Gastroenterology There are 18 staff members, The Japanese Society of Gastroenterology 8 supervisors/specialists, Japan Gastroenterological Endoscopy Society 7 supervisors/specialists, The Japan Society of Hepatology 4 supervisors/specialists, The Japan Society of Ultrasonics in Medicine 1 specialist, and experienced veterans and young M.D. staff members cooperate in providing medical care. We also have a full teaching staff for clinical training with The Japanese Society of Internal Medicine 5 certified Fellow of the Japanese Society of Internal Medicine (FJSIM) and 4 internal medicine Certified Physician specialists.
As a facility certification, it is certified as a teaching facility by the Japanese Society of Gastroenterology, the Japan The Japanese Society of Gastroenterology Japan Gastroenterological Endoscopy Society, the The Japan Society of Hepatology, and the Japanese Society of The Japan Society of Ultrasonics in Medicine. As a result of the third year of Reiwa, the number of outpatients in our department is 167 per day, the number of inpatients is 1,866 per year, and the average length of stay is 7.3 days. increase. 40 to 50 patients are receiving inpatient treatment with the 6th floor east, 7th floor west, and 9th floor east wards as basic wards. In addition, one-third of hospitalized patients are hospitalized as emergency patients, and as a designated tertiary emergency hospital, we accept emergency patients from all over Kobe City. Our department also cooperates with the emergency department, and has a system that allows emergency examinations and treatment at any time for 24 hours.
Our department is based on the cooperation of experts in each field and highly specialized co-medical
Aiming for team medicine.
Every week, we hold a “case conference” with all staff. Pharmacists and nutritionists also participate in conferences to support medical care.

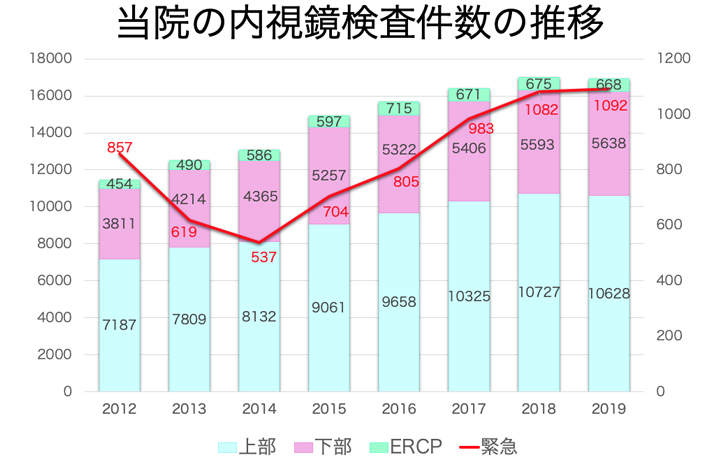
The Endoscopy Center performs approximately 18,000 endoscopic examinations and treatments annually. More than 1,000 emergency endoscopies were performed last year. We actively use sedation (using sedatives) to ensure painless endoscopy.

Medical record
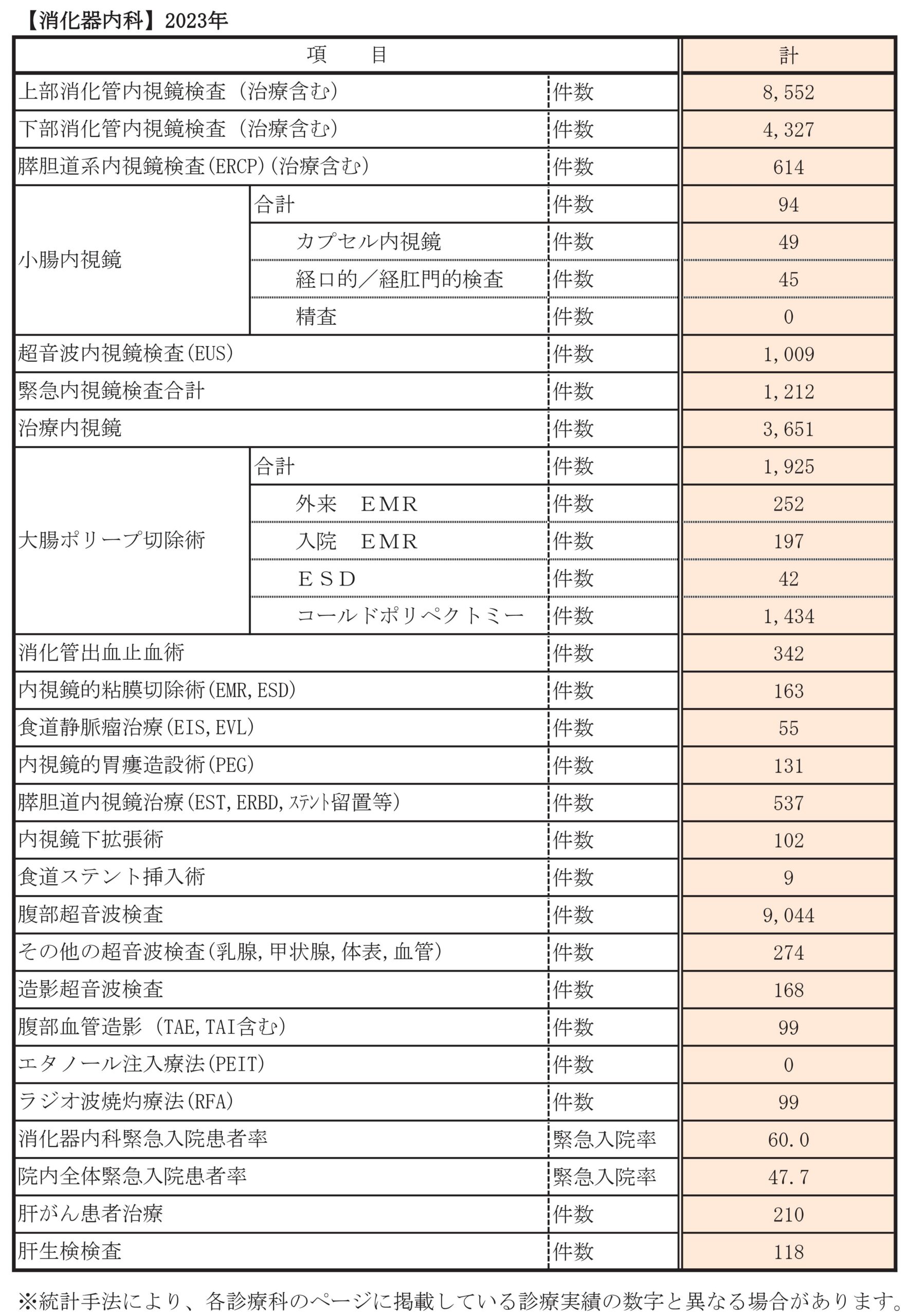
Departmental statistics
Main diseases/treatments

What is sedation endoscopy?
Sedation endoscopy at our department complies with the "Guidelines for Sedation" created by the "Japan Gastroenterological Endoscopy Society", making endoscopic examinations safer and less painful. The aim is to promote early detection of gastrointestinal cancer and less burdensome endoscopic treatment by reducing the patient's anxiety and stress about the examination and increasing the acceptability of the examination.
Conscious sedation is used for the sedation level to reduce side effects such as respiratory depression and blood pressure drop due to excessive sedation.
In addition, in order to conduct the examination more safely, all patients will be monitored with a biological information monitor during the examination, and after the examination, we will try to recover from the sedation in the recovery space. After about 30 minutes of observation, the sedation-arousal score is used to confirm that the patient's level of consciousness has fully recovered, and then the patient is sent home.
Elderly people are encouraged to come with an attendant.
On the day of the examination, please refrain from driving a car, motorcycle, or bicycle.

The Endoscopy Center is located in the Imaging Medicine Department on the 1st floor, and is operated in the largest space (approximately 857m²) among clinical hospitals in the Kinki region. It has 6 endoscopy rooms, 2 X-ray fluoroscopy rooms, and 1 multi-purpose treatment room. We have introduced the latest electronic endoscopes including endoscopes. A 12-bed recovery space will be provided, and after the sedation test, patients will move to the recovery space while lying on their beds, where a dedicated nurse will check their respiratory and circulatory conditions using a centralized monitoring monitor. We strive to ensure that our patients have a safe and comfortable examination experience. We also have a day center, and we actively provide day care (colon polypectomy).
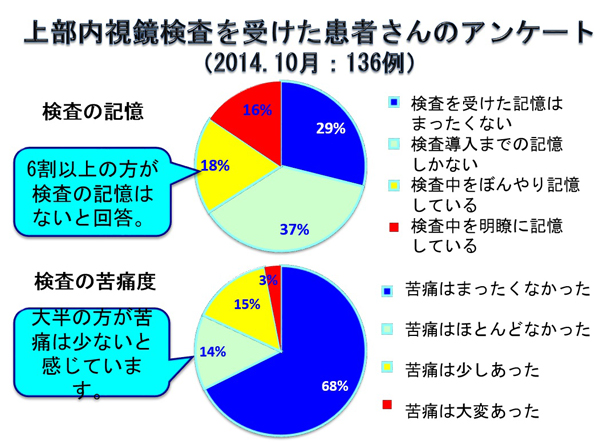
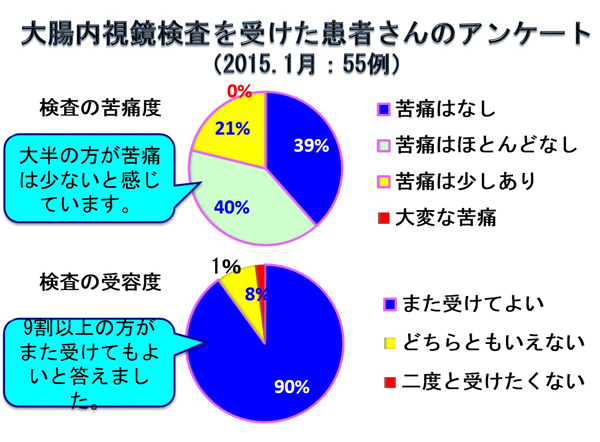
Questionnaire results for the sedation test
A questionnaire was conducted to evaluate patient satisfaction after upper gastrointestinal endoscopy (EGD) and lower gastrointestinal endoscopy (CS). Patients who underwent a sedation examination at our center in October 2014 (136 patients) for EGD and in January 2015 (55 patients) for CS cooperated.
The results are shown in the table.
When asked about their memory of having undergone EGD, 39/136 (29%) had no memory of the examination and barely remembered having undergone the examination. 50/136 patients (37%) only remembered the process from the start of the test until the scope was inserted. . In addition, when asked about the pain of the examination, more than 80% of the respondents said that they felt almost no pain during the examination, as those who had no memory of the examination naturally experienced no pain associated with the examination. As a result, 124/136 (91%) of those who underwent the sedation test answered that they would like sedation from the next time.
This evaluation exceeded our expectations, and we believe that the pain associated with endoscopy was reduced to an acceptable level.
Cancer has become a common disease with the progress of the aging society. Currently, one in two Japanese people will be diagnosed with cancer, and one in three people will die of cancer. We believe that even patients who have been hesitant about undergoing a gastroscopy or colonoscopy because they are too tired to undergo a sedation examination can feel at ease.
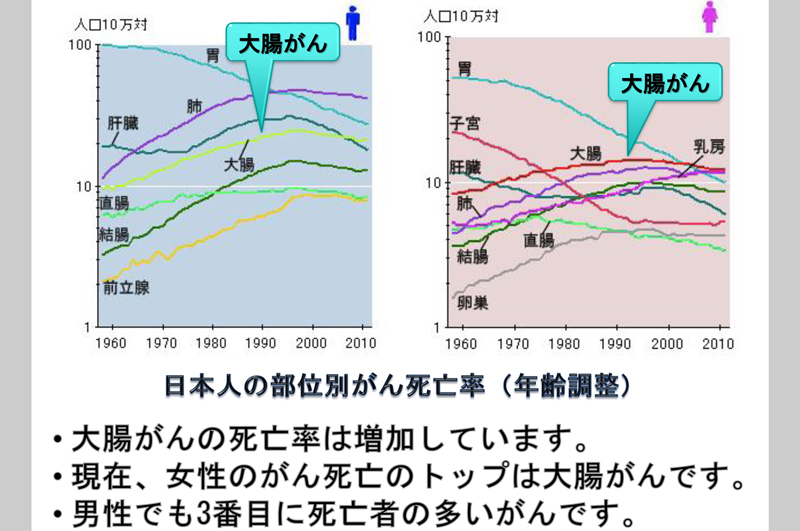
colon cancer is on the rise
Get a colon cancer screening
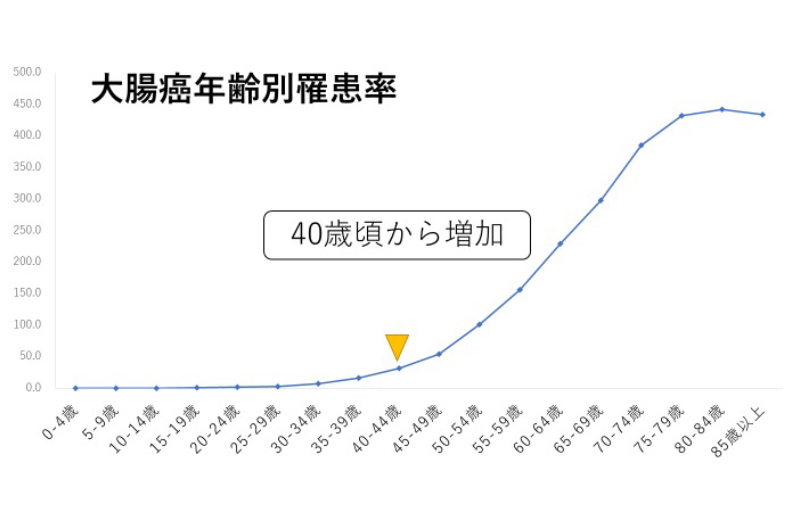
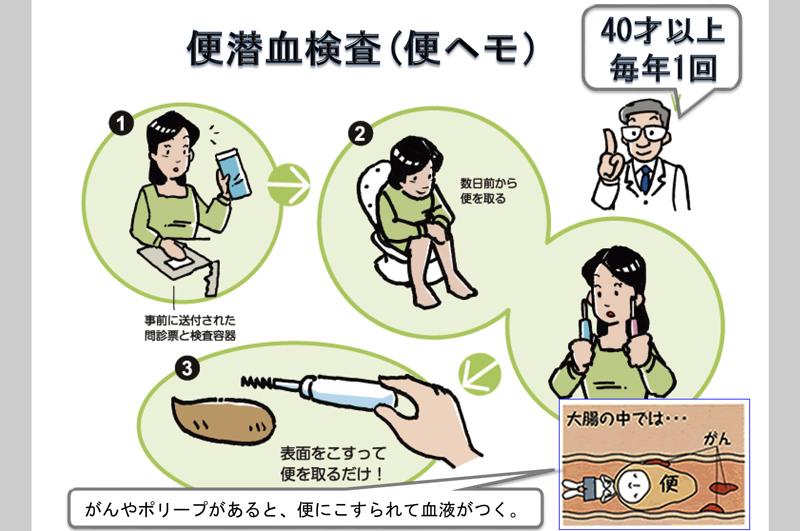
Get a colonoscopy
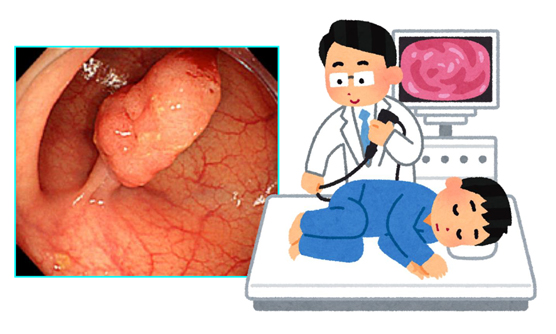
A colonoscopy is an examination in which a soft tube (scope) is inserted through the anus to observe the surface of the large intestine. In advance, you will take a laxative and intestinal tract cleansing solution and excrete stool before observing. There is a report that the mortality rate of colorectal cancer is reduced by 40% by performing endoscopy, and our department is actively doing it. Polyps found are aggressively endoscopically resected. Small lesions can be treated on an outpatient basis.
In our department, more than 5,000 colonoscopies are performed annually, and more than 2,100 one-day polypectomy procedures are performed for colorectal polyps.
Early detection is important
Early-stage cancer has few subjective symptoms, and even today, it is often found in advanced cancer. Endoscopic treatment is also possible for early stage cancer. If you have persistent abdominal pain, abnormal bowel movements (constipation/diarrhea), or anemia, we recommend that you undergo an endoscopy. Many colonic polyps (called adenomas) and early cancers can be completely cured with an endoscope. In the case of advanced cancer, the department of surgery is committed to minimally invasive treatment such as laparoscopic resection, and in the case of distant metastasis, the Oncology actively performs chemotherapy to improve treatment results.
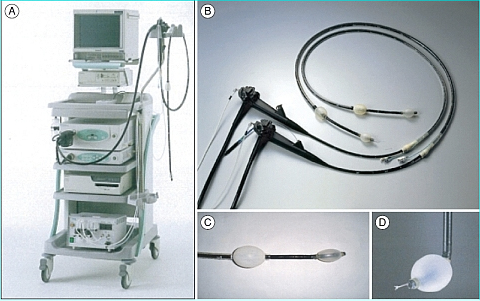
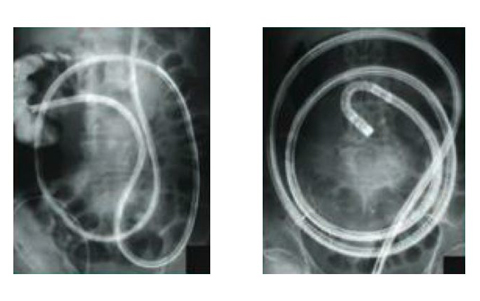
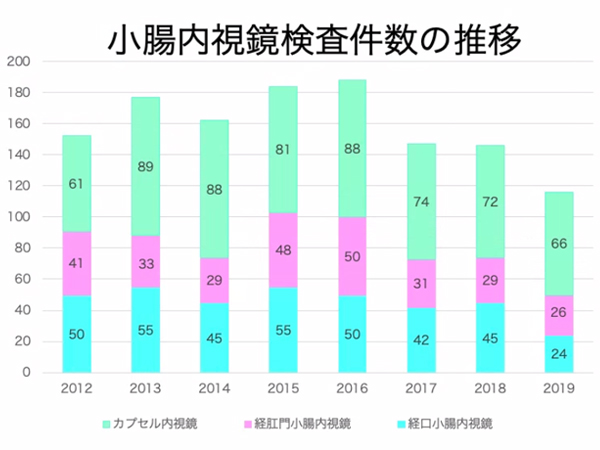
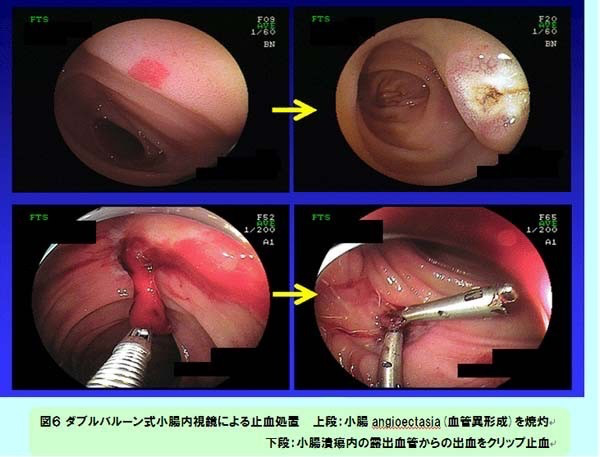
In recent years, we have been actively conducting small bowel endoscopy using a double-balloon type small bowel endoscope for small bowel diseases, which are on the rise. In 2019, it was performed in 50 cases, and accurate diagnosis and endoscopic treatment of small intestinal lesions that could not be detected by conventional examination methods have become possible. In addition, capsule endoscopy was also introduced in June 2008, and was performed in 66 cases in 2019. For small bowel lesions such as gastrointestinal hemorrhage of unknown cause, we have established a system that enables consistent medical care from screening with capsule endoscopy to detailed examination and treatment with double balloon small bowel endoscopy.
Small bowel endoscopy: shedding light on dark areas
Located between the stomach and the large intestine, the small intestine is the longest in the digestive tract, measuring 6 to 7 meters, and is responsible for the digestion and absorption of nutrients. It has long been called the "dark continent of the digestive system" because it is an organ that is difficult to inspect endoscopically. However, the development of a capsule endoscope in Israel in 2000 and a double-balloon enteroscope in Japan in 2001 have made rapid progress in the diagnosis and treatment of diseases of the small intestine.
Since 2003, our department has also performed small bowel endoscopy using a double-balloon small bowel endoscope (FTS EN450P5/20, EN450T5/W, EN-580XP, EN-580T, EC-450BI5) and achieved results. I came. In June 2008, we also introduced capsule endoscopy, which is less invasive and allows observation of the small intestine during outpatient examinations. We have established a system that allows us to provide consistent medical care, from detailed examination to treatment using a double-balloon small intestinal endoscope. We are one of the largest hospitals in the Kinki region, with more than 100 examinations per year including both.
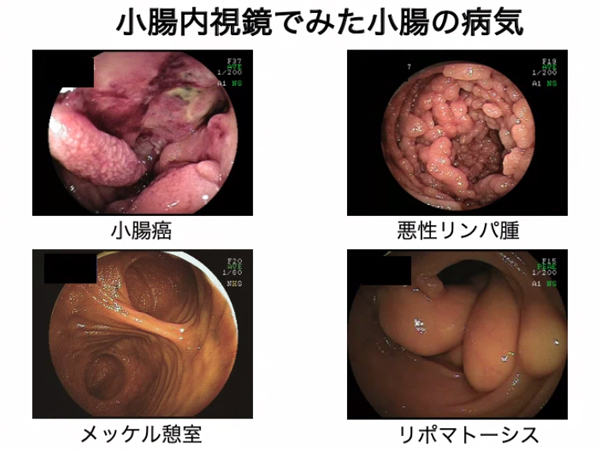
Small bowel disease and endoscopy
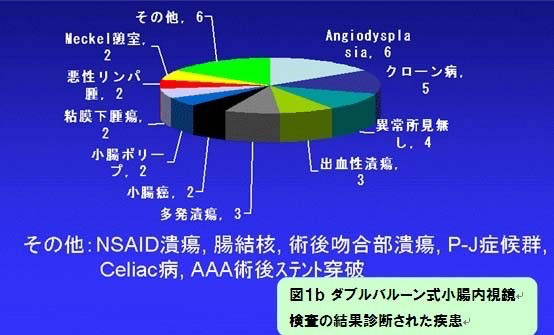
As mentioned above, there were many unknowns about the disease of the small intestine, which was called the "dark continent". However, with the introduction of double-balloon endoscopy and capsule endoscopy, the detailed pathology is becoming clearer.
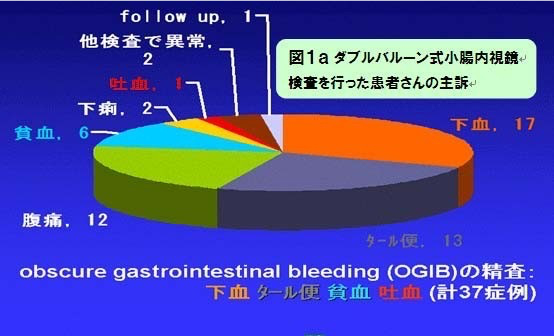
The slide shows the chief complaint (Fig. 1a) and the disease diagnosed as a result of the examination (Fig. 1b) of a patient who underwent double-balloon small bowel endoscopy at our hospital. As a result of the spread of small intestinal endoscopy, it has become clear that there are more small bowel diseases than previously thought.
Unexplained Gastrointestinal Bleeding: OGIB and Capsule Endoscopy
It may be an unfamiliar term, but Obscure Gastrointestinal Bleeding (OGIB) refers to bleeding from the gastrointestinal tract due to blood in the stool, melena, anemia of unknown cause, etc. It refers to a pathological condition in which a lesion that causes bleeding cannot be found even with conventional upper and lower gastrointestinal endoscopy. In such a condition, the cause is unknown and the patient is followed up, so anemia progresses due to repeated bleeding, and the patient's life is greatly restricted due to repeated hospitalization and discharge. Occasionally, excessive bleeding can lead to shock, which can be life-threatening. With the spread of small bowel endoscopy, it has become clear that OGIB includes cases of bleeding from small bowel lesions. For the diagnosis of OGIB, it is known that the shorter the time from bleeding to examination, the higher the diagnostic rate. Capsule endoscopy can also be used for emergency outpatient examinations, so it has the advantage of being able to respond relatively quickly to cases of sudden bleeding (Fig. 5).
On top of that, we continue to perform double-balloon enteroscopy for therapeutic indications such as hemostasis (Fig. 6).
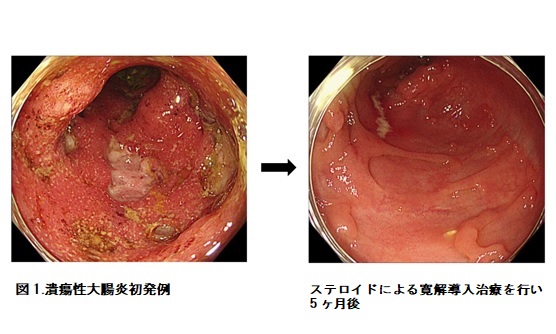
Inflammatory bowel disease mainly refers to ulcerative colitis and Crohn's disease, and the number of patients is increasing significantly in Japan. Although it is an intractable disease with repeated relapses and remissions, new therapeutic agents have been approved one after another in recent years, and treatment options are increasing.
Ulcerative colitis and Crohn's disease are diseases in which erosions and ulcers occur frequently in the gastrointestinal tract, and many factors such as genetic predisposition, environmental factors, and intestinal bacteria are involved to cause immune abnormalities. It is a chronic disease that repeats relapses and remissions, and it is important to continue treatment steadily.
In the past, it was common to develop it in the teens to 30s, but in recent years it is not uncommon to develop it at an older age. As of June 2021, there are 309 patients with ulcerative colitis and 142 patients with Crohn's disease who regularly visit our clinic.
Symptoms include diarrhea lasting for several weeks to several months, bloody stools, abdominal pain, fever, and weight loss. Crohn's disease in particular may be accompanied by anal lesions such as anal fistula and perianal abscess. It is also known that ulcerative colitis increases the risk of developing colorectal cancer after a long period of time.
If these symptoms persist, lower gastrointestinal endoscopy and small bowel endoscopy are performed for diagnosis.
In addition to conventional drug treatments such as 5-aminosalicylic acid preparations, steroids, immunomodulators (azathioprine, tacrolimus), anti-TNF-α antibodies, and granulocyte removal therapy, since 2017 JAK inhibitors, anti-α4β7 Drugs with different mechanisms of action, such as integrin antibodies and anti-IL-12/23p40 antibodies, have been approved one after another, and even severe cases can now be controlled by medical treatment in a considerable number of cases.
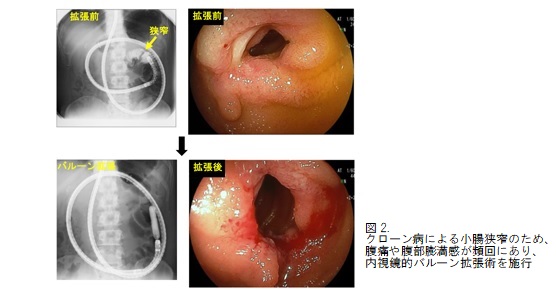
In addition, some patients with Crohn's disease require multiple surgeries due to complications such as intestinal strictures and fistulas. The most common cause of surgery is intestinal stenosis, and in order to avoid surgery as much as possible, at our hospital, after performing sufficient medical treatment, we actively perform endoscopic balloon surgery using double-balloon endoscopy. I am doing dilation. In patients with Crohn's disease who have symptoms of stenosis such as abdominal pain and bloating, we performed endoscopic balloon dilatation for intestinal stenosis at our hospital, and as a result, surgery was avoided in 52.4% of cases.
Inflammatory bowel disease is a disease that can lead to the need for emergency surgery if the diagnosis is delayed. If you have persistent diarrhea or bloody stools, do not hesitate to get tested.
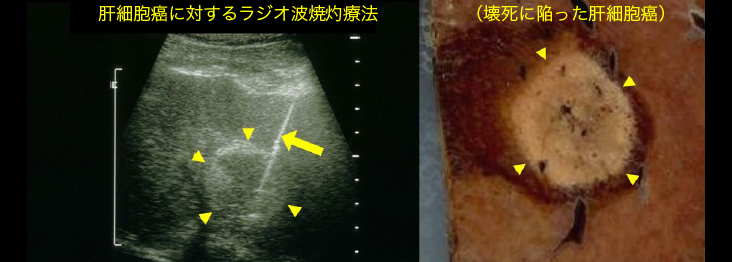
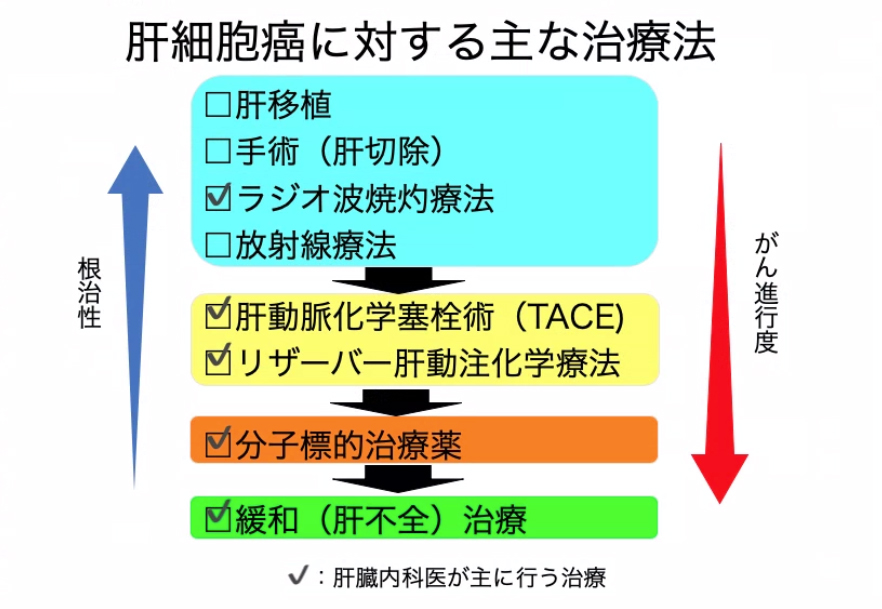
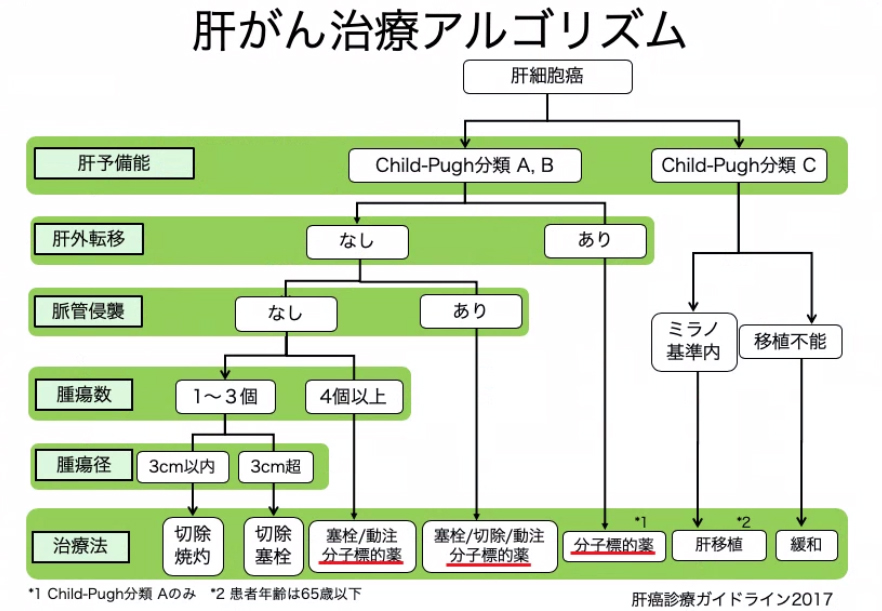
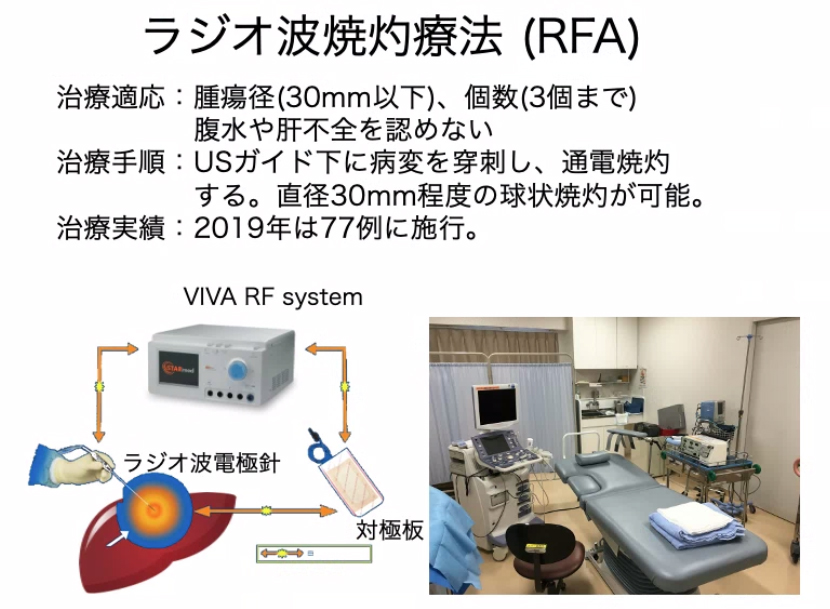
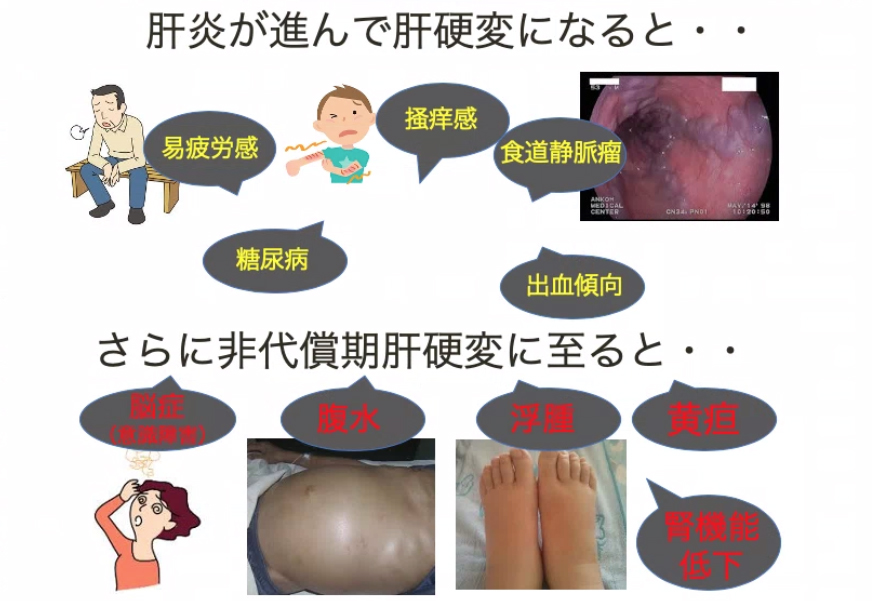
Liver cancer is the fifth leading cause of cancer deaths in Japan. It used to rank fourth, but due to advances in treatment for viral hepatitis, it has been declining since peaking around 2000. However, nearly 30,000 patients still die from liver cancer each year. In our department, we have been providing multidisciplinary treatment according to the progress of the disease based on the "Clinical Guidelines and Treatment Algorithms for Liver Cancer". As a medical treatment, radiofrequency ablation (RFA) is performed in 77 cases (2019) per year.
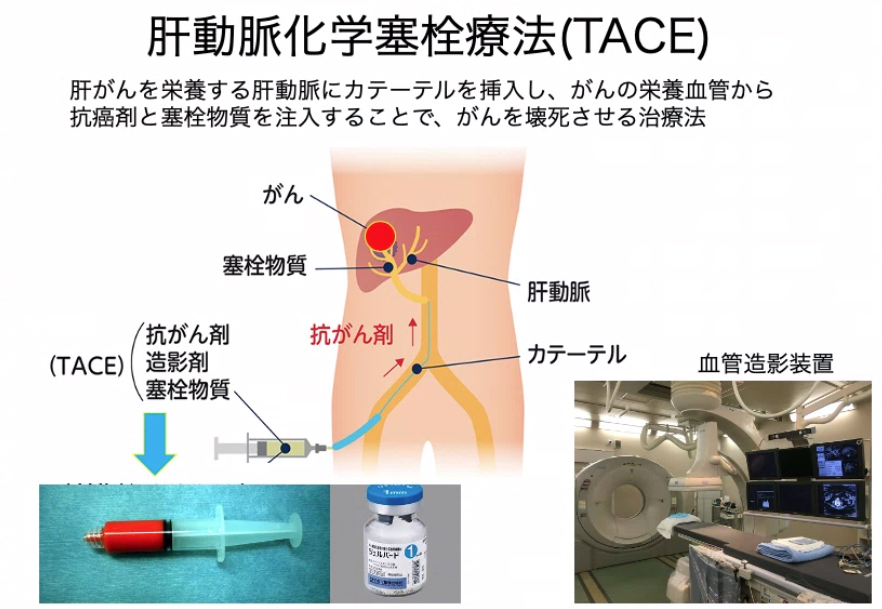
In more advanced cases, transarterial chemoembolization (TACE) is selected. TACE is a catheter treatment (IVR) developed in Japan, and we have a track record of 157 cases (2019) per year at our hospital. In addition to Conventional TACE, which uses Gelpart® as an embolic material, we also perform DEB-TACE, which uses drug-eluting spherical embolic material.
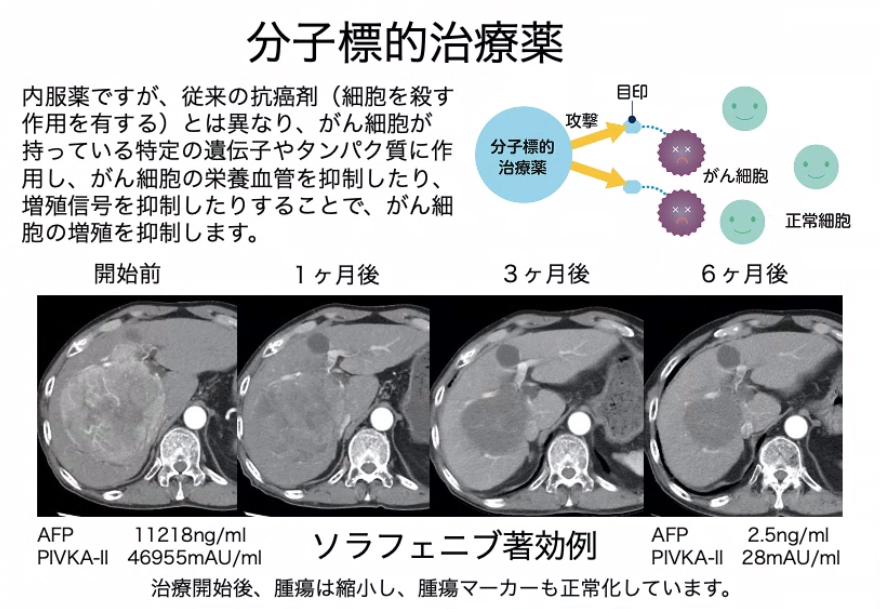
Molecularly targeted drugs developed in recent years are oral drugs that have the effect of suppressing the growth of liver cancer over the long term. Currently, sorafenib, regorafenib, and lenvatinib are available, and are being actively introduced in patients with good hepatic reserve for unresectable advanced liver cancer.
Radiation therapy is also extremely effective as a local treatment for liver cancer, and since the burden on the patient is small, in cooperation with the Radiation Oncology, moving body tracking stereotactic radiation therapy (combined with percutaneous metal marker: VISICOIL® placement) was performed. I'm here.
If it is determined that resection is indicated, we will consult with a surgeon and recommend resection after evaluating the liver reserve function. In our hospital, we also actively perform laparoscopic liver resection.
Regarding liver cancer, it is important for each clinical department to cooperate in treatment in this way, and our hospital holds conferences every week to discuss the optimal treatment policy for each individual patient. In 2019, we treated a total of 251 liver cancer patients at our department.
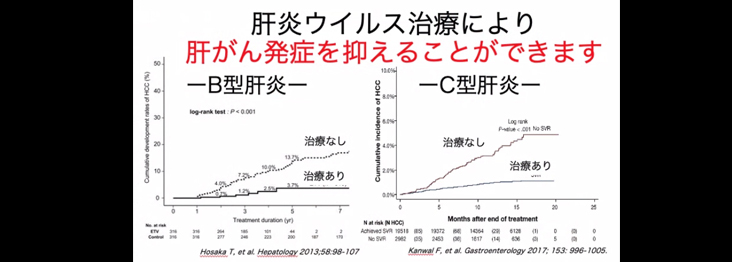
Since the days of interferon (IFN) in the 1990s, our department has actively treated hepatitis C, which accounts for 60-70% of the causes of liver cancer. However, interferon injection has strong side effects such as fever and malaise, and the therapeutic effect was not sufficient, so less than half of the patients were cured. However, in the 2010s, direct-acting oral antiviral drugs (DAAs) were developed, and now it is possible to eliminate the virus in more than 95% of patients with almost no side effects just by continuing oral medicine for several weeks. I'm here.
However, since hepatitis C itself does not cause subjective symptoms, many potential patients do not know that they are infected with the hepatitis C virus. If you have ever had a blood transfusion or surgery, we recommend that you get a hepatitis virus screening in your community or consult your family doctor. As a medical institution specializing in liver disease, our hospital also strives to proactively treat hepatitis.
Hepatitis B also accounts for about 10 to 15% of liver cancer patients, and it is said that there are 1.1 to 1.3 million Japanese people infected with hepatitis B virus (including carriers). In addition, 400 million people are infected worldwide, and it is said that 2 billion people are infected including those who have already been infected. In the past, mother-to-child transmission was common, but a project to prevent mother-to-child transmission was started in 1986, and now the carrier rate is low. However, in recent years, the number of patients who contract hepatitis B through sexual intercourse is increasing, and countermeasures are necessary.
Therapeutic drugs for hepatitis B have also made remarkable progress, and in 2000 an oral drug (nucleic acid analogue) that inhibits the growth of the hepatitis B virus was released, and now it is possible to suppress the growth of the virus and improve hepatitis. increase. However, if the oral administration is stopped, the virus will re-proliferate, and this treatment cannot eliminate the virus from the body.
In addition, people who have acquired antibodies after being infected with HB (HB-infected people) may develop hepatitis B after contracting cancer, weakening their immune system, or using drugs that suppress their immune system (such as anticancer drugs). It is a problem that it reactivates and becomes a serious condition.
If a patient who visits our hospital tests positive for hepatitis B or C, we have introduced a "hepatitis check system" on the electronic medical record so that we can contact the patient and conduct a detailed examination and treatment. operating.

The number of patients dying from cancer is on the rise as the population ages. It is said that one in two Japanese will get cancer, and one in three will die of cancer. Among gastrointestinal cancers, colorectal cancer ranks first and gastric cancer ranks second, with approximately 50,000 deaths each year. However, if cancer is detected early, it is a curable disease. Our department also actively performs endoscopic treatment for esophageal cancer, stomach cancer, and colon cancer.
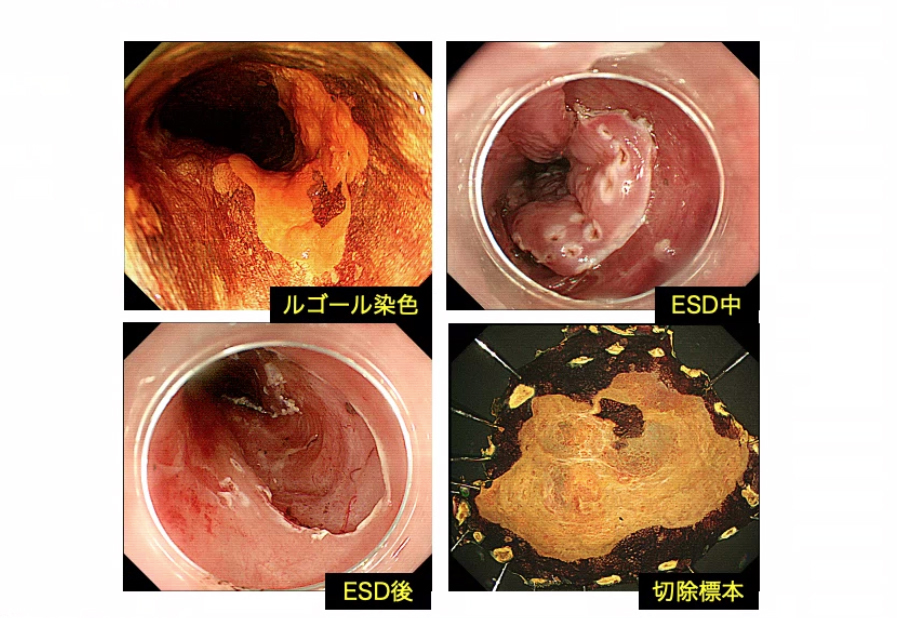
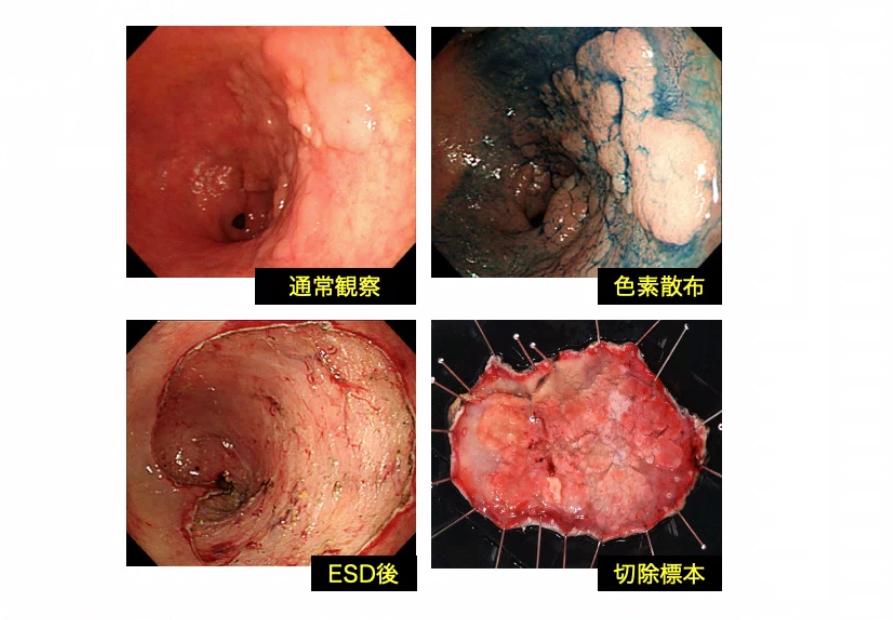
Specifically, we introduce endoscopic submucosal dissection (ESD) and treat more than 200 patients annually. ESD is capable of en bloc resection of relatively large early cancers, but it requires advanced endoscopic manipulation techniques. In our department, three endoscopists play a central role, and we perform the procedure safely under the whole-body and respiratory management by the ecological information monitor. In particular, if necessary, we have established a system that allows us to perform endoscopic resection using an operating room under general anesthesia.
Endoscopic treatment of superficial esophageal cancer
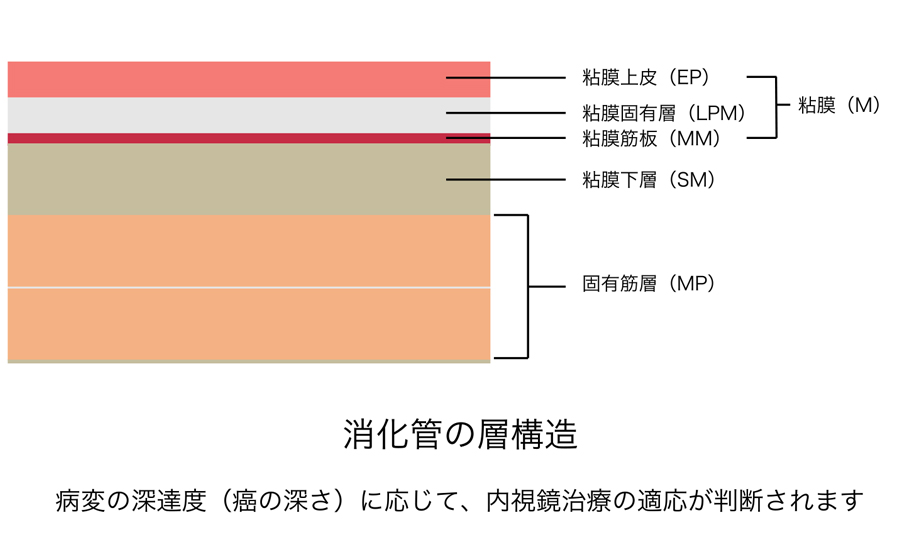
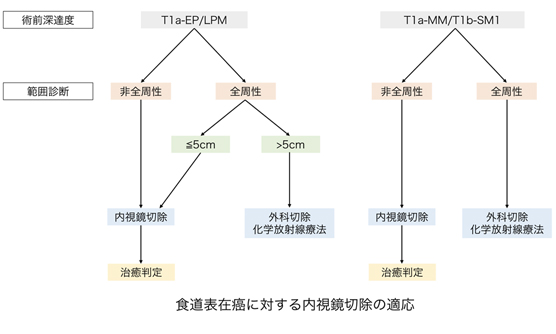
In esophageal cancer, lesions confined to the epithelium (EP)/lamina propria (LPM) have almost no possibility of lymph node metastasis, and endoscopic treatment is said to be curative. .
Cancer that is deep in the muscularis mucosae (MM) and that slightly invades the submucosa (SM1: less than 200 μm in the submucosa) can be treated endoscopically, but the possibility of lymph node metastasis is about 10-20%. It is said that there is However, considering the invasiveness of other treatments, the ESD/EMR Guidelines for Esophageal Cancer recommend endoscopic treatment as the first treatment.
Prevention of stenosis after endoscopic treatment
When the resection area is wide, post-resection stenosis becomes a problem, especially for circumferential lesions. Stenosis is inevitable if stricture prevention measures are not taken, and quality of life is significantly reduced due to obstruction. When stenosis occurs, the narrowed part is dilated under an endoscope, but the improvement may be poor and the treatment may be difficult.
In recent years, it has become possible to prevent stenosis to some extent by administering local steroid injections to the ulcer site immediately after endoscopic treatment or taking steroids internally. Nevertheless, the risk of stenosis is high in lesions that are circumferential and have a wide resected area. For lesions with a major diameter of 50 mm or less, endoscopic treatment combined with stenosis prevention is recommended, and for lesions larger than 50 mm, surgery or chemoradiotherapy is recommended from the beginning.
Endoscopic treatment of early gastric cancer
Endoscopic treatment for early gastric cancer preserves the stomach, resulting in a better quality of life than surgery. However, since endoscopic treatment for early gastric cancer is a local treatment, lesions that do not metastasize to lymph nodes around the stomach are targeted. Lesions for which the risk of lymph node metastasis is estimated to be extremely low (less than 1%) and long-term prognosis equivalent to that of surgical gastrectomy are called absolute indication lesions. Currently, the results of multicenter prospective clinical studies by the Japanese Clinical Oncology Research Group, JCOG0607 and JCOG1009/1010, have clarified the long-term results of endoscopic treatment for early gastric cancer. ”, lesions that meet the following conditions are considered absolute indication lesions.
- Nonulcerative, differentiated, intramucosal carcinoma of any size (M)
- ≤3 cm, ulcerated, differentiated, intramucosal carcinoma (M)
- ≤2 cm, non-ulcerated, undifferentiated, intramucosal carcinoma (M)
For early gastric cancer other than the above, the standard treatment is surgical gastrectomy. However, although the cure rate decreases, endoscopic treatment may be completely curable, so endoscopic treatment may be performed as a relative indication depending on the patient's situation (such as surgical gastrectomy being difficult).
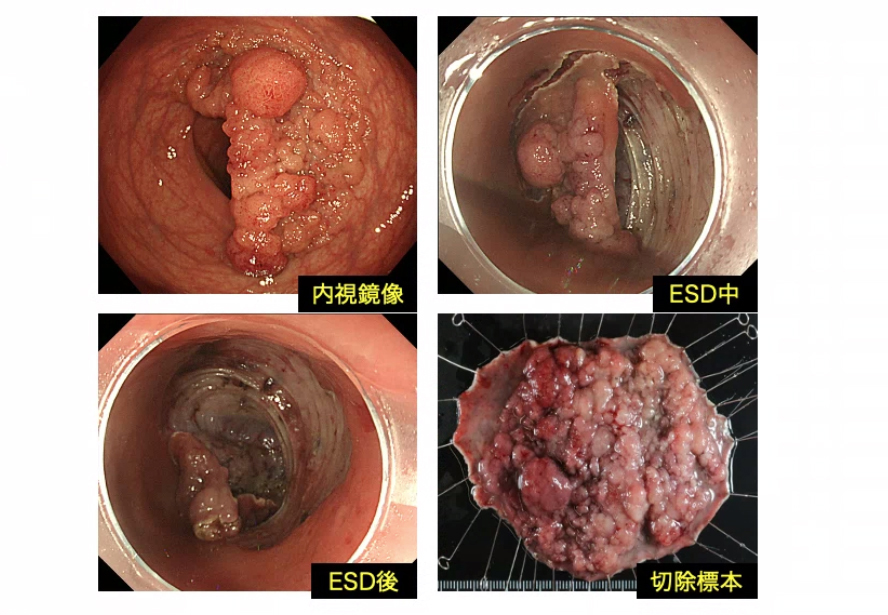
Endoscopic treatment of early colorectal cancer
Many colon polyps are treated with snares, but some early colon cancers (intramucosal carcinoma [M], mild invasion into the submucosa [SM1: submucosa less than 1000 μm]) On the other hand, it is difficult to treat with snare, and en bloc excision is performed by ESD.
Lesions that meet the following conditions are indicated for ESD.
- Larger than 2 cm, en bloc excision with snare is difficult
- Lesions with fibrosis in the submucosa
- Lesions with chronic inflammation such as ulcerative colitis
- Local residual disease after previous endoscopic treatment
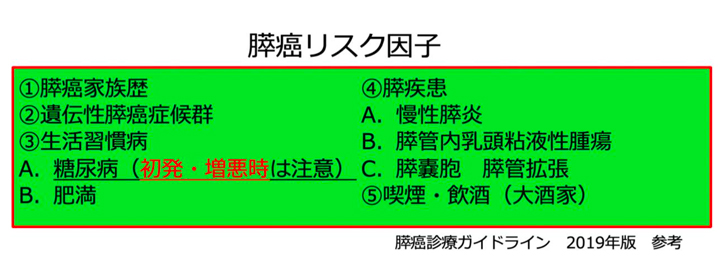
In recent years, pancreatic cancer has been on the rise, and about 37,000 people die of pancreatic cancer every year. Looking at changes in the cancer mortality rate for each organ, gastric cancer, colorectal cancer, and liver cancer are decreasing due to advances in medical care, but no signs of pancreatic cancer are observed.
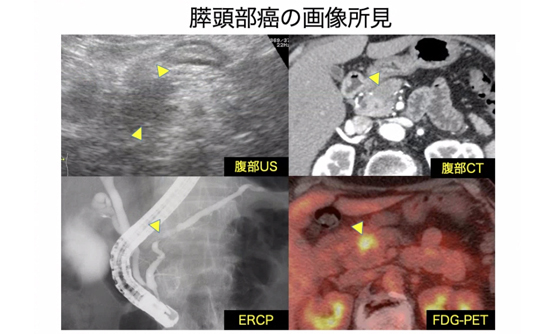
Pancreatic cancer is a disease with a poor prognosis, with a 5-year survival rate of less than 10%. However, pancreatic cancer of 1 cm or less in size is said to have a 5-year survival rate of 80%. In general, early detection of pancreatic cancer is difficult, but we believe that early detection is possible by conducting appropriate tests at appropriate times for high-risk patients with pancreatic cancer. For this reason, we are actively testing high-risk pancreatic cancer patients who are referred by local medical institutions. Even if there are no abnormalities at the time of referral, we believe that it is important to conduct regular examinations.
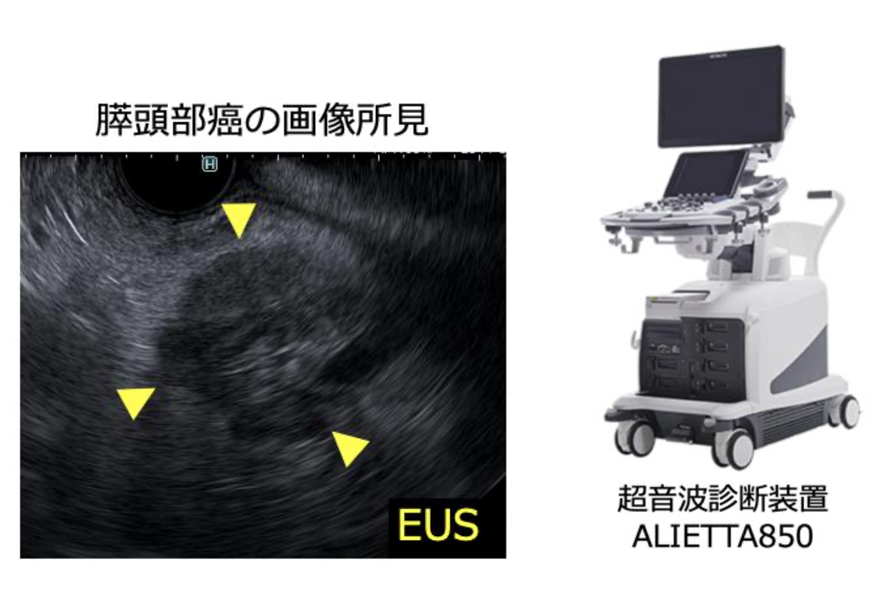
Imaging tests for pancreatic cancer include abdominal ultrasonography, CT, MRI, and endoscopic ultrasonography (EUS). EUS is an imaging test that uses an ultrasound probe at the tip of the endoscope to examine surrounding organs such as the pancreas and bile ducts through the walls of the gastrointestinal tract, such as the stomach and duodenum. Since EUS has excellent spatial resolution, it is possible to detect minute pancreatic cancers of 1 cm or less in size. Therefore, in our hospital, we actively perform EUS for pancreatic cancer high-risk patients. Recently, we have newly introduced the latest ultrasound diagnostic equipment, and we are accumulating daily examinations for the early detection of pancreatic cancer.
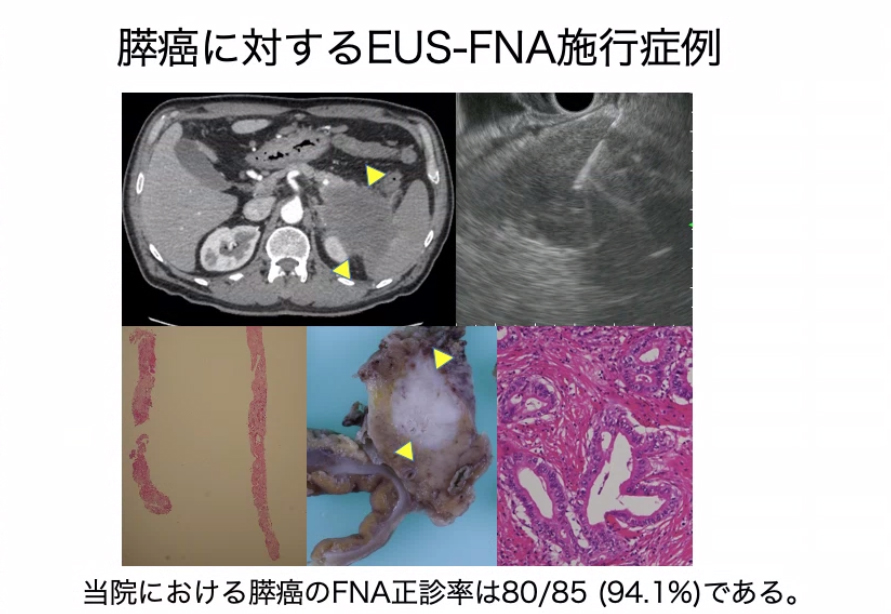
If EUS is used, a thin needle can be inserted into the pancreatic tumor from the stomach or duodenum and tumor cells can be collected. This method is called endoscopic ultrasound-guided fine needle aspiration (EUS-FNA). Collecting tissues and making a definitive diagnosis using EUS-FNA is extremely useful in deciding on a treatment policy for tumors.
Regarding the final decision on the treatment policy for pancreatic cancer, we hold conferences with the Department of Gastroenterology, Surgery, Diagnostic Radiology, and Oncology to select the optimal treatment method. In recent years, treatment methods for pancreatic cancer have also advanced, and efforts are being made to improve the patient's prognosis and quality of life.

What is the Digestive Disease Class
Liver diseases such as chronic hepatitis, liver cirrhosis, and liver cancer have been said to be "national diseases" among many Japanese people. In particular, hepatitis C was once called non-A, non-B hepatitis (hepatitis that is neither A nor B), but since HCV antibody was measured in 1989, chronic hepatitis・It has become clear that 60-70% of liver cancers are caused by hepatitis C, and that there are 1.5 to 2 million hepatitis C virus carriers in Japan. Therefore, in 2007, we started the "Liver Disease Class" so that patients with chronic liver disease and their families can receive effective treatment with accurate knowledge of the disease. Among them, interferon (IFN) treatment can cure hepatitis C, there are effective medical and surgical treatments such as TACE/RFA for liver cancer, drugs and nutrition related to liver disease, etc. has become established as a place where patients and medical staff such as doctor, pharmacists, and nutritionists study together.
However, since there are many types of gastrointestinal diseases other than liver disease, such as gastrointestinal diseases and pancreatic diseases, we developed the "Digestive Diseases Classroom" to expand the theme to the whole digestive system. It is held once a year, six times a year. Every time, 40 to 60 people participate, and it is held in a friendly atmosphere.
Contents of the Digestive Disease Class
The theme of the classroom is determined by the annual plan. First, the doctor will give a lecture on the pathology, and then the pharmacist will gently explain the topic of medicine, and the nutritionist will gently explain the topic of diet. After the lectures, there is a corner where we answer questions from participants, and we take various questions each time. Each specialist staff member carefully answers questions such as questions about illness, questions about treatment, questions that are difficult for the doctor in charge to ask, questions about medicines, questions about dietary contents, etc. so that the participants can answer their questions. Even if you are not a patient of our hospital, or if you are a family member, you are free to participate, so we would like you to feel free to participate.
The venue is the conference room on the first floor of the hospital. It is in front of a convenience store that is open 24 hours a day. There is no cost and no pre-registration is required.
Gastroenterology classroom pageclinical research
About clinical research
Our department conducts observational clinical research using existing clinical information. Observational clinical research is conducted without direct consent, but with consent given through this notice. I would like to ask for your understanding of the purpose of this research and for your cooperation in this research.
If you have any inquiries, please contact us at the following.
contact address
神戸市立医療センター中央市民病院 消化器内科部長 猪熊 哲朗
神戸市中央区港島南町2丁目1-1
TEL 078-302-4321(大代表)
clinical research
| Research subject name | Person in charge of our hospital | approval date | Explanatory text (PDF) |
| Safety and efficacy of GCD therapy for unresectable advanced biliary tract cancer | Shinsuke Akiyama | 2024/3/29 | |
|---|---|---|---|
| Optimal preoperative biliary drainage for resectable pancreatic cancer | Shinsuke Akiyama | 2024/3/29 | |
| Elucidation of clinical outcomes and related factors in patients with acute lower gastrointestinal bleeding: A multicenter retrospective study | Yohei Yabuuchi | 2024/2/7 | |
| Multi-institutional collaborative retrospective study on risk factors for lymph node metastasis in fundic gland type gastric cancer | Yohei Yabuuchi | 2024/2/6 | |
| A multi-institutional retrospective observational study on the external validity of the eCura System | Yohei Yabuuchi | 2023/12/8 | |
| A multicenter retrospective study on the therapeutic results of gel-soaked endoscopic mucosal resection for gastric tumors. | Yohei Yabuuchi | 2023/11/14 | |
| Current status of treatment for pancreatic neuroendocrine tumors in our hospital | Masaya Wada | 2023/5/2 | |
| Usefulness of one-stage percutaneous transhepatic SEMS placement for malignant bile duct stricture when transpapillary approach is difficult | Shinsuke Akiyama | 2023/9/12 | |
| Nationwide Survey of Complications of Endoscopic Esophageal Resection | Shuko Morita | 2023/8/7 | |
| Treatment results and future prospects of colorectal stents | Yoshiki Morihisa | 2023/7/24 | |
| Current status and issues of transpapillary biliary drainage for distal biliary stricture due to pancreatic cancer | Shinsuke Akiyama | 2023/4/27 | |
| Study of perioperative treatment including preoperative chemotherapy for resectable pancreatic cancer | Shinsuke Akiyama | 2023/4/18 | |
| A prospective nationwide study of needle tract seeding after endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS FNA) for pancreatic tumors. | Masaya Wada | 2023/2/14 | |
| A multicenter retrospective observational study on the safety and validity of gastric ESD in the very elderly aged 85 years and older | Yohei Yabuuchi | 2024/1/4 | |
| Observational research on drug treatment system and prognosis for patients with advanced or recurrent esophageal cancer ~Analysis of real world and clinical practice in Japan~ |
Shuko Morita | 2022/12/26 | |
| Diseases related to gastrointestinal endoscopy, construction of therapeutic procedure database | Tetsuro Inokuma | 2022/11/17 | |
| Observational research on drug treatment system and prognosis for patients with advanced or recurrent esophageal cancer ~Analysis of real world and clinical practice in Japan~ |
Shuko Morita | 2022/8/24 | |
| Fact-finding survey of pancreatic acinar cell carcinoma -multicenter joint research- | Masaya Wada | 2022/5/20 | |
| Current status of endoscopy cases in COVID-19 positive hospitalized patients | Noriaki Ando | 2022/4/4 | |
| Verification study of gastric lesion detection performance of endoscopic diagnosis support program | Youhei Yabuuchi | 2021/12/21 | – |
| Study on needle tract seeding and prognosis associated with EUS-FNAB before pancreatic body and tail cancer surgery | Shinsuke Akiyama | 2021/11/17 | |
| Endoscopic biliary drainage treatment strategy for malignant biliary stricture before pancreatic cancer surgery | Shinsuke Akiyama | 2021/11/17 | |
| Current Status of Gastrointestinal Bleeding in COVID-19 Positive Patients | Noriaki Ando | 2021/10/5 | |
| Study of preoperative biliary drainage for distal bile duct stricture due to pancreatic cancer | Shinsuke Akiyama | 2021/8/20 | |
| Current status and issues of EMR and UEMR for superficial non-papillary duodenal epithelial tumors | Shinsuke Akiyama | 2021/2/2 | |
| Usefulness of combined laparoscopic-endoscopic surgery for gastric submucosal tumor | Shinsuke Akiyama | 2021/1/19 | |
| Prophylactic suturing of mucosal defects after ESD in patients with high risk of post-hemorrhage | Soichiro Nagao | 2020/8/26 | |
| An open-label, randomized controlled trial of direct oral anticoagulant (DOAC) washout period in the perioperative period for colorectal polypectomy | Shuko Morita | 2020/6/27 | |
| National Survey of Complications Associated with Gastrointestinal Endoscopy | Tetsuro Inokuma | 2020/4/7 | |
| Current status of oral resection for superficial or hypopharyngeal cancer in our hospital | Naoto Urano | 2020/1/10 | |
| Diseases related to gastrointestinal endoscopy, construction of therapeutic procedure database | Tetsuro Inokuma | 2019/12/3 | |
| Treatment strategy for advanced hepatocellular carcinoma with molecular targeted drugs based on the therapeutic effect of sorafenib | Hiroshi Tei | 2019/7/30 | |
| Endoscopic diagnosis of invasion depth in superficial pharyngeal tumors | Shuko Morita | 2019/5/15 | |
| Clinical course of wall invasion T4b cases | Shuko Morita | 2019/5/15 | |
| A multicenter, randomized, controlled study comparing 22G normal needles and 22G Francine-shaped needles on the sampling rate of pancreatic mass lesions in endoscopic ultrasound-guided fine-needle aspiration biopsy. | Youhei Taniguchi | 2018/3/13 | ー |
| A non-randomized, confirmatory study on the efficacy and safety of cold snare polypectomy for duodenal non-papillary epithelial tumors of 10 mm or less | Tetsuro Inokuma | 2018/2/20 | ー |
| Efforts of our hospital for hepatitis C virus (HCV) antibody-positive cases | under the cedar Yoshiki |
2018/1/20 | |
| Examination of clinical epidemiological factors that predict the development of hepatocellular carcinoma after elimination of hepatitis C virus | Tetsuro Inokuma | 2017/10/5 | |
| Examination of safety and usefulness of Cricoid pressure in upper gastrointestinal endoscopy | Tetsuro Inokuma | 2017/7/20 | |
| Randomized controlled trial demonstrating the effect of eradication of Helicobacter pylori on suppressing metachronous gastric cancer in patients with early gastric cancer after ESD curative resection | Tetsuro Inokuma | 2017/7/11 | ー |
| Examination of the prognosis in patients aged 80 years or older who underwent endoscopic submucosal dissection for early gastric cancer | Shuko Morita | 2017/5/1 | |
| A case study of unexplained gastrointestinal hemorrhage and small intestinal hemorrhage with rebleeding | Masashi Fukushima | 2017/2/16 | |
| A case study of emergency upper gastrointestinal endoscopy for upper gastrointestinal hemorrhagic lesions | Shuko Morita | 2016/10/25 | |
| Examination of esophageal cancer cases that are difficult to pick up | Shuko Morita | 2016/9/1 | |
| A retrospective study on the safety of eradication of Helicobacter pylori in patients with inflammatory bowel disease (SPIRAL study) |
Hiroki Kitamoto | 2016/4/19 | |
| Comprehensive analysis of genetic abnormalities in solid tumors | Tetsuro Inokuma | 2015/8/1 | |
| A multicenter retrospective observational study on prognosis and its factors in patients with ulcerative colitis who underwent leukapheresis (LCAP) | Satoko Inoue | 2015/7/1 |
news
Introduction of our department for doctor and those who aspire to become doctor
October 18, 2021
*This content is intended for doctor and is intended to deepen the understanding of this medical institution, and is not intended for publicity or advertising for the general public.
Nice to meet you, my name is Tetsuro Tetsuro Inokuma Gastroenterology Kobe City Medical Center General Hospital.
As a main hospital in Kobe City, our department has 9 staff members and 7 Senior Resident for a total of 16 people, who are engaged in acute treatment of digestive diseases 24 hours a day. Last year, the number of hospitalized patients decreased to less than 2,000 due to the effects of the new coronavirus infection, but emergency hospitalizations accounted for 1/3 of the hospitalized patients.
The Endoscopy Center, which is located next to the Critical Care Center on the 1st floor, has 7 examination rooms and 2 X-ray fluoroscopy rooms in a space of over 800m2. We also have a recovery corner. Because it is possible to take a sufficient rest after the examination, almost all cases are currently undergoing endoscopic examinations under sedation (sedation), and approximately 18,000 examinations are performed per year. .
This time, Yohei Yabuuchi M.D. of our department, will introduce endoscopic treatment that makes full use of cutting-edge equipment and techniques.
Vice President
Gastroenterology Director
Tetsuro Inokuma
Nice to meet you, I am Yohei Yabuuchi Yabuuchi, M.D. of Gastroenterology Kobe City Medical Center General Hospital.
The field of gastrointestinal endoscopy is advancing day by day. In terms of diagnosis, real-time histological diagnosis is becoming possible, and in terms of treatment, less invasive treatment methods are being explored while ensuring curability.
In this article, I would like to explain the approach to endoscopic treatment at our hospital.
M.D. Gastroenterology
Yohei Yohei Yabuuchi
<Specialty field>
Endoscopic treatment of early cancer
<Academic specialist/ Certified Physician >
The Japanese Society of Internal Medicine Board Certified Member of the Japanese Society of Internal Medicine
The Japanese Society of Gastroenterology Gastroenterology Specialist and Supervisor
Japan Gastroenterological Endoscopy Society Board Certified Fellow of the Japan Gastroenterological Endoscopy Society
A new standard for endoscopy Providing safe and comfortable examinations
Endoscopy has traditionally been said to represent a painful examination.
In fact, some patients who underwent endoscopy in the past said, "I don't want to undergo such a painful examination again." However, after the introduction of sedation examinations using sedatives and analgesics at the time of examinations, almost no complaints of pain have disappeared. Some patients have no recollection of having undergone the test, so we believe that they will be able to undergo the test without anxiety.
On the other hand, the most common complications (including deaths) associated with endoscopy are also related to sedation.
For this reason, in our department, we continuously centrally manage and record patient information monitors during and after examinations, and alarms are set off when blood pressure or SpO2 drops, making it possible to respond quickly. We provide a comfortable inspection with a firm guarantee of safety.
Picking up early cancer using state-of-the-art equipment
Medical progress is remarkable, and new treatments and devices are being developed one after another in the gastrointestinal field.
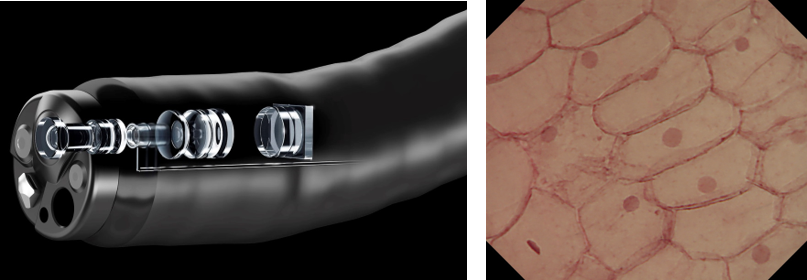
As part of our mission to provide state-of-the-art medical care, this year we have introduced the Endocyto® endoscope, which enables ultra-magnified observation up to 520 times. It is an epoch-making device that can obtain microscopic-level visual fields in vivo.
Conventional magnifying endoscopes are limited to 80x magnification, but ultra-magnifying observation not only improves the diagnosis rate of microscopic cancers, but also has the potential to make definitive diagnoses without removing tissues.
The scope itself has an outer diameter of 9.7 mm, which is smaller than a normal endoscope, and it is possible to continuously zoom from normal to 520 times magnification simply by operating the magnifying zoom lever.
Being able to observe cell nuclei may also enable tissue diagnosis by evaluating cell atypia. With the recent increase in the number of patients taking antithrombotic drugs, we believe that there is also the advantage of avoiding the risk of bleeding due to biopsy tissue examination.
Observation of nuclei in mucosal cells is possible with a super-magnifying endoscope
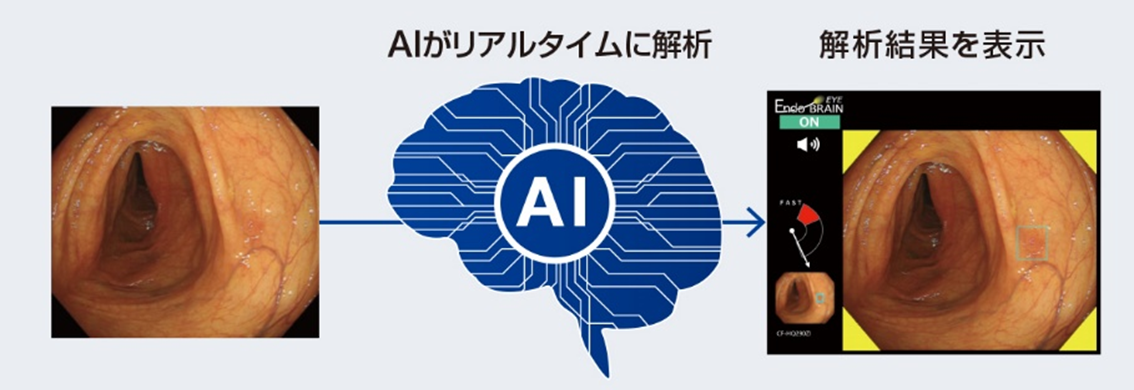
In addition, we plan to introduce “Endo BRAIN-EYEⓇ”, the first AI diagnosis support system for endoscopy, ahead of hospitals nationwide. We expect that the use of AI will enable the qualitative diagnosis of early cancers and the detection of minute tumors.
Endo BRAIN-EYE points out tumors in real time during examination
State-of-the-art therapeutic technique ESD is now possible for early-stage cancers in the entire gastrointestinal tract
With the development of endoscope equipment in recent years, many early cancers have come to be found in the gastrointestinal tract as a whole.
With the development and progress of endoscopic submucosal dissection (ESD), lesions that were previously indicated for surgery have become Entire resection is possible regardless of the size of the lesion, enabling good local control and accurate pathological evaluation It is. Endoscopic treatment has become the first choice for many early-stage cancers, since radical cure can be expected for lesions with an extremely low possibility of lymph node metastasis, although there are some differences in criteria depending on the organ. .
The greatest merit of endoscopic treatment is that the physical burden during treatment is minimal and organ function can be preserved. At our hospital, we basically operate on the path of hospitalization the day before treatment, treatment day, starting drinking water the day after treatment, and resuming eating two days after treatment.
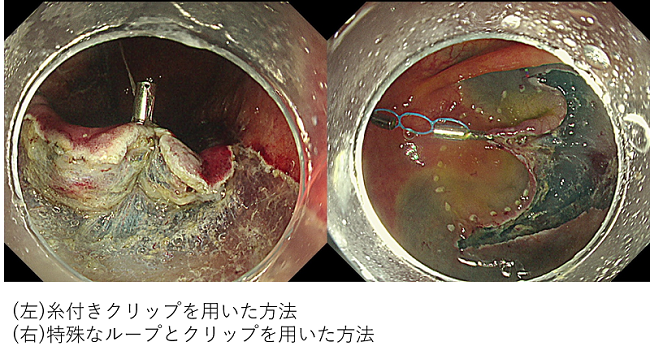
ESD is a technique that is becoming more popular, and standard lesions are widely treated, but it is also true that there are lesions that are technically difficult depending on the lesion site and size. In endoscopic treatment, only one device that can be pulled out from the scope is a weapon, but the bottleneck is that it is not possible to expand the field of view using multiple hands as in surgical operations. However, in recent years, in order to overcome this problem, it has become possible to apply countertraction by using a clip with thread or a method using a special loop.
Countertraction method
In addition, at our hospital, there are three specialists who have sufficiently studied at a high-volume center for endoscopic treatment in Japan, and we hope for treatment after sufficient discussion and treatment strategy in advance.
Recently, due to the aging society, there are some patients who do not wish to undergo surgery due to the risk of postoperative QOL deterioration, even if they are judged to have early-stage cancer that is suitable for surgery. In such cases, if the patient agrees that curability is inferior to surgery, a policy of performing only endoscopic resection and monitoring the progress is presented as an option (ESD as a relative indication). ).
If you think there is even the slightest possibility of endoscopic treatment, please do not hesitate to introduce us.
Cooperate with other departments in the hospital to provide care from the entrance to the exit of the gastrointestinal tract
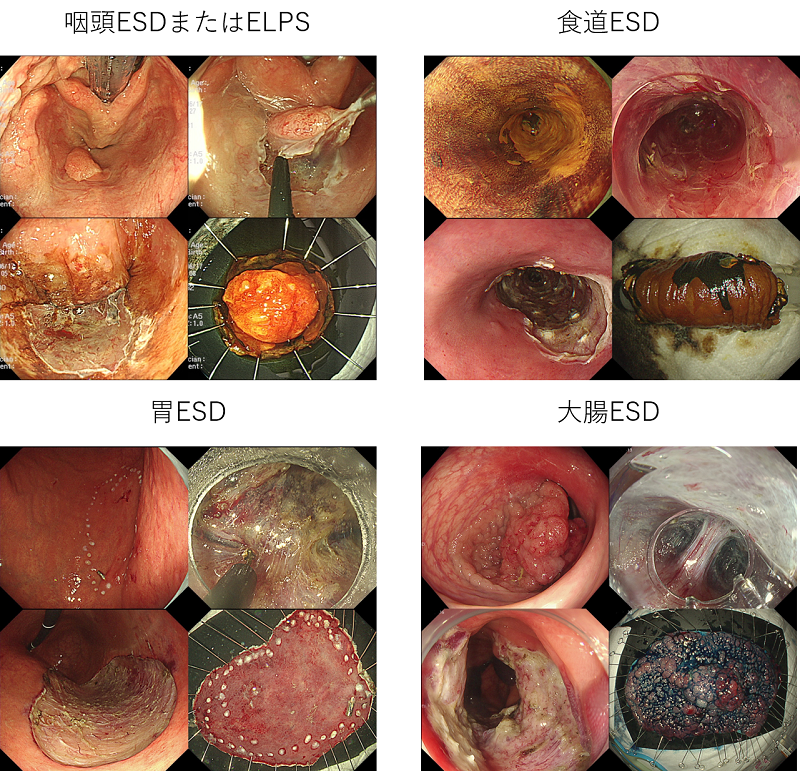
At our hospital, we perform endoscopic treatment for superficial cancer of the entire gastrointestinal tract from the entrance to the exit, including the pharynx, esophagus, stomach, duodenum, and large intestine.
For pharyngeal lesions, joint treatment with an otolaryngologist is performed, laryngeal expansion using a curved laryngoscope, ESD techniques, orally inserting forceps or electric scalpel under the assistance of an endoscope. We perform resection by ELPS (Endoscopic Laryngo-Pharyngeal Surgery), which performs subepithelial detachment.
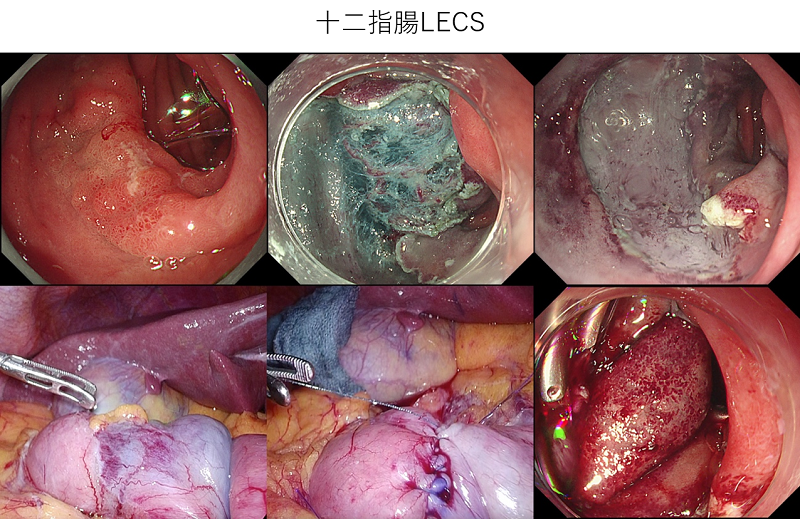
Regarding lesions of the duodenum, it is said that the risk of intraoperative and delayed perforation associated with ESD is high due to poor operability and exposure to digestive juices such as bile and pancreatic juice. To ensure safety, we also provide treatment by LECS (Laparoscopy and Endoscopy Cooperative Surgery), which is performed jointly with surgical laparoscopy.
To reduce colorectal cancer mortality -colorectal cancer screening and clean colon-
Colorectal cancer is on the rise due to the westernization of diet (high-fat/low-fiber diet), increased obesity, lack of exercise, alcohol consumption, and smoking.
Colorectal cancer is ranked 2nd in men and 1st in women in the predicted number of cancer deaths by site (2020). Colorectal cancer ranks third among males and second among females in the predicted number of cancer incidences by site (2020). The mortality rate from colorectal cancer is higher in Japan than in Europe and the United States. It is believed that colon cancer screening, mainly using endoscopy, has been successful in reducing the number of colon cancer deaths in Europe and the United States.
Colorectal cancer is a curable disease if detected early.
Colorectal cancer screening (fecal occult blood test) and endoscopy are useful for early detection and early treatment.
Multiple RCTs have demonstrated the effect of fecal occult blood testing on colorectal cancer mortality. Multiple large-scale cohort studies have also shown the effect of endoscopy on reducing colorectal cancer mortality.
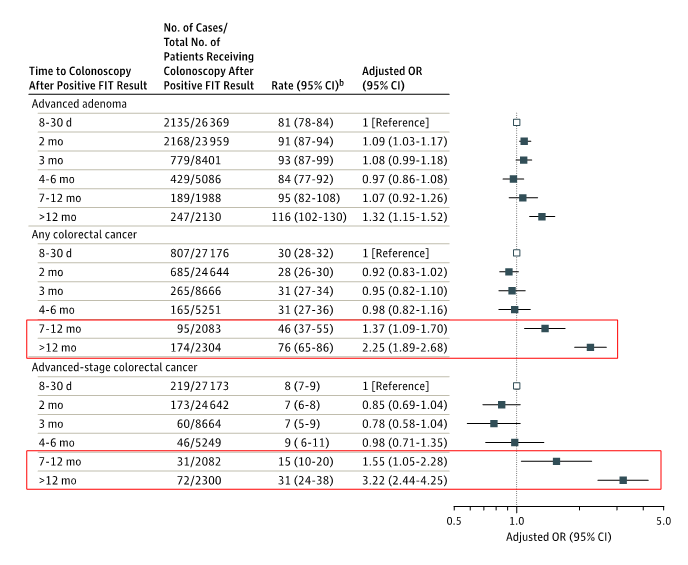
In Japan, low screening and detailed examination rates are issues. Recently, in the pandemic of the new coronavirus, refraining from seeing patients has become a problem. From overseas, it has been reported that the longer the period until the endoscopic examination of the fecal occult blood is positive, the more advanced the colorectal cancer is found, and the higher the risk of colorectal cancer death.
The longer the period between a positive fecal occult blood test and colonoscopy, the higher the rate of colorectal cancer (especially advanced cancer).
At our clinic, in parallel with corona countermeasures, we are striving to maintain the medical system so that we can provide normal medical care safely and securely under sufficient infection control measures. For example, prior to an endoscopy, based on the guidelines of the academic society, we conduct a preliminary risk assessment through medical interviews and temperature checks, and ensure that personal protective equipment is worn during the examination.
Neoplastic lesions can be treated on the same day

A scope with a magnifying function is used in all cases, enabling accurate pretreatment diagnosis and treatment selection based on magnified observation.
For low-grade adenomas of less than 10 mm, endoscopic resection without applying current, called cold snare polypectomy (CSP), is commonly performed. As the number of patients taking oral antithrombotic drugs increases as the population ages, safer minimally invasive treatment with a low bleeding risk is now possible. is.
message to teachers
Due to the spread of the new coronavirus infection since last year, I understand that many medical institutions are restricting medical treatment.
As a designated hospital for infectious diseases, our hospital also built a temporary corona ward in the hospital parking lot to accept severely ill patients in Hyogo Prefecture, and has treated more than 1000 patients so far. Reflecting on the in-hospital cluster that occurred at the beginning of the response, we have established a system to safely treat general patients by establishing the distinction between red (corona positive), orange (suspected corona), and white (general, corona negative). .
In addition, for emergency and scheduled hospitalization patients, PCR tests are performed on all cases before hospitalization to check for viruses brought in. Please feel free to introduce yourself.
Gastroenterology Senior Resident 's Plaza Let's Join Us!

A senior who has experienced three years as a Gastroenterology Senior Resident at our department (if you have also experienced two years as an Junior Resident-stage resident at our hospital, please include that period as well) and send a message to juniors who wish to become gastroenterologists.
Dr. T (2016-2030: Specialist in our Senior Resident) (Later worked at Teine Keijinkai Hospital)
Thank you for your interest in our Department of Gastroenterology.
I spent two years at Rakuwakai Otowa Hospital in Kyoto, which specializes in general and emergency care. After much deliberation over what to choose as a field of specialization and which hospital to choose as a career path, I found (1) a large number of cases, including emergency care, (2) a well-developed guidance system, and (3) an environment where I could maintain my motivation. I considered it as a condition and decided. Looking back after three years of training, I realize that it was the training destination that met my expectations the most.
Our hospital has been featured in the media, but we have been ranked number one in the national critical care center evaluation for 5 years in a row. Cases that are difficult to treat at other hospitals are often referred to us. In addition, since other specialties are also influential, it is possible to experience rare diseases such as "gastrointestinal lesions of systemic diseases". However, if there are only a large number of patients, you will not know whether the treatment you are doing is appropriate or optimal, and you will be overwhelmed by the number. At our hospital, senior physicians specialize in gastrointestinal tract, bile pancreas, liver, and inflammatory bowel disease (IBD). Technology can also be improved. Depending on the hospital, there are some tests and treatments that cannot be performed due to lack of specialists, equipment, or lack of experience, but at our hospital, you can practice and learn a wide variety of specialized tests and treatments evenly in all areas. is considered to be the greatest advantage. Based on the wide range of experience I have cultivated during my three years of training as a Senior Resident, I believe that I will be able to aim for greater heights as I pursue my studies in my specialized field.
In addition, clinical and academic activities are like the two wheels of the wheel, and I feel that each other's abilities will be enhanced by the well-balanced functioning of both. In addition to giving presentations at regional conferences, there are many opportunities to participate in international conferences and write papers in English. There are many interesting cases, and preceptors are also actively involved. There is also an academic support center in the hospital, and the environment is well-equipped. I think that this is a very good opportunity to stop, think deeply, and learn from the busy clinical environment, so I encourage you to give it a try.
Deciding which way to go is a very difficult thing, but there are some scenery that you can only see once you take a step forward. Taking the first step as a Gastroenterology at our hospital is a big advantage for me. First of all, please take a tour and see what kind of training and guidance our Senior Resident receive.
We hope that our training will be fruitful for all of you.
Dr. M (2011-2012: Junior Resident, 2013-2015: Specialist in our Senior Resident) (After that, worked at the National Cancer Center Hospital East)
I had two years of initial training at our hospital, and three years of late training at the Department of Gastroenterology. Now that I have completed the latter term training, I would like to introduce the characteristics of the training at our hospital's Gastroenterology.
The first feature I would like to mention is that we are able to provide well-balanced training in the field of Gastroenterology, which deals with a wide variety of diseases. Gastroenterology broadly divided into the gastrointestinal tract area and the hepato-biliary-pancreas area by organ. In addition to treating many organs, we also target various pathologies such as malignant tumors such as stomach cancer and colon cancer, and inflammatory diseases such as chronic hepatitis and inflammatory bowel disease. At our clinic, we are able to provide unbiased, high-level training under the guidance of experienced staff who are well-versed in each area. The number of cases is also very large, so it may be more correct to say that there is no choice but to eliminate bias (laughs). Not to mention upper and lower gastrointestinal endoscopy, which is synonymous with Gastroenterology, we can actively participate in treatments such as ESD, ERCP, TACE, and RFA. For example, I was able to experience more than 50 cases of ESD during the second term training alone. Gastroenterology need not only knowledge of internal medicine but also the ability to perform complex procedures, so I think it was ideal to have such an experience.
The second feature is that we have an extremely large number of emergency cases as Kobe City 's premier general hospital that handles up to tertiary emergencies. You can experience a wide range of pathologies that require endoscopic treatment, such as hematemesis and cholangitis, and pathologies that require medical management, such as severe acute pancreatitis and fulminant hepatitis. At first, I had to hold the endoscope in a cold sweat (laughs). I think it's done.
The third feature is that they are proactive about academic aspects such as academic conferences and paper presentations. For myself, I was able to step up gradually and experience presentations at academic conferences, from regional conferences to general meetings and even international conferences. It was sometimes difficult to do academic activities during my busy clinical work, but I was able to acquire a lot of knowledge through making presentations, and I felt a great sense of accomplishment after finishing my presentation with other professors. .
Above, I have described the characteristics of the latter term training at the Department of Gastroenterology at our hospital. To be honest, it was a busy life, but I think it's an environment where you can improve as much as you want. We are looking forward to seeing as many people as possible come to our clinic!
Dr. H (2011-2012: Junior Resident, 2013-2017: Specialist in our Senior Resident) (After that, worked at Shizuoka Cancer Center)
During my training as a Senior Resident in Gastroenterology at our hospital, I was in charge of a large number of gastrointestinal disease cases, and was able to be involved in tasks such as endoscopic examinations and treatments, as well as ward and outpatient care. I was given many opportunities to respond to emergencies, and I was able to directly experience many cases such as melena and acute abdomen. From the beginning of my first year, I often received multiple consultations at the same time as an ambulance duty, and I think I was often confused at first. However, even in such a case, I was not exhausted by myself, and while consulting with senior doctors and senior Senior Resident around me, I was able to receive appropriate advice and learn how to respond. By being entrusted with the initial Senior Resident immediately as a specialist, I can take responsibility for my medical care and improve my skills on a daily basis. In addition, by becoming the attending physician of an inpatient, it is possible to be involved responsibly in determining the treatment policy. I was also given many opportunities to experience therapeutic endoscopy. In a busy and demanding environment, I sometimes feel discouraged, but I am able to continue my training with the support of the doctor and co-medicals around me. Through inpatient, outpatient, and emergency departments, you can experience a series of common gastrointestinal diseases and sometimes relatively rare diseases in three years. Many patients have social problems, and social problem-solving skills are required.
In addition, the whole department of Gastroenterology has an atmosphere of enthusiasm for academic activities, and since there are many cases, it is possible to participate in a wide range of academic activities such as regional meetings, general meetings, paper writing, and international conferences. am. I believe that these three years will allow me to grow significantly as a doctor and as a human being.
Dr. K (2010-2011: Junior Resident, 2012-2014: Specialist of our Senior Resident, 2015-2016: Staff of our department) (After that, he entered Kyoto University Graduate School of Gastroenterology)
I had two years of initial training at our hospital, followed by three years of specialized doctor as a Senior Resident in Gastroenterology Gastroenterology
I will write about the characteristics of this hospital based on my experience in each period.
First of all, regarding the initial training, our hospital is one of the leading emergency medical centers in Japan, and we accept many emergency patients day and night, and we handle a wide range of emergency cases from primary to tertiary emergencies. Due to the high level of medical care in an environment blessed with facilities and personnel, not only emergency cases but also cases that are difficult to treat at other hospitals are widely accepted, and appropriate diagnosis and treatment are performed for acute to chronic conditions. medical treatment is possible. I believe that experiencing the first step as a doctor in such an environment with high medical standards was important in laying the foundation as a doctor. I had a relatively long rotation in all internal medicine as a course focused on internal medicine, but I was able to experience many cases from common diseases to rare diseases. The training was also helpful.
Next, in the period of specialization in Gastroenterology Senior Resident a specialized training, from the beginning of the training, I will treat the patients in charge as the attending physician, and will proactively perform everything from examinations and treatments to management for discharge from the hospital. As a general rule, the hospital does not refuse emergency cases, so bed management is sometimes tight, and it is required to proceed with examinations and treatments without waste. I was able to develop a sense of assessing the condition of the patient. Regarding actual medical treatment, Gastroenterology one of the departments of internal medicine that requires manual procedures. I didn't have to scramble for cases with the Senior Resident (rather, I can experience it as much as I hate it). With the support of a senior doctor, I am able to accurately perform emergency examinations for emergency cases, so I was able to realize that my abilities are improving day by day.
Many people are transferred to other hospitals when they finish their Senior Resident, but I was fortunate enough to be able to stay because of the number of M.D., so I worked at this hospital for two more years after completing my Senior Resident. bottom. I had experience in general Gastroenterology Senior Resident until I became a specialist, but during my term as a fixed-term doctor, I was able to take a step further into my own area of expertise and provide medical care. While experiencing a wide range of cases during my time as a Senior Resident, I became interested in the treatment of inflammatory bowel disease and small bowel disease, so I was able to devote the remaining two years to improving my small intestinal endoscopy skills. I was able to have a good experience in making the foundation of.
Our department also puts a lot of effort into academic research, and we have made many presentations at academic conferences both in Japan and overseas. At first, I didn't know how to make the presentation slides, but as I went through the number of sessions, I was able to grasp the tricks of abstract creation and presentation, and it was adopted as a theme at the general assembly level. I was able to write three papers while I was enrolled, and I think that this facility has endless possibilities if you are motivated.
After gaining experience at our hospital as described above, I am currently enrolled in graduate school at Kyoto University. After completing the basics of Gastroenterology through training at our hospital, there are many doctors who aim to further deepen their specialized fields. It seems that there are many things to study. Since it is also an affiliated hospital of Kyoto University, it is relatively flexible to transfer between affiliated hospitals, so those who want to gain more experience in general Gastroenterology will not get lost. Although it is a busy hospital, there are many things that can only be experienced here.
Dr. O (2009-2020: Junior Resident, 2011-2013: Specialist in our Senior Resident) (After that, after working at the Japanese Red Cross Wakayama Medical Center, entered the Graduate School of Gastroenterology, Kyoto University University)
After two years of initial training at our hospital, and three years of later training, I am currently conducting basic research at a university. Looking back at the training at our clinic, we will introduce the characteristics of the early and late training.
The feature of the initial training is "the best of both city hospitals and university hospitals."
Our hospital's emergency outpatient department handles primary to tertiary emergencies from children to adults, so we can examine many patients who visit us and develop the ability to respond to various medical conditions. On the other hand, at our hospital, under the guidance of many excellent instructors, medical care at the level of a university hospital is provided. You can learn and practice how to diagnose and treat. In other words, you can experience a wide variety of cases of various pathological conditions, and you can practice diagnosis and treatment at the university level under the guidance of many excellent instructors, which is the best of both city hospitals and university hospitals.
The characteristics of the latter term training are "abundant cases", "many colleagues" and "scientific research".
The greatest feature of our hospital is the abundance of cases. You can acquire a lot of knowledge and skills by experiencing various procedures through abundant cases. It is said that "seeing is believing", but I believe that nothing can replace the experience gained not only by learning and hearing, but also by seeing the case firsthand.
The second feature is that there are "many friends". There are many post-doctoral trainees in our clinic, so we can stimulate each other and work hard. In addition, by observing what senior trainees are doing, practicing and teaching juniors, in other words, by practicing “see one, do one, teach one”, learn, acquire, and establish knowledge and skills You can. Of course, it is safe because the staff who are familiar with each field will firmly support the late trainees. On the other hand, when the second term training begins, you will be in charge of patients as the attending physician, and the sense of responsibility as the attending physician will cause a lot of pressure and worries. At that time, I was very grateful to have friends who were in the same environment, shared my feelings, and encouraged each other. In addition, there is concern that the number of cases and procedures that can be experienced will decrease due to the large number of post-doctoral trainees, but please rest assured that there is no such concern.
Finally, I would like to mention "scientific research" as the third feature. It is important not only for oneself but also for the development of medical care to transmit to the world a wealth of cases and experiences of unique diseases. There are systems in place to support you. By using this system, we are in an environment where it is very easy to make presentations.
I was busy with daily medical care in the early and late stages, and it passed quickly, but looking back, I feel that those days were very fulfilling. When I was transferred to another hospital, I realized that the knowledge and experience I had accumulated so far was useful, and I think that the path I have taken so far was not wrong.
There are many other attractions of the training at our clinic, but I can't write them all, so I hope you will come and visit us. We hope that many of you will be interested in training at our school.
Dr. M (2008-2009: Junior Resident, 2010-2012: Specialist in our Senior Resident) (After that, he entered Kyoto University Gastroenterology Graduate School)
After two years of initial training at our hospital, I immediately started specialized training as a late-stage resident (Senior Resident) in Gastroenterology. The reason why I chose to stay at our hospital as a doctor in charge is that the appearance of the senior doctors in charge of performing various procedures as a consultant is very lively and fulfilling from the standpoint of a doctor in charge of the Junior Resident in the emergency outpatient department. It was because it seemed that I was sending a training that I had done. I would like to introduce some of the features of our hospital's Gastroenterology that I have personally experienced through my experience in the latter term training.
One is that, in our department, there is a culture in place in which late-stage trainees are the main players in providing medical care and treatment. For example, it is not a training style of "learning about senior doctors" like sailing on a large ship called a senior doctor on a calm sea, but a training where you become a boatman and manage to make progress while being caught in rough seas. Close to style. Of course, it is premised that I will receive various guidance from senior doctors on a daily basis, but the knowledge and skills I have acquired through my own struggles will be many times faster than just being taught. You can feel that it is about. Especially with regard to treatment, once a certain foundation has been established, an environment in which a senior doctor will watch over you and tell you to “try it first” is a very blessed environment for those who want to learn about the digestive system. It can be said.
The second point, which can be said to be a feature of our hospital as a whole, is that we are focusing on emergency care, and at the same time, we are a high volume Kobe City and a medical institution that provides advanced medical care. The point is that there are many ambulance transports and referral consultations, and you can experience a lot of cases. Even in the Department of Gastroenterology cases that require emergency treatment, such as hematemesis and cholangitis, are brought to us almost every day. I can. In fact, in the first year, I myself had more than 800 upper endoscopies and more than 300 lower endoscopies (about 10% of which were emergency endoscopies), and I was trained in Gastroenterology at a general hospital. I have been able to experience endoscopy equivalent to three years. In addition to treatment and emergencies, you can experience many rare diseases and serious conditions that you cannot easily experience at general facilities.
In addition, IVR treatment such as hepatic artery embolization therapy and radiofrequency ablation therapy for liver cancer is mainly performed by the Department of Gastroenterology It is possible to conduct intensive training in an environment. I am looking forward to working hard with as many friends as possible.
Dr. A (2002-2015: Junior Resident, 2004-2018: Specialist in our Senior Resident)
Impressions about the Senior Resident training
I think it's attractive to be able to take charge of a large number of gastrointestinal disease cases as the attending physician in the gastrointestinal Gastroenterology Senior Resident training and be responsible for examination, diagnosis, and treatment. We hold a Gastroenterology conference every week for all cases, and the attending physician gives a presentation on the determination of the treatment policy, followed by a discussion, so that we can provide the best treatment. Gastroenterology is a clinical department with many examinations, there are many procedures that must be mastered. As for this point, while I have little experience, I will do it under the guidance of the staff, but since I can experience a lot, I can improve quickly. Since I have a stance that if my skills improve, I will be able to work independently, so I can live a training life where I can feel that my abilities are improving day by day. Characteristically, in the gastrointestinal tract area, upper and lower endoscopy, ESD, and double-balloon small intestine endoscopy are often performed, and in the bile pancreatic area, there are many cases of calculi and cancer, and there are many ERCP cases. Hepatic artery embolization and radiofrequency ablation/PEIT are also performed by the chief Gastroenterology so all Gastroenterology diseases can be treated consistently among the Senior Resident. We hold conferences with surgical departments, and the level of medical care is high because of coordinated medical care. In addition, since it is a regional core hospital that accepts primary to tertiary emergencies, we can experience a large number of Gastroenterology emergencies, so we are strong in judging and treating emergency cases. In transplant surgery, living-donor liver transplants are also performed, so you can experience a wide range of self-contained gastrointestinal treatments. I think that I will be able to think carefully about the choice for the subsequent career decision during the three years because I will definitely come across a case that interests me. I was able to spend the training period as a Senior Resident in a blessed environment, and even after going out, I realized that the experience, skills, and confidence I gained there were hard to obtain elsewhere.
Impressions about initial training
I think the biggest feature of the initial training at our hospital is that you can experience many different cases with independence. In particular, in the emergency outpatient duty duties that are trained throughout the two years of the initial training, we accept patients from primary to tertiary emergencies, so we will experience a busy emergency outpatient, but we will naturally study and gain knowledge through various experiences. You will also be able to learn the techniques from pediatric drip infusion to intubation. On-duty doctors in each specialized area are on duty during the shift, so you can feel at ease on duty, and if you consult, you can receive appropriate guidance. Internal medicine conferences and autopsy review case conferences (CPC) are held regularly in the hospital, so I think that I am blessed with opportunities to experience and study case presentations inside and outside the hospital. In addition, there are many trainees in the same class, so there are many friends. I was able to spend a very fruitful and fulfilling initial training period that I could not get anywhere else, and I think I was able to grow as a doctor. Irrespective of which department you go to, I think it is a recommended hospital for those who want to make a quick start as a doctor and those who want to start a fulfilling training with many fellow trainees. You can feel that the enthusiastic attitude of the trainees supports Kobe City Medical Center General Hospital, which is able to provide safe medical care as a municipal hospital that is trusted by patients.
Materials provided by: Hospital Cafe
Dr. T (2001-2004: Junior Resident, 2003-2017: Specialist in our Senior Resident)
Impressions about the Senior Resident training
If I am asked about the advantages of the Gastroenterology Senior Resident (3 years), I will answer without hesitation, "A large number of cases and a fulfilling guidance system." In our training, you can experience various cases in both the gastrointestinal tract area and the hepato-biliary-pancreatic area. In addition, because of the large number of cases, it is possible to experience and acquire examination techniques such as endoscopy in a short period of time Hemostasis for bleeding, varicose vein treatment, EMR or ESD, stent placement, etc. In the liver area, RFA, TAE, reservoir placement for liver biopsy and liver cancer, reservoir placement, etc. In the pancreaticobiliary area, ERCP, ENBD, IDUS, PTCD, metallic stent placement, etc.). In addition, there are an extremely large number of emergencies that require emergency treatment, and the primary Senior Resident will be the first call to treat them day and night. Of course, at first, I will be guided by my preceptor, but compared to other hospitals, I think I will be able to stand on my own in a relatively short period of time. This is because, especially in the first year of the Senior Resident, you will be called many times, and you will experience most of the gastrointestinal emergencies during this time, so you will inevitably acquire treatment techniques such as endoscopy.
From the second year onwards, you will develop your own examination and treatment plans for your patients, and further refine your examination and treatment skills. In my case, I was interested in diseases in the pancreaticobiliary region, so I actively participated in examinations such as ERCP and PTCD. In addition, while striving to improve their own skills, we also provide education for trainees who have been rotated and provide guidance to junior Senior Resident.
Due to the large number of cases, it is possible to conduct a wide range of academic activities such as regional meetings and general meetings. In addition, we can actively participate in educational and enlightenment activities for gastrointestinal diseases, such as giving lectures for trainees at emergency open conferences and holding lectures for patients and their families. increase.
Gastroenterology requires a wide range of knowledge because it covers a wide range of diseases. Even if I aim to become a specialist by organ in the future, I believe that it is necessary to be familiar with the diseases of each area because I call myself a Gastroenterology. It's a busy department, but that's why I think it's interesting and rewarding that other departments don't have.
The 3-year latter term training in such a department of Gastroenterology is very hard. There are times when I have very little private time. However, I believe that I will be able to build a solid foundation as a Gastroenterology as a clinician by devoting my full effort to the course over the next three years. We are waiting for the participation of those who have high aspirations as seniors and those who are motivated.
Impressions about initial training
When I became an Junior Resident, it was before the new clinical training system was enforced. At that time, there weren't as many hospitals as there are today that are recruiting trainees, but I was looking for a training hospital with the primary condition of providing comprehensive primary care training through emergency medicine. At that time, I visited the emergency site of the Kobe City Medical Center, which accepts all patients from primary to tertiary, and was very impressed by the high level of the intern doctors working there. This led me to choose Kobe City Medical Center as my training destination, and I can say that the actual content of the training exceeded my expectations.
First of all, I was involved in emergency and anesthesia training for the first six months of my first year, but the first two months were harder than I expected. I remember making repeated mistakes and being reprimanded each time by a senior doctor. However, after overcoming this period, about three months later, I began to realize the fun of clinical practice. If you don't understand something, you can ask for direct guidance from a second-year resident doctor or a supervising doctor in the emergency department or each department, and share useful cases with your fellow trainees. It repeats every day. Over time, you will begin to see clearly that you are getting stronger.
In the second year, the guidance of a new first-year trainee is required. Teaching also organizes the knowledge you have, so both the teaching side and the learning side grow. In addition, second-year students play a sub-leader role in emergency duty, so it is necessary to grasp the situation of the emergency outpatient department as a whole. For example, a wider perspective is required, such as checking if there are any seriously ill patients waiting for Walk-in, and following up on whether the assessment and plan of patients who have already been examined are correct. . It is through these roles that I further develop my competence as a clinician.
During my two years as an Junior Resident, I had the opportunity to see a wide variety of patients, including those on duty. I experienced many tertiary emergency cases such as myocardial infarction, cerebrovascular accident, and multiple trauma. was unaware of the pregnancy).
I believe that I was able to make full use of the experience I gained in the emergency department in the subsequent internal medicine rotation training (as it was called at the time). Kobe City Medical Center receives a large number of cases, not only in the emergency area. It was a short time to visit each department, but I was able to capture the characteristics of each department. In addition, I was able to come into contact with patients with various diseases and receive intensive training. After that, I went on to a specialized course, and for me, the experience of this training in internal medicine has been a great support for my current practice.
In clinical training, there is an idea that no matter where you go, after 10 years, everyone will be together. However, personally, I believe that what kind of experiences you have during your residency period will have a great impact on your growth as a doctor later on. Kobe City Medical Center is filled with a lot of things that I really want to learn, or should learn, during my time as a medical intern. If you are interested, please come and visit us first. I hope you can feel something there.
Dr. S (2002-2013: Junior Resident, 2002-2016: Specialist in our Senior Resident)
Impressions about the Senior Resident training
One of the great experiences I had during my three-year training as a Senior Resident was that I was able to experience many emergency cases of abdominal diseases. The Senior Resident is in charge of nighttime and holiday home visits, and is in a position to consult many emergency cases such as melena and acute abdomen. (Currently, on weekday nights, all the staff are on duty for the Gastroenterology, and on holidays, the general Senior Resident and the staff are on duty at home.) Immediately after completing one case of endoscopic hemostasis, I was consulted for a case of acute pancreatitis, so every day was extremely busy. It was a tough day, like a physical challenge, and I didn't have much time to sit at my desk and study textbooks slowly, but it was a fulfilling 3 that made each of my experiences come to fruition. It was a year. In addition, I think that it was a blessed environment as a training facility that the resident Senior Resident who consulted was not isolated and unsupported, and was able to consult with a senior doctor at any time. In this way, by being entrusted with the initial response, we can gradually expand the scope of what we can do while considering where and to what extent we can take responsibility for medical care and where we need support from. I was able to do the training I went through.
In addition, being able to experience many cases was very useful in acquiring diagnostics and techniques, and I was able to experience most of the general gastrointestinal diseases in three years. In particular, there are many outpatients with chronic hepatitis and cirrhosis of the liver, so being able to experience many emergency patients with ruptured esophagogastric varices and ruptured liver cancer has become a valuable experience now that I am working at another facility. increase. In addition, because it is a core doctor facility in the region, there are many opportunities to be in charge of relatively rare diseases. To do. The Senior Resident on the staff have a deep knowledge of their specialized fields, and looking back several years after finishing my specialty, I can't help but think that the advice they gave me, as well as the ear-study I learned in daily conversations, have contributed to my current medical practice. I feel alive.
As for the specific technical aspects, I was able to experience each examination equally, such as endoscopy, abdominal ultrasound, angiography, and gastroscopy, and was able to acquire these as my own skills. Currently, I work at a facility where I do not perform angiography or gastric fluoroscopy myself, but the experience I gained during my time as a Senior Resident is very useful in general medical care. In addition, it was a good experience for me to be involved in advanced Senior Resident and therapeutic techniques such as ESD, double-balloon small intestine endoscopy, and EUS puncture cytology. Finally, there was an atmosphere in which the entire Department of Gastroenterology was enthusiastic about giving presentations at academic conferences, and I was blessed with the opportunity to make a presentation as a speaker.
Impressions about initial training
I was able to handle a sufficient number of cases in each department, and I was able to experience a large number of acute and severe cases in particular. In particular, the ICU is well-equipped, and I had a good experience learning about systemic management for severe cases. Also, at the internal medicine conference held once a week, the trainees from each department brought together rare diseases and cases that were difficult to diagnose and treat, so I learned a lot. Emergency duty was a busy and tough training, but I was able to experience from the first to the third emergency, and I was able to train under the guidance of staff and Senior Resident who specialize in emergency, and there were always multiple trainees on duty. I think it was a very good environment where we were able to stimulate each other and work hard together.
We consider presentations at academic conferences to be an important part of our clinical activities.
It is possible to organize and share knowledge by summarizing and presenting what one has experienced and learned, such as valuable cases, interesting pathologies, and ingenuity in treatment. It is also expected that presentations at academic conferences will hone their presentation skills. Senior Resident are expected to grow into full-fledged Gastroenterology through presentations at gastroenterological conferences.
Our department is one of the clinical hospitals in the Kinki region that has made the most academic presentations.
Below are the impressions of the conference presentations made by the staff of our department.
Teacher T (2014-: Our department staff)
Society overview
| Participating conference | Digestive disease Week 2017 (DDW2017) |
|---|---|
| venue | Chicago, Illinois, USA |
| Schedule | May 6-9, 2017 |
Events and Impressions at Participating Conferences
Following DDW2016 (San Diego), I participated in Digestive Disease Week 2017 (DDW 2017) for four days from May 6th to 9th, 2017. This time it was held at McCormick Place in Chicago, Illinois, USA. DDW is one of the world's largest societies related to the gastrointestinal tract. It will be held jointly by four societies of the American Society of Gastroenterological Surgeons (SSAT).
First of all, I was surprised by the scale of the conference. It was a very stimulating conference with a wide range of presentations. In addition, we received presentations from all over the world, and my presentation this time was "Cross-wired metallic stent in endoscopic bilateral stent-in-stent placement for malignant hilar obstruction". It was something. The presentation will be a poster presentation, and you will stand in front of the poster during the allotted time and directly ask questions. Every time I participate in an international conference, I am keenly aware of my lack of proficiency in English, and at the same time it motivates me to study English in the future.
Also, as an option for the academic conference, I was able to attend a baseball game in Chicago, watch the MLB game between Chicago and the New York Yankees, and listen to the performance of the world-famous Chicago Symphony Orchestra.
Through this conference, I was able to see the world's most advanced treatments and research, and I was able to experience things that I would not be able to experience in Japan, so I was able to spend a meaningful time.
Junior Resident Senior Resident
Society overview
| Participating conference | European Gastroenterology Week 2016 (UEGW2016) |
|---|---|
| venue | Vienna, Austria |
| Schedule | October 15-19, 2016 (2nd year Senior Resident) |
Events and Impressions at Participating Conferences
UEGW is an international conference in the field of gastrointestinal tracts in Europe, and is a huge conference held annually with more than 10,000 participants. In the first place, the impetus for participating in the conference was an impure motive of wanting to visit the fashionable city of Vienna. From around January 2016, I consulted with a senior doctor about topics that could be presented at international conferences. I received a notice of acceptance in July, and from there I spent almost every day looking at the hotel I was planning to stay at and researching tourist information about Vienna before the conference in October.
The academic conference is scheduled for 5 days, with educational lectures on the first 2 days and general presentations on the remaining 3 days. Looking at the conference participants by region, 65% came from the European continent, 17% from the Middle East/Asia, and 5% each from the Americas, South America, and Africa. The number of participants was the largest in Asia. Most of the presentations from Japan were from cancer centers and university hospitals, and the number of presenters from general hospitals like our hospital was small, and it felt like we were away.
The content of the academic conference is similar to that of academic conferences in Japan, and various sessions are held in parallel at several venues from morning to evening. There was no luncheon seminar, so when it came time for lunch, catered sandwiches, water, and fruits such as apples were brought to a designated area of the venue, and participants were free to take and eat them. Poster presentations are posted in the poster exhibition area from morning to evening, and the poster presenters stand by the posters from 12:30 to 13:30 in the daytime to answer questions about the posters. It was not the case that all the participants would speak their posters. My own presentation was a bit of a maniac, and fortunately I was able to get through it without any difficult questions.
After the conference (which was the most enjoyable part of the trip), I spent as much time as my physical strength allowed to visit Vienna and watch the orchestra. Vienna has a lot of tourist attractions around the central area called the Ring, and all of them are reasonably sized to go around on foot, trams, and subways, and I was able to see most of them during my short stay .
It was my first time attending an international conference, so I was nervous, but not only was the city of Vienna wonderful, but Japanese doctor of a slightly older generation than me stood on the platform of the conference venue at symposiums and workshops, in front of Westerners. Seeing them confidently present their work was very stimulating and made me keenly aware of the need for English proficiency. I was away from the hospital for about a week, but I am very grateful to the doctors in the department for kindly sending me to the conference.
Dr. I (2012-2013: Junior Resident, 2014-2016: Specialist in our Senior Resident)
Society overview
| Participating conference | Digestive Disease Week 2016 (DDW2016) |
|---|---|
| venue | San Diego, California, USA |
| Schedule | May 24-27, 2016 (3rd year Senior Resident) |
Events and Impressions at Participating Conferences
Digestive Disease Week, held annually in the United States, is an authoritative conference on digestive diseases that gathers the latest basic and clinical research topics from around the world. In 2016, it was held from May 24th to 27th, and especially since the 24th and 25th were holidays, it was crowded with many participants. Every day, there were presentations in each area of specialization, and from 8:00 in the morning until the evening, there were many poster sessions during the lunch break, where enthusiastic discussions took place. This time, I was fortunate enough to make two presentations at the poster session on the 24th, "Treatment Predictors of Tolvaptan," and on the 26th, "The Lecture on Duodenal Stents."
At DDW2016, various latest researches from North America, Europe, and Asian countries were selected as the subjects, and we were able to see interesting presentations every day. Devices and treatment methods that have not been used in Japan were very new, and there were some that I really wanted to introduce. Discussions were more lively than at academic societies in Japan, and every session was extremely productive. It was a great experience for me to have the opportunity to present two presentations in the poster session. doctor from South America and the Middle East also took an interest in the presentation of tolvaptan, and asked questions from a different perspective than in Japan. Also, in the presentation of the duodenal stent, I actively discussed with an Indian doctor, and found that the way of thinking about stent selection and indwelling method is completely different from that of Japan. While continuing our good things, we would like to make each treatment more sophisticated by incorporating new methods. Also, the common language is English, and I often felt during the exhibition that I needed to improve my communication in English so that I could accurately convey what I wanted to say and think. This was my first time participating in DDW, but I learned a lot because I was able to come into contact with many different things. And I would like to make use of what I learned this time in clinical practice.

In the spring of 2018, the internal medicine specialist training program will start.
As a core facility, our hospital will also disclose a program to train specialists in each area of internal medicine, so please refer to the hospital website.
As a policy of Gastroenterology, 4 months from the start of the first year are devoted to subspecies (digestive organs) training, and during this period, students learn the basics of digestive organs and basic procedures such as endoscopy. . After that, we will start basic area training, but while aiming to broaden our horizons as a physician by having them handle a specified number of cases in each area, we will also focus on work so that our experience in subspecial areas does not become hollow. I am taking care of The second year will be an out-of-hospital training period, but the affiliated facilities are Kobe City Municipal Medical Center Nishi Municipal Hospital, Nishi Kobe Medical Center, Hyogo Prefecture Amagasaki General Medical Center, Japanese Red Cross Wakayama Medical Center, Tenri Yorozu Consultation Center Hospital, and Otsu Red Cross. At hospitals and other hospitals affiliated with the Department of Gastroenterology Kyoto University, we provide training mainly in the subspecialty area. In the third year, as the final year of the Senior Resident, we plan to have the main force of medical treatment at our department.
In the Gastroenterology field, it is important to experience many cases and master many procedures. Aim.
1. Practical (Practical) Principle
The greatest feature of our department is the principle of actual combat (practice). It goes without saying that textbook knowledge is extremely important as a foundation, but in actual clinical practice, things that do not follow the textbook or are not found anywhere in the textbook often occur. Medical care exists to save the suffering patients right in front of us, and humans are not so simple as to be divisible by theory (and sometimes evidence). In this respect, medicine can be said to be both an academic field and a practical science. We consider experience to be the most important thing. I believe that the result of hard work, learning, and effort in order to save actual patients will not only improve the abilities of individual doctor, but also raise the level of the entire Gastroenterology group and the hospital as a whole. Would you like to sweat with us at the actual site?
2. One-on-one guidance system
For example, no one can suddenly perform a gastroscopy from the start. Of course, we do not want them to do so. First, they learn the significance of the examination, understanding of the pathology, diagnostics, and handling of equipment, etc., and then they aim to master the examination under the guidance of senior doctors. While the new doctor patient is sweating while performing the examination, the supervising physician is also present, his hands sweating. The moment they turn around and look at you, you will be able to get the appropriate guidance. We do not teach by hand-holding. While assessing the patient's ability, advice and a helping hand will be offered when more advanced judgment or treatment is needed.
3. Abundant and valuable cases (experience)
As one of the leading hospitals in the Kinki region, not to mention Kobe City, we are able to experience a wide range of conditions from mild to severe. Compared to general clinical training hospitals, we are in charge of many cases in a short period of time, so specialists such as the Gastroenterology Society, Endoscopy Society, Hepatology Society, etc. Rare conditions, such as one case per year (sometimes in a lifetime), are also commonly encountered. It is a hospital that considers 10 cases of pathological conditions that are reported as one case at research meetings and academic societies. However, just because there are many cases, we never neglect one case at a time. For patients, this is their first illness and their first anxiety, and as specialists, we are required to respond calmly and sincerely.
4. Clarification of complex pathologies by a group of experts
We often encounter seemingly "incomprehensible" pathologies. At that time, please consult a senior doctor first without worrying about it alone. You should be able to get valuable advice, but if you still have trouble, consult with each clinical department. It is a daily occurrence that cirrhotic patients with heart disease suffer from disturbance of consciousness due to electrolyte imbalance caused by respiratory infection and recover from the critical condition under ICU management. Of course, it is necessary for the doctor in charge to be fully active, but before you know it, the helping hands of specialists are reaching out from all over the place.
5.Traditional training system (training program)
For more than 30 years, our hospital has trained clinicians through our own clinical training program and sent them out across the country. In the training program for internal medicine specialists to start in 2018, based on that experience, we examined the guidance system for internal medicine as a whole. Please refer to the hospital website for details. What I would like to emphasize here is that this system was not created overnight, but was refined through repeated trial and error. This is still going on today, and every month we gather from hospital executives to young staff members to repeatedly review and improve problems. In other words, the postgraduate education that we have practiced is like a "cradle of toughness." becomes. I don't think there is necessarily a need for a charismatic instructor or a new and eccentric program.
15 years have passed since the start of the "new clinical training system" formulated by the Ministry of Health, Labor and ministry of Health, Labor and Welfare notation. The significance of aiming for training in a wide range of fields in the first two years after graduating can be evaluated, but it can be said that the merits and demerits are mixed, as it caused a crisis of medical collapse that became apparent afterwards. Even if the Buddha was created by a bureaucrat, it is only us medical professionals who can put the soul into it. "Tradition was not built in a day".
6.Let's Join Us!
We appeal to young people who will bear the future of medical care with passion. Would you like to sweat with us? It's a dizzying day, but it's also a day where I feel a sense of fulfillment. Even as medical care becomes highly specialized, the gastrointestinal field covers an extremely large number of diseases and pathological conditions, and can be treated with a variety of techniques. We welcome you with open arms.
Papers and conference presentations
- Yabuuchi Y et al.: Effective Endoscopic Delineation With Acetic Acid Spray and Narrow Band Imaging in Underwater Endoscopic Mucosal Resection for Sessile Serrated Lesion. The American Journal of Gastroenterology 117:840, 2022
- Aoyama N et al.: A case of neuroendocrine neoplasm of the minor duodenal papilla. Clinical Journal of Gastroenterology:2022
- Aoyama N et al.: Olmesartan-associated sprue-like enteropathy. BMJ 2022;15:e254189: 2022
- Tanaka K et al.: Endoscopic submucosal dissection for a superficial esophageal squamous cell carcinoma located in a Rokitansky diverticulum. Endoscopy E-Videos CC BY-NC-ND 4.0 ・ Endoscopy 2022; 54(S 02): E986-E987:2022
- Hosotani K et al.: Endoscopic submucosal dissection for complete removal of a residual colorectal tumor involving a diverticulum. Endoscopy E-Videos CC BY-NC-ND 4.0 ・ Endoscopy 2022; 54(S 02): E908-E909:2022
- Yabuuchi Y et al.: A novel technique to improve endoscopic accessibility in laparoscopic endoscopic cooperative surgery for a duodenal lesion. Endosc Int Open 2022; 10(12): E1597-E1598:2022
- Hosotani K et al.: Detecting remnant sessile serrated lesion after piecemeal cold snare polypectomy using acetic acid with narrow-band imaging. Endosc Int Open 2022; 10(12): E1595-E1596:2022
- Aoyama N et al.: Pancreatic metastasis from lung adenocarcinoma. Journal of General and Family Medicine:2023
- Daichi Imamura et al.: Clinical features of 174 cases of IgA vasculitis. The 119th Annual Meeting The Japanese Society of Internal Medicine, Kyoto/Web, April 16, 2022
- Tanjia, Motoyoshi: Study of common bile duct stone treatment by EPBD/EPLBD in our hospital. The 108th Annual Meeting The Japanese Society of Gastroenterology, Tokyo/Web, 2022/4/21
- Shinsuke Akiyama et al.: Endoscopic biliary drainage treatment strategy for malignant biliary stricture before surgery for pancreatic cancer. The 108th Annual Meeting The Japanese Society of Gastroenterology, Tokyo/Web, 2022/4/23
- K. Tanaka et al.: Ingenuity of ESD for Japan Gastroenterological Endoscopy Society cancer in Rokitansky diverticulum.
- Yohei Yabuuchi et al.: D-LECS for superficial non-papillary duodenal Japan Gastroenterological Endoscopy Society tumors: from safe and reliable ESD to suturing.
- Gensho Tanjia et al.: Results of continuous pancreatic juice Japan Gastroenterological Endoscopy Society for pancreatic duct stenosis without mass in our hospital.
- Yoshiki Morihisa et al.: A case of adult-onset IgA vasculitis with characteristic gastrointestinal lesions. The 108th Annual Meeting Japan Gastroenterological Endoscopy Society Kinki Branch, Kyoto, June 11, 2022
- Soichiro Nagao et al.: Usefulness of Japan Gastroenterological Endoscopy Society classification in community hospitals and future issues.
- Oshikawa D. et al.: A case of duodenal accessory papilla Japan Gastroenterological Endoscopy Society tumor associated with Crohn's disease.
- Fujio, Y. et al.: A case of diverticular hemorrhage in the duodenal horizontal part successfully hemostasis by Japan Gastroenterological Endoscopy Society
- Shimokawa, G. et al.: A case of accidental ingestion of a large number of Japan Gastroenterological Endoscopy Society batteries that were removed endoscopically.
- Ryoko Tatsuno et al.: Diagnostic performance of EUS-FNA for small pancreatic neuroendocrine tumors in our hospital. The 117th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, 2022/10/8
- Toshiya Nanjo et al.: A case of small bowel MALT lymphoma with small bowel obstruction.The 117th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, 2022/10/8
- Oshikawa D. et al.: A study of 37 cases of adult intussusception. The 117th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, 2022/10/8
- Tsukamoto K. et al.: Two cases of fenofibrate-intolerant primary biliary cholangitis successfully treated with pemafibrate.The 117th meeting of the Kinki branch of The Japanese Society of Gastroenterology, Osaka, October 8, 2022
- Shimokawa, G. et al.: A case of intratumoral hemorrhage during administration of lenvatinib after TAE for giant hepatocellular carcinoma.The 117th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, 2022/10/8
- Takehito Ogawa et al.: Two cases of acute necrotizing esophagitis with edematous wall thickening of the esophagus on CT.The 117th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, 2022/10/8
- Yukie Fujio et al.: A case of hypophysitis caused by administration of Nivolmab for esophageal cancer.The 117th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, 2022/10/8
- Asuka Sone et al.: A case of irAE (immune-related adverse event) cholangitis developed during administration of an immune checkpoint inhibitor.The 117th meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, 2022/10/8
- Katsuyama, S. et al.: A case of pancreatic MiNEN discovered by abdominal pain and diagnosed by surgical resection.The 117th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, 2022/10/8
- Shinsuke Akiyama et al.: Necessity and prognosis of preoperative EUS-FNAB for resectable pancreatic body and tail cancer. JDDW2022, Fukuoka/Web, 2022/10/28
- Tanya, M. et al.: Results of serial pancreatic juice cytology for intraductal papillary mucinous tumor with contrast-enhanced nodule in our hospital. JDDW2022, Fukuoka/Web, 2022/10/28
- Kenta Yamamoto et al.: Current status of drainage treatment for malignant biliary obstruction in our hospital. JDDW2022, Fukuoka/Web, 2022/10/29
- Soichiro Nagao et al.: Examination of Japan Gastroenterological Endoscopy Society bleeding in the elderly.
- Yukie Fujio et al.: A case of methotrexate-associated lymphoproliferative disease diagnosed by bloody stool. The 109th Annual Meeting of the Kinki Branch Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2022/11/5
- Satoko Inoue et al.: Effects and prospects of Japan Gastroenterological Endoscopy Society balloon dilatation for Crohn's disease intestinal stenosis.
- Kazuya Hosoya et al.: Evaluation of colonoscopy quality indicator using Japan Japan Gastroenterological Endoscopy Society Database and future issues.
- Daisuke Oshikawa et al.: A case of secondary Japan Gastroenterological Endoscopy Society fistula requiring differentiation from bloody stool caused by exacerbation of ulcerative colitis.
- Takehito Ogawa et al : Japan Gastroenterological Endoscopy Society tract cancer.
- Shinsuke Akiyama et al.: Current status and issues of Japan Gastroenterological Endoscopy Society step-up approach for peripancreatic fluid retention.
- Toshiya Nanjo et al.: A case study of Japan Gastroenterological Endoscopy Society after placement of a metal biliary stent for malignant biliary stenosis in our hospital.
- Asuka Sone et al.: A case of esophageal perforation caused by an overtube during endoscopic treatment for early esophageal cancer. The 109th Annual Meeting of the Kinki Branch Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2022/11/5
- Soichiro Nagao et al.: Results of combination therapy with atezolizumab and bemacizumab for hepatocellular carcinoma in a city hospital.The 118th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, January 21, 2023
- Satoko Inoue et al: Remission maintenance effect of vedolizumab in ulcerative colitis. The 118th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, January 21, 2023
- Asuka Sone et al.: Current status of transpapillary pathological diagnosis of biliary stricture due to cholangiocarcinoma in our hospital.The 118th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, January 21, 2023
- Kazuyuki Tsukamoto et al.: A case of amoebic colitis presenting with hemorrhagic shock.The 118th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, January 21, 2023
- Ryoko Tatsuno et al.: Preoperative diagnosis of Meckel's diverticulum -From the experience of 20 cases at our hospital-.The 118th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, January 21, 2023
- Arino H. et al.: A case of metachronous rupture of an aneurysm of the pancreaticoduodenal artery with median arcuate ligament syndrome.The 118th meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, January 21, 2023
- Yukie Fujio et al.: A case of intrahepatic cholangiocarcinoma with disseminated recurrence due to preoperative percutaneous biliary drainage.The 118th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, 2023/1/21
- Toshiya Nanjo et al.: A case of malignant perihilar bile duct obstruction treated with EUS drainage.The 118th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, January 21, 2023
- Soichiro Nagao et al.: Prophylactic suturing of mucosal defects after gastric ESD in patients with high risk of post-operative bleeding. The 95th Annual Meeting of the Japanese Gastric Cancer Society, Sapporo, February 24, 2023
- Hosoya K. et al.: A study of surveillance-detected gastric cancer after gastric ESD. The 95th Annual Meeting of the Japanese Society of Gastric Cancer, Sapporo, 2023/2/25
- Morita S: Multicenter prospective in vivo study of an endocytoscope system(ECS) for superficial esophageal cancer. Journal of Gastroenterology 56, pages808–813, 2021
- Ueda T et al.: Shaggy white lesion with morphological changes in the oesophagus. Gut DOI: 10.1136/gutjnl-2021-326643, 2022
- Shinsuke Akiyama: Usefulness of joint laparoscopic-endoscopic surgery for gastric submucosal tumors. The 107th Annual Meeting of the The Japanese Society of Gastroenterology, Tokyo/Web, April 15, 2021
- Tanya, Motoyoshi: Examination of early symptoms in pancreatic duct cancer treatment at our hospital. The 107th Annual Meeting of the The Japanese Society of Gastroenterology, Tokyo/Web, 2021/4/15
- Karawatari S. et al.: Treatment and prognosis of primary gastrointestinal follicular lymphoma. The 101st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Hiroshima/Web, May 14, 2021
- Tomoya Ueda et al.: A study on predictors of bleeding after gastric ESD. The 101st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Hiroshima/Web, May 15, 2021
- Shinsuke Akiyama et al.: Current status and issues of EMR and UEMR for superficial non-papillary duodenal epithelial tumors. The 101st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Hiroshima/Web, May 14, 2021
- Soichiro Nagao et al.: A study of electrohydraulic impact lithotripsy (EHL) in our hospital. The 101st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Hiroshima/Web, May 14, 2021
- Kazuya Hosoya et al.: Study of short-term and long-term results of gastric ESD in elderly people aged 85 years and over. The 101st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Hiroshima/Web, May 16, 2021
- Hiroshi Tei: Seven cases of reactive lymphoid hyperplasia in the liver -report including long-term natural history-. The 57th Annual Meeting The Japan Society of Hepatology, Sapporo/Web, June 18, 2021
- Shuichiro Karawatari et al.: (Additional remarks 1) Examination of 11 lesions pathologically diagnosed as cancer after cold snare polypectomy at our hospital. The 106th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka/Web, 2021 /7/10
- Noriaki Ando et al.: Study of Japan Gastroenterological Endoscopy Society submucosal dissection (ESD) for early gastric cancer in the elderly -from the aspect of functional evaluation-. 7/10
- Tomoya Ueda et al.: A case of dissecting hepatic aneurysm diagnosed by Japan Gastroenterological Endoscopy Society hemorrhage due to duodenal perforation.
- Yoshiki Morihisa et al.: Japan Gastroenterological Endoscopy Society consideration of 9 cases of intestinal AVM experienced at our hospital.
- Shinsuke Akiyama et al.: (Additional remarks 1) Experience of using Japan Gastroenterological Endoscopy Society for intractable bleeding and perforation associated with ERCP-related procedures.
- Hiroshi Tei et al.: Clinical characteristics of increasing metabolic syndrome liver cancer.The 115th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Web, 2021/9/18
- Tomoya Ueda et al.: A case of esophageal epidermization that was difficult to differentiate from esophageal cancer for a long time.The 115th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Web, 2021/9/18
- Masayuki Shimoyama et al.: A Case of Early Gastric Neuroendocrine Carcinoma Diagnosed Preoperatively.The 115th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Web, 2021/9/18
- Shuichiro Karawatari et al.: A case of gastrointestinal follicular lymphoma that led to therapeutic intervention with transformation during long-term follow-up.The 115th meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Web, 2021/9/18
- Yoshiki Morihisa et al.: A case of acute pancreatitis caused by hypertriglyceridemia during pregnancy.The 115th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Web, 2021/9/18
- Takuya Kobayashi et al.: A case of pancreatic body and tail cancer with needle tract seeding after EUS-FNA performed for postoperative diagnostic purposes.The 115th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Web, 2021/9/18
- Noriaki Ando et al.: A case of mucinous cystic tumor that turned malignant after 18 years.The 115th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Web, 2021/9/18
- Daichi Imamura et al.: A case of IgA vasculitis with severe abdominal pain.The 115th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Web, 2021/9/18
- Kosuke Tanaka et al.: A report of a case of past HBV infection that was reactivated by steroid administration alone.The 115th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Web, 2021/9/18
- Soichiro Nagao et al.: Examination of the usefulness and safety of UEMR for surface colorectal tumors of 10 mm or less. JDDW2021, Kobe/Web, 2021/11/4
- Hosotani K et al.: Optimized optical stratification by JNET classification with chromoendoscopy for colorectal lesions ?10 mm. JDDW2021,Kobe/Web, 2021/11/5
- Motoyoshi Tanji et al.: Examination of PET in pancreatic ductal cancer treatment at our hospital. JDDW2021, Kobe/Web, 2021/11/6
- Satoko Inoue: Report of three cases of olmesartan-associated sprue-like enteropathy. The 59th Annual Meeting of the Japanese Society of Small Intestines, Tokyo/Web, 2021/11/27
- Shinsuke Akiyama et al.: Japan Gastroenterological Endoscopy Society biliary drainage for distal bile duct stenosis due to pancreatic cancer.
- Tomoya Ueda et al.: Examination of Japan Gastroenterological Endoscopy Society characteristics of gastric cancer detected after gastric ESD.
- Yabuuchi, Y. et al.: Possibility of Underwater EMR under NBI observation after spraying acetic acid for Japan Gastroenterological Endoscopy Society serrated lesions.
- Motoyoshi Tanji et al.: Experience of choledoscopic electrohydraulic shock wave lithotripsy (EHL) for difficult-to-treat bile duct stones in our hospital. The 107th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Kobe/Web, 2021 /12/11
- Satoko Inoue et al.: Role of capsule Japan Gastroenterological Endoscopy Society in treatment of Crohn's disease.
- Kazuya Hosoya et al.: Comparison of short-term results of Underwater EMR and Conventional EMR for non-Japan Gastroenterological Endoscopy Society colorectal tumors less than 10 mm.
- Yoshiki Morihisa et al.: A case of Japan Gastroenterological Endoscopy Society gastritis and duodenum diagnosed with gastrointestinal hemorrhage.
- Noriaki Ando et al.: Secondary aortoduodenal fistula experienced at our hospital. The 107th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Kobe/Web, 2021/12/11
- Shuichiro Japan Gastroenterological Endoscopy Society et al.: A case of en bloc resection by Underwater EMR for a tumor at the appendiceal orifice.
- Takuya Kobayashi et al.: A case of definite diagnosis of pancreatic metastasis of mammary gland Japan Gastroenterological Endoscopy Society tumor by EUS-FNA.
- Kosuke Tanaka et al.: 4 cases of breast cancer Japan Gastroenterological Endoscopy Society metastasis experienced at our hospital.
- Shinsuke Akiyama et al.: Needle tract seeding and prognosis associated with EUS-FNAB before pancreatic body and tail cancer surgery.The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web, 2022/2/5
- Noriaki Ando et al.: Current status of gastrointestinal bleeding in COVID-19 positive patients.The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web, 2022/2/5
- Yoshiki Morihisa et al.: A study of endoscopic hemostasis difficult cases for diverticular bleeding in the large intestine. The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web, 2022/2/5
- Morita, S. et al.: A case study of Nivolumab administration for esophageal cancer in our hospital. The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web, 2022/2/5
- Takaori, K. et al.: A case of small intestinal GIST with peculiar morphology and difficult preoperative diagnosis.The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web, 2022/2/5
- Daisuke Oshikawa et al.: Experience of decompression therapy using PEG-J for chronic idiopathic intestinal pseudo-obstruction.The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web, 2022/2/5
- Karawatari S. et al.: A case of autoimmune hepatitis and primary sclerosing cholangitis after chronic hepatitis C treatment with a direct-acting antiviral drug.The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web , 2/5/2022
- Soichiro Nagao et al.: A case of gangliocytic paraganglioma treated endoscopically.The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web, 2022/2/5
- Tomoya Ueda et al.: A case of pancreatic leiomyoma diagnosed with acute cholangitis.The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web, 2022/2/5
- K. Tanaka et al.: A case of primary MALT lymphoma from the appendix. The 116th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka/Web, 2022/2/5
- Kitamoto H et al.: Successful Endoscopic Removal of a Large Pancreatic Stone in a Patient After Pancreaticoduodenectomy. Clinical Gastroenterology and Hepatology Volume18, Issue5: A30-A31, 2020/5
- Hosotani K et al.: A case of anal intraepithelial neoplasia resected by endoscopic submucosal dissection after magnifying narrow-band imaging evaluation. Gastrointestinal Endoscopy GIE :Published 2020/6/9/li\u003e
- Okubo Y et al.: Recurrence of pembrolizumab-induced severe gastritis after tapering steroid therapy. Journal of Gastroenterology and Hepatology:Published 2020/9/18/li\u003e
- Hosotani K et al.: Underwater endoscopic mucosal resection for complete R0 removal of colorectal polyp in a patient with ulcerative colitis. Endoscopy: doi:10.1055/a-1346-8769, 2021/2/16
- Tanaka, Y. et al.: Endoscopic images of olmesartan-associated sprue-like bowel disease. The 104th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Web, 2020/6/27
- Yoshiki Morihisa et al.: A case of Campylobacter enterocolitis in a hemophilia patient with massive bleeding. The 104th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Web, 2020/6/27
- Soichiro Nagao et al.: A case of submucosal submucosal hematoma of the large intestine during administration of warfarin. The 104th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Web, 2020/6/27
- Akiyama, S. et al.: Current state of endoscopic treatment for duodenal diverticular bleeding. The 104th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Web, 2020/6/27
- Shinsuke Akiyama: Superficial non-papillary duodenal epithelial tumor (SNADET). The 106th Annual Meeting of the The Japanese Society of Gastroenterology, Web, 2020/8/11-13
- Masaya Wada: Investigation of surgical indication for pancreatic mucinous cystic tumor (MCN) from a resected case at our hospital. The 106th Annual Meeting of the The Japanese Society of Gastroenterology, Web, 2020/8/11-13
- Naoto Urano: Current status of oral resection for superficial or hypopharyngeal cancer in our hospital. The 106th Annual Meeting of the The Japanese Society of Gastroenterology, Web, 2020/8/11-13
- Tanaka, Y. et al.: A case study of liver injury caused by immune checkpoint inhibitors in our hospital. The 106th Annual Meeting of the The Japanese Society of Gastroenterology, Web, 2020/8/11-13
- Morita, S.: Clinical course of 7 cases of early gastric cancer followed up. The 99th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2020/9/2-3
- Shuko Morita: Is endocyto effective in diagnosing esophageal squamous cell carcinoma? - Based on evidence -. The 99th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2020/9/3
- Shinsuke Akiyama et al.: Current state of joint laparoscopic endoscopic surgery for gastric submucosal tumors in our hospital. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Satoko Inoue: Short-term and long-term therapeutic effects of tofacitinib for ulcerative colitis. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Taniguchi, Y. et al.: Study on tumor size of 10 mm or less in resected TS1 pancreatic cancer. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Tanaka, Y. et al.: Clinical features of immune checkpoint inhibitor-associated enteritis in our hospital. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Ando N. et al.: A case of duodenal NET with tissue diagnosis by EUS-FNA. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Tomoya Ueda et al.: A case of dissecting hepatic aneurysm that was diagnosed with gastrointestinal bleeding due to duodenal perforation. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Haohang Chung et al.: Treatment strategies for advanced hepatocellular carcinoma using molecular targeted drugs with sequential therapy in mind. The 113th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2020/10/3
- Kokubo Y. et al.: A case of cerebral infarction during administration of sorafenib for advanced hepatocellular carcinoma. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Ryoko Tatsuno et al.: A case of primary amyloidosis diagnosed with severe liver dysfunction and nephrotic syndrome. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Soichiro Nagao et al.: A case of polyarteritis nodosa with ruptured hepatic aneurysm as the initial symptom. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Tanjia, M. et al.: Investigation of postoperative recurrence of liver metastasis in advanced pancreatic ductal cancer in our hospital. The 113th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka/Abstract, 2020/10/3
- Noriaki Ando et al.: A study of 9 cases of duodenal NET at our hospital. JDDW2020, Kobe/Web, 2020/11/5
- Yohei Taniguchi et al.: Comparison of Metallic Stent vs Plastic Stent in preoperative drainage for pancreatic cancer. JDDW2020, Kobe/Web, 2020/11/5
- Morita, S.: Local submucosal injection of steroid without local injection needle. The 74th Annual Meeting of the The Japan Esophageal Society, Tokushima/Web, 2020/12/10-11
- Soichiro Nagao et al.: Prophylactic closure of mucosal defects after ESD in patients with high risk of post-operative bleeding. The 105th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2020/12/19
- Tanaka, Y. et al.: A case of superficial esophageal carcinoma for which observation by ultra-magnifying endoscopy was useful for diagnosis. The 105th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2020/12/19
- Akiyama, S. et al.: Current state of hemostasis for duodenal diverticular bleeding. The 105th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2020/12/19
- Taniguchi, Y. et al.: A study of electrohydraulic impact lithotripsy (EHL) in patients with difficult choledocholithiasis in our hospital. The 105th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2020/12/19
- Shuichiro Karawatari et al.: A case of gastric torsion associated with hiatal hernia undergoing elective surgery after endoscopic reduction. The 105th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2020/12/19
- N. Ando et al.: A case in which the SO clip was useful in endoscopic resection of Brunner's gland hamartoma of the duodenum. The 105th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2020/12/19
- Tatsuno, R. et al.: A case of duodenal GIST associated with autoimmune pancreatitis. The 105th Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Kyoto/Web, 2020/12/19
- Masaya Wada: Results of somatostatin receptor scintigraphy and FDG-PET in diagnosing pancreatic neuroendocrine tumors. The 51st Annual Meeting of the Japan Pancreas Society, Kobe/Web, 2021/1/8
- Ryoko Tatsuno et al.: A case of de novo autoimmune hepatitis after living-donor liver transplantation diagnosed with severe liver dysfunction. The 114th regular meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Web, 2021/2/27
- Soichiro Nagao et al.: A case of hepatocellular carcinoma with extrahepatic development in a normal liver that was difficult to diagnose. The 114th regular meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Web, 2021/2/27
- N. Ando et al.: A case of resection of lymphocyte-rich HCC with high PDL-1 expression. The 114th regular meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Web, 2021/2/27
- Yukari Tanaka et al.: A case of small enteritis as an irAE during long-term use of an immune checkpoint inhibitor. The 114th regular meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Web, 2021/2/27
- Karawatari S. et al.: A case of small bowel Burkitt's lymphoma with intussusception. The 114th regular meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Web, 2021/2/27
- Kitamoto H et al.: A Rare Tumor Disseminated to the Gastrointestinal Tract After Treatment for HIV-Associated Lymphoproliferative Disease. Gastroenterology 2019 Volume156 Issue8 Pages2136–2138,2019/6/1
- Kitamoto H et al.: Chronic GI bleeding in a middle-aged woman. Gut Aug 2019, Volume 68 Issue 8, 1385-1429, 2019/8/1
- Kitamoto H et al.: Scanning early catches the worm: Abdominal ultrasound as a possible screening method for intestinal cestodes. Lancet Vol.394 No.10205,2019/10/5
- Daiki Fumihara et al.: Experience of using lenvatinib for regorafenib-refractory cases in our hospital. The 55th Annual Meeting of the The Japan Society of Hepatology, Tokyo, May 30, 2019
- Masaya Wada: Endoscopic ultrasonography for peripancreatic fluid retention in pancreatic cysts. The 97th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 31, 2019
- Ayako Morita: Endoscopic diagnosis of the depth of invasion in superficial pharyngeal tumors. The 97th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 31, 2019
- Yohei Taniguchi: Investigation of preoperative full covered metallic stent (fCSEMS) for middle-lower malignant biliary stricture. The 97th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, June 1, 2019
- Urano, N.: A study of non-curative resection cases of gastric cancer with ESD. The 97th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, June 1, 2019
- Morita, S.: Clinical course of a case with T4b wall invasion. The 73rd Annual Meeting of the The Japan Esophageal Society, Fukuoka, June 6, 2019
- Tanaka, Y. et al.: A study of emergency IVR for non-variceal upper gastrointestinal bleeding for which endoscopic hemostasis was difficult. The 102nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2019/7/6
- Satoko Inoue et al.: Clinical features of colitic cancer associated with ulcerative colitis. The 102nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2019/7/6
- Tomoya Ueda et al.: A case in which fully covered self-expandable metallic stent placement was useful for refractory biliary fistula after laparoscopic cholecystectomy. The 102nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2019/7/6
- Soichiro Nagao et al.: A case of micro PanNET in which EUS-FNA was useful in differentiating pancreatic metastasis from renal cell carcinoma. The 102nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2019/7/6
- Yuki Okubo et al.: A case of pembrolizumab-associated gastritis that was relieved by steroids. The 102nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2019/7/6
- Yuka Ikeda et al.: A case of acutely progressing gastrointestinal amyloidosis in which tocilizumab was effective. The 102nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2019/7/6
- Daiki Fumihara et al.: Two cases of hypopharyngeal carcinoma that was difficult to detect by normal endoscopy and to observe the entire appearance. The 102nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2019/7/6
- Akiyama, S. et al.: ESD experience for esophageal granulocytoma. The 102nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2019/7/6
- Karawatari S. et al.: A study of upper gastrointestinal endoscopic foreign body removal cases in our hospital. The 102nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2019/7/6
- Taniguchi, Y. et al.: Study of preoperative biliary drainage for pancreatic cancer -Metallic Stent vs. Plastic Stent-. The 50th Annual Meeting of the Japan Pancreas Society, Tokyo, 2019/7/12
- Wada, M. et al.: A case of pancreatitis thought to be an immune-related adverse event caused by pembrolizumab. The 50th Annual Meeting of the Japan Pancreas Society, Tokyo, 2019/7/12
- Wada, M. et al.: A case study of resected pancreatic mucinous cystic tumor (MCN) in our hospital. The 50th Annual Meeting of the Japan Pancreas Society, Tokyo, 2019/7/13
- Shinsuke Akiyama et al.: Examination of usefulness of EUS-FNA for gastric submucosal tumors. The 111th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2019/10/5
- Hosoya K. et al.: Study of eCuraC-2 cases of gastric cancer after ESD. The 111th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2019/10/5
- Shuichiro Karawatari et al.: A case of locally advanced unresectable pancreatic cancer successfully treated with gemcitabine + nab-paclitaxel combination therapy and conversion surgery was possible. The 111th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2019/10/5
- Soichiro Nagao et al.: A case of ulcerative colitis requiring surgical treatment for stricture of the descending colon. The 111th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2019/10/5
- Daiki Fumihara et al.: A case of long-term efficacy of lenvatinib for hepatocellular carcinoma refractory to regorafenib. The 111th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2019/10/5
- Tanaka, Y. et al.: A case in which mycophenolate mofetil was remarkably effective against steroid-resistant severe liver injury caused by anti-PD-1 antibody. The 111th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2019/10/5
- Tomoya Ueda et al.: A case in which hepatic artery embolization was useful for portal hypertension associated with diffuse intrahepatic arterioportal shunt. The 111th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2019/10/5
- Yuki Okubo et al.: A case of gastric metastasis of hepatocellular carcinoma diagnosed by hemorrhage. The 111th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2019/10/5
- Morita, A.: Endoscopic medical diagnosis and treatment in the gastrointestinal tract. The 64th Annual Meeting of the Japanese Society of Oral and Maxillofacial Surgeons, Hokkaido, 2019/10/27
- Yukari Tanaka: A case study of liver injury caused by immune checkpoint inhibitors in our hospital. The 43rd Western Society of the The Japan Society of Hepatology, Shimonoseki, 2019/12/12
- Kazuya Hosoya et al.: A study on the significance of the second look in patients taking antithrombotic drugs. The 103rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, January 18, 2020
- Shinsuke Akiyama et al.: Current status of EMR for superficial non-papillary duodenal epithelial tumors in our hospital. The 103rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, January 18, 2020
- Yuki Okubo et al.: Two cases of gastric metastasis of hepatocellular carcinoma diagnosed by bleeding. The 103rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, January 18, 2020
- Toda Jun et al.: A case of intestinal follicular lymphoma with various endoscopic images. The 103rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, January 18, 2020
- Shuichiro Karawatari et al.: A case of ESD for a lesion diagnosed as AIN (anal intraepitheerial neoplasia) by NBI magnifying observation. The 103rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, January 18, 2020
- Shigesato, N. et al.: A case of eosinophilic gastroenteritis with discrepancy between endoscopic and pathological findings. The 103rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, January 18, 2020
- Soichiro Nagao et al.: A case in which a rendezvous method using a percutaneous cholangioscopy and a single endoscope (SBE) was useful for complete enterojejunal anastomotic obstruction. The 103rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, January 18, 2020
- Tomoya Ueda et al.: A case in which electrohydraulic shock wave lithotripsy (EHL) under transoral cholangioscopy was useful for Mirizzi syndrome. The 103rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, January 18, 2020
- Daiki Fumihara et al.: A case of NET-G3 with pancreatic and bile duct dilatation, which was difficult to diagnose preoperatively. The 103rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, January 18, 2020
- Satoko Inoue: Our hospital experience with tofacitinib for ulcerative colitis. The 112th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 29, 2020
- Suginoshita, Y. et al.: The 112th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology. Kyoto, 2020/2/29
- Zheng, Hao et al.: Strategy for treatment of advanced hepatocellular carcinoma with molecular-targeted drugs based on the therapeutic effect of sorafenib. The 112th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 29, 2020
- Yuki Okubo et al.: Clinical and imaging characteristics of TS1 pancreatic cancer in our hospital. The 112th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 29, 2020
- Daiki Fumihara et al.: Two cases of advanced hepatocellular carcinoma that progressed rapidly after discontinuing lenvatinib. The 112th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 29, 2020
- Shigesato, N. et al.: A case of PBC-AIH overlap syndrome with metachronous pathology of PBC/AIH. The 112th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 29, 2020
- Tomoya Ueda et al.: A case in which electrohydraulic shock wave lithotripsy (EHL) under the oral biliary tract was useful for relieving basket incarceration. The 112th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 29, 2020
- Masaya Wada et al.: Is somatostatin receptor scintigraphy useful in diagnosing pancreatic endocrine tumors? . The 112th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 29, 2020
- Urano, N. et al.: (Additional remarks) Oral resection of oropharyngeal and hypopharyngeal carcinomas in the elderly. The 112th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 29, 2020
- Toda, J. et al.: Four cases of fissure tapeworm in the Japan Sea experienced at our hospital. The 112th Regular Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 29, 2020
- Ueno Y: CORRELATION BETWEEN ENDOSCOPIC FEATURES AND HISTOLOGICAL SUBTYPES OF SMALL INTESTINAL LYMPHOMAS ESGE2019, Prague, April 5, 2019
- Morita S: Endoscopic Subepithelial Dissection for Superficial Pharyngeal Cancer: A Case Series of 44 Superficial Cancers. ESGE2019, Prague, 2019/4/5
- Toyonaga H et al.: Traumatic bile duct neuroma diagnosed by boring biopsy with cholangioscopy. Gastrointestinal EndoscopyVolume87, Issue 5, p1361–1362, May2018(published online 2017/11/1),2018/5/1
- Taniguchi Y et al.: A study of TS1 pancreatic cancer in our hospital. The 104th Annual Meeting of the The Japanese Society of Gastroenterology, Tokyo, April 20, 2018
- Taniguchi, Y. et al.: Investigation of Metallic stent placement in the bile duct for malignant biliary stricture. The 95th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 10, 2018
- Inoue T. et al.: Results of local excision for superficial or hypopharyngeal carcinoma. The 95th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 10, 2018
- Okubo, Y. et al.: Usefulness of balloon endoscopy in diagnosis of Meckel's diverticulum. The 95th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 10, 2018
- Satoko Inoue et al.: Endoscopic balloon dilatation for small bowel and colonic strictures. The 95th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 10, 2018
- Fumihara, D. et al.: Pathological diagnosis ability of EUS-FNA for autoimmune pancreatitis in our hospital. The 95th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 11, 2018
- Masashi Fukushima et al.: Current status of emergency balloon endoscopy for gastrointestinal bleeding in our hospital. The 95th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 11, 2018
- Wada, M. et al.: Usefulness of EUS placement as a gold marker placement method for pancreatic cancer moving body-tracking intensity-modulated radiotherapy. The 100th Kinki Branch Regular Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 26, 2018
- Urano, N. et al.: Handling of antithrombotic drugs in gastric ESD. The 100th Kinki Branch Regular Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 26, 2018
- Takahiro Inoue et al.: Treatment results of colorectal ESD using a traction clip, and the experience of using the same clip in ESD beginners. The 100th Kinki Branch Regular Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 26, 2018
- Yukari Ueno et al.: Investigation of 4 cases of gastric metastasis of breast cancer experienced at our hospital. The 100th Kinki Branch Regular Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 26, 2018
- Toyonaga, H. et al.: Pre- and post-onset findings in gastric lesions of Cronkhite Canada syndrome. The 100th Kinki Branch Regular Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 26, 2018
- Ikeda, Y. et al.: A study of 3 cases of ischemic enteritis experienced at our hospital. The 100th Kinki Branch Regular Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 26, 2018
- Yuki Okubo et al.: A case of multiple inflammatory CAP polyp in the small intestine that could be stopped by balloon endoscopy. The 100th Kinki Branch Regular Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 26, 2018
- Fumihara, D. et al.: A case of ruptured pseudoaneurysm after fully covered metallic stent placement for papillary hemorrhage. The 100th Kinki Branch Regular Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 26, 2018
- Naoki Aoyama et al.: A case of pancreatic duct malunion with marked main pancreatic duct dilatation for which pancreatoscopy was useful for diagnosis. The 100th Kinki Branch Regular Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 26, 2018
- Haohang Chung et al.: Two cases of sequential therapy with Peg-INFα2a for low levels of HBs antigen and core-related antigen during administration of nucleic acid analogues. The 54th Annual Meeting of the The Japan Society of Hepatology, Osaka, 2018/6/14
- Yoshiki Suginoshita et al.: Efforts of our hospital for hepatitis C virus (HCV) antibody-positive cases. The 54th Annual Meeting of the The Japan Society of Hepatology, Osaka, 2018/6/14
- Inoue T. et al.: Examination of treatment results of colorectal ESD in beginners. The 109th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2018/9/29
- Zheng, H. et al.: A study of carcinogenesis after DAA treatment for hepatitis C in our hospital. The 109th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2018/9/29
- Taniguchi Y et al.: Use of preoperative full covered metallic stent for malignant biliary stricture. The 109th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2018/9/29
- Daiki Fumihara et al.: A case in which lenvatinib was effective for hepatocellular carcinoma refractory to sorafenib and regorafenib. The 109th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2018/9/29
- Yukari Ueno et al.: A case of olmesartan-related sprue-like bowel disease diagnosed by double-balloon endoscopy. The 109th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2018/9/29
- Toyonaga, H. et al.: A case of intestinal Behcet's disease with trisomy8-positive myelodysplastic syndrome, which repeatedly caused major problems. The 109th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2018/9/29
- Ikeda, Y. et al.: A study of acute hepatitis E in our hospital over the past 8 years. The 109th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2018/9/29
- Yuki Okubo et al.: A case of small bowel perforation due to peritoneal metastasis after surgery for small bowel cancer. The 109th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2018/9/29
- Naoki Aoyama et al.: A case of metastatic pancreatic tumor diagnosed by EUS-FNA during lung adenocarcinoma treatment. The 109th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2018/9/29
- Yoshiki Suginoshita: Opening up the future of ultrasound. The 45th Kansai Regional Scientific Meeting of the The Japan Society of Ultrasonics in Medicine, Kobe, 2018/10/20
- Haohang Chung: Opening up the future of ultrasound. The 45th Kansai Regional Scientific Meeting of the The Japan Society of Ultrasonics in Medicine, Kobe, 2018/10/20
- Naoki Aoyama et al.: Imaging findings of 50 cases of pancreatic neuroendocrine tumor (PNET) in our hospital. JDDW2018, Kobe, 2018/11/3
- Wada, M. et al.: Ingenuity of endoscopic ultrasonographic sewage cyst drainage (EUS-CD) for peripancreatic fluid retention in our hospital. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Urano, N. et al.: ESD of remnant stomach cancer -excision along the suture line-. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Inoue T. et al.: Endoscopic approach to early diagnosis of pharyngeal cancer in our hospital. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Aoyama, Naoki et al.: A case of non-specific multiple small intestinal ulcers diagnosed due to repeated intestinal obstruction. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Fumihara, D. et al.: Two cases of small intestinal NET. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Yuka Ikeda et al.: Four cases of metastasis of lung cancer to the small intestine experienced at our hospital. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Yukari Ueno et al.: A case of a dialysis patient with deposition of lanthanum carbonate in the gastric mucosa. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Yuki Okubo et al.: Usefulness of double-balloon endoscopy in diagnosis of small bowel cancer. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Tomoya Ueda et al.: A case of multiple metastases to the stomach, duodenum, and large intestine 21 years after surgery for breast cancer. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Toyonaga, K. et al.: A case of pancreatic malignant lymphoma with duodenal obstruction. The 101st Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2018/11/10
- Masashi Fukushima et al.: A study of olmesartan-related sprue-like intestinal disease experienced at our hospital. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Taniguchi, Y. et al.: Current status of treatment of pancreatic neuroendocrine tumors (PNET) at our hospital. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Zheng, H. et al.: A case study of regorafenib administration for advanced hepatocellular carcinoma in our hospital. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Toyonaga, H. et al.: A case of mantle cell lymphoma with multiple lymphomatous polyposis in the pharynx, esophagus, and large intestine. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Yuki Okubo et al.: A case in which endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) was useful in diagnosing malignant pyloric stenosis. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Yukari Ueno et al.: Usefulness of double-balloon endoscopy in the diagnosis of malignant lymphoma of the small intestine. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Aoyama, Naoki et al.: A case of ileal arteriovenous malformation treated by IVR. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Ikeda, Y. et al.: A case of recurrence of hepatitis C with severe jaundice after living-donor liver transplantation in which SOF/LDV was successful. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Daiki Fumihara et al.: A study on the efficacy of tolvaptan treatment for refractory ascites in our hospital. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Hirai, T. et al.: Single resection case of intrabiliary papillary tumor. The 110th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Kyoto, February 23, 2019
- Taniguchi Y: Intraductal vs. transpapillary fully covered self-expandable metal sent placement for malignant biliary stricture. DDW2018,Washington, DC,2018/6/2-5
- Okubo Y et al.: Usefulness of double-balloon enteroscopy for diagnosis of Meckel's diverticulum. UEG2018, Vienna, 2018/10/20-24
- Toyonaga H et al.: Preoperative biliary drainage using plastic stents versus self-expandable metal stents for periampullary cancer. UEG2018, Vienna, 2018/10/20-24
- Fukushima M: Investigation of cases of obscure gastrointestinal bleeding and small bowel bleeding that led to rebleeding. Gastro2018, Bangkok, 2018/12/5-8
- Hatamori H, Wada M, Taniguchi Y, Inokuma T: Pancreatic pseudocyst localized in the gastric wall after EUS-guided FNA of type 1 autoimmune pancreatits.Gastrointestinal Endoscopy Vol.86 Issue5 P919-921,2017/6/2
- Ogawa S , Imai Y , Inokuma T : Mimicking Gastric Natural Killer/T-Cell Lymphoma . Gastroenterology Vol.153 Issue1 e22-e23,2017/6/2
- Toyonaga H, Masashi F, Inokuma T, Imai Y: Mantle cell lymphoma involving the esophagus evaluated by magnifying endoscopy with narrow-band imaging.Gastrointestinal Endoscopy Volume87 Issue1 P305-306,January2018,published online 2017/7/15
- Toyonaga H, Taniguchi Y, Inokuma T: Traumatic bile duct neuroma diagnosed by boring biopsy with cholangioscopy . Gastrointestinal Endoscopy Volume87 Issue 5 P1361 – 1362, May2018, published online 2017/11/1
- Toyonaga H, Morita S, Inokuma T, Ezoe Y (Ishikawa Gastrienterology Clinic):Cricoid pressure to prevent gastric deflation during esophagogastroduodenoscopy.VIDEOGIE Volume3 Issue3 P102-105,March2018,published online 2017/12/12
- Yohei Taniguchi: Experience of using EZ Shot 3 plus with coiled sheath for pancreatic neoplastic lesions. The 103rd Annual Meeting of the The Japanese Society of Gastroenterology, Tokyo, April 22, 2017
- Shuko Morita: Poster Venue 3 (Event Hall, 3rd Floor, Osaka International Conference Hall) Poster 14 Stomach-Hemorrhage after ESD. The 93rd Annual Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 11, 2017
- Taniguchi Y,Wada M,Inokuma T:Cross-wired metallic stents for bilateral endoscopic stent placement for malignant hilar biliary obstruction. Inokuma T: Cross-wired metallic stents for bilateral endoscopic stent placement for malignant hilar biliary obstruction.) The 93rd Japan Gastroenterological Endoscopy Society General Meeting, Osaka, 2017/5/11
- Masashi Fukushima, Satoko Inoue, Tetsuro Inokuma: [Additional comments] Examination of cases of unexplained gastrointestinal bleeding and small intestinal bleeding with rebleeding. The 93rd Annual Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 11, 2017
- Urano, N. ESD for gastric cancer in elderly over 80 years old. The 93rd Annual Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 11, 2017
- Naoki Aoyama, Naoto Urano, Yuki Okubo, Daiki Fumihara, Keisho Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: A case study of upper gastrointestinal endoscopic foreign body removal cases in our hospital. The 93rd Annual Meeting Japan Gastroenterological Endoscopy Society, Osaka, May 11, 2017
- Keito Toyonaga, Yohei Taniguchi, Naoki Aoyama, Kei Okumura, Hiroyuki Hatamori, Takuhiko Ito, Kazuhiro Matsumoto, Hiroki Kitamoto, Masashi Fukushima, Naoto Urano, Shuko Morita, Satoko Inoue, Masaya Wada, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: Investigation of therapeutic results and safety of the OTSC system for gastrointestinal perforation and fistula. The 93rd Annual Meeting Japan Gastroenterological Endoscopy Society, Osaka, May 11, 2017
- Masaya Wada, Yohei Taniguchi, Naoki Aoyama, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takuhiko Ito, Kazuhiro Matsumoto, Hiroki Kitamoto, Masashi Fukushima, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Yukihiro Imai, Tetsuro Inokuma: Results of EUS-FNA for metastatic pancreatic tumor in our hospital. The 93rd Annual Meeting Japan Gastroenterological Endoscopy Society, Osaka, May 11, 2017
- Hiroyuki Hatamori, Masashi Fukushima, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Hiroto Toyonaga, Kei Okumura, Takahiro Inoue, Yohei Taniguchi, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: Evaluation of usefulness and safety of ERCP under emergency double balloon endoscopy. The 93rd Annual Meeting Japan Gastroenterological Endoscopy Society, Osaka, May 12, 2017
- Morita A, Arano N, Inokuma T: Prognostic study in patients aged 80 years or older who underwent endoscopic submucosal dissection for early gastric cancer. The 93rd Annual Meeting of the Japan Gastroenterological Endoscopy Society, Osaka, May 2017 /12
- Hiroshi Tei, Suginoshita Y., Taniguchi Y., Fukushima M., Wada M., Inokuma T.: Treatment effect of DAAs for genotype 1 type C liver cirrhosis in our hospital. The 53rd Annual Meeting The Japan Society of Hepatology, Hiroshima, 2017 /6/8- 6/9
- Urano N, Fukushima M, Fukushima S, Morita S, Morita T, Inokuma T, Imai Y: Japan Gastroenterological Endoscopy Society resection of pharyngeal tumor in our hospital.
- Masaya Wada, Yohei Taniguchi, Tetsuro Inokuma: Current status of diagnostic EUS-FNA for pancreatic disease in our hospital.
- Hatamori H, Taniguchi Y, Fukushima M, Wada M, Inokuma T: Usefulness and safety of double-balloon endoscopy EPLBD in cases of common bile duct stones in postoperative reconstructed intestinal tract. The 98th Japan Gastroenterological Endoscopy Society Kinki Branch Meeting, Kobe, 2017/6/17
- Keito Toyonaga, Naoto Urano, Naoki Aoyama, Kei Okumura, Hiroyuki Hatamori, Takuhiko Ito, Kazuhiro Matsumoto, Hiroki Kitamoto, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshi, Tetsuro Inokuma, Keiichiro Uehara: A case of methotrexate-associated Japan Gastroenterological Endoscopy Society disease.
- Naoki Aoyama, Masashi Fukushima, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takuhiko Ito, Kazuhiro Matsumoto, Hiroki Kitamoto, Yohei Taniguchi, Masaya Wada, Shuko Morita, Naoto Urano, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma, Keiichiro Uehara: A case of sprue-like intestinal disease thought to be caused Japan Gastroenterological Endoscopy Society
- Kei Okumura, Satoko Inoue, Naoki Aoyama, Hiroto Toyonaga, Hiroyuki Hatamori, Takuhiko Ito, Kazuhiro Matsumoto, Hiroki Kitamoto, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Shuko Morita, Naoto Urano, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: A case of small-Japan Gastroenterological Endoscopy Society T cell lymphoma that was difficult to diagnose and progressed rapidly.
- Yuki Okubo, Naoto Urano, Daiki Fumihara, Naoki Aoyama, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma, Yukihiro Imai: Two cases of duodenal Brunner adenocarcinoma resected by Japan Gastroenterological Endoscopy Society
- Takahiro Inoue, Yohei Taniguchi, Kazuhiro Matsumoto, Naoki Aoyama, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Hiroshi Tei, Satoko Inoue, Yoshiki Suginoshi , T. Inokuma: A case of pancreatic pseudocyst with perforation of the portal vein for which Japan Gastroenterological Endoscopy Society was useful. 17
- Daiki Fumihara, Shuko Morita, Yuki Okubo, Naoki Aoyama, Hiroto Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Naoto Urano, Satoko Inoue, Hiroshi Chung, Yoshiki Suginoshi, Tetsuro Inokuma, Satoshi Kaihara: Two cases of Japan Gastroenterological Endoscopy Society fistula.
- Yoshiro Katayama, Masaya Wada, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: 4 cases of Japan Gastroenterological Endoscopy Society NET -examination of treatment experience at our hospital-. /17
- Shuko Morita: Current status and possibility of endoscopic full-thickness gastrectomy.ENDOSCOPY FORUM JAPAN 2017, Otaru, August 5-6, 2017
- Suginoshita Y, Hiroshi Tei, Wada M, Inokuma T: Investigation of DAAs therapeutic effects on genotype 1b hepatitis C and post-treatment The Japanese Society of Gastroenterology carcinoma cases. Osaka, September 23, 2017
- Masaya Wada, Yohei Taniguchi, Tetsuro Inokuma, Toshiyuki The Japanese Society of Gastroenterology: EUS Shimogane marker implantation for dynamic tracking IMRT for locally advanced unresectable pancreatic cancer. /twenty three
- Kei Okumura, Yoshiki Suginoshita, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Hiroto Toyonaga, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue , Hiroshi Tei, T. Inokuma: Investigation of efficacy of tolvaptan for refractory ascites in our hospital. The 107th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, September 23, 2017.
- Daiki Fumihara, Yohei Taniguchi, Yuki Okubo, Naoki Aoyama, Hiroto Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshi, Tetsuro Inokuma: A case in which placement of a fully covered self-expandable metallic stent was useful for postoperative The Japanese Society of Gastroenterology fistula.
- Naoki Aoyama, Masashi Fukushima, Yuki Okubo, Daiki Fumihara, Keisho Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma, Yukihiro Imai: A study on small intestinal follicular lymphoma in our hospital. The 107th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, September 23, 2017
- Yuki Okubo, Masashi Fukushima, Daiki Fumihara, Naoki Aoyama, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: Usefulness of balloon endoscopy in diagnosis of Meckel's diverticulum. The 107th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, September 23, 2017
- Shogo Shirota, Satoko Inoue, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: A juvenile-onset jejunal artery aneurysm with repeated massive bleeding and useful small-intestinal endoscopy. The 107th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, September 2017. /twenty three
- Masashi Fukushima, Satoko Inoue, Tetsuro Inokuma: Clinical features of orsalmethane-associated sprue-like enteropathy. JDDW2017, Fukuoka, 2017/10/13
- Taniguchi Y, Aoyama N, Toyonaga K, Okumura K, Hatamori H, Fukushima M, Wada M, Urano N, Morita S, Inoue S, Hiroshi Tei, Suginoshishita Y, Inokuma T: In our hospital Current status of pancreatic cancer treatment.JDDW2017, Fukuoka, 2017/10/14
- Shuko Morita: Panel discussion 1 (Second venue, East building, 3F, large conference room) Long-term prognosis of early-stage cancer with non-curative Japan Gastroenterological Endoscopy Society.
- Yohei Taniguchi: Liver/pancreas (6th venue, East building, 2nd floor, Japan Gastroenterological Endoscopy Society training room).
- Yohei Taniguchi, Masaya Wada, Tetsuro Inokuma: Clinical and imaging characteristics of Japan Gastroenterological Endoscopy Society pancreatic cancer in our hospital.
- Inoue T, Morita A, Japan Gastroenterological Endoscopy Society N, Inokuma T, Maeda K: Long-term prognosis of superficial or hypopharyngeal carcinoma treated with local excision at our hospital. Branch regular meeting,Kyoto,2017/11/18
- Keito Toyonaga, Masashi Fukushima, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: A case of Japan Gastroenterological Endoscopy Society hiatal hernia presenting with upside-downstomach.
- Yuki Okubo, Yohei Taniguchi, Daiki Fumihara, Naoki Aoyama, Hiroto Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: Two cases of breast cancer metastasis with obstruction and Japan Gastroenterological Endoscopy Society diagnosed.
- Kei Okumura, Naoto Urano, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Hiroto Toyonaga, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: A case of Kaposi Japan Gastroenterological Endoscopy Society of the stomach and large intestine followed by treatment.
- Naoki Aoyama, Masaya Wada, Yuki Okubo, Daiki Fumihara, Keisho Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma, Yukihiro Imai: A case of gastric glomus tumor diagnosed preoperatively by Japan Gastroenterological Endoscopy Society-FNA.
- Satoko Inoue, Masashi Fukushima, Tetsuro Inokuma: Efficacy and limitations of Japan Gastroenterological Endoscopy Society balloon dilatation for Crohn's disease.
- Hiroyuki Hatamori, Yohei Taniguchi, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Hiroto Toyonaga, Kei Okumura, Takahiro Inoue, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: Successful placement of a fully covered self-expandable metal stent for refractory biliary jejunal anastomotic stenosis. /11/18
- Daiki Fumihara, Satoko Inoue, Yuki Okubo, Naoki Aoyama, Hiroto Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: Two cases of Japan Gastroenterological Endoscopy Society malformation of the large intestine that were not diagnosed by the first endoscopy.
- Tomoya Ueda, Naoto Urano, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: A case of small intestinal anisakiasis for which abdominal ultrasonography (US) was useful for diagnosis. The 99th Annual Meeting of the Kinki Branch Japan Gastroenterological Endoscopy Society, Kyoto, 2017 /11/18
- Urano, N., Fukushima, M., Morita, A., Inokuma, T.: A study of ESD non-curative resection cases of gastric cancer in our hospital.
- Masashi Fukushima, Satoko Inoue, Tetsuro Inokuma, Yukihiro Imai: Diagnosis and clinical features of malignant tumors of the small intestine in our hospital. The 108th regular meeting of the Kinki branch of the Japanese Society of Gastroenterology, Kyoto, March 17, 2018
- Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: DAA The Japanese Society of Gastroenterology results for hepatitis C in our hospital and SVR subsequent carcinoma.
- Yuki Okubo, Yohei Taniguchi, Daiki Fumihara, Naoki Aoyama, Hiroto Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: A case of biliary bleeding after placement of a metal stent in malignant biliary stenosis.The 108th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, March 17, 2018.
- Keito Toyonaga, Masashi Fukushima, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma: A case of small intestinal GIST requiring emergency surgery for bleeding control.The 108th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, March 17, 2018.
- Daiki Fumihara, Yoshiki Suginoshita, Yuki Okubo, Naoki Aoyama, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue , Hiroshi Tei, T. Inokuma: A case of autoimmune hepatitis after treatment with a direct-acting antiviral (DAA) for chronic hepatitis C. The 108th regular meeting of The Japanese Society of Gastroenterology Kinki Branch, Kyoto, March 2018/ 17
- Naoki Aoyama, Yohei Taniguchi, Yuki Okubo, Daiki Fumihara, Keisho Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Satoko Inoue, Hiroshi Tei, Yoshiki Suginoshita, Tetsuro Inokuma, Yukihiro Imai: A case of NEC (neuroendocrine carcinoma) for which EUS-FNA was useful in differentiating from common pancreatic duct cancer. The 108th regular meeting of the Kinki branch of the Japanese Society of Gastroenterology, Kyoto, 2018 /3/17
- Shuichiro Karawatari, Satoko Inoue, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Hiroto Toyonaga, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Hiroshi Tei, Sugiyuki Yoshiki Shimo, Tetsuro Inokuma: Two cases of localized upper gastrointestinal amyloidosis. The 108th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, March 17, 2018.
- Soichiro Nagao, Satoko Inoue, Yuki Okubo, Daiki Fumihara, Naoki Aoyama, Keito Toyonaga, Kei Okumura, Hiroyuki Hatamori, Takahiro Inoue, Yohei Taniguchi, Masashi Fukushima, Masaya Wada, Naoto Urano, Shuko Morita, Hiroshi Tei, Suginoshita Y., Inokuma T.: Two cases of ileal endometriosis with ileus. The 108th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Kyoto, March 17, 2018.
- Taniguchi Y: CROSS-WIRED METALLIC STENTS IN ENDOSCOPIC BILATERAL STENT-IN- STENT PLACEMENT FOR MALIGNANT HILAR BILIARY OBSTRUCTION.DDW2017, Chicago, May 9, 2017
- HatamoriH,FukushimaM,InokumaT:Efficacyandsafetyofurgentdoubleballoonenteroscopy-assisted endoscopic retrograde cholangiopancreatography.APDW2017,Hong Kong,2017/9/23-26
- InoueT,TaniguchiY,InokumaT:Endoscopicpapillarylargeballoondilationforlargeormultiple common bile duct stones: efficacy, safety, and stone recurrence.APDW2017,Hong Kong, 2017/9/23-26
- Taniguchi Y, Inokuma T:APDW2017.Hong Kong,2017/9/25,Toyonaga H,Taniguchi Y, Inokuma T:Treatment results and safety of over-the-scope-clip system for gastrointestinal tract perforations and fistulas.APDW2017,Hong Kong ,2017/9/25
- Toyonaga H, Taniguchi Y, Wada M, Inokuma T: Unilateral versus bilateral stent-in-stent placement of metal stents for malgnant hilar biliary obstruction.UEG2017, Barcelona, 2017/10/28-11/1
- Fukushima, M. et al.: A case of olmesartan-associated sprue-like enteropathy. Stomach and intestine Vol.51 No.4 P497-502,2016/4/25
- Minamide, R. et al.: A case of multiple pancreatic neuroendocrine tumors associated with von Hippel-Lindau disease. Pancreas Vol.31 No.2 P150-157,2016/4/25
- Kitamoto, H. et al.: A case of gastric submucosal hematoma during percutaneous endoscopic gastrostomy and complication of bumper burial syndrome in the early postoperative period.Home medical care and endoscopic treatment vol.20 No.1,2016 /9/1
- Takuhiko Ito et al.: A case of anal squamous cell carcinoma that was diagnosed as early-stage anal squamous cell carcinoma by NBI magnifying observation.
- Morita, A. et al.: Esophageal and Barrett's esophageal case atlas 5 Superficial esophageal cancer (0-IIa+IIc). NBI/BLI/LCI endoscopy atlas based on new diagnostic criteria and classification, 1st edition, 1st printing, Japan. Medical Center (Tokyo), 2016/10/20
- Ito T et al.: The prospect of endoscopic submucosal dissection for early anal canal squamous cell carcinoma.Clinical Journal of Gastroenterology Vol.9 Issue6 P384-388,2016/12/1
- Hiroyuki Hatamori et al.: A case in which a balloon catheter with a side hole was useful in endoscopic duodenal stent placement for malignant gastroduodenal stenosis with gallbladder-duodenal fistula. Gastrological Endoscopy Vol.59(1), 2017/1 /twenty five
- Hiroshi Tei al.: Results of combination therapy with daclatasvir and asunaprevir in our hospital. The 102nd Annual Meeting of the Japanese Society of Gastroenterology, Tokyo, April 21, 2016
- Satoko Inoue: A study of 3 patients with ulcerative colitis who were successfully treated with anti-TNF-α antibody as third line therapy. The 102nd Annual Meeting of the The Japanese Society of Gastroenterology, Tokyo, April 21, 2016
- Yohei Taniguchi et al.: Endoscopic papillary sphincterectomy (EST) + large diameter balloon dilatation (EPLBD) in our hospital. The 102nd Annual Meeting of the The Japanese Society of Gastroenterology, Tokyo, April 23, 2016
- Kei Okumura et al.: Examination of the eradication rate of Helicobacter pylori in our hospital. The 102nd Annual Meeting of the The Japanese Society of Gastroenterology, Tokyo, April 23, 2016
- Kitamoto, H. et al.: A case study of percutaneous endoscopic gastrostomy in elderly patients at our hospital. The 91st Annual Meeting of the Japanese Gastroenterological Endoscopy Society, Tokyo, May 12, 2016
- Hatamori, H. et al.: Clinical study of 51 cases of volvulus sigmoid colon in our hospital. The 91st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 12, 2016
- Masashi Fukushima: A strategy for diagnosing malignant tumors of the small intestine in our hospital. The 91st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 13, 2016
- Yohei Taniguchi: Endoscopic ultrasound-guided fine-needle aspiration from the lower gastrointestinal tract (EUS-FNA).The 91st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 13, 2016
- Takuhiko Ito et al.: Investigation of the usefulness of stent placement therapy for Gastric Outlet Obstruction (GOO) caused by malignant tumors in our hospital. The 91st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 13, 2016
- Kazuhiro Matsumoto et al.: A case study of colonic stent placement in our hospital. The 91st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 13, 2016
- Shuko Morita: Hands-on 4 gastric ESD by a female preceptor. The 91st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 14, 2016
- Kitamoto H et al.: Clinical features of Cytomegalovirus enterocolitis (Study of cases of CMV enterocolitis in our hospital). The 91st Annual Meeting of the Japan Gastroenterological Endoscopy Society, Tokyo, May 14, 2016
- Masaya Wada et al.: Treatment results of sofosvir/ribavirin combination therapy for genotype 2 chronic hepatitis C and cirrhosis in our hospital. The 52nd Annual Meeting of the The Japan Society of Hepatology, Chiba, May 19, 2016
- Kitamoto, H. et al.: Endoscopic approach to small bowel malignant tumor in our hospital. The 96th branch meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Kyoto, June 11, 2016
- Naoto Urano et al.: Approach to gastric corpus greater curvature ESD in our hospital. The 96th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Kyoto, June 11, 2016
- Naoki Aoyama et al.: A case of esophageal GIST observed and diagnosed endoscopically. Japan Gastroenterological Endoscopy Society Kinki Branch 96th Branch Regular Meeting, Kyoto, June 11, 2016
- Ito T. et al.: A case of gastric glomus tumor that was difficult to control and was resected laparoscopically.The 96th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Kyoto, June 11, 2016
- Hiroyuki Hatamori et al.: A case of mild intestinal strongyloidiasis with endoscopic confirmation.The 96th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Kyoto, June 11, 2016
- Kei Okumura et al.: Study of EBL (Endoscopic Band Ligation) for colonic diverticular hemorrhage in our hospital. The 96th regular meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Kyoto, June 11, 2016
- Kazuhiro Matsumoto et al.: A case of Choledochocele.The 96th regular meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Kyoto, June 11, 2016
- Hironori Kitamoto: Study on recurrence of cytomegalovirus enteritis associated with ulcerative colitis. The 7th Annual Meeting of the Japanese Association for Inflammatory Bowel Disease, Kyoto, July 10, 2016
- Hironori Kitamoto: A study of percutaneous endoscopic gastrostomy for acute onset of dysphagia. The 21st Annual Meeting of PEG and Home Medical Research Society, Takamatsu, September 3, 2016
- Kitamoto, H. et al.: Side effects and optimization of thiopurine preparations. The 105th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2016/9/17
- Hiroshi Tei al.: Results of daclustervir + asunaprevir combination therapy in our hospital. The 105th regular meeting of the Kinki branch The Japanese Society of Gastroenterology, Osaka, September 17, 2016
- Yohei Taniguchi et al.: Stentinstent by using BONASTENTM-Hilar for unresectable malignant perihilar biliary stenosis.The 105th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2016/9/17
- Toyonaga, K. et al.: A case of Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis with acute liver failure. The 105th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, September 17, 2016
- Kei Okumura et al.: Ascites filtration and concentrated The Japanese Society of Gastroenterology therapy (CART) for refractory ascites in patients with cirrhosis.
- Hatamori, H. et al.: A case of pancreatic fistula with a specific morphology after EUS-FNA for autoimmune pancreatitis.The 105th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2016/9/17
- Ito, T. et al.: A case of gastrointestinal pancreas found in blood and diagnosed by EUS-FNA. The 105th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, September 17, 2016
- Naoki Aoyama et al.: Three cases of type II enteropathy-associated T-cell lymphoma (ESTL) followed up by small intestinal endoscopy.The 105th meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, September 17, 2016
- Matsumoto, K. et al.: A case of ruptured duodenal varices treated with endoscopic sclerotherapy. The 105th meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, September 17, 2016
- Masaya Wada et al.: A study of narrowly defined congenital biliary dilatation in our hospital. The 52nd Annual Meeting of the The Japan Biliary Association, Yokohama, September 30, 2016
- Arano, N. et al.: Study of non-ESD gastric cancer cases in our hospital. JDDW2016, Kobe, 2016/11/3
- Satoko Inoue et al.: Clinical features of eosinophilic gastroenteritis in our hospital. JDDW2016, Kobe, 2016/11/4
- Yohei Taniguchi et al.: Self-expandable metallic stent (SEMS) for non-resectable hilar biliary stenosis in our hospital. JDDW2016, Kobe, 2016/11/5
- Masaya Wada et al.: Study of EUS-FNA complications in our hospital. JDDW2016, Kobe, 2016/11/5
- Naoto Urano et al.: ESD for early gastric cancer in the elderly. The 97th branch meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Kyoto, November 26, 2016
- Morita S et al:[Additional remarks] A study of esophageal cancer cases difficult to be picked up -A study of esophageal cancer cases in our hospital that were performed upper gastrointestinal endoscopy within the past 2 years but could not be pointed out-. Japan Gastroenterological Endoscopy Society The 97th Regular Meeting of Kinki Branch, Kyoto, 2016/11/26
- Masaya Wada et al.: Current status of EUS-FNA for pancreatic cancer in our hospital. Japan Gastroenterological Endoscopy Society Kinki Branch 97th Branch Regular Meeting, Kyoto, November 26, 2016
- Kazuhiro Matsumoto et al.: A case of listerial bacteremia with esophageal cancer as the entry point. The 97th branch regular meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Kyoto, November 26, 2016
- Takuhiko Ito et al.: A case of gastric leiomyoma that was surgically resected due to severe bleeding.The 97th regular meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Kyoto, November 26, 2016
- Naoki Aoyama et al.: A case of whipworm that was accidentally discovered and removed during lower gastrointestinal endoscopy. The 97th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Kyoto, November 26, 2016
- Hiroyuki Hatamori et al.: A case of dedifferentiated liposarcoma that was difficult to diagnose by EUS-FNA. The 97th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Kyoto, November 26, 2016
- Kei Okumura et al.: A case of malignant lymphoma of the small intestine discovered after massive bleeding.The 97th regular meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Kyoto, November 26, 2016
- Kitamoto, H. et al.: A case of lymphomatoid gastropathy with endoscopic follow-up. The 97th branch meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Kyoto, November 26, 2016
- Hiroto Toyonaga et al.: A case of bile duct stump neuroma for which observation by cholangioscopy (SpyGlassTMDS) and biopsy were useful for diagnosis. Japan Gastroenterological Endoscopy Society Kinki Branch 97th Branch Regular Meeting, Kyoto, 2016/ 11/26
- Yohei Taniguchi et al.: Experience of using EZShot3plus for pancreatic tumor.The 106th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 25, 2017
- Kitamoto, H. et al.: A case of endoscopic treatment for residual pancreatic stones after pyloric ring-preserving pancreatoduodenectomy of the entire stomach. The 106th meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 25, 2017
- Kei Okumura et al.: A case of gastrointestinal amyloidosis associated with acutely advanced rheumatoid arthritis. The 106th regular meeting of the Kinki branch of the Japanese Society of Gastroenterology, Osaka, February 25, 2017
- Naoki Aoyama et al.: A case of duodenal parapapilla neuroendocrine tumor. The 106th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, 2017/2/25
- Hiroyuki Hatamori et al.: A study of volvulus of the sigmoid colon in our hospital. The 106th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 25, 2017
- Toyonaga, H. et al.: Invasive liver abscess syndrome caused by hyperviscous Klebsiella pneumoniae. The 106th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 25, 2017
- Ito T et al.: Predictive Factors for Efficacy of Tolvaptan in Patients With Refractory Ascites in Decompensated Liver Cirrhosis.Digestive Disease Week 2016,San Diego,2016/5/21
- Ito T et al.: The Efficacy of an Endoscopic Self-Expandable Metal Stent for Gastric Outlet Obstruction by Malignancies.Digestive Disease Week 2016,San Diego,2016/5/23
- Taniguchi Y et al.: A Newly Designed Cross-Wired Metallic Stent for Unresectable Malignant Hilar Bile Duct Obstruction.Digestive Disease Week 2016,San Diego,2016/5/24
- KitamotoHetal.:Cytomega1ovirusenterocolitisinpatientswithulcerativecolitis.AOCC2016,Kyoto, 2016/7/7-9
- Matsumoto K et al.: Feasibility and safety of laparoscopic and endoscopic surgery for gastric submucosal tumors .UEG 2016,Vienna Austria,2016/10/15-19
- Hatamori H et al.:Efficacy and safety of urgent double balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography.UEG 2016,Vienna Austria,2016/10/15-19
- Morita S:Current status of GI women in Asia.APDW2016,Kobe,2016/11/5
- Kitamoto H et al.:Regorafenib-Induced Hyperammonemic Encephalopathy in Metastatic Colon Cancer.Journal of Cancer Prevention & Current Reseach,Vol.3 No.2 00076,2015/10/19
- Minamide T et al.: A case of arteriovenous malformation of the small intestine treated by endoscopic therapy.GASTROENTEROLOGICAL ENDOSCOPY Vol.57 No.10 P2448-2454,2015/10/29
- Ito T et al.: Gastric metastasis of pancreatic neuroendocrine tumor 5 years after surgical resection of the primary lesion.Digestive Endoscopy Vol.27 No.7 P782,2015/11
- Matsumoto K et al.: Rupture of small intestinal varices treated by endoscopy. GASTROENTEROLOGICAL ENDOSCOPY Vol.57 No.11 P.2519-2523,2015/11/28
- Fukushima M et al.: Severe spruelike enteropathy associated whith olmesartan observed by double-ballon enteroscopy.GASTROINTESTINAL ENDOSCOPY Vol.83 No.1 P269-270,2016/1
- Kitamoto, H. et al.: Small bowel DLBCL examined by small bowel endoscopy at our hospital. The 101st Annual Meeting of the The Japanese Society of Gastroenterology, Sendai, April 23, 2015
- Yohei Taniguchi: A study of acute cholangitis in the elderly in our hospital. The 101st Annual Meeting of the The Japanese Society of Gastroenterology, Sendai, April 23, 2015
- Zheng The Japan Society of Hepatology Hiroshi Tei al.: Post-marketing status and results of simeprevir combination treatment with three drugs -Study at three facilities in our city-.
- Takuhiko Ito et al.: Possibility of ESD treatment for early-stage squamous cell carcinoma of the anal canal. The 89th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Nagoya, May 29, 2015
- Masashi Fukushima et al.: Clinical study of gastrointestinal lesions caused by vasculitis in our hospital. The 89th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Nagoya, May 29, 2015
- Kitamoto, H. et al.: Usefulness of electric dilator for treatment of bile duct-jejunal anastomotic stricture. The 89th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Nagoya, May 29, 2015
- Kitamoto, H. et al.: Current status of stent placement therapy for patients with malignant gastroduodenal stenosis in our hospital. The 89th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Nagoya, May 29, 2015
- Masaya Wada et al.: Results of endoscopic ultrasound-guided pancreatic cyst drainage (US-CD) in our hospital. The 89th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Nagoya, May 30, 2015
- Naoto Urano et al.: ESD for Barrett esophageal cancer. The 89th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Nagoya, May 30, 2015
- Yohei Taniguchi et al.: Treatment of acute cholangitis associated with choledocholithiasis in the elderly and very elderly at our hospital. The 89th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Nagoya, May 30, 2015
- Masaya Wada: Study of EUS-FNA for pancreatic neuroendocrine tumors (PNET) in our hospital. The 46th Annual Meeting of the Japan Pancreas Society, Nagoya, June 20, 2015
- Naoto Urano et al.: Current status of colorectal ESD in our hospital and treatment ideas. The 95th Kinki Branch Annual Meeting of the Japanese Society of Endoscopy, Osaka, June 20, 2015
- Yohei Taniguchi et al.: A study on choledocholithiasis in the elderly in our hospital. The 95th Kinki Branch Annual Meeting of the Japanese Endoscopy Society, Osaka, June 20, 2015
- Kitamoto, H. et al.: A study of a case of percutaneous endoscopic gastrostomy enlargement in our hospital.
- Hiroyuki Hatamori: A case in which the use of a balloon catheter (Bouncer) for calculus removal was useful in a difficult case of duodenal stent placement.The 95th Kinki Branch Meeting of the Japanese Endoscopy Society, Osaka, June 20, 2015
- Kazuya Hosoya et al.: A case of small intestinal NET in which small intestinal endoscopy was useful for preoperative diagnosis.The 95th Kinki Branch Meeting of the Japanese Endoscopy Society, Osaka, June 20, 2015
- Kazuhiro Matsumoto et al.: A case of ischemic enteritis with portal venous gas.The 95th Kinki Branch Annual Meeting of the Japanese Endoscopy Society, Osaka, June 20, 2015
- Kei Okumura et al.: A case of ulcerative colitis (UC) with pneumatosis cystoides intestinalis (PCI).The 95th Kinki branch meeting of the Japan Endoscopy Society, Osaka, 2015/ 6/20
- Masashi Fukushima et al.: A case of olmesartan-associated sprue-like enteropathy. The 95th Kinki Branch Annual Meeting of the Japanese Society of Endoscopy, Osaka, June 20, 2015
- Takuhiko Ito et al.: A case of bile duct cancer found 19 years after surgery for duodenal papillary carcinoma that was successfully cured.
- Kitamoto, H. et al.: Two cases of stage IV intestinal cancer with hepatic encephalopathy during Regorafenib therapy. The 13th Annual Meeting of the Japanese Society of Medical Oncology, Sapporo, 2015/7/16
- Yohei Taniguchi et al.: Effectiveness of endoscopic treatment using an electric dilator for biliary jejunal anastomotic stenosis.The 51st Annual Meeting of the The Japan Biliary Association, Utsunomiya, 2015/9/17-18
- The Japanese Society of Gastroenterology Ito et al.: A case of giant hepatic cyst in which pure ethanol injection therapy was successful.
- Kitamoto, H. et al.: Regarding the relationship between fecal occult blood test-positive cases and colon The Japanese Society of Gastroenterology in our hospital.
- Kei Okumura et al.: A case of acute hepatitis E caused by ingestion of horsemeat. The 103rd Annual Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka, September 26, 2015
- Matsumoto K. et al.: A case of diffuse large B-cell lymphoma (DLBCL) penetrating the duodenum. The 103rd Annual Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka, September 26, 2015
- Ryusuke Minamide et al.: A case of The Japanese Society of Gastroenterology that was successfully treated with cola dissolution and endoscopic lithotripsy.
- Hiroyuki Hatamori et al.: A case of tuberculous lymphadenitis diagnosed with EUS-The Japanese Society of Gastroenterology for mediastinal lymphadenopathy.
- Kazuhiro Matsumoto et al.: Study of ischemic enteritis. JDDW2015, Tokyo, 2015/10/8
- Masashi Fukushima et al.: Current status of emergency ERCP using balloon endoscopy for postoperative bowel reconstruction in our hospital. JDDW2015, Tokyo, 2015/10/8
- Kazuya Hosoya et al.: A study of 33 cases of pancreatic neuroendocrine tumor (PNET) in our hospital. JDDW2015, Tokyo, 2015/10/8
- Tatsunori Minamide et al.: Current status of Laparoscopy and endoscopy cooperative surgery (LECS) for gastric submucosal tumors in our hospital. JDDW2015, Tokyo, October 8, 2015
- Morita, S. et al.: Depth diagnosis of superficial pharyngeal tumor. JDDW2015, Tokyo, 2015/10/9
- Yohei Taniguchi et al.: Clinical features of autoimmune pancreatitis in our hospital and diagnostic ability of E U S – F N A. JDDW2015, Tokyo, 2015/10/9
- Takuhiko Ito et al.: Usefulness of stent placement therapy for gastric outlet obstruction (GOO) associated with malignant tumors in our hospital. JDDW2015, Tokyo, 2015/10/9
- Kei Okumura et al.: Clinical study of cystoid pneumatosis (PCI) -Chronic and fulminant types are the same disease-.JDDW2015, Tokyo, 2015/10/9
- Kitamoto, H. et al.: Usefulness and limitations of emergency capsule endoscopy for gastrointestinal bleeding of unknown cause. JDDW2015, Tokyo, 2015/10/10
- Masaya Wada et al.: Results of EUS-FNA for gastrointestinal submucosal tumors in our hospital.The 95th branch meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Osaka, November 7, 2015
- Tatsunori Minamide et al.: (Additional remarks 2) Current status of laparoscopy and endoscopy cooperative surgery (LECS) for gastric submucosal tumors in our hospital.The 95th regular meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Osaka, 2015/11 /7
- Yohei Taniguchi et al.: Usefulness of an electric dilator for treatment of biliary jejunal anastomotic stenosis.The 95th regular meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2015/11/7
- Masashi Fukushima et al.: Endoscopic examination of malignant lymphoma of the small intestine. The 95th regular meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2015/11/7
- Kitamoto, H. et al.: A study of acute GVHD enteritis in our hospital. Japan Gastroenterological Endoscopy Society Kinki Branch 95th Branch Regular Meeting, Osaka, November 7, 2015
- Kei Okumura et al.: A case of esophageal submucosal hematoma with chest pain.The 95th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Osaka, November 7, 2015
- Ryusuke Minamide et al.: A case of disseminated strongyloidiasis after chemotherapy for malignant lymphoma.The 95th branch regular meeting of the Kinki branch of the Japan Gastroenterological Endoscopy Society, Osaka, 2015/11/7
- Kazuhiro Matsumoto et al.: A case of small intestinal ulcer due to microscopic polyangiitis that was difficult to diagnose.The 95th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Osaka, November 7, 2015
- Hiroyuki Hatamori et al.: A case of intestinal MALT lymphoma with diffuse changes.The 95th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Osaka, November 7, 2015
- Takuhiko Ito et al.: Usefulness of Evolution for duodenal stenosis due to malignant tumor. The 95th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Osaka, 2015/11/7
- Junko Ito et al.: A case of small intestinal follicular lymphoma recovered by double-balloon endoscopy due to retention of capsule endoscopy.The 95th branch meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Osaka, 2015/11/7
- Yuta Tsujisaka et al.: A case of portal venous gas caused by ischemic enteritis triggered by gastric ulcer bleeding.The 95th branch regular meeting of the Japan Gastroenterological Endoscopy Society Kinki Branch, Osaka, 2015/11/7
- Kitamoto, H. et al.: A case study of percutaneous endoscopic gastrostomy expansion in our hospital. The 19th Annual Meeting of the Japan Society of Metabolism and Clinical Nutrition, Yokohama, January 9, 2016
- Kazuya Hosoya et al.: Pancreatic neuroendocrine tumor (PNET) in our hospital. The 104th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 6, 2016
- Matsumoto, K. et al.: A case of pancreatic pleural effusion associated with visceral inversion.The 104th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 6, 2016
- Hiroyuki Hatamori et al.: A case of eosinophilic enteritis following chronological changes in endoscopic findings.The 104th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 6, 2016
- Ryusuke Minamide et al.: A case of multiple small bowel hemangiomas observed endoscopically.The 104th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 6, 2016
- Takuhiko Ito et al.: Study of efficacy of tolbabstan for refractory ascites associated with liver cirrhosis in our hospital. The 104th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 6, 2016
- Kei Okumura et al.: A case of intrahepatic eosinophilic granuloma formation. The 104th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 6, 2016
- Kitamoto, H. et al.: A case of small intestinal aneurysm with submucosal tumor.The 104th regular meeting of the Kinki branch of the The Japanese Society of Gastroenterology, Osaka, February 6, 2016
- Ito T et al.: The Efficacy of an endoscopic self-expandable metal stent for gastric outlet obstruction by malignancies.23rd United European Gastroenterology Week,Barcelona,2015/10/24-28
- Fukushima M et al.: Usefulness of double-balloon enteroscopy for diagnosis of Meckel's diverdiculum.Asian Pacific Digestive Week 2015,Taipei,2015/12/3-6
- Taniguchi Y: Evaluation of treatment for acute cholangitis in the elderly patients.Asian Pacific Digestive Week2015,Taipei,2015/12/3-6
- Kitamoto H et al.: Usefulness and Limitations of emergent capsule endoscopy in patients with obscuregastrointestinal bleeding.Asian Pacific Digestive Week 2015, Taipei, December 3-6, 2015.
- Hosotani K et al.: Endoscopic removal of foreign bodies from the gastrointestinal tract: Retrospective analysis of 284 patients .Asian Pacific Digestive Week2015,Taipei,2015/12/3-6
- Minamide T et al.: Pancreatic Lesions with von Hippel-Lindau Disease.Asian Pacific Digestive Week 2015,Taipei,2015/12/3-6
- Matsumoto K et al.:The characteristics of ischemic enteritis.Asian Pacific Digestive Week 2015,Taipei,2015/12/3-6
- Masashi Fukushima: A case of enteropathy-associated T-cell lymphoma observed by double-balloon endoscopy. Stomach and intestine Vol.49 No.9 reprint, 2014/8/25
- Fukushima M et al.:A case series of Meckel's diverticulum:usefulness of double-ballon enteroscopy for diagnosis.BMC Gastroenterology 2014(Vol.14),2014/8/30
- Ogawa S et al.:Case of primary hepatic gastrinoma:Diagnostic usefulness of the selective arterial calcium injection test.Hepatology Research (Article first published online:18 Sep2014), 2014/9/18
- Fukushima M et al.: Granulocytic sarcoma of the small intestine in a prtient with chronic myelomonocytic leukemia ,Diagestive Endoscopy 2014(Vol.26:757-758), 2014/11/3
- Satoshi Ogawa et al.: A case of jejunal ectopic pancreatic cancer for which MRI was useful for diagnosis.Journal of the The Japanese Society of Gastroenterology Vol.112(2015) No.1 P70-77,2015/1/5
- Tomonori Matsumoto et al.: II. Specifics Special histological type (clinicopathological features) Mucinous carcinoma/signet ring cell carcinoma. Nippon Rinsho Vol. 20
- Mikio Fujita et al.: Investigation of FOLFOX 6 /SOX + Cetuximab therapy as first-line therapy for advanced recurrent colorectal cancer. The 100th Annual Meeting of the The Japanese Society of Gastroenterology, Tokyo, April 24, 2014
- Satoshi Ogawa et al.: Examination of contrast-enhanced ultrasonography findings in 3 cases of liver reactive lymphoid hyperplasia. The 87th Annual Meeting of the The Japan Society of Ultrasonics in Medicine, Yokohama, May 9-11, 2014
- Masashi Fukushima et al.: Diagnosis, treatment and prognosis of gastrointestinal follicular lymphoma. The 87th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Fukuoka, May 15-17, 2014
- Kitamoto, H. et al.: A study of adult intussusception in our hospital. The 87th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Fukuoka, May 15-17, 2014
- Hironori Kitamoto et al.: Current status of stent placement therapy for patients with malignant gastroduodenal stenosis in our hospital. The 87th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Fukuoka, May 15-17, 2014
- Kazuya Hosotani et al.: Experience of gastrointestinal foreign bodies in our hospital. The 87th Annual Meeting Japan Gastroenterological Endoscopy Society, Fukuoka, May 15-17, 2014
- Naoto Urano et al.: Gastric ESD for the elderly. The 87th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Fukuoka, May 15-17, 2014
- Yohei Taniguchi et al.: Gallbladder drainage (PTGBD) for acute cholecystitis after biliary metal stent placement, followed by endoscopic ultrasound-assisted gallbladder drainage (EUS-GBD). The 87th Annual Meeting of the Japan Gastroenterological Endoscopy Society, Fukuoka ,2014/5/15-17
- Yohei Taniguchi et al.: Evaluation of the treatment results, risk of recurrence, and short- to medium-term course of endoscopic papillotomy (EST) + large diameter balloon dilatation (FPLBD). The 87th Annual Meeting of the Japan Gastroenterological Endoscopy Society,Fukuoka,2014/5/15-17
- Masaya Wada.: Endoscopic papillary large balloon dilation (EPLBD) for bile duct stones in our hospital. The 87th Annual Meeting Japan Gastroenterological Endoscopy Society, Fukuoka, May 15-17, 2014
- Naoto Urano et al.: ESD case study for Barrett esophageal Japan Gastroenterological Endoscopy Society.
- Ryusuke Japan Gastroenterological Endoscopy Society et al.: Study of ischemic enteritis.
- Masashi Fukushima et al.: Clinical study of idiopathic mesenteric Japan Gastroenterological Endoscopy Society in our hospital.
- Masaya Wada.: Current status of diagnosis and treatment of Japan Gastroenterological Endoscopy Society tumors in our hospital.
- Kazuya Hosotani et al.: A case of Japan Gastroenterological Endoscopy Society cancer with submucosal tumor-like morphology.
- Kazuhiro Matsumoto et al.: A case of simultaneous multiple gastric cancers of gastric Japan Gastroenterological Endoscopy Society cell carcinoma and adenocarcinoma.
- Takuhiko Ito et al.: A case of pancreatic neuroendocrine tumor (P-NET) recurrence as metastatic gastric tumor 5 years after Japan Gastroenterological Endoscopy Society.
- Hironori Kitamoto et al.: A case of PNET with extension of the main pancreatic duct diagnosed preoperatively. The 92nd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, June 21, 2014
- Mikio Fujita et al.: A Retrospective Study of HER2-status and Combined Chemotherapy with Trastuzumab in Advanced Gastric Cancer.The 12th Annual Meeting of the Japanese Society of Medical Oncology, Fukuoka, 2014/7/17 -19
- Mikio Fujita et al.: Usefulness of partial splenic artery embolization in gastrointestinal cancer chemotherapy. The 52nd Annual Meeting of the Japan Society of Clinical Oncology of Oncology, Yokohama, August 28-30, 2014
- Yohei Taniguchi et al.: Study on treatment results and recurrence of endoscopic papillotomy (EST) + large diameter balloon dilatation (The Japan Biliary Association).
- Masaya Wada.: Trial of bile duct stone removal using a large balloon at our hospital. The 101st Annual Meeting of the Kinki Branch The Japanese Society of Gastroenterology, Osaka, 2014/10/4
- Hironori Kitamoto et al.: A surgical case of localized autoimmune pancreatitis that was difficult to differentiate from pancreatic The Japanese Society of Gastroenterology.
- Hiroyuki Hatamori et al.: A case of giant esophageal leiomyoma diagnosed by EUS-The Japanese Society of Gastroenterology and treated by thoracoscopic resection.
- Kazuya Hosotani et al.: Current status of gastric variceal The Japanese Society of Gastroenterology using Histoacryl for gastric variceal bleeding in our hospital.
- Ryusuke Minamide et al.: A case of small intestinal arteriovenous malformation diagnosed by endoscopic mucosal resection. The 101st Annual Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka, 2014/10/4
- Kazuhiro Matsumoto et al The Japanese Society of Gastroenterology A case of hepatitis B successfully treated with sequential therapy.
- Takuhiko Ito et al.: A case of ileocecal resection due to intestinal heaviness caused by ileocecal inflammation. The 101st Annual Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Osaka, 2014/10/4
- Satoko Inoue et al.: Study of The Japanese Society of Gastroenterology treatment for ulcerative colitis in our hospital.
- Mikio Fujita et al.: Study of Her2 positive unresectable advanced recurrent gastric cancer. JDDW2014, Kobe, 2014/10/23
- Yohei Taniguchi et al.: Treatment results and recurrence of endoscopic papillary sphincterectomy (EST) + large diameter balloon dilation (EPLBD). JDDW2014, Kobe, 2014/10/24
- Takuhiko Ito et al.: Investigation of metastatic gastric tumor experienced at our hospital. JDDW2014, Kobe, 2014/10/25
- Masaya Wada.: A study of 7 cases of Solid-pseudopapillary neoplasm (SPN) in our hospital. JDDW2014, Kobe, 2014/10/25
- Kazuhiro Matsumoto et al.: Study of gastric endocrine cell carcinoma in our hospital. JDDW2014, Kobe, 2014/10/25
- Kazuya Hosotani et al.: A study of 12 cases of small bowel GIST in our hospital. JDDW2014, Kobe, 2014/10/26
- Urano, N. et al.: Japan Gastroenterological Endoscopy Society drug oral administration and gastric ESD incidence.
- Masashi Fukushima et al.: Treatment results of ERCP using balloon Japan Gastroenterological Endoscopy Society for postoperative reconstructed bowel at our hospital.
- Hironori Kitamoto et al.: Usefulness of capsule endoscopy for patients with gastrointestinal bleeding of unknown cause in our hospital. The 93rd Annual Meeting of the Kinki Branch of the Japan Gastroenterological Endoscopy Society, Osaka, November 15, 2014
- Takuhiko Ito et al.: A case of squamous cell carcinoma of the anal canal that was successfully resected by Japan Gastroenterological Endoscopy Society mucosal exfoliation ESD.
- Matsumoto, Kazuhiro et al.: A case of small intestinal varicose vein rupture achieved hemostasis by extravascular injection of Japan Gastroenterological Endoscopy Society and Aethoxysklerol.
- Kitamoto, Hironori et al.: A case of giant hepatic angiomyolipoma that required differentiation from hepatocellular adenoma.The 41st Annual Meeting of the The Japan Society of Ultrasonics in Medicine Kansai, Kyoto, 2014/11/22
- Hiroshi Tei et al.: Effectiveness The Japanese Society of Gastroenterology limitations of nucleic acid analogues for chronic hepatitis B and cirrhosis.
- Masashi Fukushima et al.: Current status of emergency balloon endoscopy for The Japanese Society of Gastroenterology bleeding in our hospital.
- Kazuya Hosotani al.: A case of unresectable advanced esophageal cancer with fistula formation during the course, but improved QOL and relatively long-term survival with The Japanese Society of Gastroenterology treatment. Branch regular meeting, Kyoto, 2015/2/21
- Ryusuke The Japanese Society of Gastroenterology et al.: A case of gastric abscess caused by a toothpick.
- Kitamoto, H. et al.: A case of small intestinal DLBCL after treatment for parotid gland MALT lymphoma. The 102nd Annual Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 21, 2015
- Takuhiko Ito et al.: A case of giant hepatocellular carcinoma treated with few side effects using beads for thromboembolism. The 102nd Annual Meeting of the Kinki Branch of the The Japanese Society of Gastroenterology, Kyoto, February 21, 2015
- Kazuhiro Matsumoto et al.: A case of residual The Japanese Society of Gastroenterology liver cancer.
- Taniguchi Y et al.: Efficacy and Safety Endoscopic papillary large balloon dilation following with an Endoscopic sphincterotomy (EST+EPLBD) for large or multiple common bile duct stones(CBDS). APDW2014, Indonesia. 2014/11/22-25
- Inokuma T et al.: Clinical consideration of metastatic gastric tumor. APDW2014, Indonesia,2014/11/22-25
- Fujita M et al.: A phase II study of 5-FU/I-LV/oxaliplatin(mFOLFOX6)in patisnts with metastatic or unresectable small bowel adenocarcinoma: A post hoc analysis.ASCO-GI,San Francisco,2015/1/15 -17