程度とされています。特に高齢者と喫煙続行者は予後が悪いことが知られています。またCOPDの方は後年、肺癌を合併しやすいと考えられています。
最後に
45歳以上で10年以上の喫煙歴があり、咳、痰、労作時の息切れ感がある人は一度病院受診されることをおすすめします。
ぜんそく(喘息)とは空気の通り道である「気管支」の慢性の病気です。喘息患者さんの気管支には慢性的な炎症があり、このため刺激に対して反応しやすくなっています(気道過敏性といいます)。刺激に対して気管支が反応して細くなった状態が「喘息発作」で、細くなった気管支を通して呼吸をするので、呼吸をするときにゼイゼイ・ヒューヒューという音がし、息苦しさを感じます。気管支の狭窄は治療により、あるいは自然に改善するのが喘息の特徴です(可逆性の気流制限)。喘息は症状の強い病気ですが、症状への慣れが起こりやすいため、病状を正しく判断することが難しくなり、そのため適切な治療がなされないことが少なくありません。喘息を正しく治療するためには、まず、喘息という病気を理解することが必要です。
気道炎症とは
喘息患者さんの気道には慢性的に炎症があります。好酸球という細胞が炎症に関与していることが知られていましたが、最近ではリンパ球や好中球など他の炎症細胞やその他、様々な物質も関与していることが分かってきました。症状のないときにも炎症は持続しているため、発作時以外でも治療は続ける必要があります。(後述)
炎症の程度をみるためには、痰の中にある炎症細胞の数や吐く息の中の一酸化窒素(NO)という物質の濃度を測定します。
気道過敏性とは
喘息患者さんの気管支は炎症を起こしていて、ちょうど火傷したときみたいに腫れています。火傷をしていると、ちょっと触っただけでも痛みを感じるのと同じように、喘息患者さんの気管支も刺激に対して過敏に反応するようになります。(これを気道過敏性といいます)。普通の人では刺激にならないようなもの、例えばタバコの煙、花粉、あるいは冷たい空気などに簡単に反応して、空気の通り道が細くなります。
気道過敏性の程度は気管支を収縮する物質(メサコリンなど)を用いて評価することができます(メサコリン気道過敏性検査)。
可逆性の気流制限とは
気管支が細くなると空気の流れが制限されます。これを気流制限といいます。喘息患者さんの気流制限は治療により元に戻るのが特徴とされてきました。これを可逆性の気流制限といいます。近年、喘息患者さんの気流制限が徐々に固定化していくことが分かってきました。つまり、気管支が徐々に硬くなり、細くなるのです。(リモデリングといいます。)発作の予防と同時に、進行する気流制限の予防が喘息治療における今後の重要なポイントと考えられています。
喘息患者はどれくらいいるのでしょうか?
呼吸器の病気の中では最も多く、100人中3~5人いると推定されています。喘息の有病率は年々増加しています。また中高年ではじめて発症する人も多く、近年は高齢者の喘息が注目を集めています。
喘息の症状は?
喘息の症状には以下のものがあります。
- 息が苦しい、息がすぐに切れる(呼吸困難)
- 喉や胸がゼイゼイ・ヒューヒュー・ピーピー鳴る(喘鳴、ぜんめい)
- 咳が何日も続く(痰の絡むことも空咳のこともあります)
喘息患者さんのすべてが喘鳴や呼吸困難があるわけではありません。一部の人では咳だけが喘息の症状であることもあります(咳喘息)。喘息の咳は夜間から早朝、そして運動時に出ることが多く、喘鳴や胸部の症状も夜間や早朝に強まる傾向にあります。ごく軽い喘息症状でも放置しておくと次第に増悪する場合が多いようです。症状が軽いうちにきちんと治療することで、症状が次第に悪化することを防ぐことができます。
なぜ喘息になるの?
喘息の根本的な原因は未だによく知られていません。喘息の患者さんは家族にも喘息の方がいる場合も多く、何らかの遺伝的素因が関与していることが分かっています。近年の遺伝子解析の進歩で喘息に関係する遺伝子が一部解明されつつありますが、その全貌が明らかになるのには、まだまだ時間を要するでしょう。
喘息にはタイプがありますか?
一つの分け方として、ハウスダスト・ダニ・花粉などへのアレルギーが強く見られる喘息(アトピー型喘息といいます。)と、アトピー体質に乏しい喘息(非アトピー型といいます。)があります。近年、喘息の多様性が強調されており、他にも様々な分類が試みられています。
1. アトピー型喘息
室内環境や屋外の様々な有機物に対して、アレルギーを起こして喘息になるタイプです。アトピー性皮膚炎やアレルギー性鼻炎を合併しやすく、アレルゲンの回避や除去が有効なことがあります。
2.非アトピー型
喘息発作を引き起こすアレルギー物質が特定できないタイプです。
危険な発作の兆候とはどんなものですか?
次のような症状がでる前に病院に受診することが必要です。もしでてしまったらただちに(場合によっては救急車で)病院を受診する必要があります。
- 会話の際、息継ぎが必要、大きな声がでない
- いつも使う吸入薬(気管支拡張薬)の効きが悪い・効かない
- 軽くても連日起こる発作
- 最近、重症の発作を起こしたことがある場合(入院したり救急外来に飛び込んだり)
- トイレにいけないとき、失禁してしまうとき
- 苦しくて横になれない状態が続くとき
喘息は根治可能ですか?
現状では残念ながら喘息という疾患は根治できません。ただ発症後早いうちに十分に治療すれば、多くの喘息患者さんでは完全に症状を落ちつかせるようにコントロールすることはできます。一部の患者さんでは完全に治療を中止できる場合もありますが、その場合でも症状が再発する可能性は常に残っています。一方、喘息の症状を放置しておくと、炎症のため気管支や肺の組織が破壊されて、機能が次第に落ちて回復しなくなると考えられています。こうなると治療を中止できないばかりか、治療をしても症状が十分改善しなくなります。早期の適切な治療が大切です。
喘息の治療薬について教えてください
喘息の治療薬は毎日用いる長期管理薬と発作のときに頓用で用いる発作治療薬に分けられます。
長期管理薬
長期管理薬の主役は吸入ステロイドです。ステロイドは喘息の本態である気道の炎症を最も強力に抑えることができる薬で、吸入で用いることにより全身性の副作用はほとんどなく安全に用いることができます。毎日吸入することで気道の炎症を抑制し、気道過敏性(前述)を改善、発作を予防します。
吸入ステロイド単独でコントロールできない場合
吸入ステロイドと長時間作動型のβ2刺激薬の合剤を用います。その他、ロイコトリエン受容体拮抗薬、テオフィリン製剤、長時間作動型の抗コリン薬といった薬を併用します。吸入ステロイドや併用薬を十分に使用してもコントロールできない重症喘息に対しては、近年抗IgE抗体や抗IL-5抗体といった生物学的製剤が使えるようになりました。
発作治療薬
発作治療薬の主役は短時間作動型気管支拡張薬(短時間作動型β2刺激薬)の吸入です。吸入ステロイドを毎日吸入し、症状が出たときに短時間作動型β2刺激薬の頓用吸入をするのが基本です。より重症の発作ではステロイドを飲み薬や点滴で用います。ただし、喘息治療の本来の目標は、普段の治療で発作治療薬を必要としない状態にコントロールすることにあります。
コントロールが不良になる要因は何かありますか。
喘息発作の原因となるアレルゲンが分かっている場合は、アレルゲンの回避や除去に努めましょう。タバコは厳禁です。禁煙は必ず守ってください。アレルギー性の鼻炎や副鼻腔炎、胃酸の逆流(逆流性食道炎)、肥満、睡眠時無呼吸症候群などを合併していると、喘息のコントロールが不良になることが知られています。また、過度のストレスなど、精神的要因も喘息悪化のリスクとなることが知られております。このように、合併症の評価・治療やアレルゲンの回避や禁煙指導など、トータルに管理していくことが喘息管理においては重要と考えられます。
喘息治療薬は安全ですか?
治療の中心となる薬は吸入ステロイド薬とβ2刺激吸入薬ですが、いずれも全身的副作用は極めて少なく、安全性に特に問題はありません。たとえ妊娠中でも安全です。妊娠中最も大事なことは、喘息発作を起こさないことです。発作を起こすと酸素が十分に行き渡らなくなり、それが最も胎児にダメージを与えるといわれています。
きちんと治療すれば、健康な生活ができますか?
適切な治療により、多くの患者さんは次のようなことができるようになります。
- 喘息症状なしに様々な運動やスポーツに参加し、活動的に生活できる。
- 喘息症状を気にすることなしに眠れる。
- 喘息が悪化するシーズンや誘因に出会ったときも、喘息の発作を防止できる。
- 肺が充分機能し、良い肺機能を維持できる。
つまり、健常者と変わらない日常生活ができるのです。
一言で肺炎といっても肺炎の中にもいろいろなものがあります。
細菌性の肺炎、ウイルス性の肺炎、薬剤による肺炎、自己免疫疾患による肺炎…などなど。
そのなかでも一般的にいわれる肺炎とは細菌性肺炎、つまりばい菌によって引き起こされる肺炎の事を言います。(その他の肺炎については間質性肺炎の項をご参照下さい。)
昔、抗生物質が無い時代には多くの人が肺炎により命を落としてきました。薬剤が発達した現在では外来治療で治ることも多いです。しかし時に重症化することもあり、現在でも特に高齢者の死因の重要な部分を占めています。
原因となる微生物は?
外来の患者さんの肺炎の原因となる菌
肺炎双球菌、インフルエンザ桿菌(冬にインフルエンザを起こすインフルエンザウイルスとは違うものです)、黄色ブドウ球菌、モラクセラカタラリス、マイコプラズマ、などといった名前のばい菌が原因となることが多いです。
その他にはインフルエンザウィルス(こちらは、かの有名なインフルエンザを引き起こす張本人です。)等のウィルスが多いと報告されています。ウイルスと細菌は同じ微生物でもその大きさや増殖方法に違いがあり全く別のものと考えてください。
実際の臨床の場では原因病原体がわからないことも多いです。
症状は?
熱発、咳、痰といったいわゆる風邪症状を示すことが多いです。他に胸痛、全身倦怠感、呼吸困難等の症状が出ることもあります。これらの症状は肺炎に特有というわけではなく、症状だけでは肺炎という診断はできません。
検査は?
肺炎という診断をするために、胸部レントゲン写真(時には胸部CTスキャン)、血液検査などが必要です。また、原因となる病原体が何かを調べるために、痰の顕微鏡検査や培養検査などを行います。
治療は?
原因となるばい菌に対する抗生物質投与が治療の基本となります。もちろん、安静や水分・栄養分の補給は重要です。
軽症であれば外来治療が可能ですが、外来治療無効の場合や、脱水症状等の全身症状が強い場合、呼吸困難が強い場合には入院の上、点滴治療や酸素吸入が必要なこともあります。このようなことは、高齢者や何らかの基礎疾患がある方の場合に多いです。
予防はできるの?
こうすれば必ず予防できるという方法はありません。
しかし、人混みを避ける、うがい手洗いの励行、といった誰でも知っていることを行うことが、特に抵抗力が落ちている患者さんには重要になります。
慢性的な誤嚥がある方では、食後1~2時間は横にならない、就寝前1~2時間は食べたり飲んだりしないようにしてもらいます。うがい液などを用いて口の中をできるだけ清潔に保ち、ばい菌の口の中での増殖を減らすとともに可能なら上半身を少し起こした状態で眠るようにしてもらいます。こうすることで誤嚥のリスクを軽減させることができます。
また上記のとおり高齢者や何らかの基礎疾患がある方では重症化しやすいため、インフルエンザワクチンや肺炎の原因菌で一番多い肺炎球菌に対するワクチンの接種をかかりつけの医師に相談しましょう。
呼吸リハビリテーションとは?
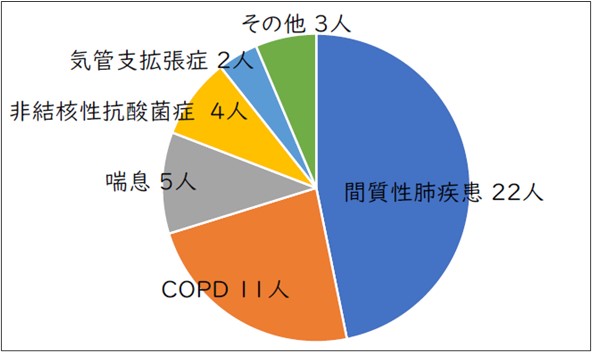
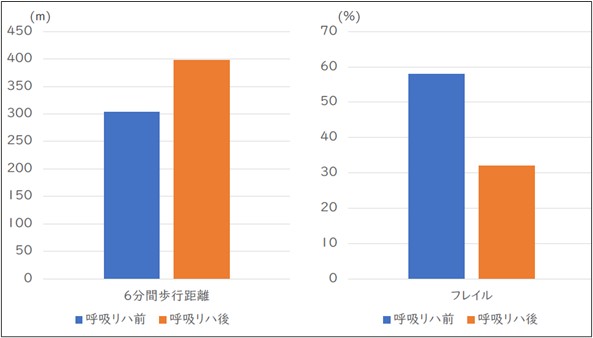
呼吸リハビリテーション(呼吸リハ)は、息切れを和らげ、体力や生活のしやすさを改善するための専門的なリハビリです。COPD(慢性閉塞性肺疾患)、間質性肺疾患、喘息、非結核性抗酸菌症、気管支拡張症など、さまざまな呼吸器疾患の方に効果が期待できます。
呼吸リハは、呼吸器の病気を持つ方が健康状態の回復と維持をめざし、より安心して暮らせるようになるための“総合的なサポート”です。医師、理学療法士、作業療法士、看護師、管理栄養士、ソーシャルワーカーなど多職種の専門家がチームとなり、患者さんと一緒に「できる限り自分らしく生活できること」を目指して取り組みます。呼吸リハビリを通じて、患者さんと医療者が協力しながら、自分で病気を管理していく力を育てていくことが大切です。
呼吸リハビリテーションで行うこと
運動のトレーニング
呼吸の病気があると体力や筋肉が落ちやすくなります。そのため、自転車こぎ(エルゴメーター)、歩行練習、下肢や体幹の筋力トレーニングなどを、専門スタッフが安全に見守りながら行います。運動量は心肺機能や運動能力などの評価に基づき、一人ひとりに合わせて調整するため、無理なく取り組むことができます。
コンディショニング(運動しやすい身体づくり)
運動を効果的に行うために、身体の状態を整える「コンディショニング」を行います。内容として、腹式呼吸・口すぼめ呼吸などの呼吸練習、胸を広げる体操や胸郭の可動域を改善する運動、体のストレッチ、リラクセーション、痰を出しやすくする排痰法などが含まれます。これらにより、運動中の息切れが軽くなり、安全で効率の良いトレーニングが可能になります。
生活を楽にするための支援
階段、歩行、家事、外出などで息が苦しくなりやすい場面を整理し、動き方や休み方のコツ、ペース配分の工夫などを提案します。日常生活がより安全で楽に過ごせるよう、個々の状況に合わせたサポートを行います。
食事と栄養のサポート
体力や筋肉を保つためには食事も大切です。体重の変化や栄養バランス、たんぱく質の不足、食べる量やタイミングについて専門家が評価し、適切な栄養のとり方をアドバイスします。呼吸器の病気では、しっかり食べること自体が治療の一部になります。
病気を自分で管理する力をつける
病気の理解、薬や吸入の正しい使い方、悪化(増悪)のサインの見つけ方、家での安全な運動の方法、活動量を増やす工夫、ストレスとの付き合い方などを学びます。これらは「自分で病気を管理する力(セルフマネジメント)」につながり、安心して生活を続けるために役立ちます。
呼吸リハは、患者さん一人ひとりの状態に合わせて行うオーダーメイドのプログラムです。特にご高齢の方や呼吸の力が低下している方では、状態に応じて適切な内容を選び、無理のない範囲で少しずつレベルを上げていくことが大切です。当院の呼吸リハでは、このように患者さんごとに合わせた方法で進められるよう、十分なサポート体制を整えています。
呼吸リハビリテーションの効果
呼吸リハによって、以下のような効果が期待できます。
- 息切れが軽くなる
- 長く歩けるようになる
- 生活・家事・買い物が楽になる
- 入院や増悪(急な病状悪化)が減る
当院で外来リハビリを行った患者さんでも、運動能力やフレイル(=体力や筋力が弱ってきた状態のこと)の改善が見られています。
呼吸リハビリテーションを希望される患者さんへのご案内
対象となる方
慢性の呼吸器疾患や肺炎・肺手術などの影響で、息切れの悪化や歩く力が低下し、日常生活に支障が出ている患者さん
※年齢は問いません。在宅酸素療法中、神戸市外に在住でも参加可能です。
期間、場所、費用
外来リハビリテーション
- 場所
- 南館2F リハビリテーション室(ポートライナー医療センター駅すぐ
- 時間
- 1回あたり約1時間、週1~2回。期間は最長6か月まで(患者さんの状況に応じてご相談します)。
- 費用
- 医療保険が適用となり、1回あたりの自己負担額は 500~1,000円程度 です。
入院リハビリテーション
当院では、患者さんの状態に応じて入院での呼吸リハビリテーションも行える体制を整えています。息切れや体力の低下が強い場合や、通院が難しい場合には、入院でより安全に集中的なリハビリを受けていただくことができます。
入院が必要な際には、まず当院に短期間入院して初期評価とリハビリの導入を行い、その後、神戸市内の連携回復期リハビリテーション病院(神戸リハビリテーション病院、西記念ポートアイランドリハビリテーション病院、神戸平成病院)へ転院して、4~8週間ほどリハビリを継続します。その後は、外来でリハビリを続けることができます。 入院費用は、リハビリ以外の一般的な入院と同様です。



申し込み
呼吸リハビリテーションの申し込みは、当科外来から行っています。当科に通院中の患者さんで呼吸リハビリをご希望の方は、診察時に担当医へお知らせください。当科を受診されていない方は、現在のかかりつけ医の先生を通じて、当科初診外来の予約をお取りいただくようお願いいたします。
呼吸リハビリテーションの概要と効果
呼吸リハは、息切れの軽減・運動耐容能の改善・生活機能の向上を目的とした科学的根拠に基づく包括的介入です。対象疾患は COPD、間質性肺疾患、喘息、気管支拡張症など幅広く、慢性呼吸器疾患患者に共通する息切れ・身体機能低下・日常生活の困難を改善するための運動療法・呼吸練習・コンディショニング・栄養支援・生活指導・セルフマネジメント支援を組み合わせて実施します。当院で外来呼吸リハを行った患者さんにおいても運動能力の向上や、フレイルの改善が実際に確認されています。
高齢の呼吸器疾患患者では、種々の慢性疾患が併存することが多く、呼吸機能の低下に加えて 筋力低下・活動量の減少・フレイル が併存しやすく、症状の悪化や入院リスクを高めます。そのため呼吸リハでは、単なる運動訓練にとどまらず、多面的支援によって包括的介入を行い、生活機能の改善・在宅生活の維持・再入院予防を目指します。
当院と神戸市における呼吸リハの提供体制
慢性呼吸器疾患においてリハビリの推奨度は高く、有症状の呼吸器疾患患者には「リハを行うかどうか」ではなく「どのようにリハビリを行うか」という視点で実装の取り組みが必要です。しかしながら、現実的には医療資源や診療報酬の問題もあって、急性期を除く回復期・生活期において十分な呼吸リハビリテーションを提供できる体制を有する地域は、これまでほとんどありませんでした。
当院では、呼吸器内科医、理学療法士、作業療法士、看護師、管理栄養士、ソーシャルワーカーなどが連携し、高齢者の特徴に合わせたオーダーメイドのリハビリプログラムを外来で提供できる体制を整えています。また、通院が困難な場合や、より集中的な介入が望ましい場合は、当院での短期入院の後、神戸市内の連携回復期リハビリテーション病院で継続的に入院リハビリを行える仕組みを整備しています。これらの病病連携は、神戸市が提供する地域一体化リハビリテーションプログラム(CURE-KOBE)の一部として提供され、さらに退院後は地域の医療機関の皆様とともに、地域全体として健康寿命の延伸を目指しています。
呼吸リハの紹介手順
対象となる患者さん
慢性呼吸器疾患や肺炎・肺手術などの影響で、呼吸機能・身体機能が低下し、日常生活に支障が出ている患者さん
※年齢は問いません。在宅酸素療法中、神戸市外に在住でも参加可能です。
予約取得
対象となる患者さんがおられましたら、当科初診外来の予約をお取りいただくようお願いいたします。呼吸リハビリテーションを目的とした紹介の場合、普段の診療や投薬は、原則としてこれまでの医療機関で継続していただきます。
そのため、
- 呼吸リハ目的の紹介であること
- 当院での薬剤調整や診療継続をご希望されるかどうか
について、紹介状にご記載いただきますようお願いいたします。
予約について
医療機関からのWEB・FAX予約はこちらをご覧ください。
※WEB予約をご利用されるには事前に登録が必要です。くわしくはこちらをご覧ください。
ご予約の際の診療情報提供書はこちら(PDF/WORD)です。
問い合わせ先
患者総合支援センター FAX:(078)302-2251
TEL:(078)302-6031
予約受付時間 月~金 9:00~19:00・土 9:00~13:00 ※祝・日・年末年始除く
期間、場所、費用
外来リハビリテーション
- 場所
- 南館2F リハビリテーション室(ポートライナー医療センター駅すぐ)
- 時間
- 1回あたり約1時間、週1~2回。期間は最長6か月まで
(患者さんの状況に応じてご相談します)。
- 費用
- 医療保険が適用となり、1回あたりの自己負担額は 500~1,000円程度 です。
入院リハビリテーション
息切れや体力の低下が強い場合や、通院が難しい場合には、入院でより安全に集中的なリハビリを受けていただくことができます。入院が必要な際には、まず当院に短期間入院して初期評価とリハビリの導入を行い、その後、神戸市内の連携回復期リハビリテーション病院(神戸リハビリテーション病院、西記念ポートアイランドリハビリテーション病院、神戸平成病院)へ転院して、4~8週間ほどリハビリを継続します。その後は、外来でリハビリを続けることができます。入院費用は、リハビリ以外の一般的な入院と同様です。



患者さんが住み慣れた地域でできる限り自立した生活を続けられるよう、当院も、地域の先生方と力を合わせて取り組んでまいります。
引き続き、忌憚のないご意見とご支援を賜りますようお願い申し上げます。
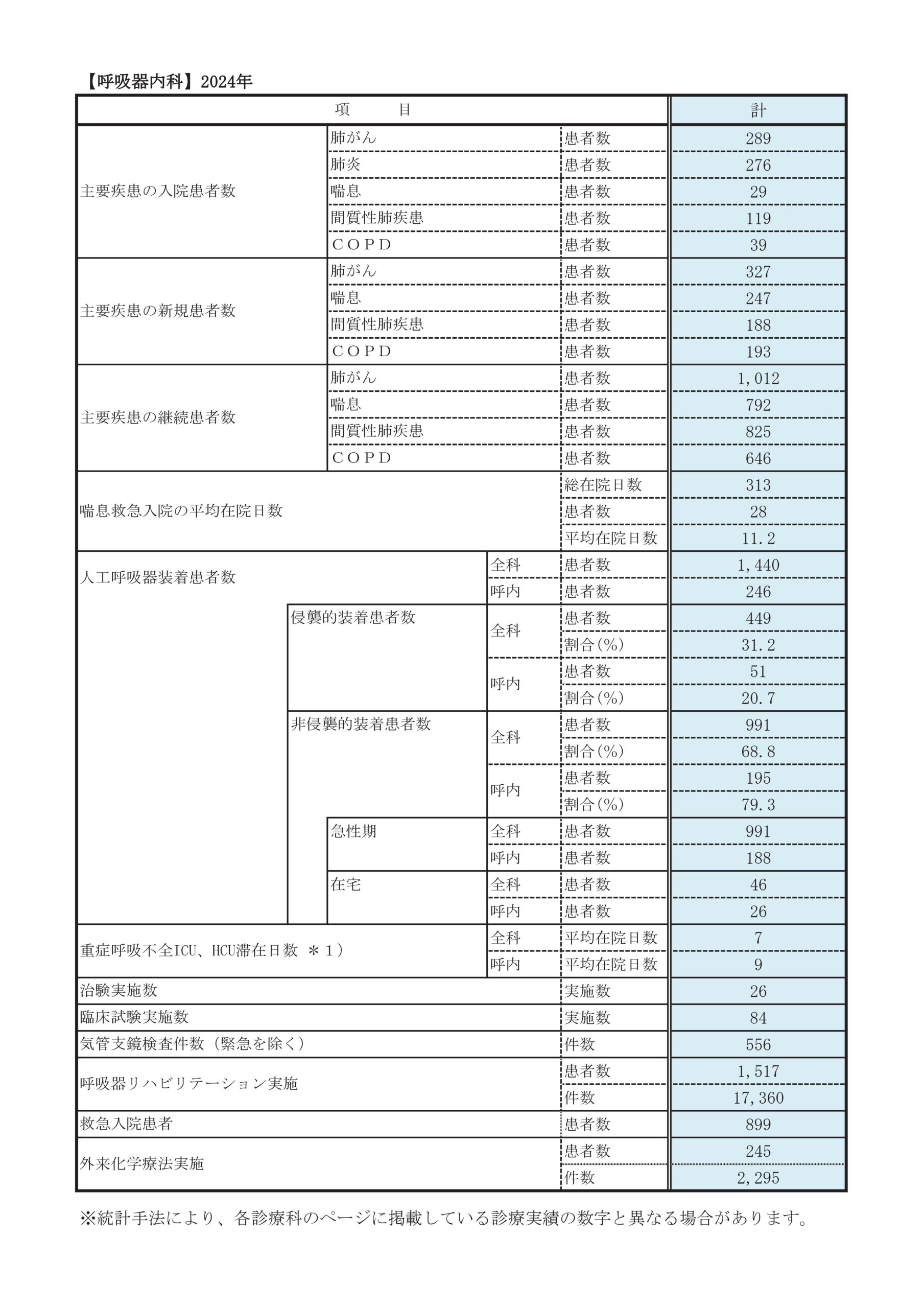
診療実績
診療科別統計
臨床研究
| 研究課題名 | 研究責任者 | 研究実施期間 | 添付資料 |
|---|---|---|---|
| 進展型小細胞肺癌患者に対する初回治療 カルボプラチン/エトポシド/アテゾリズマブ併用療法の 実地診療における有効性、安全性を検討する 多施設前向き観察研究における5年アップデート |
佐藤悠城 |
2026年1月~ |
|
| 胸部悪性疾患における免疫応答解析に基づくT細胞誘導二重特異性抗体治療の効果予測因子および耐性機序に関する多施設共同研究 |
佐藤悠城 |
2025年11月~ |
|
| 日本人のⅣ期HER2 変異陽性非小細胞肺癌に対するT-DXd 治療に関する多施設共 同後ろ向き観察研究(REAL-HER2 Study)(WJOG21224L) |
佐藤悠城 |
2025年11月~ |
|
| 弧立結節影を呈する肺MAC症および肺M.kansasii症に関する後方視的研究 |
平林亮介 |
2025年8月~ |
|
| EGFR遺伝子変異陽性肺癌患者においてHER2異常がEGFR-TKIの効果と予後に与える影響の解明(HERITAGE study) |
神戸寛史 |
2025年8月~ |
|
| EGFR uncommon変異を有する進行・再発非小細胞肺がん患者における初回EGFR-TKI治療の臨床アウトカムに関する他施設共同後ろ向き観察研究 |
佐藤悠城 |
2025年6月~ |
|
| 限局型小細胞肺癌に対する化学放射線療法による放射線肺臓炎の実態を調査する多施設共同後ろ向きコホート試験 |
佐藤悠城 |
2025年4月~ |
|
| デュピルマブ投与による好酸球性臓器障害の実態調査 |
立川 良 |
2025年2月~ |
|
| 肺扁平上皮がんにおけるSPARC 発現強度とカルボプラチン+nab-パクリタキセル及びドセタセルの効果の関連を検討する後ろ向き観察研究(CJLSG2402) |
佐藤悠城 |
2024年12月~ |
|
| 日本版PCTガイド下抗菌薬治療アルゴリズムを用いた抗菌薬投与の有用性の検討 |
立川 良 |
2024年11月~ |
|
| 慢性閉塞性肺疾患の患者に対する増悪入院後のリハビリテーションについて |
白川千種 | 2024年10月~ 2028年3月 |
|
| 住民の健康改善に資するエビデンス創出を目指した多地域コホート研究:LIFE Study | 白川千種 | 2024年10月~ 2028年3月 |
|
| 線維化を伴う間質性肺炎の急性憎悪で入院した患者の入院前のフレイルの有無と予後の関連性についての後ろ向き観察研究 | 立川 良 | 2024年10月~ 2026年12月 |
|
| 悪性胸水に対する胸膜癒着術の検討 | 佐藤悠城 | 2024年7月~ 2026年3月 |
|
| アジアにおける肺癌個別化医療の確立を目指したゲノムスクリーニング研究(LC-SCRUM-Asia 5期) | 佐藤悠城 | 2024年7月~ 2027年3月 |
|
| 在宅高流量鼻カニュラ酸素療法(HFNC)の使用実態とその有効性に関する多施設共同研究 | 富井啓介 | 2024年4月~ 2025年3月 |
|
| 日本の急性期総合病院を対象とした下気道感染症のデータベース構築と再発性下気道感染症に対する抗緑膿菌活性をもつ抗菌薬の経験的使用の有効性の検討:多施設後ろ向きコホート研究(多機関共同研究) | 富井啓介 | 2023年11月~ 2027年12月 |
|
| 固形癌における免疫応答解析に基づくがん免疫療法の効果予測診断法確立に関する多施設共同研究 | 富井啓介 | 2023年11月~ 2026年3月 |
|
| 過敏性肺炎の全国疫学調査 | 富井啓介 | 2023年9月~ 2027年3月 |
|
| EGFR遺伝子L858R変異陽性進行再発非扁平上皮非小細胞肺癌に対するRamucirumab + Erlotinibの有効性及び安全性を評価する多機関共同・後方視的観察研究(REAL-SPEED) | 佐藤悠城 | 2023年8月~ 2026年12月 |
|
| 局所進行非小細胞肺癌に対する化学放射線療法を受けた患者の後ろ向き研究(HOPE-005/CRIMSON)に付随する画像評価の検討 | 佐藤悠城 | 2023年2月~ 2028年1月 |
|
| EGFR変異陽性肺癌患者における組織転化症例における免疫微少環境と臨床経過の検討(HISTORIC-TR) | 佐藤悠城 | 2023年1月~ 2025年5月 |
|
| 非小細胞肺癌における薬物療法耐性後の個別化医療の確立を目指した、遺伝子スクリーニングとモニタリングのための多施設共同前向き観察研究(LC-SCRUM-TRY) |
佐藤 悠城 | 2022年10月~ 2035年9月 |
|
| 要介護1以上かつ65歳以上の慢性閉塞性肺疾患の患者に対する早期リハビリテーションと再入院との関連 | 富井啓介 | 2022年7月~ 2027年3月 |
|
| EGFR遺伝子L858R変異陽性進行再発非扁平上皮非小細胞肺癌におけるTP53遺伝子変異の意義および治療耐性メカニズムの検討(WJOG14420LTR) | 佐藤悠城 | 2022年2月~ 2028年2月 |
|
| 進行・再発非小細胞肺癌のバイオマーカー検査と標的治療に関する実態調査プロジェクト | 佐藤悠城 | 2022年1月~ 2025年12月 |
|
| 希少ドライバー遺伝子異常をもつ肺癌患者の後方視的調査 | 佐藤悠城 | 2021年7月~ 2027年3月 |
|
| COVID-19の病態解析・重症化のメカニズムの解明 | 富井啓介 | 2021年6月~ 2026年1月 |
|
| COVID-19の予後予測因子の同定と臨床応用に関する研究 | 富井啓介 | 2020年9月~ 2025年3月 |
|
| 新型コロナウイルス感染症の重症化機構の解明 | 富井啓介 | 2020年9月~ 2025年3月 |
|
| EGFR遺伝子変異陽性非小細胞肺癌に対する初回治療Osimertinibの多施設実態調査に付随する薬剤性肺障害の検討 | 佐藤悠城 | 2020年9月~ 2025年3月 |
|
| びまん性肺疾患の疫学およびバイオマーカに関する研究 | 富井啓介 | 2020年8月~ 2030年4月 |
|
| 進展型小細胞肺癌患者に対する初回治療カルボプラチン/エトポシド/アテゾリズマブ併用療法の実地診療における有効性、安全性を検討する多施設前向き観察研究に付随するバイオマーカー研究【APOLLO-Bio】 | 富井啓介 | 2020年3月~ 2025年9月 |
|
| EGFR変異陽性肺癌患者における組織転化の実態調査【HISTORIC】 | 佐藤悠城 | 2020年5月~ 2025年5月 |
|
| コロナウィルス肺炎(CoVP)とインフルエンザウィルス肺炎(InVP)、非ウィルス性市中肺炎(nVCAP)の臨床像に関する多施設共同研究 | 富井啓介 | 2020年4月~ 2025年4月 |
|
| SCRUM-Japan疾患レジストリを活用した 新薬承認審査時の治験対照群データ作成のための 前向き多施設共同研究【SCRUM-Japan Registry】 | 富井啓介 | 2020年2月~ 2028年3月 |
|
| 進行肺がん患者における分子標的治療の止め時に関する多施設観察研究 | 佐藤悠城 | 2019年8月~ 2027年3月 |
|
| 成人市中発症肺炎(COP)における肺炎球菌性肺炎の疫学研究 | 富井啓介 | 2018年8月~ 2027年3月 |
お知らせ
医師、医師を目指す方向け当科のご紹介
※本コンテンツは、医師の方を対象とし、当医療機関についての理解を深めていただけるよう作成しているものであり、一般の方を対象とする宣伝・広告等を目的としたものではありません。 はじめまして、神戸市立医療センター中央市民病院 呼吸器内科の富井 啓介(とみい けいすけ)と申します。
当科では、地域医療支援病院の使命のもと、あらゆる呼吸器疾患に対して24時間365日対応しており、地域の先生方との病診病病連携を通じて地域全体の医療に貢献することをモットーとしております。
本日はその中でも、当院の特色である多職種医療チームが支える肺がんと間質性肺疾患の最新診療をご紹介します。
富井 啓介
副院長
呼吸器内科 部長
①肺がんについて
当院の肺がん治療の特徴
肺がんは2019年の本邦のがん種別癌死亡数で1位とされ、予後不良の疾患ですが、近年治療法の進化が著しく、目覚ましい進歩を遂げている領域です。
当院は阪神エリアを代表する地域がん診療拠点病院として、スタッフ6名、後期研修医10名のもと、
- 総合病院の強みを活かした幅広い診療科間連携のもと適切な標準治療を届けること
- がん遺伝子パネル検査や治験/臨床試験を介して新規治療への橋渡しを行うこと
を通して地域の患者さんやかかりつけ医の先生方に安心して受診や紹介を頂ける病院を目指し、一丸となって肺がん診療に取り組んでおります。
進行度に応じた最適な治療選択とチーム医療による患者QOLの向上
がんの病巣が胸郭内に留まる早期肺がんについては、手術、放射線療法、化学療法の組み合わせを駆使し、あらゆる可能性を考え、根治を目標とした治療を目指します。当院では呼吸器がん診療に関わる呼吸器内科、呼吸器外科、放射線治療科が揃っており、毎週合同カンファレンスを行い密に連携することで、患者さんに合った最良の治療を、最適なタイミングで提供するようにしています。
一方、遠隔転移を伴う進行肺がんは化学療法が主体となります。従来の殺細胞性抗がん剤に加えて、昨今ではPD-1/PD-L1やCTLA-4を標的とした免疫チェックポイント阻害薬や、がんの原因となる遺伝子を特異的に阻害する分子標的薬を用います。分子標的薬はEGFR、ALKが有名ですが、これ以外にROS1、MET、BRAF V600Eに対する阻害薬が保険診療下で使用できるようになりました。これらの治療を駆使し、より多くの患者さんに、一昔前までは到底考えられなかった長期の生存やQOLの維持ができるようになりました。
一方で、抗がん剤の副作用は多彩です。特に免疫チェックポイント阻害薬の副作用はimmune-related adverse events (irAE)と言われ、発見や発症後のマネジメントに熟練を要し、場合によっては内分泌内科、膠原病内科などの専門診療科の連携を要する場合があります。当院では関連する診療科・部門の垣根を越えて適正使用チームを作っており、総合病院の強みを生かした全身管理を行います。また当院は日本でも有数の救命救急センターを有しておりますので、万一の緊急時に安心して受診していただくことが可能です。 さらに院内の緩和ケアチームも活動しておりますので、治療と並行して適切な緩和ケアを行うこともできます。QOLの維持につながる状況であれば、緩和的な放射線療法や、胸水に対するドレナージ等も対応しております。
高度がん治療の提供による患者メリットについて
高度がん治療の一環として、早期から進行期まで全ての病期で、数多くの治験や臨床試験を実施しております。患者さんにとって、新しい薬剤や治療法にアクセスできることや、場合によっては医療費の負担軽減など大きなメリットがあります。 昨今プレシジョン・メディシンという言葉が叫ばれるようになりましたが、がん治療の中でも特に肺がんの薬物療法はこの分野をリードしています。実際に非小細胞肺がんの患者さんに詳細な遺伝子検査を行うと、半数の患者さんに何らかの遺伝子変異が見つかり、分子標的薬を保険診療下で使用することが出来ます。また当院はがんゲノム医療連携病院でありますので、標準的治療が終了した患者さんに対するがん遺伝子パネル検査を行い、効果が期待できる治療薬がないか、検討することが出来ます。この場合にがん細胞の組織採取が重要ですが、当院では超音波ガイド下の気管支鏡やCTガイド下生検など、組織生検に非常に積極的に取り組んでおります。
肺がん疑いの患者さんがいる場合は、まずご紹介ください
進行期肺がんでも約半数は無症状ですので、レントゲンで疑わしいと判断されたすぐの段階で構いません。高齢の患者さんや併存疾患を合併した患者さんであっても、遺伝子変異やPD-L1の状況次第では積極的な治療適応となる場合がありますのでまずはご紹介ください。またがん遺伝子パネル検査目的の紹介も積極的に受け付けております。肺がんにおいては、免疫療法、分子標的薬、殺細胞性抗がん剤2種類に耐性化した時期、胸腺腫瘍・悪性胸膜中皮腫では1種類目の殺細胞性抗がん剤に耐性化した時期ががん遺伝子パネル検査の良いタイミングと考えられます。該当される患者さんで、がん遺伝子パネル検査を希望される方は、当院のがんゲノム検査外来(火曜日午後)にご紹介頂けますと幸いです。
②間質性肺疾患について
間質性肺疾患とは、肺の間質に炎症や線維化を起こす疾患の総称です。病気の進行速度は急性(日単位)から慢性(年単位)まで様々で、咳や息切れが主な症状です。原因は感染・喫煙・アレルギー・自己免疫・薬剤など様々で、まず原因の特定と治療(除去)を行います。
放射線診断科や病理診断科と合同での間質性肺疾患の診断
間質性肺疾患は多彩な呼吸器疾患の中でも特に診断が難しいとされている難病です。当科は間質性肺疾患の診療の経験が豊富で、多くの患者さんが来院されます。診断にあたっては、病歴、身体所見、血液検査、HRCT所見、そして気管支鏡や胸腔鏡による肺生検の結果を総合的に評価する必要があります。そのため呼吸器内科だけでなく、放射線診断科や病理診断科と協議を行い、その診断や治療方針を決定します。
当科では、定期的に全国の間質性肺疾患を専門とする放射線診断科や病理診断科の医師とともに勉強会を行い、これまでの症例について協議を行って診断の精度を高めています。最近では、気管支鏡によって従来の鉗子生検よりも大きな組織を採取できる凍結生検(クライオバイオプシー)を導入し、より容易に病理学的な情報を得ることが可能となりました。
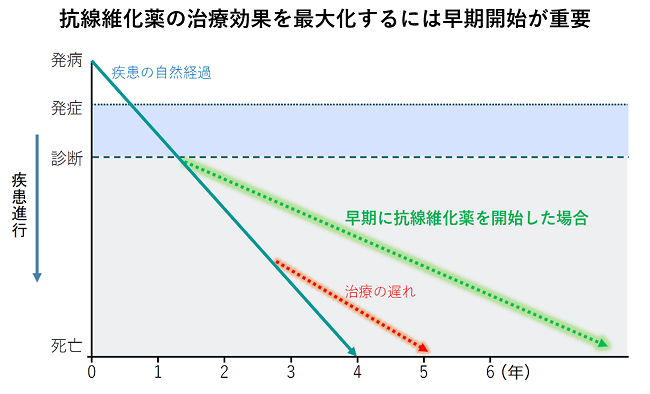
間質性肺疾患に対する新しい薬物療法(抗線維化薬)
特発性肺線維症に対しては、ピルフェニドン(ピレスパ®)とニンテダニブ(オフェブ®)という2種類の抗線維化薬が保険適用となり、薬物療法の中心となっています。これらの薬剤は、線維化の進行を抑え、急性増悪の頻度を減らし、予後を改善させる効果が示されています。最近ニンテダニブは、特発性肺線維症以外の間質性肺疾患に対しても、進行性に線維化がみられる場合に使用可能となりました。ただし病状が進行し肺活量が高度に低下してしまうと、これらの薬剤を用いても症状や肺活量を改善させることは困難です。そのためできるだけ早期に診断し、これらの薬剤を適切なタイミングで開始し、進行を防ぐことが重要と考えられます。また当院では第3の抗線維化薬の治験も継続中です。
多職種チームによる患者サポート
進行性の間質性肺疾患では、最善の治療を行っていても、肺機能の悪化に伴う息切れ・活動量の低下・体重減少が見られることがあります。進行期においては、薬物療法よりも、むしろ機能維持のためのリハビリや緩和治療が重要となる場合もあります。当科では、多職種が介入できる体制を外来でも整えており、包括的な呼吸リハビリテーション、生活指導やアドバンスケアプランニング、公的制度申請など、専門職が協働して患者さんをサポートします。
間質性肺疾患は早期診断早期治療が肝!
間質性肺疾患はできるだけ早期に診断を行い、適切な時期に治療を開始することが大事です。コロナ禍の中ですが、当科ではWebを利用したリハビリテーション教室など、感染対策にも工夫を行いながら診療を行っております。患者さんが咳や息切れを訴えたり、胸部写真やC Tでよく分からない陰影を軽微でも認めた場合には、遠慮なく地域連携室を通して当院へご紹介いただけますと幸いです。
当院の新型コロナウイルス流行下での診療体制について
2020年3月から兵庫県でも新型コロナウイルス感染症が流行し、当院も感染症指定病院として重症例を中心とした対応に日夜取り組んでおります。専用病棟の設置や入院前PCR検査など、考えられる最大の対応を行い、院内感染の予防とともに通常診療の維持を図っております。
新型コロナウイルスとの戦いはまだ続きますが、流行下で検診等の受診控えが目立っており、今後がん患者さんの増加が強く危惧されます。
またコロナ禍の中、リハビリ指導を対面で行うことが困難となっておりますので、当科ではWebを用いた呼吸リハビリテーション教室を行っています。ご自宅のパソコンやスマートフォンを使って、当院の医師や理学療法士から、講義や実技指導を受けていただくことができます。 今後も当院では、あらゆる治療の可能性を探りながら症状緩和や生活の質の維持など患者さんのニーズに応え、見捨てることのない最善の治療を展開してまいりますので、お気軽にご相談ください。
地域医療連携のための勉強会
中央市民病院びまん性肺疾患勉強会
2005年3月より年2回当院講堂にて開催しておりましたが、新型コロナウィルスの影響にて、第30回びまん性肺疾患勉強会(2020年7月11開催)よりZOOMを用いたオンライン配信のみで開催しておりましたが、ようやくコロナも落ち着て参りましたので、2023年10月より当院講堂とZOOM配信のハイブリッドにて実施しております。
次回「第40回びまん性肺疾患勉強会」の開催予定日は、2025年6月28日(土)となっておりますので、参加ご希望の先生は、下記メールアドレスより、参加申し込みいただきます様お願い致します。
| お申込みメールアドレス | konai@kcho.jp |
|---|---|
| メール件名 | 「びまん性肺疾患参加申し込み」 |
2024年11月9日に開催しました、「第39回びまん性肺疾患勉強会」は、64名の先生方にご参加頂きました。ご参加頂きました先生方には、この場を借りて御礼申し上げます。
神戸市立医療センター中央市民病院
呼吸器内科部長代行 立川 良