当院消化器内科は、日本消化器病学会指導医/専門医7名、日本消化器内視鏡学会指導医/専門医7名、日本肝臓学会指導医/専門医3名、日本膵臓学会指導医1名、日本胆道学会指導医1名、日本炎症性腸疾患学会指導医1名を含む医師16名の体制で、各分野のエキスパートを擁し、専門性が高く良質な医療を提供できる体制になっています。また、日本内科学会認定総合内科専門医5名・日本専門医機構内科専門医3名と内科専門医の取得者数も多く、全人的医療を心掛けるとともに充実した内科専門研修にも対応しています。
施設認定としては、日本消化器病学会・日本消化器内視鏡学会・日本肝臓学会・日本超音波医学会・日本膵臓学会・日本胆道学会・日本炎症性腸疾患学会の指導施設に認定されています。令和6年度の実績として、当科の外来患者数は1日平均168.2名、入院患者数は年間2154名、平均在院日数6.2日であり、地域医療機関と連携した急性期医療を担っています。6階東・7階西・9階東病棟を基本病棟として約40名の患者さんが入院治療を受けています。消化器内科は救急疾患の多い領域ですが、当院は厚生労働省の「救命救急センター」の評価において11年連続全国1位の評価をいただいており、救急部と協力しいつでも緊急検査・治療ができる体制をとっています。
各分野のエキスパートと専門性の高いメディカルスタッフが協力し、高品質なチーム医療を提供いたします。
毎週、スタッフ全員で「症例カンファレンス」を行い、薬剤師・栄養士も参加して診療をサポートしています。その他、外科との合同カンファレンス・病理カンファレンス・IBDカンファレンス・内視鏡カンファレンス・食道癌カンファレンスを行い、質の高い医療を心掛けています。

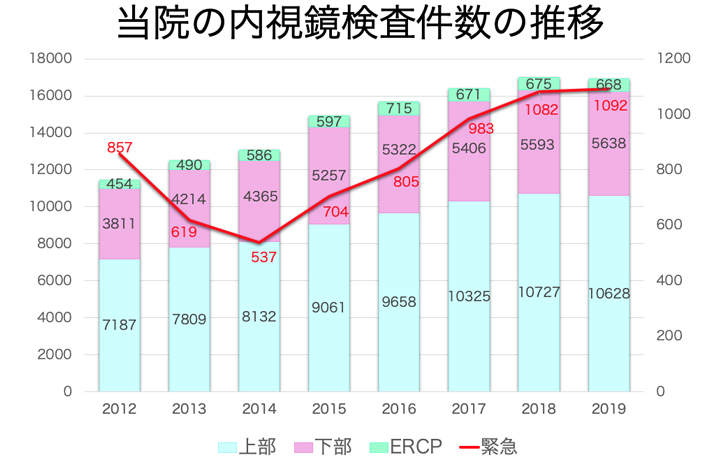
内視鏡センターでは、年間約14,000件の内視鏡検査・治療を行っています。緊急内視鏡も昨年は9,00件以上実施しました。積極的にセデーション(鎮静剤使用)を行っており、苦痛が少なく、かつ丁寧な内視鏡検査を心掛けています。

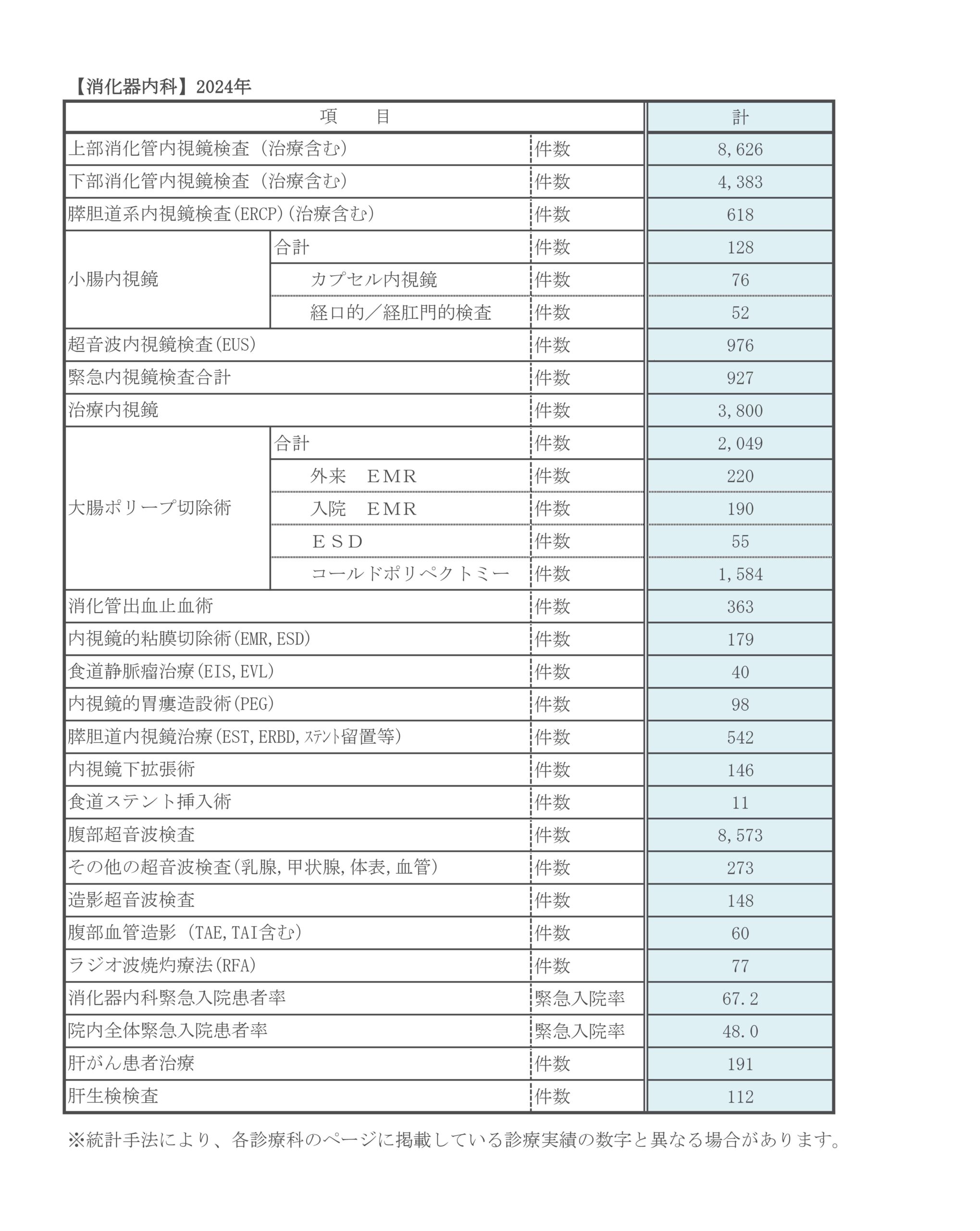
診療実績
診療科別統計
主な疾患・治療法

セデーション内視鏡検査とは
当科での鎮静剤を使用しての(セデーション)内視鏡検査は、「日本消化器内視鏡学会」作成の「鎮静に関するガイドライン」に準拠し、苦痛の少ない内視鏡検査をより安全に施行することで患者さんの検査に対する不安・ストレスを軽減し、検査の受容性を高めることで消化管癌の早期発見・負担の少ない内視鏡治療を推進することを目的としています。
鎮静レベルは、意識下鎮静(conscious sedation)を心がけ、過度の鎮静による呼吸抑制・血圧低下などの副作用を低減するようにしています。
また、より安全に検査をおこなうため、検査中は全例で生体情報モニターによる監視をおこない、検査後はリカバリースペースにてセデーションからの回復を図ります。30分程度の観察後、鎮静覚醒スコアにより意識レベルの十分な回復を確認の上、帰宅してもらうようにしています。
高齢の方には、付添の方と一緒に来ていただくことをお勧めしています。
検査当日は、自動車・バイク・自転車などの運転は控えていただきます。

内視鏡センターは1階映像医学部門にあり、近畿の臨床病院では最大規模(約857m²)のスペースで運用しています。内視鏡検査室6室・X線透視室2室・多目的治療室1室を有し、内視鏡システムは(OLYMPUS社製 EVIS LUCERA ELITE)10台を導入し、拡大内視鏡・経鼻内視鏡を含む最新型電子内視鏡を導入しています。12ベッドのリカバリースペースを設け、セデーション検査後はベッドに寝たままでリカバリースペースに移動し、専属ナースが呼吸・循環状態を集中監視モニターでチェックします。患者さんに安全で快適な検査を受けていただけるように配慮しています。デイセンターも併設し、日帰り治療(大腸ポリープ切除)も積極的におこなっています。
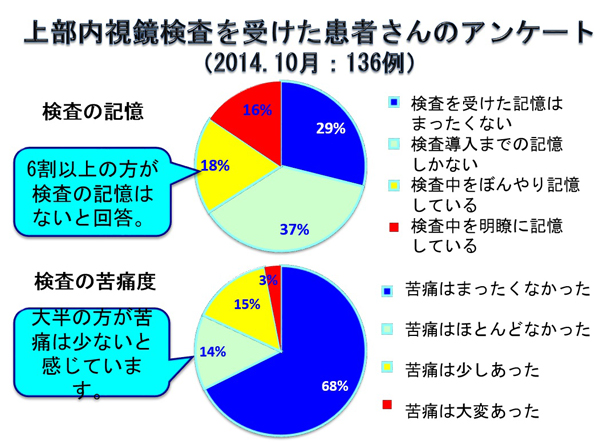
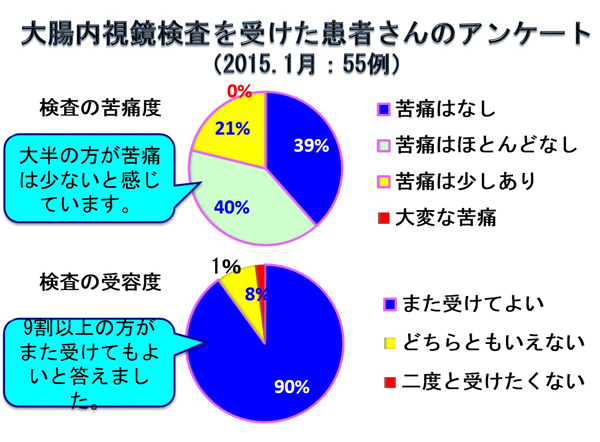
セデーション検査に対するアンケート結果
上部消化管内視鏡検査(EGD)・下部消化管内視鏡検査(CS)後に患者さんの満足度を評価する目的でアンケートを実施しました。EGDは平成26年10月(136名)、CSは平成27年1月(55名)に当センターでセデーション検査を受けた患者さんに、協力していただきました。
その結果は、表に示すとおりです。
EGDを受けた記憶に関する質問では、39/136例(29%)で検査中の記憶が全く無く、検査を受けたこともほとんど覚えていないとのことでした。50/136例(37%)では、検査が開始されスコープが挿入されるまでの記憶しかないとのことで、これらを合わせた66%の患者さんは、検査中のことは覚えていないようです。また、検査の苦痛に関する質問では、当然ながら記憶の無い方で検査に関する苦痛はないため、80%以上の方で検査に伴う苦痛はほとんど感じなかったという評価を得ました。その結果として、セデーション検査を受けた124/136例(91%)の方は、次回からもセデーションを希望すると回答されました。
これは、我々にとって予想以上の評価であり、内視鏡検査に伴う苦痛は許容範囲内に軽減されたと考えています。
高齢化社会の進行とともに癌はcommon diseaseとなり、日本人の2人に1人が癌に罹患し、3人に1人が癌で命を落とす現状です。今まで、「胃カメラ・大腸カメラはしんどいから受けたくない。」と躊躇していた患者さんにも、セデーション検査は安心して受けていただけると考えます。
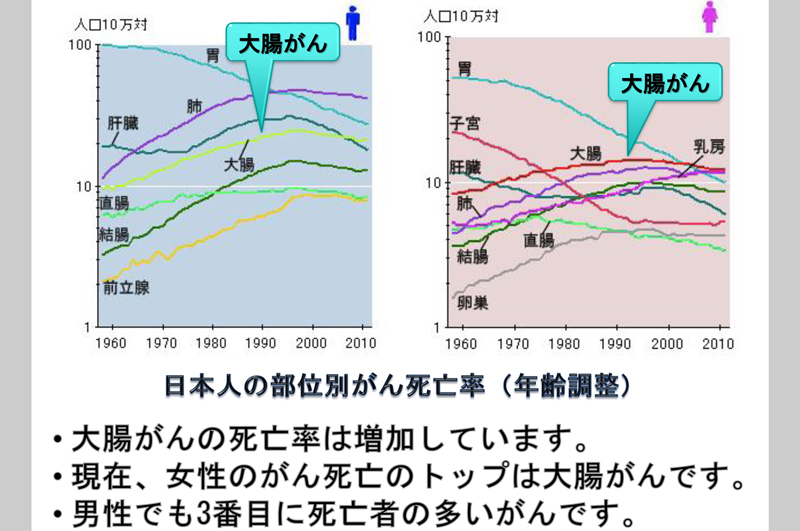
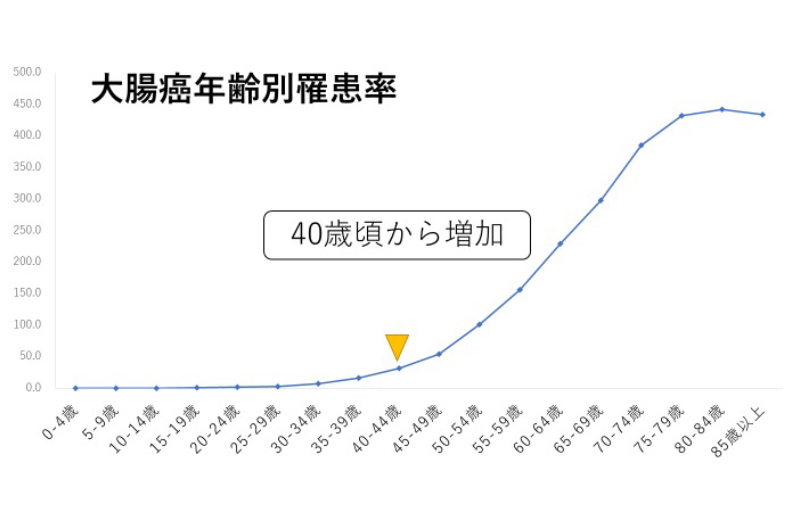
大腸癌は増加しています
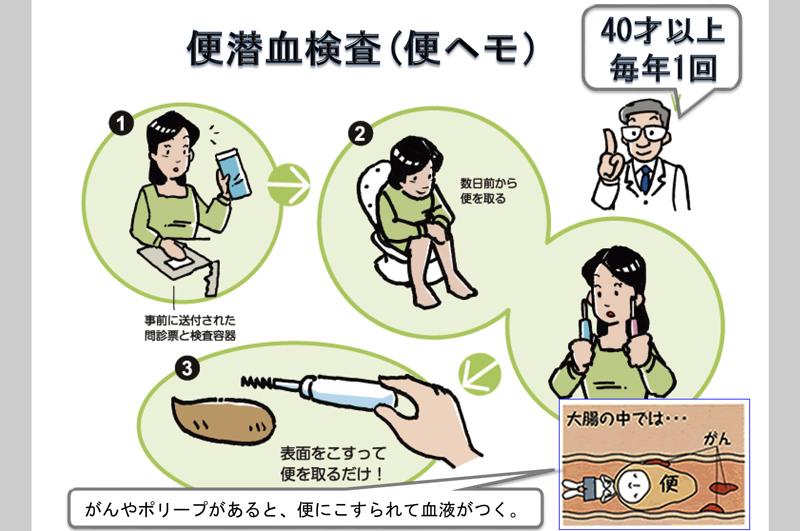
大腸癌検診を受けましょう
大腸内視鏡検査を受けましょう
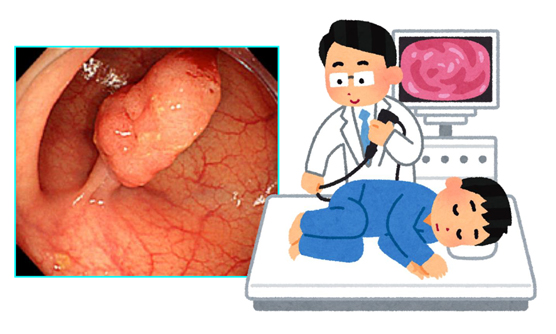
大腸内視鏡検査とは、肛門から柔らかい管(スコープ)を挿入して、大腸の表面を観察する検査です。事前に、下剤と腸管洗浄液を内服して、便を排泄してから観察をおこないます。内視鏡検査をおこなうことで、大腸がんでの死亡率が40%減少するという報告があり、当科でも積極的におこなっています。見つかったポリープは積極的に内視鏡的に切除を行います。小さな病変であれば、外来治療も可能です。
当科では、大腸内視鏡検査を年間5000件以上施行し、大腸ポリープに対し「日帰りポリープ切除」を年間2100件以上実施しております。
早期発見が重要です
早期癌は自覚症状に乏しく、現在でも進行癌で発見されることも少なくありません。早期癌であれば、内視鏡治療も可能です。もし、持続する腹痛・排便異常(便秘/下痢)・貧血などがある場合は、内視鏡検査を受けることをお勧めします。大腸ポリープ(腺腫といいます)・早期癌の多くは内視鏡で根治可能です。進行癌の場合は外科が腹腔鏡下切除など低侵襲治療を心がけており、遠隔転移を来たしている場合も腫瘍内科が積極的に化学療法を行い、治療成績の向上に努めております。
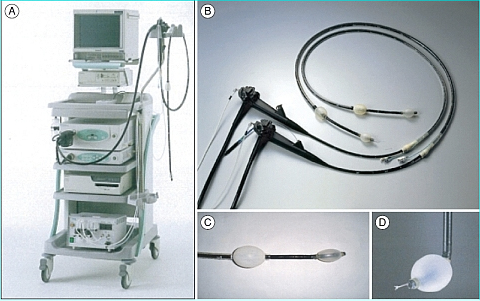
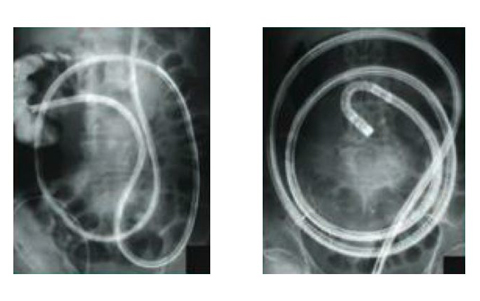
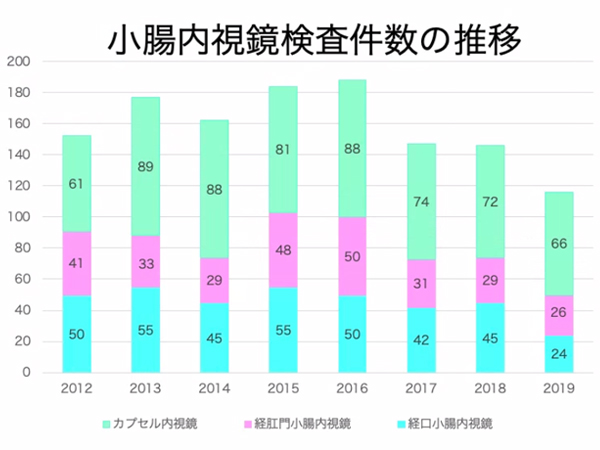
昨今、増加傾向にある小腸疾患に対し、ダブルバルーン式小腸内視鏡を用いて、積極的に小腸内視鏡検査を実施しています。令和元年度は50例に施行し、従来の検査法ではわからなかった小腸病変の正確な診断と内視鏡治療が可能となってきました。また、カプセル内視鏡も、平成20年6月より導入し、令和元年度は66例に施行しています。原因不明の消化管出血など小腸病変に対し、カプセル内視鏡によるスクリーニングから、ダブルバルーン式小腸内視鏡による精査・治療まで一貫した診療をおこなえる体制を整えています。
小腸内視鏡検査:暗黒の領域に光を当てる
小腸は胃と大腸の間にあり、消化管の中では最も長く6〜7メートルあり、栄養素の消化吸収を担っています。従来より、内視鏡検査が困難な臓器であり「消化器の暗黒大陸」といわれてきました。しかし、2000年にイスラエルでカプセル内視鏡、2001年に我が国でダブルバルーン式小腸内視鏡が相次いで開発され、小腸疾患の診断と治療が急速に進歩してきました。
当科でも、2003年からダブルバルーン式小腸内視鏡(FTS社EN450P5/20,EN450T5/W,EN-580XP,EN-580T,EC-450BI5)を用いた小腸内視鏡検査をおこない成果をあげてきました。また、より負担が少なく、外来検査にて小腸の観察が可能であるカプセル内視鏡も、2008年6月より導入し、原因不明の消化管出血など小腸病変に対し、カプセル内視鏡によるスクリーニングから、ダブルバルーン式小腸内視鏡による精査・治療まで一貫した診療をおこなえる体制を整えております。両方会わせて年間100件を越える検査数は、近畿でも最も多い病院の一つであります。
小腸疾患の実態と内視鏡検査
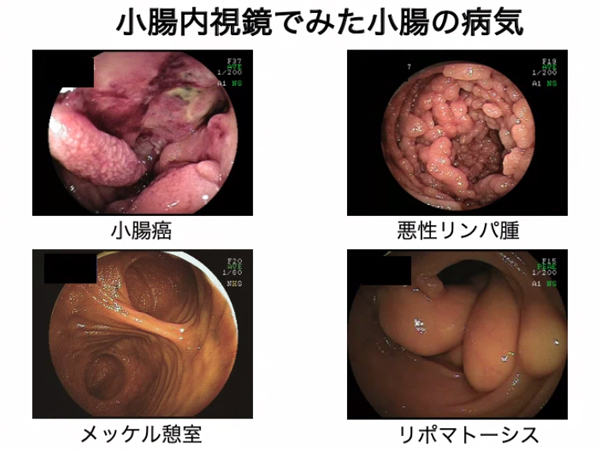
前述したように、「暗黒大陸」といわれていた小腸の疾患については実態不明な点が多々ありました。しかしダブルバルーン式小腸内視鏡やカプセル内視鏡の導入により、詳細な病態が明らかになりつつあります。
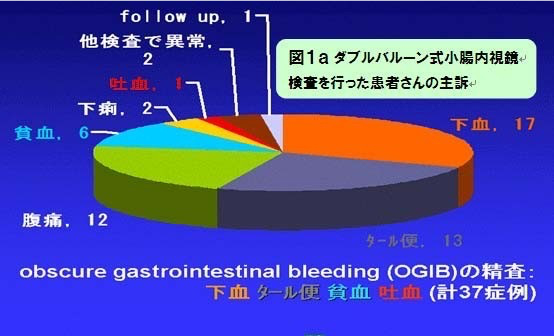
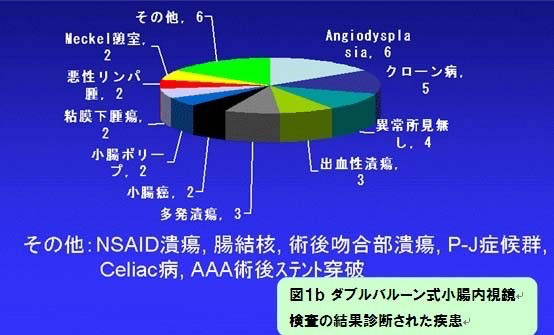
スライドは、当院においてダブルバルーン式小腸内視鏡検査を施行した患者さんの、主訴(図1a)と、検査の結果診断された疾患(図1b)をあらわしたものです。小腸内視鏡検査の普及の結果、従来考えられてきた以上に、小腸疾患は多数存在することが明らかになってきました。
原因不明消化管出血:OGIBとカプセル内視鏡検査
聞き慣れない言葉かもしれませんが、原因不明消化管出血(Obscure Gastrointestinal Bleeding:OGIB)とは、血便や下血、原因不明の貧血等で消化管からの出血が強く疑われるにもかかわらず、従来の上部・下部消化管内視鏡検査を施行しても出血の原因となる病変を発見できない病態を指します。こういった病態では、原因不明のまま経過観察となるため、繰り返す出血により貧血が進行したり、入退院の繰り返しにより患者さんの生活が大きく制限を受けることになります。時には多量出血によってショック状態となり、生命の危険が生じる可能性もあります。小腸内視鏡の普及で、OGIBの中に、小腸病変からの出血例が含まれることが明らかとなってきました。OGIBの診断には、出血から検査までの時間が短ければ短い程、診断率が向上することが知られています。そこで、カプセル内視鏡は、外来緊急検査も可能であるため、急な出血症例に対しても比較的速やかに対応できるメリットがあります(図5)。
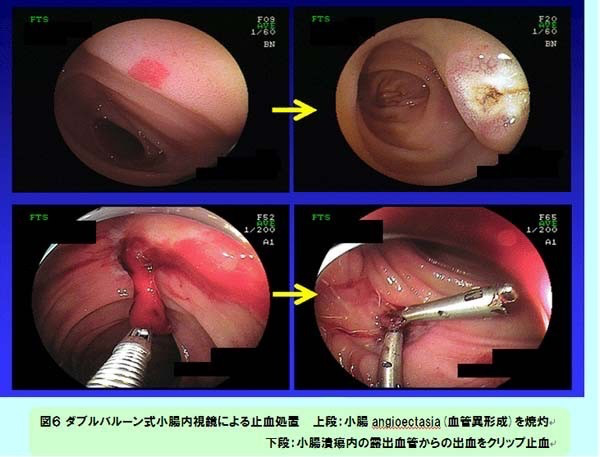
その上で、止血処置などの治療適応の場合は、引き続きダブルバルーン式小腸内視鏡検査をおこなうようにしています(図6)。
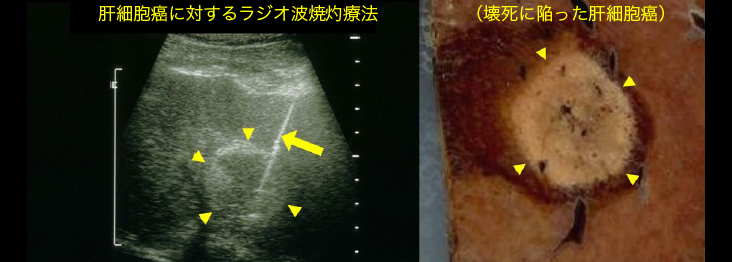
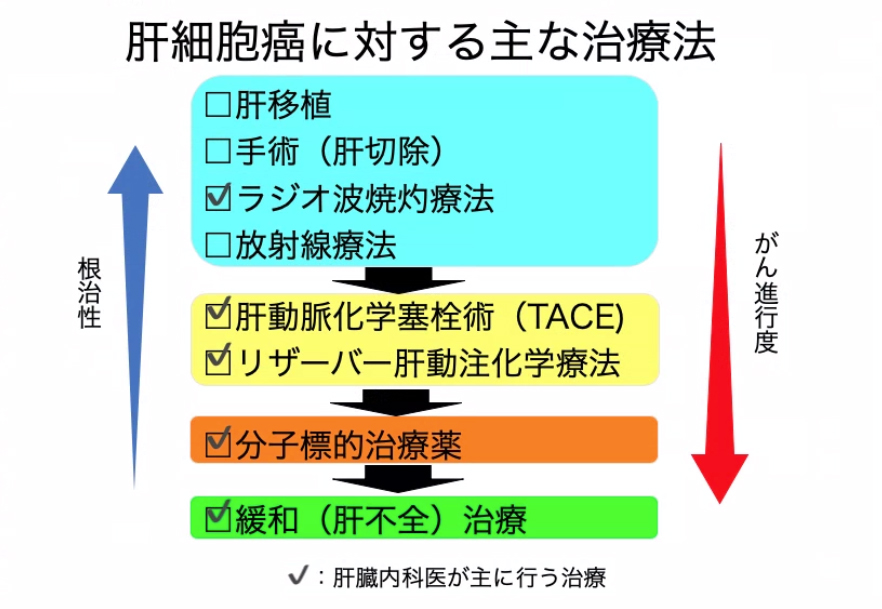
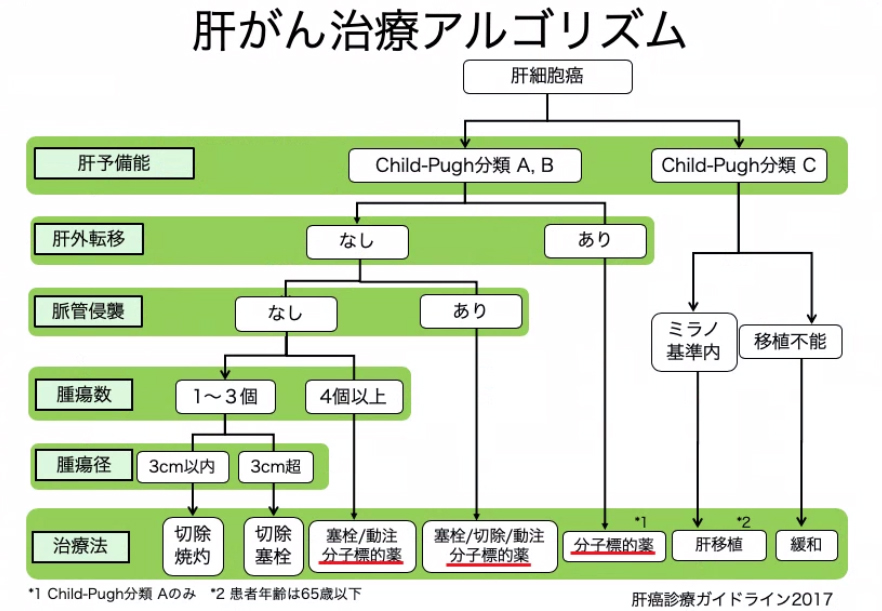
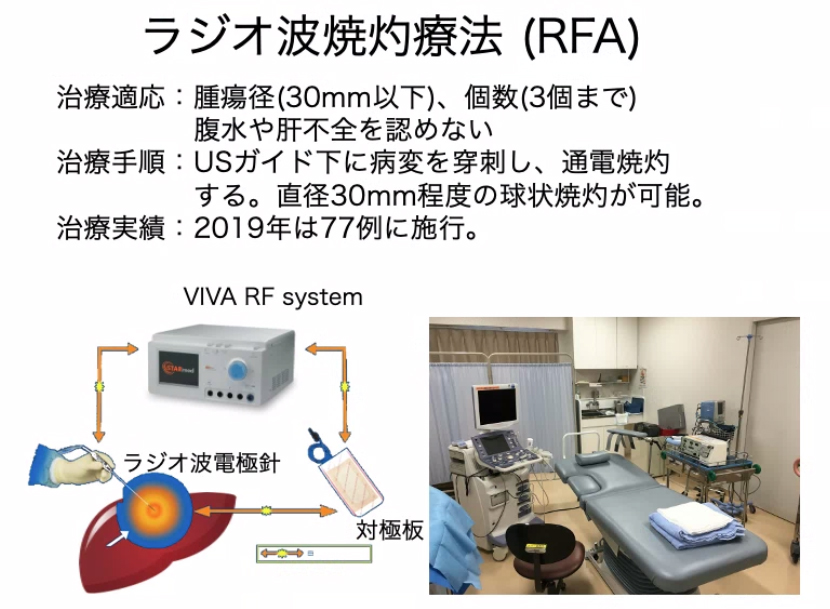
日本人の癌死亡者数で5番目に多いのが肝癌です。以前は4番目でしたが、ウイルス性肝炎に対する治療が進歩したため2000年頃をピークに減少傾向にあります。しかし、今でも年間3万人弱の患者さんが肝癌で亡くなっています。当科では、以前より「肝癌診療ガイドライン・治療アルゴリズム」に基づき、病態の進行度に応じた集学的治療をおこなっています。内科的治療として、ラジオ波焼灼療法(RFA)を年間77例(2019年)に施行しています。
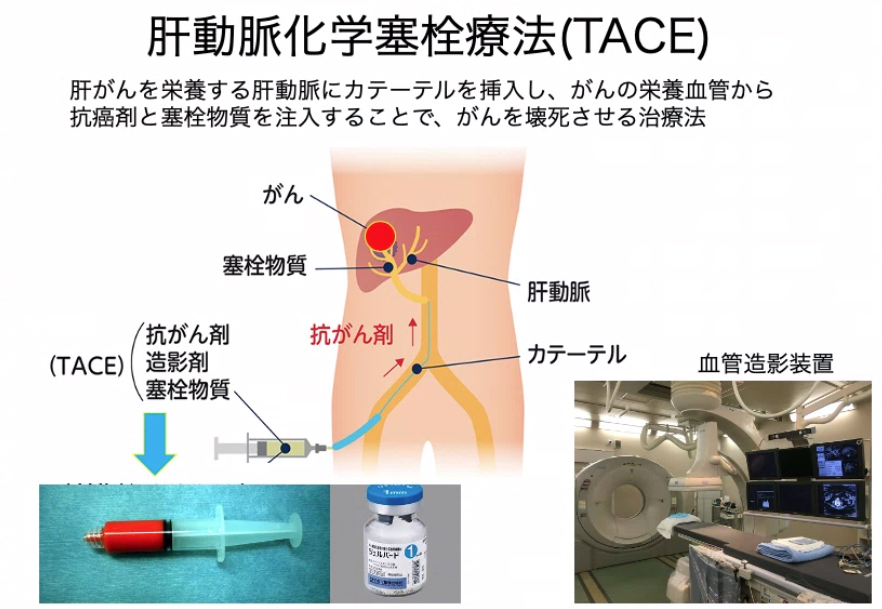
より病態が進行している場合は、肝動脈化学塞栓療法(TACE)を選択しています。TACEは、日本で開発されたカテーテル治療(IVR)で、当院では年間157例(2019年)の施行実績があります。また、塞栓物質としてジェルパート®を用いるConventional TACE以外に、薬剤溶出性球状塞栓物質を用いるDEB-TACEもおこなっています。
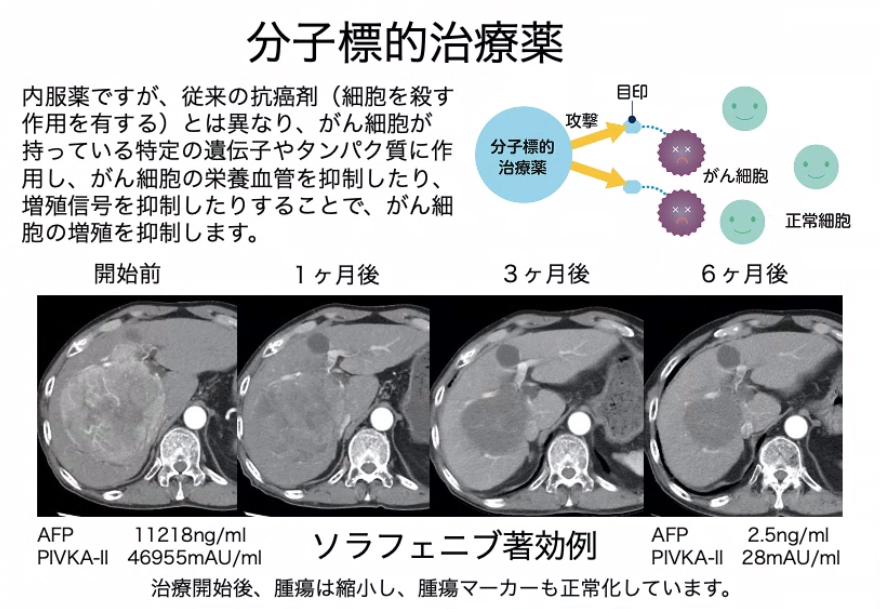
近年開発された分子標的治療薬は、肝癌の増殖を長期間にわたり抑制する作用のある内服薬です。現在、ソラフェニブ、レゴラフェニブ、レンバチニブが使用可能であり、切除不能進行肝癌では、肝予備能の良好な症例で積極的に導入しています。
放射線治療も肝癌の局所治療としては極めて有効であり、患者さんへの負担も少ないため、放射線治療科と協力して動体追尾定位放射線治療(経皮的金属マーカー:VISICOIL®留置を併用)をおこなっています。
切除適応と判断された場合は、外科にコンサルトし、肝予備能を評価した上で、切除をすすめます。当院では、腹腔鏡下肝切除術も積極的におこなっています。
肝癌については、このように各診療科が協力して治療に当たることが重要であり、当院では毎週カンファレンスを開催して、個々の患者さんに最適の治療方針について協議しています。2019年には、当科にてのべ251名の肝癌患者さんの治療をおこないました。
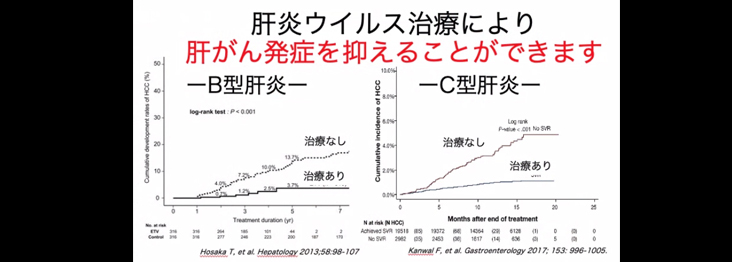
肝癌の原因の60〜70%を占めるC型ウイルス性肝炎に対し、当科では、1990年代のインターフェロン(IFN)の時代から積極的に治療してきました。しかし、インターフェロン注射は発熱・倦怠感等の副作用が強く、治療効果も十分ではなく、半数以下の患者さんしか治癒することはできませんでした。しかし、2010年代になり直接作用型経口抗ウイルス薬(DAAs)が開発され、現在では、内服薬を数週間継続するだけで、ほとんど副作用もなく、95%以上の患者さんのウイルス排除が可能となっています。
しかし、C型肝炎自体は自覚症状をきたすことがないため、肝炎ウイルスに感染していることを知らない潜在的な患者さんが少なくありません。輸血や手術を受けたことのある方は、地域の肝炎ウイルス検診を受けたり、かかりつけ医に相談することをお勧めします。当院も、肝疾患専門医療機関として、積極的な肝炎治療を心がけています。
B型肝炎も肝癌患者の10〜15%程度を占め、日本人でB型肝炎ウイルス感染者(キャリアを含む)は110〜130万人いるといわれています。また、世界中では、4億人が感染しており、既感染者を含むと20億人が感染しているといわれています。かつては、母子感染が多くみられましたが、1986年から母子感染防止事業がスタートし、現在はキャリア率も低くなっています。しかし、近年は、性交渉でB型肝炎にかかる患者さんも増加しており、対策が必要です。
B型肝炎の治療薬も進歩が目覚ましく、2000年にB型肝炎ウイルスの増殖を抑制する内服薬(核酸アナログ製剤)が発売され、現在では、ウイルス増殖を抑え肝炎を改善することは可能となっています。しかし、内服を中止したりすると再増殖をきたし、この治療でウイルスを体内から排除することはできません。
また、一度かかって抗体を獲得した方(HB既感染者)が、癌などに罹患し免疫力が低下したり、免疫を抑制する薬剤(抗癌剤など)を使用したりした後に、B型肝炎が再活性化し、重篤な状態になることが問題となっています。
当院を受診された患者さんで、B型・C型肝炎検査が陽性となった場合、患者さんに連絡して精査・治療ができるように「肝炎チェックシステム」を電子カルテ上に導入し、運用しています。

高齢化社会の進行とともに、癌で死亡する患者数は増加傾向にあります。日本人の二人に一人が癌にかかり、三人に一人が癌で死亡すると言われています。消化器癌の中では、大腸癌が一位、胃癌が二位を占め、それぞれ年間5万人程度が死亡しています。しかし、癌も早期発見すれば、治る病気であります。当科でも、食道癌・胃癌・大腸癌に対し、積極的な内視鏡治療を実施しています。
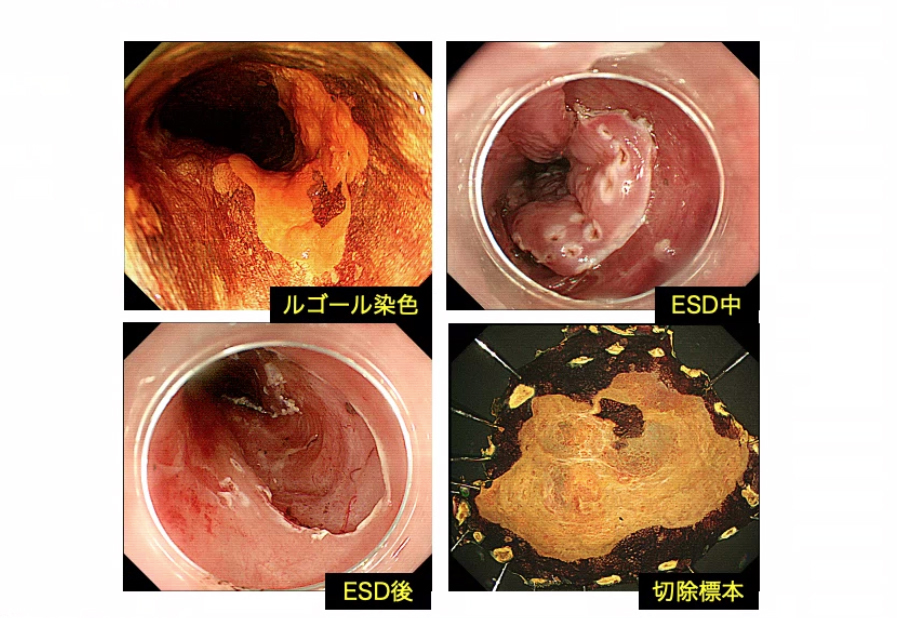
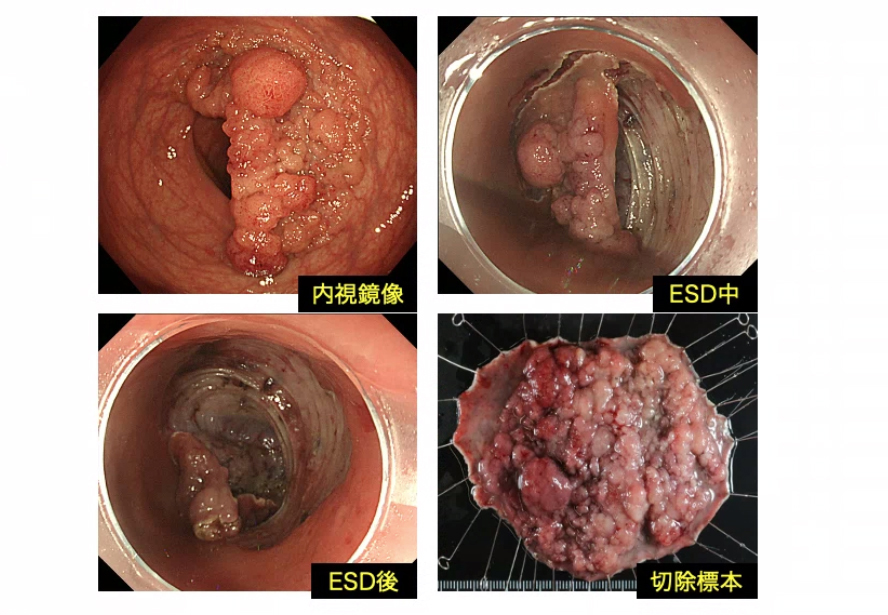
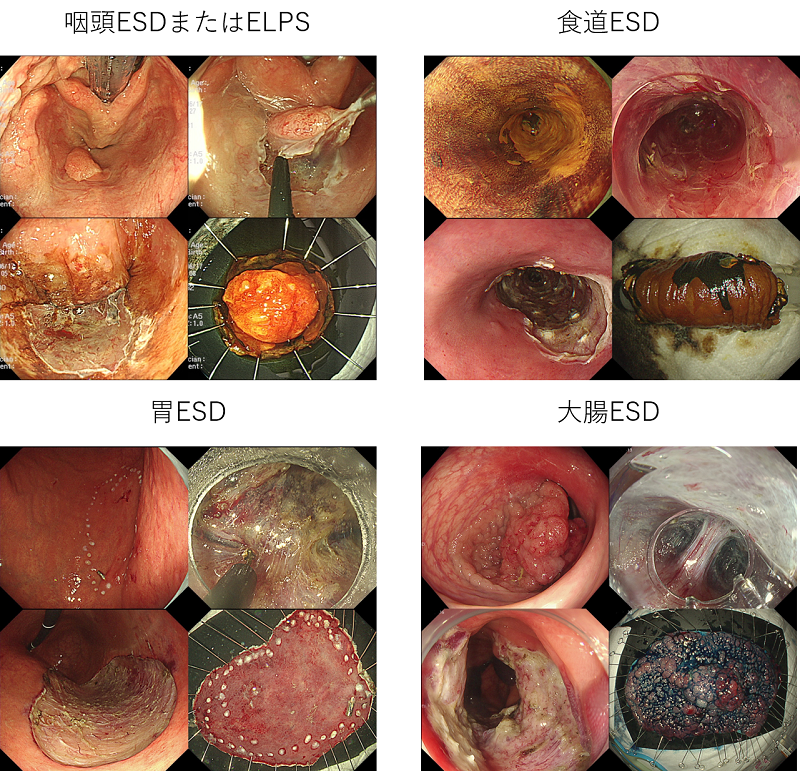
具体的には、内視鏡的粘膜下層剥離術(ESD)を導入して、年間200例以上の患者さんを治療しています。ESDは比較的大きな早期癌も一括切除することが可能ですが、手技的には高度の内視鏡操作技術を要します。当科では、内視鏡専門医3名が中心となり、生態情報モニターによる全身・呼吸管理のもとで、安全に施行しています。特に、必要な場合は、全身麻酔下で手術室を使用した内視鏡切除も実施できる体制を確保しています。
食道表在癌の内視鏡治療
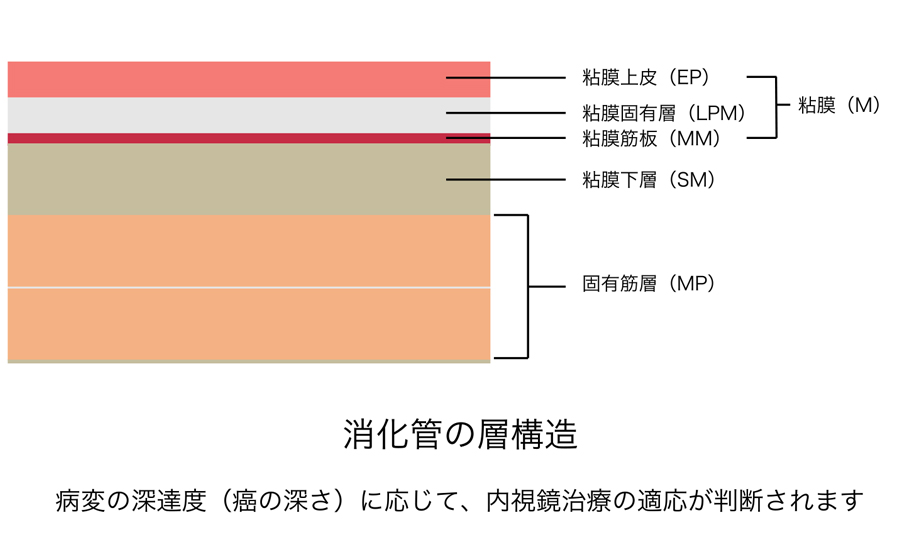
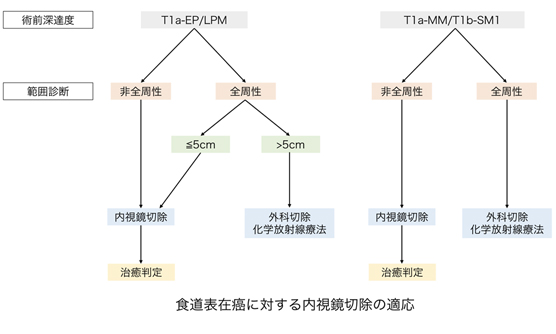
食道癌では、癌の深さが上皮(EP)/粘膜固有層(LPM)内にとどまる病変では、リンパ節転移の可能性はほとんどなく、内視鏡治療により根治性が得られるとされています。
癌の深さが粘膜筋板(MM)、粘膜下層にわずかに浸潤するもの(SM1:粘膜下層200μm未満)も内視鏡治療は可能ですが、リンパ節転移の可能性が10〜20%程度あるとされています。しかしながら、他の治療法の侵襲性を考慮し、「食道癌に対するESD/EMRガイドライン」では初回治療としての内視鏡治療が推奨されています。
内視鏡治療後の狭窄予防について
切除範囲が広範囲となる場合、特に全周性の病変では切除後の狭窄が問題となります。狭窄予防処置を行わなかった場合には狭窄が必発であり、通過障害により生活の質が著しく低下します。狭窄が生じた場合には、狭くなった部分を内視鏡下で拡張する処置を行いますが、改善が乏しく治療に難渋する場合があります。
近年では、内視鏡治療直後の潰瘍部にステロイドの局注を行ったり、ステロイドの内服を行ったりすることで、ある程度狭窄予防ができるようになってきました。それでも全周性で切除範囲が広い病変では狭窄のリスクが高いため、「食道癌に対するESD/EMRガイドライン」では、癌の深さが上皮(EP)/粘膜固有層(LPM)にとどまると診断される病変では、長径50mm以下の病変では狭窄予防を併用した上での内視鏡治療、長径50mmより大きい病変では、最初から外科手術や化学放射線療法を行うことが推奨されています。
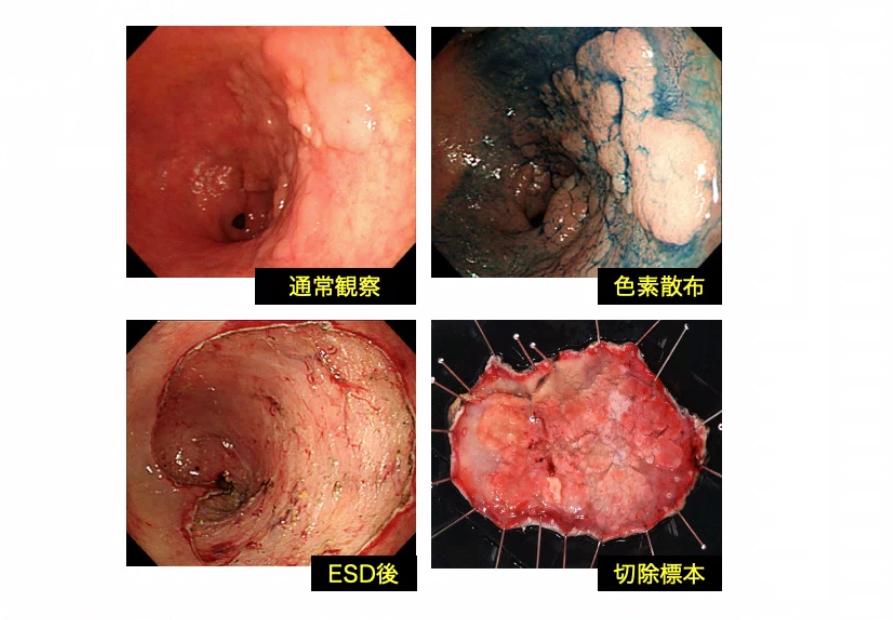
早期胃癌の内視鏡治療
早期胃癌に対する内視鏡治療では胃が温存されることから、外科手術と比較して良好なQOLが得られます。ただし、早期胃癌に対する内視鏡治療は、局所治療なので、胃周囲のリンパ節に転移がない病変が対象となります。リンパ節転移の危険性が極めて低い(1%以下)と推定され、外科的胃切除と同等の長期予後が得られる病変を絶対適応病変といいます。現在、JCOG0607およびJCOG1009/1010といった日本臨床腫瘍研究グループによる多施設共同前向き臨床研究の結果により、早期胃癌に対する内視鏡治療の長期成績が明らかとなり、「胃癌に対するESD/EMRガイドライン(第2版)」では、以下の条件にあてはまる病変が絶対適応病変とされています。
- 大きさは問わず、潰瘍のない、分化型、粘膜内癌(M)
- 3cm 以下、潰瘍のある、分化型、粘膜内癌(M)
- 2cm 以下、潰瘍のない、未分化型、粘膜内癌(M)
上記以外の早期胃癌においては、標準治療は外科的胃切除となります。ただし、治癒率が下がるものの内視鏡治療で根治の可能性もあるため、(外科的胃切除が困難といった)患者さんの状況によっては相対適応として内視鏡治療を行う場合もあります。
早期大腸癌の内視鏡治療
大腸ポリープに対して、多くがスネアを用いた治療が行われますが、一部の早期大腸癌(粘膜内癌[M]、粘膜下層への軽度浸潤癌[SM1:粘膜下層 1000μm 未満])に対しては、スネアでの治療が難しく、ESDによる一括切除を行います。
以下の条件にあてはまる病変をESDの適応としています。
- 2cm 以上でスネアによる一括切除が困難
- 粘膜下層に線維化を伴う病変
- 潰瘍性大腸炎など慢性的炎症がある病変
- 以前の内視鏡治療後の局所遺残病変
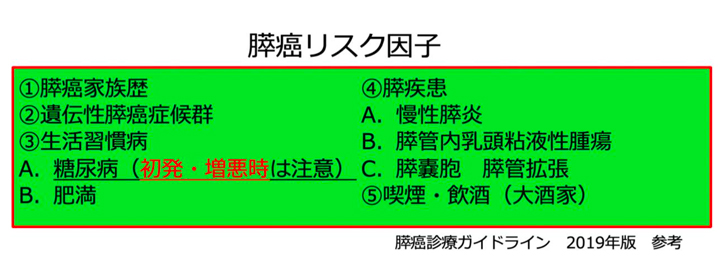
近年では膵癌は増加の一途をたどっており、年間約37000人の方が膵癌により死亡しています。各臓器別の癌死亡率の推移をみると、医療の進歩により胃癌や大腸癌、肝臓癌では減少しつつありますが、膵癌においてはその徴候は認められていません。
膵癌は5年生存率10%にも満たず、予後不良な疾患です。しかし、大きさ1cm以下の膵癌では5年生存率80%にも達すると言われており、いかに早期発見し治療へ移行していくかが課題となっています。一般的に膵癌は早期発見が難しいとされていますが、膵癌高リスク患者さんに対して適切なタイミングで適切な検査を行っていくことで早期発見も可能であると考えています。そのため地域医療機関からも膵癌高リスク患者さんをご紹介いただき、積極的に検査を行っています。仮に紹介時に異常が無い場合でもあっても、定期的に検査を行っていくことが肝要であると考えています。
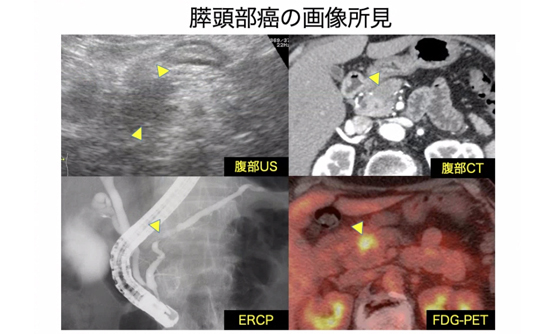
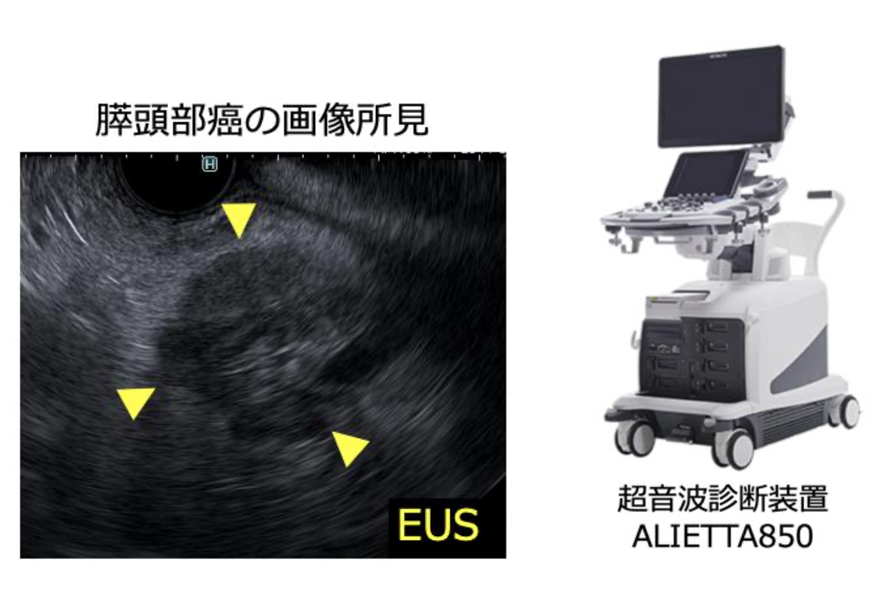
膵癌の画像検査としては腹部超音波検査やCT,MRI,超音波内視鏡検査(EUS)などがあります。EUSは内視鏡の先端に超音波プローブを備えており、胃や十二指腸などの消化管壁越しに膵臓や胆管などの周囲の臓器を調べる画像検査法です。EUSは空間分解能に非常に優れているため、大きさ1cm以下の微小な膵癌を検出することが可能です。そのため当院では膵癌高リスク患者さんに対して積極的にEUSを行っています。最近では最新型超音波診断装置を新たに導入し、膵癌早期発見のために日々検査を積み重ねています。
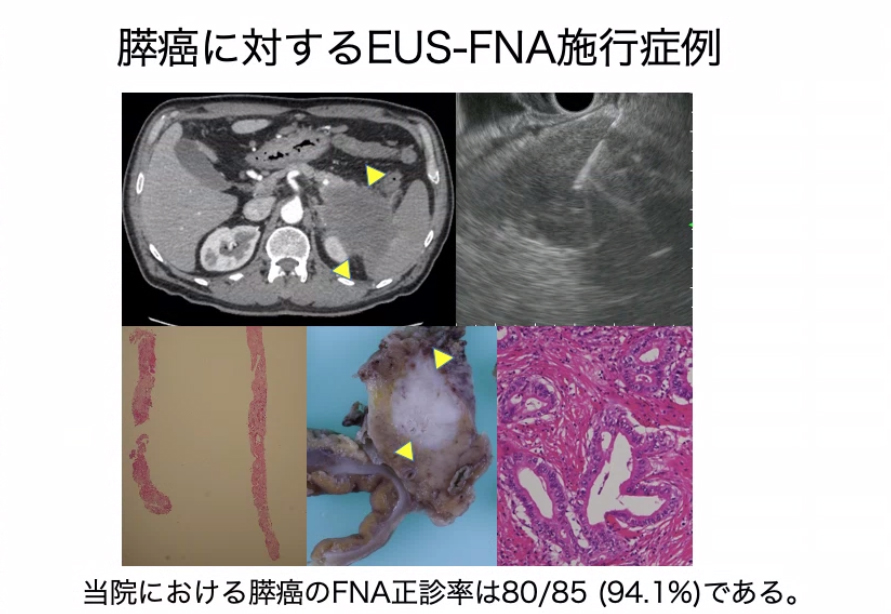
EUSを使用すれば胃や十二指腸から膵腫瘍に対して細い針を刺すことができ腫瘍細胞を回収することができます。この方法を超音波内視鏡下穿刺吸引法(EUS-FNA)と言います。EUS-FNAにて組織を回収し確定診断をおこなっていくことは腫瘍の治療方針決定に非常に有用です。
膵癌の治療方針の最終決定に関しては、消化器内科・外科・放射線診断科・腫瘍内科とカンファレンスを行い、最適な治療法を選択しています。近年、膵癌の治療法も進歩してきており、患者さんの予後や生活の質が改善するように努めています。

消化器病教室とは
慢性肝炎・肝硬変・肝臓癌などの肝臓病は、日本人に非常に多く「国民病」と言われてきました。特に、C型肝炎は、かつては非A非B型肝炎(A型でもB型でもない肝炎)と言われてきましたが、1989年にHCV抗体が測定されるようになってから、慢性肝炎・肝臓癌の60〜70%はC型肝炎が原因であり、日本人にはC型肝炎ウイルスのキャリア(保有者)が150〜200万人いることが明らかになってきました。そのため、慢性肝疾患をもつ患者さんや家族の方に、正確な病気の知識をもって、効果的な治療を受けていただくために「肝臓病教室」を平成19年に開始しました。その中で、インターフェロン(IFN)治療がC型肝炎を治癒させること、肝臓癌に対してもTACE/RFAなどの有効な内科的治療や外科的治療があること、肝臓病に関わる薬剤・栄養などを、医師・薬剤師・栄養士などの医療スタッフと患者さんが一緒に勉強する場として定着してきました。
しかし、消化器疾患は肝臓病以外にも、胃腸の病気・膵臓の病気など多岐にわたることもあり、テーマを消化器全体に広げた「消化器病教室」と発展させ、平成24年から2ヶ月に1回のペースで年6回継続開催しています。毎回、40〜60名の方に参加いただき、和気あいあいとおこなわれています。
消化器病教室の内容
教室のテーマは年間計画で決めています。最初に医師から病態の講義をおこない、その後、薬剤師から薬の話題、栄養士から食事の話題についてやさしく解説させていただきます。講義のあとには、参加者からの質問に答えるコーナーを設けており、毎回、いろいろな質問をお受けしています。病気に関する質問・治療に関する質問・担当の先生には聞きにくい質問・薬に関する質問・食事内容に関する質問など、各専門スタッフが参加者の疑問が解けるように丁寧にお答えしています。当院の患者さんでなくても、また家族の方でも参加自由ですので、気楽に加わってもらいたいと考えます。
会場は、病院一階の会議室です。24時間オープンしているコンビニの前にあります。費用は無料で、事前登録の必要もありません。
消化器病教室ページ臨床研究
臨床研究について
当科では、既存診療情報を用いた観察臨床研究を実施しております。観察臨床研究とは、直接の同意は頂かず、この掲示によるお知らせを持って同意を頂いたものとして実施されます。皆様方におかれましては研究の趣旨をご理解いただき研究へのご協力を賜りますようお願い申し上げます。
問い合わせがございましたら下記までご連絡いただきますようお願い申し上げます。
連絡先
神戸市立医療センター中央市民病院 消化器内科部長 神田 直樹
神戸市中央区港島南町2丁目1-1
TEL 078-302-4321(大代表)
臨床研究
| 研究課題名 | 当院責任者 | 承認日 | 説明文 (PDF) |
| 免疫抑制下におけるB型肝炎ウイルス再活性化リスクの予測と評価 | 神田直樹 | 2025/10/8 | |
|---|---|---|---|
| 胆道癌に対するがん遺伝子パネル検査の現状とFGFR2融合遺伝子陽性例の治療成績 | 丹家元祥 | 2025/7/24 | |
| 家族性大腸腺腫症患者における胃腫瘍に対するゲル浸漬下内視鏡的粘膜切除術の有用性に関する多施設遡及的検討 | 籔内洋平 | 2025/2/12 | |
| 血液中miRNA測定による消化器癌の診断法確立に向けた研究 | 和田将弥 | 2024/10/22 | |
| 当院での胃瘻造設術の現況と高齢者における合併症に関する検討 | 坂野利樹 | 2024/10/10 | |
| 20mm以下の表在性非乳頭部十二指腸上皮性腫瘍(SNADET)に対するconventional EMRとunderwater EMRの比較 | 押川大介 | 2024/8/23 | |
| 高齢発症潰瘍性大腸炎(UC)の臨床的特徴と治療選択に関する検討 | 押川大介 | 2024/9/25 | |
| 胃底腺型胃癌におけるリンパ節転移の危険因子に関する多機関共同後ろ向き研究 | 籔内洋平 | 2024/11/12 | |
| 切除不能胆道癌に対するGC療法とGCD療法の比較検討 | 秋山慎介 | 2024/7/17 | |
| 食道癌に対する化学放射線療法後遺残再発症例に対して内視鏡治療施行症例の検討 | 森田周子 | 2024/6/25 | |
| 未分化型早期胃癌に対する内視鏡的粘膜下層剥離術後の内視鏡的根治度C-2病変における転移・再発危険因子および長期予後に関する検討 | 籔内洋平 | 2024/11/12 | PDF 別紙PDF |
| 切除不能進行胆道癌に対するGCD療法の安全性と有効性に関する検討 | 秋山慎介 | 2024/3/29 | |
| 切除可能膵癌に対する至適な術前胆道ドレナージに関する検討 | 秋山慎介 | 2024/3/29 | |
| 急性下部消化管出血患者のクリニカルアウトカムの実態とその関連因子の解明:多施設共同後ろ向き研究 | 籔内洋平 | 2024/2/7 | |
| 胃腫瘍に対するゲル浸漬下内視鏡的粘膜切除術の治療成績に関する多施設後ろ向き研究 | 籔内洋平 | 2023/11/14 | |
| 当院における膵神経内分泌腫瘍に対する治療の現状 | 和田将弥 | 2023/5/2 | |
| 経乳頭的アプローチ困難時の悪性胆管狭窄に対する一期的経皮経肝的SEMS留置術の有用性 | 秋山慎介 | 2023/9/12 | |
| 食道内視鏡切除術の偶発症に関する全国調査 | 森田周子 | 2023/8/7 | |
| 膵癌による遠位胆道狭窄に対する経乳頭的胆道ドレナージ術の現状と課題 | 秋山慎介 | 2023/4/27 | |
| 切除可能膵癌に対する術前化学療法を含む周術期治療の検討 | 秋山慎介 | 2023/4/18 | |
| 膵腫瘍に対する超音波内視鏡下穿刺吸引生検 (EUS FNA) 後の穿刺経路腫瘍細胞播種(Needle tract seeding)の前向き全国調査 | 和田将弥 | 2023/2/14 | |
| 進行・再発食道がん患者の薬物治療体系と予後に関する観察研究調査 ~日本におけるリアルワールドと実地臨床の分析~ |
森田 周子 | 2022/12/26 | |
| 進行・再発食道がん患者の薬物治療体系と予後に関する観察研究調査 ~日本におけるリアルワールドと実地臨床の分析~ |
森田周子 | 2022/8/24 | |
| 膵腺房細胞癌の実態調査-多施設共同研究- | 和田将弥 | 2022/5/20 | |
| COVID‐19陽性入院患者における内視鏡施行症例の現状 | 安藤徳晃 | 2022/4/4 | |
| 内視鏡診断支援プログラムの胃病変検出性能検証研究 | 籔内洋平 | 2021/12/21 | – |
| 膵体尾部癌術前のEUS-FNABに伴うneedle tract seedingと予後に関する検討 | 秋山慎介 | 2021/11/17 | |
| 膵癌術前の悪性胆道狭窄に対する内視鏡的胆道ドレナージ治療戦略 | 秋山慎介 | 2021/11/17 | |
| COVID-19陽性患者における消化管出血の現状 | 安藤徳晃 | 2021/10/5 | |
| 膵癌による遠位胆管狭窄に対する術前胆道ドレナージの検討 | 秋山慎介 | 2021/8/20 | |
| 表在性非乳頭部十二指腸上皮性腫瘍に対するEMR、UEMRの現状と課題 | 秋山慎介 | 2021/2/2 | |
| 胃粘膜下腫瘍に対する腹腔鏡内視鏡合同手術の有用性 | 秋山慎介 | 2021/1/19 | |
| 後出血ハイリスク患者における ESD 後粘膜欠損の予防的縫縮術について | 長尾宗一郎 | 2020/8/26 | |
| 大腸ポリープ切除周術期における直接経口抗凝固薬(DOAC)の休薬期間に関する非盲検化ランダム化比較試験 | 森田周子 | 2020/6/27 | |
| 消化器内視鏡に関連した偶発症の全国調査 | 猪熊哲朗 | 2020/4/7 | |
| 当院における中・下咽頭表在癌に対する経口切除の現状 | 占野尚人 | 2020/1/10 | |
| 消化器内視鏡に関連する疾患、治療手技データベース構築 | 神田直樹 | 2019/12/3 | |
| ソラフェニブの治療効果を踏まえた分子標的治療薬による進行肝細胞癌治療戦略 | 鄭 浩柄 | 2019/7/30 | |
| 表在咽頭腫瘍における深達度の内視鏡診断 | 森田周子 | 2019/5/15 | |
| 壁深達度T4b症例の臨床経過 | 森田周子 | 2019/5/15 | |
| 超音波内視鏡下穿刺吸引生検法における膵腫瘤性病変の検体採取率について22G通常針と22Gフランシーン形状針を比較検討する多施設共同無作為化比較試験 | 谷口洋平 | 2018/3/13 | ー |
| 10㎜以下の十二指腸非乳頭部上皮性腫瘍に対するCold snare polypectomyの有効性および安全性に関する非ランダム化検証的試験 | 猪熊哲朗 | 2018/2/20 | ー |
| C型肝炎ウイルス(HCV)抗体陽性症例に対する当院の取り組み | 杉之下 与志樹 |
2018/1/20 | |
| C型肝炎ウイルス排除後の肝細胞癌発症を予測する臨床疫学的因子の検討 | 猪熊哲朗 | 2017/10/5 | |
| 上部消化管内視鏡検査におけるCricoid pressureの安全性と有用性の検討 | 猪熊哲朗 | 2017/7/20 | |
| ヘリコバクター・ピロリ陽性かつ早期胃癌ESD治癒切除後患者における、ピロリ菌除菌による異時性胃癌抑制効果を証明するランダム化比較試験 | 猪熊哲朗 | 2017/7/11 | ー |
| 80歳以上の早期胃癌内視鏡的粘膜下層剥離術施行症例における予後の検討 | 森田周子 | 2017/5/1 | |
| 再出血を来した原因不明消化管出血、小腸出血症例の検討 | 福島政司 | 2017/2/16 | |
| 上部消化管出血性病変に対して緊急上部消化管内視鏡を試行した症例の検討 | 森田周子 | 2016/10/25 | |
| 拾い上げ困難な食道癌症例の検討 | 森田周子 | 2016/9/1 | |
| 炎症性腸疾患患者に対するヘリコバクター・ピロリ除菌の安全性に関する後方視的検討 (SPIRAL study) |
北本博規 | 2016/4/19 | |
| 固形腫瘍における遺伝子異常の網羅的解析 | 猪熊哲朗 | 2015/8/1 | |
| 白血球除去療法(LCAP)を施行した潰瘍性大腸炎患者の予後およびその因子に関する多施設共同レトロスペクティブ観察研究 | 井上聡子 | 2015/7/1 |
お知らせ
医師、医師を目指す方向け当科のご紹介
2021年10月18日
※本コンテンツは、医師の方を対象とし、当医療機関についての理解を深めていただけるよう作成しているものであり、一般の方を対象とする宣伝・広告等を目的としたものではありません。
はじめまして、神戸市立医療センター中央市民病院 消化器内科の猪熊 哲朗(いのくま てつろう)と申します。
当科は、神戸市の基幹病院として、スタッフ9名、専攻医7名の計16名が、24時間体制で消化器疾患の急性期治療に従事しております。昨年度の年間入院患者数は新型コロナウィルス感染症の影響で2000名弱に減少しましたが、入院患者の1/3を緊急入院症例が占めております。
内視鏡診療には特に力を入れており、1階救命救急センター隣にある内視鏡センターでは、800㎡を越えるスペースに7室の検査室と2室のX線透視室を備え、広いリカバリーコーナーも設けています。検査後に十分な休息を取ることができるため、現在、ほぼ全例でセデーション(鎮静)下の内視鏡検査を受けてもらえるようになっており、約18000件/年の検査を実施しています。
今回は、最先端の機器と手技を駆使した内視鏡診療を当科の籔内 洋平副医長より紹介させていただきます。
副院長
消化器内科 部長
猪熊 哲朗
はじめまして、神戸市立医療センター中央市民病院 消化器内科副医長の籔内 洋平(やぶうち ようへい)と申します。
消化管内視鏡の領域は、日々進歩しています。診断においてはリアルタイムな組織学的診断が可能となりつつありますし、治療においては根治性は担保しつつもより低侵襲な治療法が模索されています。
本稿では、当院における内視鏡診療の取り組みをご説明させていただきます。
消化器内科 副医長
籔内 洋平(やぶうち ようへい)
<専門分野>
早期癌の内視鏡治療
<学会専門医・認定医>
日本内科学会 認定内科医
日本消化器病学会 消化器病専門医・指導医
日本消化器内視鏡学会 消化器内視鏡専門医
内視鏡検査の新常識 安全・安楽な検査を提供
従来より内視鏡検査は、苦痛を伴う検査の代表と言われてきました。
実際、過去に内視鏡検査を受けた患者さんから「あんなしんどい検査は二度と受けたくない」といわれたこともありました。しかし、検査時に鎮静剤・鎮痛剤を用いたセデーション検査を導入してからは、ほとんど、苦痛を訴えられることはなくなりました。患者さんによっては検査を受けた記憶もない方もおられるくらいで、不安なく受けてもらえると考えています。
その一方で、内視鏡に伴う偶発症(死亡例も含む)が最も多いのもセデーションに関連するものです。
そのため、当科では、検査中から検査後まで連続して生体情報モニターを集中管理・記録しており、血圧・SpO2の低下などにはアラームがなることで迅速に対応可能となっています。安全がしっかり担保されたうえでの、安楽な検査を提供しています。
最先端機器を駆使した早期がんの拾い上げ
医療の進歩は目覚ましく、消化器領域でも新たな治療・機器が次々と開発されています。
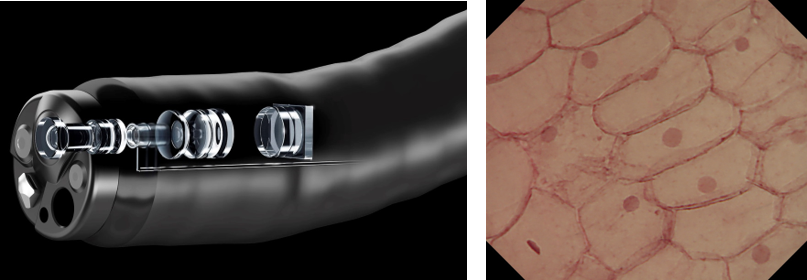
当科としても、最先端の医療を提供するという使命から、今年度、最大520倍の超拡大観察が可能な内視鏡「EndocytoⓇ(エンドサイト)」を導入しました。顕微鏡レベルの視野が生体内で得られるという画期的な機器です。
通常の拡大内視鏡では80倍の拡大観察が限界でしたが、超拡大観察では、微小な癌の診断率向上に加えて、組織を取らずに確定診断ができる可能性があります。
スコープ自体は外径9.7㎜と通常の内視鏡より細径であり、拡大ズームレバー操作だけで、通常から520倍拡大観察までが連続的に可能となっています。
細胞核まで観察できることは、細胞異型を評価することで、組織診断までできる可能性があります。昨今、抗血栓薬内服患者が増加しているなかで、生検組織診による出血のリスクを回避できるメリットもあると考えます。
超拡大内視鏡により粘膜細胞内の核が観察可能
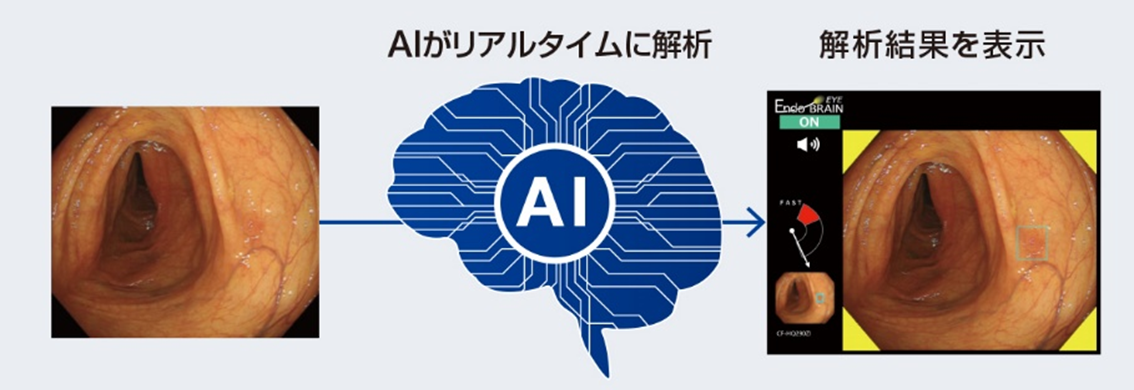
また、内視鏡初のAI診断支援システムである「Endo BRAIN-EYEⓇ」を全国の病院に先駆けて導入する予定です。AIを活用することで早期癌の質的診断・微小な腫瘍の拾い上げができると期待しています。
Endo BRAIN-EYEが検査中にリアルタイムに腫瘍を指摘
最先端の治療手技 全消化管における早期癌に対してESDが可能に
近年の内視鏡機器の発展に伴い、消化管全般において多くの早期癌がみつかるようになってきました。
これまでは外科手術の適応とされていた病変も、内視鏡的粘膜下層剥離術(ESD)の開発・進歩によって、病変のサイズに関わらず一括での切除が可能となり、良好な局所のコントロールおよび正確な病理学的評価が可能となっております。リンパ節転移の可能性が極めて低い病変に対しては根治が期待できることから、臓器によって多少の基準の違いはあるものの多くの早期癌に対して内視鏡治療が第一選択となってきています。
内視鏡治療は治療時の身体的負担が少なく、臓器機能の温存できるのが最大のメリットになります。当院では基本的に、治療前日に入院、治療日、治療翌日より飲水開始、治療翌々日より食事再開というパスで運用しており、5-7日程度で退院可能です
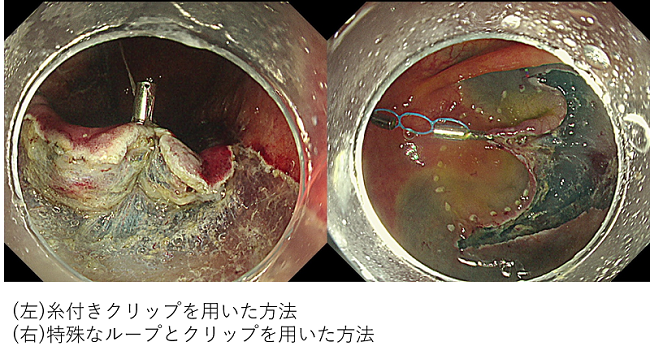
ESDは普及しつつある手技で標準的な病変は広く治療されていますが、病変部位やサイズによっては技術的難易度が高い病変が存在するのも事実です。内視鏡治療では、スコープから出せる一つのデバイスだけが武器になりますが、外科手術の時のように複数の手を用いて視野を展開できないというのがネックとなります。しかし、近年はこの問題を克服すべく、糸付きクリップを用いた方法や特殊なループを用いた方法によりカウンタートラクションをかけることが可能となってきております 。
カウンタートラクションの方法
また当院では国内の内視鏡治療のハイボリュームセンターで十分な研鑽を積んだ専門医が3名在籍しており、事前に十分なディスカッションおよび治療戦略を練ってから治療に望んでおります。
最近では高齢化社会の影響もあり、外科手術適応の早期癌と判断されても、術後のQOLの低下のリスクから外科手術を希望されない患者様もおられます。そのようなケースでは、根治性が外科手術より劣ることを患者様のご同意が頂ければ、内視鏡的切除のみを行って経過を見るという方針も選択肢として提示されます(相対適応としてのESD)。
少しでも内視鏡治療の可能性がないかなと思われる場合は遠慮なくご紹介ください。
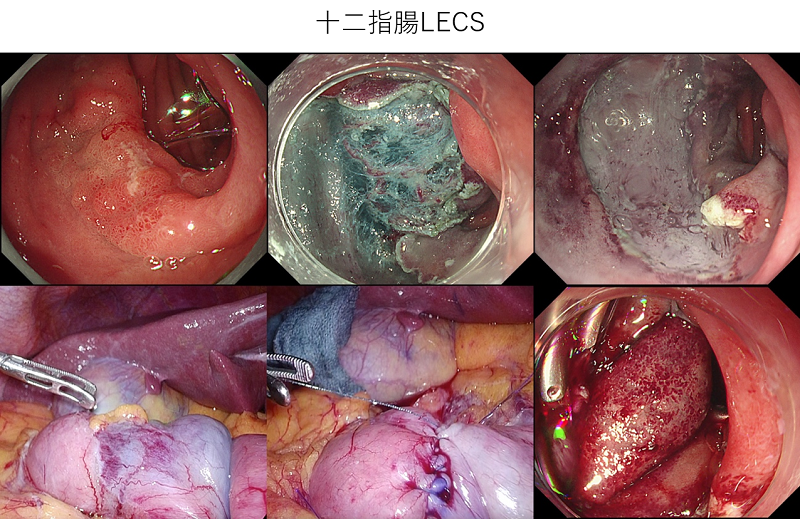
院内他科と連携し、消化管の入口から出口まで対応
当院では消化管の咽頭・食道・胃・十二指腸・大腸と入口から出口までの全消化管の表在癌に対して内視鏡治療を行っております。
咽頭部の病変に関しては、耳鼻科との合同治療を行っており、彎曲側喉頭鏡を用いた喉頭展開を行い、ESDのテクニックや、経口的に鉗子や電気メスを挿入し内視鏡補助下に上皮下層剥離を行うELPS(Endoscopic Laryngo-Pharyngeal Surgery)による切除を行っております。
また十二指腸の病変に関しては、その操作性の悪さや胆汁・膵液と言った消化液の暴露によって、ESDに伴う術中および遅発性穿孔のリスクが高いとされていることから、サイズや部位によっては安全性を担保し、外科の腹腔鏡と合同で行うLECS(Laparoscopy and Endoscopy Cooperative Surgery)による治療も行っております 。
大腸癌死亡を減少させるために -大腸癌検診とクリーンコロン-
食生活の欧米化(高脂肪・低繊維食)、肥満の増加、運動不足や飲酒、喫煙等の影響で、大腸癌は増加傾向にあります。
大腸癌は部位別予測癌死亡数(2020年)では男性で2位、女性で1位となっています。大腸癌は部位別予測癌罹患数(2020年)でも、男性で3位、女性で2位となっています。欧米と比べても、大腸癌による死亡率は、日本の方が高くなっています。欧米で大腸癌死亡数が減少した背景には、内視鏡を中心とした大腸癌検診が奏功していることが考えられています。
大腸癌は、早期に発見すれば根治できる病気です
早期発見・早期治療のため、大腸癌検診(便潜血検査)や内視鏡検査が有用です。
便潜血検査による大腸癌死亡減少効果は複数のRCTで証明されています。内視鏡検査による大腸癌死亡減少効果も複数の大規模コホート研究で示されています。
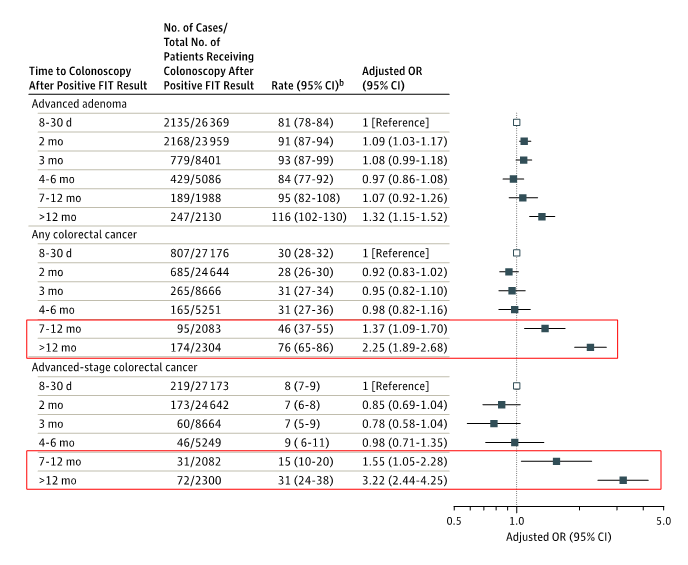
日本においては低い検診受診率および精検受診率が課題となっています。最近では、新型コロナウイルスのpandemicの中、患者の受診控えが問題となっています。海外からは、便潜血陽性であった際に、精査の内視鏡検査までの期間が長くなるほど、大腸癌が進行期にみつかり、大腸癌死亡リスクが上昇することが報告されています。
便潜血検査陽性から大腸内視鏡検査までの期間が長くなると大腸癌(特に進行癌)の割合が高くなる
当院ではコロナ対策と並行して、十分な感染対策のもと、通常診療を安心・安全に提供できるよう診療体制の整備に努めています。例えば、内視鏡検査前は、学会の指針に基づき、問診や検温による事前のリスク評価と検査時の個人防護具の徹底を行っています。
腫瘍性病変は日帰りで治療可能

全例で拡大機能付きスコープを用いており、拡大観察に基づく正確な治療前診断・治療選択が可能となっています。
10mm未満の低異型度腺腫であれば、cold snare polypectomy (CSP)とよばれる通電を行わない内視鏡切除を行うことが一般的となっています。高齢化に伴い抗血栓薬内服患者も増える中、出血リスクが低い、より安全な低侵襲治療が可能となっていますので、便潜血検査陽性となった患者様を積極的にご紹介頂ければ幸いです。
先生方へのメッセージ
昨年からの新型コロナウィルス感染症の蔓延で、多くの医療機関で診療制限がおこなわれていると理解しています。
当院も、感染症指定病院として兵庫県下の重症患者を受け入れるためコロナ臨時病棟を病院駐車場に建設し、現在まで1000名を超える患者さんの治療をおこなってきました。対応当初に発生した院内クラスターへの反省から、レッド(コロナ陽性)オレンジ(コロナ疑い)ホワイト(一般、コロナ陰性)の区別を確立し、一般患者さんの診療も安全におこなえる体制を確立しています。
また、緊急・予定入院の患者さんには、入院前にPCR検査を全例におこない、ウイルスの持ち込みもチェックしております。安心してご紹介いただきますよう、お願い申しあげます。
消化器内科専攻医の広場 Let’s Join Us!

当科にて、消化器内科専攻医3年間を経験した先輩(当院初期研修医2年間も経験した場合はその期間についても)から、消化器を志望する後輩へのメッセージを送ります。
T先生(H28-30:当科専攻医)(その後、手稲渓仁会病院に勤務)
当院消化器内科に興味を持っていただきありがとうございます。
私は総合診療・救急診療に力を入れている京都の洛和会音羽病院で2年間初期研修を行いました。そして、その後の進路として専門分野として何を選ぶのか、どの病院を選択するのかで大いに悩んだ結果、①救急を含めた豊富な症例数、②充実した指導体制、③モチベーションを維持できる環境、を条件として検討し決めました。3年間の研修を終えた後に振り返って思うと、最も希望にあった研修先であったと実感しています。
当院はメディアでも取り上げられていましたが、全国救命救急センター評価で5年連続1位を獲得しており、救急患者を連日多数受け入れていることから症例には事欠きません。他院では治療困難な症例が紹介されてくることはしばしばです。また他の専門科も有力であることから、「全身疾患の消化器病変」といった希少な疾患も経験することが可能です。しかし、単に数が多いだけでは自分が行っている治療が妥当なのか・最適なのかがわからず数に忙殺されてしまいます。当院では消化管・胆膵・肝臓・炎症性腸疾患(IBD)の各専門家が上級医におられることにより、適切な治療を最短で提供しつつ、きめ細やかな指導を受けながら自らの技術も向上させることが可能です。病院によっては専門家がいない、機器がない、経験が少ない等で行えない検査・治療もありますが、当院では全領域において満遍なく、実に多彩な専門的な検査・治療を実践し学ぶことができるのは最大のメリットであると考えます。3年間の専攻医研修で培った幅広い経験を基盤として、専門領域の研鑽を積む際により高みを目指すことができると思います。
また臨床と学術活動は両輪の様なもので、双方がバランスよく機能することによってお互いの能力がより高まると実感しています。地方会での発表に加え、国際学会や英語論文執筆などもチャンスは多数あります。興味深い症例は多く、指導医も積極的に関与していただけます。院内には学術支援センターも整備されており、環境は十分に整っています。忙しい臨床の中で立ち止まって、深く考え、学ぶための非常に良い機会だと思いますのでぜひ積極的にトライしてみてください。
道を決めるというのは非常に悩ましいものですが、一歩踏み出してみて初めて見える景色もあります。消化器内科としての第一歩を当院で踏み出せたことは、私にとって大きなアドバンテージとなっています。まずは見学で当院の専攻医がどういった研修・指導を受けているのかを実際にご覧になってください。
皆様にとって当院の研修が実り多いものとなることを祈っています。
M先生(H23-24:初期研修医、H25-27:当科専攻医)(その後、国立がん研究センター東病院に勤務)
私は当院で2年間の初期研修を行い、消化器内科で3年間の後期研修を行いました。後期研修を終えた今、当院消化器内科での研修の特徴をご紹介したいと思います。
第一の特徴として述べたいことは、消化器内科という多様な疾患を扱う領域にあって、非常にバランスの取れた研修を行うことができるという点です。消化器内科学は、臓器で大別して消化管領域と肝胆膵領域とに大別されます。ただでさえ扱う臓器が多い上、胃癌・大腸癌といった悪性腫瘍や慢性肝炎・炎症性腸疾患などの炎症性疾患といったように、様々な病態を対象としています。当院では各領域に精通した経験豊富なスタッフの先生方の指導のもと、偏りのないハイレベルな研修を行うことができます。症例数も非常に多いので、否が応でも偏りがなくならざるを得ない、という方が正しいかもしれません(笑)。消化器内科の代名詞とも言える上部・下部消化管内視鏡検査は言うまでもなく、ESD・ERCP・TACE・RFAといった治療も術者として積極的に携わることができます。例えばESDに関しては、後期研修の間だけでも50例以上を経験することができました。消化器内科医は内科としての知識だけでなく複雑な手技をこなす力も必要なため、これだけの経験を積むことができる環境は理想的だったと思います。
第二の特徴としては、3次救急までを扱う神戸市随一の総合病院として救急症例が非常に多いことです。吐下血や胆管炎といった内視鏡治療を要する病態から、重症急性膵炎や劇症肝炎といった内科的なマネジメントを要する病態まで幅広く経験することができます。最初は冷や汗をかきながら内視鏡を握るということもありましたが(笑)、上級医に助けて頂いたり他の後期研修医と協力しながら症例をこなすうち、心に余裕を持って対処できるようになったと思います。
第三の特徴としては、学会・論文発表などの学術的な面に関しても積極的な点です。私自身、地方会から総会、さらには国際学会といったように、徐々にステップアップして学会発表を経験することができました。多忙な臨床の合間に学術活動を行うのはきついこともありましたが、発表作成を通じて飛躍的に知識が身に付きますし、他の先生方とともに発表し終えた後の達成感は良いものです。
以上、当院消化器内科での後期研修の特徴を述べさせて頂きました。正直多忙な生活ではありましたが、自分が望めばいくらでも力を付けることができる環境だと思います。一人でも多くの方が当院の後期研修に来られることを楽しみにしています!
H先生(H23-24:初期研修医、H25-27:当科専攻医)(その後、静岡県立がんセンターに勤務)
当院の消化器内科専攻医研修では、数多くの消化器疾患症例を担当し、内視鏡検査・治療および病棟・外来診療などの業務に携わることができました。救急対応をする機会も多く与えられ、吐下血や急性腹症など多くの症例を直接経験することができました。1年目の初期から救急当番として同時に複数のコンサルトを受けることも多くあり、最初は困惑することも多かったと思います。しかしそんなときも一人で困り果てることはなく、周りの上級医や専攻医の先輩方に相談しながら、適切なアドバイスを頂き、対応を覚えていくことができました。専攻医としてすぐに初期対応を任されることで、責任をもって診療を行うことができ、日々実力を向上させていけます。また入院患者の主治医となることで、治療方針決定にも責任をもってかかわっていくことができます。治療内視鏡も数多く経験する機会が与えられ、最初は手取り足取りですが、徐々に任されるようになり、技術を磨くチャンスがあります。忙しく厳しい環境で、ときに挫けそうになりますが、周りの医師やコメディカルの方々に支えられながら研修を積んでいくことができます。3年間で入院、外来、救急を通じて、一般的な消化器疾患は一通り経験でき、ときに比較的まれな疾患も経験することができます。社会的な問題をかかえる患者も多く、社会的解決能力が求められます。
また消化器内科全体が学術活動にも熱心な雰囲気にあり、症例も豊富なため、地方会・総会、論文執筆や国際学会など幅広い学術活動が可能で、演者として数多くの学会発表を経験できる環境です。医師として人間としておおいに成長できる3年間になると思います。
K先生(H22-23:初期研修医、H24-26:当科専攻医、H27-28:当科スタッフ)(その後、京都大学消化器内科大学院に進学)
私は当院で2年間の初期研修を行い、その後3年間の消化器内科専攻医として専門研修を行って、さらに2年間任期付医師として消化器内科で勤務させていただきました。
それぞれの時期の経験を基にこの病院の特徴を書かせていただきます。
まず初期研修ですが、当院は全国的にも有数の救命救急センターであり、日夜救急患者さんを多数受け入れており、1次~3次救急まで幅広い救急症例に対応しています。設備環境・人員にも恵まれた環境で診療レベルが高いことから、救急症例に限らず他院で診療困難な症例に関しても広く受け入れており、急性期~慢性期の病態に対して適切な診断と診療を行うことが可能です。このような医療水準の高い環境で医師としての第一歩を経験することは、医師としての基礎を築く上で重要なことだったと思います。私は内科重点コースとして全内科を比較的長めにローテートしましたが、common diseaseから稀少疾患まで多くの症例を経験させていただき、内科医としての素養を身に着けることが出来て、以降の専門研修においても役に立ちました。
次に専門研修としての消化器内科専攻医の時期ですが、研修の初期から主治医として担当患者さんの診療を行い、検査・治療から退院に向けたマネジメントまで主体的に行っています。原則救急症例は断らない病院であるため、病床運営に逼迫することもあり、検査や治療を無駄なく進めていくこがを求められるため、自然と先を見越した動きが出来るようになり、患者さんの病状を見極める感覚が養われました。実際の診療については、消化器内科は内科の中でも手技も必要となる科ですが、症例数が非常に多いことから基本検査・治療/特殊検査とも非常に多く、手技の研鑽の上で他の専攻医と症例の取り合いになることはありませんでした(むしろ嫌というほど経験出来ます)。救急症例に対する緊急検査も上級医の先生のサポートの元、的確に行っておりますので、日に日に自分の能力が向上していくことを実感出来ました。
多くは専攻医を終了した時点で他院に異動となるのですが、私は医員の枠の関係で幸運にも残留することができたので、専攻医終了後に2年間さらに当院で勤務しました。専攻医までは消化器内科領域全般を経験していましたが、任期付医師の期間では自分の専門領域に一歩踏み込んで診療を行うことが出来ました。専攻医の期間に幅広い症例を経験した中で、私は炎症性腸疾患や小腸疾患の診療に興味を持ったため、残り2年間では小腸内視鏡の技術の向上に充てることが出来、専門領域の基礎を作る上で良い経験が出来ました。
また当科は学術研究にも非常に力を入れており、国内・海外の学会で多数発表させて頂きました。始めは発表のスライドもどう作れば良いかわからない状態でしたが、場数を踏むうちに抄録作成・発表のコツもつかむことが出来て、総会レベルの主題にも採択されるようになりました。論文も在籍中に3本執筆出来ましたし、やる気があれば可能性はいくらでもある施設だと思います。
以上のように当院での経験を積んだ後、現在は京都大学の大学院に進学しております。当院での研修により消化器内科としての基礎が出来た後は、さらに専門領域を深めることを目標とされる先生方が多く、私のように大学院に進学したり、がんセンターに行って研鑽を積むことが多いようです。京都大学の関連病院でもあるため、関連病院間での異動も比較的融通が利くので、消化器内科全般の経験をさらに積みたいという方も路頭に迷うことはないでしょう。忙しい病院ではありますが、ここでしか経験出来ないことも多数ある恵まれた環境ですので、やる気に満ち溢れた先生方は是非一度見学に来てみて下さい!
O先生(H21-22:初期研修医、H23-25:当科専攻医)(その後、日赤和歌山医療センターを経て、京都大学消化器内科大学院に進学)
私は当院で2年間初期研修を行い、その後3年間の後期研修を経て、現在は大学で基礎研究を行っています。当院での研修を振り返って、初期・後期研修の特徴を紹介させていただきます。
初期研修の特徴は「市中病院と大学病院両方のいいとこどり」です。
当院の救急外来は小児から大人まで、一次から三次救急まで対応しているため、来院する多くの患者さんを診察し、様々な病態に対応する力をつけることが出来きます。一方、当院には多くの優秀な指導医の先生のもと、大学病院レベルの診療が行われており、内科・外科ローテーションでは大学病院でしか経験しないようなまれな疾患に対してどのように診断・治療するべきかを学び・実践することが出来ます。つまり、様々な病態の豊富な症例を経験できるとともに多くの優秀な指導医のもとで大学レベルの診断・治療を実践できるという「市中病院と大学病院両方のいいとこどり」ができます。
後期研修の特徴は「豊富な症例」「多くの仲間」「学術研究」です。
当院の最大の特徴は「豊富な症例」です。豊富な症例を通して様々な手技を経験することで多くの知識・技術を身につけることが出来ます。「百聞は一見に如かず」といいますが、学んだり聞いたりしただけでなく、その症例を目の当たりにすることで得られる経験は何ものにも代えがたいと思います。
2つ目の特徴は「多くの仲間」がいることです。当院には後期研修医が多くいるため、お互いを刺激しあい切磋琢磨することができます。さらに先輩後期研修医がしていることを見て、自分が実践し、後輩に教える、つまり「see one, do one, teach one」を実践することで知識・技術を学び、身につけ、定着させることが出来ます。もちろん、各分野に精通したスタッフが後期研修医たちをしっかりと支えてくれるので安心です。一方、後期研修が始まると主治医として患者さんを担当することとなり、主治医としての責任感から重圧や悩みも多く生じます。その時に同じ環境にある仲間がいて、気持ちを共有し、励ましあえたのは非常にありがたいことでした。なお、多くの後期研修医がいることによって経験できる症例や手技が減るのではないかという懸念が生じますが、その心配は全くないので安心してください。
最後に3つ目の特徴として「学術研究」を挙げたいと思います。豊富な症例や特異な疾患の経験を世界に発信することは自分のためだけでなく、医療の発展にも重要なことでありますが、当院は病院全体で臨床研究や学会・論文発表などを支援してくれる制度があります。この制度を利用することで非常に発表がしやすい環境にあります。
初期も後期も日常診療に追われ、あっという間に過ぎてしまいましたが、後から振り返ると非常に充実した日々だったと感じます。他の病院に赴任した時に自分の今まで積んできた知識・経験が生きていることを実感し、今まで進んできた道が間違っていなかったと思えます。
当院での研修の魅力はこれ以外にもたくさんありますが、書ききれないのでぜひ見学に来ていただけたらと思います。多くの方に当院での研修を希望していただけたら幸いです。
M先生(H20-21:初期研修医、H22-24:当科専攻医)(その後、京都大学消化器内科大学院に進学)
私は当院で2年間初期研修を行った後、そのまま消化器内科の後期研修医(専攻医)として専門研修を開始しました。後期研修医として当院に残る道を選んだのは、コンサルタントとして何でもバリバリと処置をこなす先輩後期研修医たちの姿が、救急外来で働く初期研修医の立場から見て、非常に生き生きと充実した研修を送っているように見えたからでした。実際に私自身が後期研修を経験した中で実感している当院消化器内科の特長をいくつか紹介します。
一つは、当科では、従来より、後期研修医がメインとなって診療・処置に当たる風土が整っているという点です。例えて言うと、上級医という大船に乗って穏やかな海を航海するような「上級医について教えてもらう」研修スタイルではなく、自らが船頭となって荒波にもまれながらも何とか進んでいく研修スタイルに近いです。もちろん、上級医の先生方から日々いろいろと指導していただきながら、ということは前提ですが、自分で悪戦苦闘しながら得た知識・技術は、ただ教えてもらうだけの何倍もの早さで身についていることが実感できます。特に処置については、一定の土台が出来た後には、上級医の先生に見守っていただきながら「まずはやってみろ」と言っていただける環境は、これから消化器を学びたい人にとっては非常に恵まれた環境といえます。
二つ目は、当院全体の特長とも言えることですが、当院は救急に力を入れていると同時に、high volume center、高度医療を行う医療機関として、神戸市内はもとより、周辺地域からの救急搬送・紹介受診が多く、症例を豊富に経験できるという点です。消化器内科でも吐下血や胆管炎など、緊急対応を要する症例が毎日のように搬送されてきて、仕事としては大変な部分もありますが、緊急内視鏡止血術などの修練もたくさん積むことができます。実際、私自身も当初の1年間で、上部内視鏡800件以上、下部内視鏡300件以上(いずれもそのうち約1割は緊急内視鏡)と、一般の病院での消化器内科研修3年間分にも匹敵するほどの内視鏡を経験することができています。また、処置や緊急だけでなく、一般の施設ではなかなか経験できないようなまれな疾患・重篤な病態も多く経験できます。
他にも、肝癌に対する肝動脈塞栓療法・ラジオ波焼灼療法などIVR治療も消化器内科が主体的におこなっており、後期研修医のうちからERCPやESDまで研修をできるなど、非常にactivityの高い環境の中で密度の濃い研修を行うことが出来ます。一人でも多くの仲間と一緒に切磋琢磨できることを楽しみにしています。
A先生(H14-15:初期研修医、H16-18:当科専攻医)
専攻医研修についての感想
消化器内科専攻医研修では数多くの消化器疾患症例を主治医として受け持ち、検査・診断・治療に至るまで責任を持って診療にあたることができるのが魅力だと思います。すべての症例について消化器内科カンファレンスを毎週行っており、治療方針の決定について主治医がプレゼンテーションを行った上でdiscussionを行い、最良の治療法を提供できるようにしております。消化器内科は検査が多くある診療科であるため、身につけなければいけない手技が数多くあります。この点についても経験の浅い間はスタッフの指導を受けながら行いますが数が多く経験できるので上達も早いです。技術が上達すれば自立して行っていくスタンスを持っているので、日々実力が向上しているのが実感できる研修生活を送ることができます。特徴として消化管領域は上下部内視鏡やESDやダブルバルーン小腸内視鏡検査も多く行っている他、胆膵領域は結石や癌症例も多くERCP件数は豊富で、肝臓領域は肝臓癌治療で肝動脈塞栓術やラジオ波焼灼術/PEITも消化器内科主治医が行っているので総ての消化器内科疾患を専攻医の間に一貫して診療できることです。外科ともカンファレンスを行っており、協調した診療が行われているのでレベルが高く、外科治療適応症例についても深く学ぶ機会に恵まれています。また一次から三次救急まで受け入れている地域中核病院であることから、消化器内科救急が特に数多く経験できるので緊急症例の判断・処置に強くなります。移植外科では生体肝移植も行われていることもあって深く幅広い自己完結型の消化器診療を経験できます。その後の進路決定への選択についても興味のある症例に必ず巡り会えるので三年間の間にじっくりと考えられると思います。恵まれた環境にあって専攻医研修期間過ごすことができて、そこで得られた経験と技量と自信は他で得難いものであったと外に出てからもより実感できました。
初期研修についての感想
当院の初期研修は様々な症例を数多く主体性を持って経験できることが最大の特徴であると思います。特に初期研修の2年間を通して研修する救急外来当直業務においては、一次救急から三次救急患者まで受け入れているので多忙な救急外来を経験することとなりますが、おのずと勉強することになり様々な経験を通して知識や小児の点滴から挿管にいたるまでの手技も身につけられるようになります。当直中は各専門領域の当直医が控えているので安心して当直できる上、コンサルトを行えば適切な指導を受けることができます。院内には内科カンファランスや剖検検討症例会(CPC)が定期的に行われているので院内外の症例発表を経験して勉強する機会にも恵まれていると思います。また同期の研修医がたくさん入るので仲間が多く、救急外来では屋根瓦方式による指導が行われているので上下の研修医仲間とのつながりも強くなります。私も他で得られない大変実りある充実した初期研修期間を送ることができて医師として成長させてもらえたと思います。どの科に進む如何に関係なく、医師としてのスタートダッシュを切りたいと考えている方や多くの研修医仲間とともに充実した研修を始めたいと考えている方にはおすすめの病院と考えます。研修医の熱気あふれる姿勢が患者さんから信頼あつい市民病院として安心した診療を提供できている神戸市立医療センター中央市民病院を支えていると実感できると思います。
素材提供:ホスピタルカフェ
T先生(H13-14:初期研修医、H15-17:当科専攻医)
専攻医研修についての感想
消化器内科後期研修(専攻医3年間)で優れている点を尋ねられたら、私は迷わず“豊富な症例数と充実した指導体制”と答えます。当科の研修では、消化管領域、肝胆膵領域ともさまざまな症例を経験することができます。また、症例数が多いゆえに、短期間で内視鏡をはじめとした検査技術を経験・習得することができます(具体的には、消化管領域では、上下部内視鏡検査のほか、消化管出血に対する止血術、静脈瘤治療、EMRまたはESD、ステント留置術など、肝臓領域では、肝生検や肝癌に対するRFA、TAE、リザーバー留置術など、胆膵領域では、ERCP、ENBD、IDUS、PTCD、metallic stent留置術など)。また、中でも緊急処置が必要な救急疾患が非常に多く、専攻医はfirst callとして昼夜を問わず処置に入ります。もちろん最初は指導医の先生に手取り足取り教えてもらいながらですが、他の病院と比べると比較的短期間で独り立ちできるように思います。というのは、特に専攻医1年目は呼び出される回数も多く、この間にほとんどの消化器救急疾患を経験するため、必然的に内視鏡をはじめとした処置の技術が身につくからです。
2年目以降は、患者さんの検査・治療計画を自分で立案しつつ、検査・処置の腕にさらに磨きをかけることになります。私の場合、胆膵領域の疾患に興味があったため、特にERCPやPTCDなどの検査を積極的に参加させてもらいました。また、自らのスキルアップに努める一方で、ローテーションで回ってきた研修医の教育、後輩専攻医への指導も行います。
症例が豊富なため、地方会・総会などで幅広い学会活動が可能です。また、救急オープンカンファレンスで研修医対象の講義を行ったり、また患者さんや家族を対象とした講演会を開催したりするなど、消化器疾患の教育・啓蒙活動にも積極的に関わることもできます。
消化器内科は、疾患の守備範囲が広いため、幅広い知識が必要になります。将来的に臓器別専門医を目指すにしても、消化器内科医を名乗るからには、各領域の疾患に精通しておく必要があると考えます。忙しい科ですが、それゆえに内科の中でも他の科にはない面白さ、やりがいがあると思います。
そんな消化器内科での3年間の後期研修は非常にハードです。プライベートな時間がほとんど取れない時期もあります。しかし、この3年間、全力投球で打ち込むことにより、消化器内科医としての、また臨床医としての基礎を確実に築き上げることができると思います。先輩として高い志をもつ方、やる気のある方の参加をお待ちしています。
初期研修についての感想
私が初期研修医になった頃は、まだ新臨床研修制度が施行される前でした。当時は研修医を公募する病院も今ほど多くはありませんでしたが、私は「救急医療を通じて充実したプライマリケアの研修を行う」ことを第一条件に、研修病院を探していました。そんな時、一次から三次まですべての患者さんを受け入れる中央市民病院の救急現場を見学し、現場で働く研修医のレベルの高さに非常に感銘を受けました。このことがきっかけで、中央市民病院を研修先に選ぶことになったのですが、実際の研修内容は期待をさらに上回るものだったと言えます。
まず1年次の最初から6ヶ月間、救急・麻酔の研修に携わりましたが、最初の2ヶ月は予想していたよりもハードな毎日でした。失敗を繰り返し、その度に上級医の先生から叱責を受け、何とか見返してやろうと必死にがんばっていたのを覚えています。しかしこの時期を乗り越え、3ヶ月目くらいになって、臨床の面白さが実感できるようになりました。分からないことは2年目の研修医の先生や救急部および各科の指導医の先生から直接指導を仰ぎ、ためになる症例は同期の研修医仲間で分かち合う。毎日その繰り返しです。そのうちに、自分に実力がついていくのがはっきりわかるようになります。
2年目になると、今度は新しく入ってくる1年目研修医の指導が求められます。教えることは自分の持つ知識の整理にもなりますので、教える側も教わる側も成長するのです。また、救急当直では2年目がサブリーダー的な役割を担いますので、救急外来全体の状況を把握する必要があります。例えばWalk-inの待ち患者さんの中に重症の方がいないかチェックしたり、すでに診察を受けておられる患者さんのassessmentやplanが正しいかどうかをfollowするなど、さらなる広い視野が求められます。こうした役割を通じて、臨床医としての能力がさらに培われていくのです。
初期研修医時代の2年間、当直も含めて、本当にいろいろな患者さんたちを診させていただきました。心筋梗塞、脳血管障害、多発外傷などの3次救急症例は何度も経験させてもらいましたし、腹痛を主訴に来院された女性が救急外来で分娩するという貴重な経験もしました(本人も妊娠には気づいていなかったようです)。
このようにして救急部で培われた経験は、その後の(当時でいう)内科ローテーション研修でも十分生かすことができたと思います。中央市民病院には、救急領域に限らず本当に豊富な症例が集まってきます。各科を回るのは短い期間でしたが、それぞれの科の特徴を捉えることができました。また、さまざまな疾患の患者さんに接し、密度の濃い研修を受けることができました。その後専門課程に進んだ今の自分にとって、この内科研修の経験こそが今の診療の大きな支えになっています。
臨床研修は、どこで行っても10年経てばみんな一緒になる、という考え方があります。しかし個人的には、研修医時代にどのような経験をするかが、その後の医者としての成長に大きな影響を与えると考えます。中央市民病院には、研修医時代に是非とも学んでおきたい、いや学ぶべきものがたくさん詰まっています。興味のある方は、まず一度見学にいらしてください。そこで何かを感じ取ってもらえたらと思います。
S先生(H12-13:初期研修医、H14-16:当科専攻医)
専攻医研修についての感想
専攻医としての3年間の研修を通じてとても良い経験となったのは、腹部疾患の救急症例を数多く経験できたことでした。専攻医は夜間休日の宅直を担当しており、吐下血や急性腹症などの緊急症例を多数コンサルトされる立場にあります。(現在は、平日夜はスタッフ全員分担による消化器内科当直、休日は専攻医とスタッフによる宅直体制です)思い返すと、一晩に吐血患者1例と下血患者2例が同時に来院したことや、内視鏡的止血術を1例終えた直後に、急性膵炎の症例をコンサルトされるということもあり、非常に多忙な毎日でした。体力勝負のようなハードな一日もあり、デスクに座って教科書をゆっくり勉強するような時間はなかなかありませんでしたが、自らが経験した事柄の一つ一つが実になっていくような充実した3年間でした。また、コンサルトされた専攻医が孤立無援で困るようなことはなく、上級医の先生にはいつでも相談できたことが、研修施設として恵まれた環境であったと思います。このように、初期対応を任されることで、どこからどこまでを自分が責任を持って診療できるか、どこからは応援が必要かを考えながら対応し、次第に自分にできる範囲を広げていくという段階を経た研修ができました。
また数多く症例を経験できることが、診断学や技術を習得するうえで大変役に立ち、一般的な消化器疾患は、3年間でほぼ経験できました。なかでも慢性肝炎、肝硬変の通院患者が多いことから、食道胃静脈瘤破裂や肝癌破裂の救急患者を多数経験できたことは、他の施設で働くようになった現在、貴重な経験となっています。そして、地域の中核的医療施設であることから、比較的稀な疾患を担当する機会も多く、他の医師の担当症例であっても、カンファレンスなどを通じて症例を共有できた点についても特筆に価します。スタッフの先生方は、専門領域に関する造詣が深く、専攻医を終了して数年が経過した今振り返ると、いただいた助言はもちろん、日常会話の中での耳学問も含めて今の自分の診療に活きていると実感します。
具体的な技術面については、内視鏡、腹部超音波、血管造影、胃透視などの各検査を偏りなく経験し、自分の技術として習得することができました。現在は血管造影や胃透視を自分で行うことがない施設で働いていますが、専攻医時代に習得した経験が診療全般にとても役に立っています。またESDや、ダブルバルーン小腸内視鏡、EUS下穿刺細胞診などの専攻医にとっては発展的な診断治療技術についても携わることができ、良い経験となりました。最後に、消化器内科全体が学会発表に熱心な雰囲気にあり、演者として発表する機会に恵まれた点も、後期研修として良い環境であった思います。
初期研修についての感想
各科で充分な症例数を担当することができ、特に急性期症例や重症例を多数経験することができました。特にICUが充実しており、重症例についての全身管理を学ぶよい経験ができました。また週1回の内科カンファレンスでは、稀な疾患や診断治療に難渋した症例などを各科の研修医がそれぞれ持ち寄り提示するので、とても勉強になりました。救急当直は忙しく厳しい研修でしたが、1次から3次救急まで経験でき、救急を専門とするスタッフや専攻医の指導のもとで研修できたことと、常に複数の研修医が当直し、お互いに刺激しあって切磋琢磨することができたことが、非常に良い環境であったと思います。
我々は、学会発表も重要な診療活動の一環と考えています
貴重な症例・興味深い病態・治療での工夫など、自らが経験・学習したことをまとめて発表することで、知識の整理と共有が可能となります。また、学会発表によりプレゼン能力に磨きをかけることが期待されます。専攻医は、消化器関連学会での発表を通じて、一人前の消化器内科医に成長することが期待されます。
当科は、近畿の臨床病院としては最も多くの学会発表をおこなっている病院のひとつです。
以下に、当科スタッフの学会発表感想記を紹介します。
T先生(H26〜:当科スタッフ)
学会の概要
| 参加学会 | Digestive disease Week 2017 (DDW2017) |
|---|---|
| 開催地 | シカゴ、米国イリノイ州 |
| 開催日程 | 2017年5月6日~9日 |
参加学会での出来事と感想
DDW2016(サンディエゴ)に引き続き、今年も2017年5月6日〜9日までの4日間、Digestive Disease Week 2017(DDW 2017)に参加しました。今回は、米国イリノイ州シカゴのマコーミックプレイスで開催されました。DDWは消化器関連の学会では世界最大規模の学会であり、「アメリカ消化器内視鏡学会(ASGE)」、「アメリカ消化器病学会(AGA)」、「アメリカ肝臓病学会(AASLD)」、「アメリカ消化器外科学会(SSAT)」の4学会が共同で開催します。
まず、驚かされたのが学会の規模です、会場となったマコーミックプレイスは東京ビックサイト(日本最大)の3倍の広さがあり、発表内容も消化器関連の研究、最新の技術、医薬品についてと多岐にわたる内容が発表され、非常に刺激的な学会でした。また、演題は世界中から集まり、今回私の演題は「Cross-wired metallic stent in endoscopic bilateral stent-in-stent placement for malignant hilar obstruction」というもので、肝門部悪性胆管狭窄に対してステント治療に関するものでした。発表に関してはポスター発表であり、決められた時間中はポスターの前に立ち、直接質疑応答を行います。毎回、国際学会に参加すると自分の英語が未熟なのを痛感させられるのと同時に、今後の英語学習のモチベーションにつながります。
また、学会のオプションとしてシカゴでは野球観戦を行い、MLBのシカゴ vs NYヤンキースの試合を見に行くことができ、また世界的に有名なシカゴ交響楽団の演奏も聞きに行くことができました。
今回、学会を通じて世界の最先端の治療や研究が見ることでき、また日本ではなかなか体験できないことも経験することでき有意義な時間を過ごすことができました。
H先生(H25-26:初期研修医、H27-29:当科専攻医)
学会の概要
| 参加学会 | 欧州消化器病週間 2016 (UEGW2016) |
|---|---|
| 開催地 | ウィーン、オーストリア |
| 開催日程 | 2016年10月15日~19日 (専攻医2年目) |
参加学会での出来事と感想
UEGWはヨーロッパにおける消化器分野の国際学会で毎年10000人以上の参加者が集まって開催される巨大な学会です。そもそも学会に参加したきっかけは、ウィーンというおしゃれな街に行ってみたいという不純な動機でした。2016年1月頃から上級医の先生と国際学会で発表できるような演題を相談し、慣れない英語に悪戦苦闘しながら2016年4月の演題登録の締め切りに何とか間に合わせました。7月に採択通知が届き、そこから毎日のように宿泊予定のホテルを眺めたりウィーンの観光情報について調べたりして10月の学会本番を迎えました。
学会は5日間の日程となっていますが、初めの2日間が教育講演、残り3日間が一般演題という構成となっています。学会の参加者を地域別に見てみるとヨーロッパ大陸が65%、中東・アジアが17%、アメリカ大陸、南米大陸、アフリカ大陸からそれぞれ5%となっており、国別に見ると日本は5番目に参加者が多くアジアの中で最多でした。日本からの発表の大半ががんセンターや大学病院からのもので当院のような一般病院からの発表者は少数でやはりアウェー感がありました。
学会の内容としては日本の学会と同様で、朝から夕まで様々なセッションがいくつかの会場ごとに平行して行われています。ランチョンセミナーはなく昼食の時間になると、ケータリングのサンドイッチと水、りんごなどの果物が会場の定められた場所に運びこまれ、参加者が自由にそれらを取って食べるという点が斬新でした。ポスター発表に関してはポスター展示場で朝から夕まで掲載されており、昼間の12時半から13時半までポスター発表者がポスター脇に待機しておりポスターに関する質疑応答を行うというもので日本のように参加者全員がポスターを口演するというものではありませんでした。僕自身の発表内容はややマニアックで、幸い困難な質問もなく乗り切ることが出来ました。
学会終了後は、(これが今回の一番の楽しみでしたが)体力の許す限りウィーン観光やオーケストラ鑑賞を行いました。ウィーンはリングと呼ばれる中心地周囲に観光名所が集まっておりいずれも徒歩やトラムという路面電車、地下鉄で回れる手頃な広さであり、短期滞在ながら大半の観光名所を見学することが出来ました。
初めての国際学会で緊張しましたが、ウィーンという街が素晴らしかっただけではなく、自分より少し上の世代の日本の医師達が、シンポジウムやワークショップで学会場の檀上に立ち、欧米人の前で堂々と発表している姿を見て非常に刺激を受け改めて英語力の必要性を痛感しました。1週間ほど病院を留守にしましたが、科内の先生方には快く学会に送り出して頂き非常に感謝しています。
I先生(H24-25:初期研修医、H26-28:当科専攻医)
学会の概要
| 参加学会 | Digestive disease Week 2016(DDW2016) |
|---|---|
| 開催地 | サンディエゴ、米国カリフォルニア州 |
| 開催日程 | 2016年5月24日~27日 (専攻医3年目) |
参加学会での出来事と感想
米国で毎年開催されるDigestive Disease Weekは、世界中から最新の基礎や臨床研究の演題が集まる権威ある消化器病の学会である。2016年は5月24日から27日まで開催され、特に24・25日は休日でもあったことから多くの参加者で賑わっていた。毎日、各専門領域ごとに発表があり、朝は8時から夕方まで、昼休憩には多数のポスターセッションで熱心な討論が行われていた。今回、私はポスターセッションで24日に「トルバプタンに関する治療効果予測因子」、また26日には「十二指腸ステントに関する演題」と幸運にも2つの発表を行うことができた。
DDW2016では、北米・欧州・アジア諸国からさまざまな最新の研究が演題として採択され、連日興味深い発表を目にすることができた。日本国内には使用されていないデバイスや治療法などは大変新鮮であり、ぜひ導入したいと思ったものも幾らかあった。国内の学会よりも討論が活発に行われており、どのセッションも非常に充実したものとなっていた。ポスターセッションでは2演題発表する場をいただき、大きな経験となった。トルバプタンの発表では南米や中東の国の医師も興味をもってみていただき、国内とは違った観点からの質問も頂いた。また、十二指腸ステントの発表ではインド人の医師と積極的に討論を行い、ステントの選択、留置の方法などの考え方が日本のそれとは全く異なるものであることがわかった。当方のよいものは継続しながら、そこに新しい手法を取り入れることで各々の治療をより洗練されたものにしていきたい。また、共通の言語は英語であり、自分の言いたいことや考えを正確に伝えることができるよう、英語での伝え方をもっとうまくできるようにしなければならない、と会期中はたびたび感じた。今回DDWは初めての参加であったが、いろいろな普段と違ったものに触れることができ大変勉強になった。そして、今回学んだことを実地臨床に役立てていきたいと思う。

平成30年春から、内科専門医研修プログラムがスタートします。
当院も基幹施設として各領域の内科専門医の養成を図るプログラムを開示しますので、病院HPを参照ください。
消化器内科の方針としては、1年目のスタートより4ヶ月間はサブスペ(消化器)研修にあてており、この期間に消化器の基礎・内視鏡検査などの基本手技を学んでもらいます。その後、基本領域研修に入りますが、各領域の症例を規定数担当してもらい、内科医としての視野を広げることを目標とする一方で、サブスペ領域の経験が空洞化しないように業務面での配慮をしています。2年目は院外研修期間となりますが、連携施設は神戸市立医療センター西市民病院、西神戸医療センター、兵庫県立尼崎総合医療センター、日赤和歌山医療センター、天理よろづ相談所病院、大津赤十字病院など京都大学消化器内科関連病院で、サブスペ領域主体の研修をおこないます。3年目は専攻医最終学年として当科にて診療の主力を担ってもらう予定です。
消化器領域は、多くの症例を経験し、多くの手技をマスターすることが重要ですので、ハイボリュームセンターの利点を十分活用して、3年計画で一人前の消化器内科医を育てることを目指します。
1.実戦(実践)主義
当科の最大の特徴は、実戦(実践)主義にあります。教科書的知識は基礎として非常に大切であることはいうまでもありませんが、実際の臨床現場では、むしろ教科書どおりにはいかないことや教科書のどこにものっていないことが、頻繁に起こります。目の前で苦しんでいる患者さんを救うために医療は存在するのであり、人間は理論(時にエビデンス)で割り切れるほど単純な存在ではありません。そういった点で、医学は学問でありながら実学ともいえます。我々は、経験を最も大切なものと考えます。実際の患者さんを救うために、悩み学び努力した結果が、医師個人の実力を高めるのはもちろん、消化器内科グループ全体からひいては病院全体のレベルを上げると考えます。我々と一緒に、実践の現場で汗を流しませんか。
2.マンツーマン指導体制
たとえば、最初からいきなり胃カメラ検査ができる人などいません。もちろん、そんなことをしてもらっては困ります。まず、検査の意義・病態の理解・診断学・機器の取扱方法等を学習した上で、上級医の指導の下で検査の修得を目指します。新人医師が汗だくになって検査をしているうしろで、指導医も手に汗をにぎりながら立ち会います。不安になって振り向いて目があった瞬間に適切な指導が得られるでしょう。決して、手取り足取りで教えるわけではありません。本人の力量を評価しながら、さらに高度な判断や処置が必要なときに、助言と(救いの)手がでてきます。
3.豊富で貴重な症例(経験)
神戸市内は言うに及ばず近畿でも有数の症例を数える病院として、軽症から重症まで極めて幅の広い病態を経験することができます。一般的な臨床研修病院と比べても短期間で多くの症例を担当するため、消化器病学会・内視鏡学会・肝臓学会などの専門医は問題なくクリアできるでしょう。普通、一年(時には一生)に一例経験するかどうかといったまれな病態も、普通に出会います。研究会や学会で一例報告になるような病態を10例まとめて検討するような病院です。しかし、症例が多いからといって、一例一例をおろそかにすることは決してありません。患者さんにとっては、初めての病気・初めての不安であり、我々は専門家として、冷静かつ誠意を持って対応することが求められます。
4.複雑な病態を専門家集団で解明する
一見「わけわからん」病態にも、頻繁に遭遇します。その時は、ひとり悩まずにまず上級医に相談してください。貴重なアドバイスがもらえるはずですが、それでも困ったときには、各診療科にコンサルトします。心疾患を有する肝硬変患者さんが、呼吸器感染症をきっかけに電解質バランスをくずして意識障害をきたしICU管理で危機的状態を脱却するなんてことは、日常茶飯事ですから。担当医がフル回転することはもちろん必要ですが、いつの間にか専門家の救いの手があちこちから伸びてきます。
5.伝統あるトレーニングシステム(研修プログラム)
当院では、30年以上も前から、独自の臨床研修プログラムで臨床医を育て全国に送り出してきました。平成30年度からスタートする内科専門医研修プログラムにおいても、その経験をもとに内科全体で指導体制を検討しました。その詳細は病院HPを参照いただければと思います。ここで、強調したいことは、この体制が一朝一夕でできたのもではなく、試行錯誤を繰り返すなかで磨かれてきたものだということです。それは、現在も続いており、毎月病院幹部から若手スタッフまで集まり、問題点の検討・改善を繰り返しております。我々の実践してきた卒後教育は、換言すれば「厳しいゆりかご」みたいなもので、多くの実臨床での経験を積む中で、誰が教えるでもなく、皆が教えお互いに学び、いつの間にか一人前になるのです。そこには、カリスマ指導医や目新しい奇をてらったプログラムは必ずしも必要ないと考えます。
厚生労働省の策定した「新臨床研修制度」がスタートして、15年が経過しました。卒後2年間で幅広い領域の研修を目指すという意義は評価される点もありますが、その後、顕在化した医療崩壊の危機を引き起こしたことから、功罪相半ばするものといえるのではないでしょうか。仏は官僚が作ったとしても、魂を入れられるのは我々医療者でしかありません。「伝統は一日にしてならず」です。
6.Let’s Join Us!
熱い情熱をもって医療の未来を担う若者に呼びかけます。我々と一緒に汗を流しませんか。目の回るような毎日ですが、充実感を感じる毎日でもあります。医療の高度専門化が進むなかでも、消化器領域は非常に多くの疾患・病態をカバーし、多彩な手技をもって治療にあたることができます。我々は、いつでも手を広げて歓迎します。
論文・学会発表実績
- Akiyama S et al.:Peroral Cholangioscopy Using an Ultra-slim Upper Endoscope.Internal Medicine DOI:https://doi.org/10.2169/internalmedicine.3557-24,2024/4
- Yabuuchi Y et al.:Endoscopic submucosal dissection using the tunneling method for early gastric cancer occupying the entire fornix.Endoscopy(2024; 56(S 01): E445-E446)DOI:https://doi.org/10.1055/a-2321-9626,2024/5
- 籔内洋平:PPI/P-CABの長期内服に伴い多発胃神経内分泌腫瘍(NET)を生じた1例.胃と腸 第59巻 第5号 P737-745,2024/5
- 井上聡子:診断講座 IBD診断・治療マネジメントの実際 第10回オルメサルタン関連スプルー様腸疾患.IBD ResearchVol.18No.2,2024/6
- Nagao S et al.:Multiple Gastric Neuroendocrine Tumors Associated with Long-term Use of a Proton Pump Inhibitor and a Potassium-competitive Acid Blocker.Internal Medicine DOI:https://doi.org/10.2169/internalmedicine.2857-23,2024/7
- Arino H et al.:Metachronous Rupture of Pancreatoduodenal Artery Aneurysm with Median Arcuate Ligament Syndrome: A Case Report and Review of 11 Cases.Internal Medicine DOI:https://doi.org/10.2169/internalmedicine.3338-23,2024/8
- Morihisa Y et al.:Gastrointestinal submucosal haematoma.Endoscopy Inside view DOI:https://doi.org/10.1136/flgastro-2024-102787,2024/9
- Akiyama S et al.:Portal-Vein Compression Caused by Double-Pigtail Plastic Biliary Stent.JGH Open DOI:https://onlinelibrary.wiley.com/doi/10.1002/jgh3.70094,2025/1
- Akiyama S et al.:Successful retrieval of a migrated pancreatic stent via endoscopic ultrasound-guided transluminal drainage using an ultraslim upper endoscope.Digestive Endoscopy DOI:https://doi.org/10.1111/den.15015,2025/3
- 押川大介(日本赤十字社和歌山医療センター) :当院における内視鏡的乳頭筋切開術(EST)後出血に寄与する危険因子の検討.第110回日本消化器病学会総会,徳島,2024/5/10
- 森久芳樹:当院で経験した潰瘍性大腸炎関連腫瘍6例の検討.第110回日本消化器病学会総会,徳島,2024/5/11
- 丹家元祥:当院における胆道癌ゲノム医療の現状についての検討.第110回日本消化器病学会総会,徳島,2024/5/11
- 籔内洋平 他:大腸内視鏡検査におけるEndoBRAIN-EYEを用いた観察の有用性に関する非盲検化ランダム化比較試験.第107回日本消化器内視鏡学会総会,東京/Web,2024/5/30
- 長尾宗一郎 他:胃酸分泌抑制薬の長期内服に関連して発生した多発胃神経内分泌腫瘍の1例.第107回日本消化器内視鏡学会総会,東京/Web,2024/5/31
- 森田周子 他:食道癌に対する化学放射線療法後遺残再発症例に対して内視鏡治療施行症例の検討.第112回日本消化器内視鏡学会近畿支部例会,大阪,2024/6/29
- 籔内洋平:ビデオシンポジウム1 分かち合いたい内視鏡経験・症例-消化管.第112回日本消化器内視鏡学会近畿支部例会,大阪,2024/6/29
- 長尾宗一郎 他:咽頭出血に対して耳鼻科医との連携により止血に成功した一例.第112回日本消化器内視鏡学会近畿支部例会,大阪,2024/6/29
- 秋山慎介 他:切除可能膵癌に対する至適な術前胆道ドレナージに関する検討.第112回日本消化器内視鏡学会近畿支部例会,大阪,2024/6/29
- 丹家元祥 他:内視鏡的乳頭切除術後に後腹膜穿孔を来し外瘻チューブにより保存的加療を行えた症例.第112回日本消化器内視鏡学会近畿支部例会,大阪,2024/6/29
- 宇山航平 他:胃底腺ポリポーシスを伴う胃腫瘍に対してGel immersion EMRが有用であった1例.第112回日本消化器内視鏡学会近畿支部例会,大阪,2024/6/29
- 坂野利樹 他:内視鏡所見から術前診断しえたリンパ球浸潤胃癌の一例.第112回日本消化器内視鏡学会近畿支部例会,大阪,2024/6/29
- 上野昌太朗 他:直接経口胆道鏡(POCS)下EHLで完全結石除去に成功した術後再検腸管の積み上げ結石の一例.第112回日本消化器内視鏡学会近畿支部例会,大阪,2024/6/29
- 三宅雄也 他:アザシチジンが著効したMDS関連腸疾患.第112回日本消化器内視鏡学会近畿支部例会,大阪,2024/6/29
- 森田周子:食道癌に対する化学放射線療法後に発症した食道単純ヘルペスウイルス感染症の1症例.第78回日本食道学会各術集会,東京,2024/7/4
- 森田周子:食道癌の診療の基本と最前線.第46回日本消化器内視鏡学会近畿セミナー,Web,2024/9/3-17
- 長尾宗一郎 他:85歳以上の超高齢者に対する早期胃癌ESD後の長期予後に関連する因子について.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 小林拓哉 他:壁在結節を有するIPMNにおけるERCPの現状と課題.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 上野昌太朗 他:当院における肝細胞癌に対するデュルバルマブ+トレメリブマブ併用療法の初期使用経験.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 秋山慎介 他:切除不能胆道癌に対するGC療法とGCD療法の比較検討.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 森久芳樹 他:難治性潰瘍性大腸炎に対する当院でのタクロリムス(TAC)治療の変遷.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 押川大介 他:高齢発症潰瘍性大腸炎(UC)の臨床的特徴と治療選択に対する検討.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 三宅雄也 他:憩室出血の出血源同定にCO2血管造影が有用であった1例.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 坂野利樹 他:5-FU+CDDP+Pembrolizumabが著効した多発転移を伴う食道癌の一例.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 藤尾行恵 他:食道癌に対するPembrolizumab投与により、サイトカイン放出症候群を来した一例.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 宇山航平 他:肝腫瘍生検後に出血性ショックを来し、致死的経過を辿った一例.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 德冨佑太郎 他:偽性腸閉塞を契機に診断された全身強皮症の一例.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 阪本万規穂 他:食道癌に対して化学放射線療法を行い、原発巣とリンパ節転移に対して著効したのちに脳転移が判明した一例.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 蓑島貴成(日本赤十字社和歌山医療センター):腎細胞癌術後33年目に膵転移再発をきたした1例.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 髙折克至(日本赤十字社和歌山医療センター):正中弓状靭帯圧迫症候群により動脈瘤破裂をきたし、急性膵炎との鑑別を要した後腹膜血腫の一例.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 森久芳樹 他:十二指腸潰瘍出血における止血困難例とPNI(Prognostic nutritional index)の関連.日本消化器病学会近畿支部第121回例会,京都,2024/9/28
- 籔内洋平 他:胃Gel immersion EMRの有用性及び安全性:多施設遡及的研究.JDDW2024(消化器内視鏡学会),神戸/Web,2024/10/17
- 秋山慎介 他:切除不能進行胆道癌に対するGCD療法の安全性と有効性に関する検討.JDDW2024(消化器病学会),神戸/Web, 2024/11/2
- 森久芳樹 他:Multi-Option時代におけるクローン病の狭窄病変に対する内視鏡的バルーン拡張術の現状.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 押川大介 他:20mm以下の表在性非乳頭部十二指腸上皮性腫瘍(SNADET)に対するconventional EMRとunderwater EMRの比較.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 藤尾行恵 他:小腸腫瘍の診療における小腸内視鏡の役割と限界.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 小林拓哉 他:胆管空腸吻合部良性狭窄に対するバルーン内視鏡下ERCPの治療成績.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 秋山慎介 他:EUS-TDルートを介して迷入膵管ステント回収に成功した一例.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 簑島貴成(日本赤十字和歌山医療センター):大腸憩室出血におけるSRH同定に関連する因子の検討.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 坂野利樹 他:当院での胃瘻造設術の現況と高齢者における合併症に関する検討.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 髙折克至(日本赤十字和歌山医療センター):難治性食道Candida症合併により術前診断が困難であったverrucous carcinomaの一例.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 三宅雄也 他:内視鏡的に止血し得た小腸憩室出血の1例.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 宇山航平 他:劇症型アメーバ性大腸炎による腸管穿孔で致死的経過を辿った一例.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 德冨佑太郎 他:当院で経験した消化管アミロイドーシスの内視鏡像.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 上野昌太朗 他:術前診断が困難であった胆嚢内乳頭状腫瘍(intracholecystic papillary neoplasm:ICPN)の一例.第113回日本消化器内視鏡学会近畿支部例会,大阪,2024/12/7
- 森田周子:消化管穿孔・瘻孔・異物に対する診断と内視鏡治療.第47回日本消化器内視鏡学会近畿セミナー,Web,2024/12/29-
- 籔内洋平:Young Investigator Session 3 上部消化管.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 押川大介 他:当院におけるアテゾリズマブ・ベバシズマブ併用療法の成績と後治療に関する検討.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 小林拓哉 他:胆管狭窄を有する胆道癌に対する経乳頭的病理診断能の検討.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 藤尾行恵 他:他病変への術前化学療法の効果により、内視鏡治療が可能となった下咽頭癌、頚部食道癌の一例.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 今井明日香 他:当院における妊娠患者に対する内視鏡検査の安全性の検討.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 坂野利樹 他:進行食道胃接合部癌の治療後に白血病を発症した一例.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 森久芳樹 他:難治性の免疫関連有害事象(irAE)大腸炎の臨床的特徴.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 上野昌太朗 他:十二指腸乳頭部adenomyomaに上皮内癌を併発した一例.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 德冨佑太郎 他:内視鏡的整復に成功した間膜性胃軸捻転症の一例.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 三宅雄也 他:貧血を契機に診断に至った好酸球性胃腸炎の1例.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 宇山航平 他:Spontaneous Regressionを呈した横行結腸癌の1例.日本消化器病学会近畿支部第122回例会,京都,2025/2/15
- 籔内洋平:eCura systemの外的妥当性に関する多機関共同後ろ向き観察研究 ~KONOE project~.第97回日本胃癌学会総会,名古屋,2025/3/14
- Yabuuchi Y:A multicenter, randomized open-label trial comparing 1-day cessation of direct oral anticoagulants before and after colorectal polypectomy- MADOWAZU trial -.DDW2024,Washington.D.C,2024/5/19
- Morihisa Y et al.:Standard vs. Computer-Aided Detection Assisted Colonoscopy for Detection of Colorectal Neoplasia: An Open-Label Randomized Controlled Trial ; CADe did not Improve Detection.DDW2024,Washington.D.C,2024/5/20
- Tanaka K et al.:Breast cancer metastasis to the stomach mimicking early gastric cancer.Journal of Gastroenterology and Hepatology doi:10.1002/jgh3.12959,2023/8
- Nagao S et al.:Multiple Gastric Neuroendocrine Tumors Associated with Long-term Use of a Proton Pump Inhibitor and a Potassium-competitive Acid Blocker.Internal Medicine doi:10.2169/internalmedicine.2857-23,2023/11
- 籔内洋平:内視鏡AIがもたらす医師の負担軽減とその医療経済的価値.月刊新医療 第50巻第10号,2023/10
- Akiyama S et al.:Varicella-Zoster Virus Esophagitis Prior to the Onset of Skin Lesions.Internal Medicine doi:10.2169/internalmedicine.3235-23,2024/3
- 丹家元祥 他:当院における膵癌術後の遠隔転移再発におけるリスク因子の検討.日本消化器病学会第109回総会,長崎,2023/4/6
- 籔内洋平 他:10-14mmの病変に対するCold Snare Endoscopic Mucosal Resectionから見るCold手技の限界.日本消化器病学会第109回総会,長崎,2023/4/8
- 宇山航平 他:EUS-FNAにより組織診断した膵原発悪性リンパ腫の一例.第120回日本内科学会講演会,東京/Web,2023/4/14-16
- 井上聡子:シンポジウム3「消化管出血に対する内視鏡診療の現況と展望(小腸・大腸)」.第110回日本消化器内視鏡学会近畿支部例会,大阪,2023/6/24
- 長尾宗一郎 他:PPI/P-CAB長期内服による高ガストリン血症を背景とした多発胃NETの1例.第110回日本消化器内視鏡学会近畿支部例会,大阪,2023/6/24
- 籔内洋平 他:穹窿部全体を占める早期胃がんに対するESDにおける工夫.第110回日本消化器内視鏡学会近畿支部例会,大阪,2023/6/24
- 丹家元祥 他:当院における膵癌ゲノム医療の現状についての検討.第110回日本消化器内視鏡学会近畿支部例会,大阪,2023/6/24
- 蓑島貴成 他:術前診断が困難であった、十二指腸乳頭部癌に併存した浸潤性膵管内乳頭粘液腺癌の1例.第110回日本消化器内視鏡学会近畿支部例会,大阪,2023/6/24
- 髙折克至 他:胆管金属ステント抜去に難渋し、ステント上端内翻により抜去に成功して1例.第110回日本消化器内視鏡学会近畿支部例会,大阪,2023/6/24
- 山村総一郎 他:腎細胞癌術後に多彩な消化管転移をきたした一例.第110回日本消化器内視鏡学会近畿支部例会,大阪,2023/6/24
- 宇山航平 他:胆管狭窄フォロー中に繰り返す胆管生検により膵頭部癌の診断に至った一例.第110回日本消化器内視鏡学会近畿支部例会,大阪,2023/6/24
- 秋山慎介:膵癌による遠位胆道狭窄に対する経乳頭的胆道ドレナージ術の現状と課題.第59回日本胆道学会学術集会,札幌,2023/9/14
- 秋山慎介:Young Investigator Session 3 膵2(膵癌).日本消化器病学会近畿支部第119回例会,大阪,2023/9/30
- 鄭 浩柄 他:FIB-4高値を呈した糖尿病患者に関する検討.日本消化器病学会近畿支部第119回例会,大阪,2023/9/30
- 蓑島貴成 他:黒色食道を呈した急性壊死性食道炎の3例.日本消化器病学会近畿支部第119回例会,大阪,2023/9/30
- 秋山慎介 他:経乳頭的アプローチ困難時の悪性胆管狭窄に対する一期的経皮経肝的SEMS留置術の有用性.日本消化器病学会近畿支部第119回例会,大阪,2023/9/30
- 三木秀晃 他:膵性胸水を伴う膵仮性嚢胞に対して超音波内視鏡下膵嚢胞ドレナージ術(EUS-CD)が奏功した1例.日本消化器病学会近畿支部第119回例会,大阪,2023/9/30
- 三宅雄大 他:切除不能膵癌に対してconversion surgeryを行い、pathological CRが得られた一例.日本消化器病学会近畿支部第119回例会,大阪,2023/9/30
- 髙折克至 他:急速進行肝細胞癌に対して肝動注リザーバー療法が著効した一例.日本消化器病学会近畿支部第119回例会,大阪,2023/9/30
- 山村総一郎 他:冠動脈バイパス術後で外科的切除が困難と判断された早期胃癌に対し、内視鏡的粘膜下層剥離術を行った一例.日本消化器病学会近畿支部第119回例会,大阪,2023/9/30
- 三谷莉永 他:幽門側胃切除術Roux-en-Y再建後の結石性胆管炎に対し経皮経肝胆嚢ドレナージルートを経由して総胆管結石の採石に成功した1例.日本消化器病学会近畿支部第119回例会,大阪,2023/9/30
- 髙折克至 他:Meckel憩室の診断におけるダブルバルーン内視鏡の有用性に関する検討.JDDW2023,神戸,2023/11/2
- 森田周子:胃の内視鏡診断 綺麗な画像で胃癌を診断.JDDW2023,神戸,2023/11/4
- 和田将弥 他:当院における膵神経内分泌腫瘍に対する治療の現状.JDDW2023,神戸,2023/11/4
- 秋山慎介 他:切除可能膵癌に対する術前化学療法を含む周術期治療の検討.JDDW2023,神戸,2023/11/4
- 小林拓哉 他:軽症・中等症の総胆管結石性胆管炎に対する一期的結石除去の有用性の検討.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 田中晃輔 他:当院における胃粘膜下腫瘍に対する腹腔鏡内視鏡合同手術の現状.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 籔内洋平 他:10-20mm大の大腸鋸歯状病変に対するUnderwater Endoscopic Mucosal Resectionの有用性と安全性に関する多施設前向き観察研究.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 森久芳樹 他:大腸ステントの治療成績と今後の展望.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 長尾宗一郎 他:大腸憩室出血に対するバリウム充填法の有用性についての検討.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 三木秀晃 他:生物学的製剤の導入を要した免疫関連有害事象(irAE)大腸炎の臨床的特徴についての検討.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 蓑島貴成 他:食道病変により大量出血を呈したIgA血管炎の1例.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 髙折克至 他:出血性ショックに至ったサイトメガロウイルス小腸炎に対して内視鏡的診断及び止血に成功した一例.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 森 敬之 他:虫垂腫瘍を内視鏡的切除後、遅発性に腹腔内出血を来した一例.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 山村総一郎 他:残膵癌を疑い、膵頭十二指腸切除術を施行し膵放線菌症と診断した一例.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 三谷莉永 他:内視鏡的膵管ドレナージチューブによる十二指腸穿孔に対してOver-The-Scope Clip システムでの縫縮が有用であった1例.第111回日本消化器内視鏡学会近畿支部例会,大阪,2023/11/18
- 鄭 浩柄:アテゾリズマブ・ベバシズマブ併用療法後に肝切除を施行し得た進行肝細胞癌の一例.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 森田周子:若手医師のための胃癌診断101.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 長尾宗一郎 他:胃ESD後出血予防のための粘膜欠損縫縮術について.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 森久芳樹 他:切除不能進行肝細胞癌に対するアテゾリズマブ・ベバシズマブ併用療法の臨床成績と治療効果予測因子.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 小林拓哉 他:胆膵内視鏡におけるスコープ穿孔についての検討.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 田中晃輔 他:内視鏡的アプローチ困難な部位に存在する表在型非乳頭部十二指腸上皮性腫瘍に対する腹腔鏡内視鏡合同手術における工夫.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 蓑島貴成 他:黒色便を契機に診断した食道癌肉腫の1例.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 三木秀晃 他:自己免疫性肝炎に対してステロイド投与開始後に縮小を認めた肝偽リンパ腫の一例.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 大島章裕 他:MASHを背景に発症し黄疸遷延を認めた急性E型肝炎の一例.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 三宅雄大 他:胆嚢癌に対する化学療法中に癌性髄膜炎を発症した一例.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 森 敬之 他:Gemcitabine/Cisplatinに Durvalumabを上乗せし奏功した胆嚢癌の一例.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 山村総一郎 他:血便で発症した続発性消化管アミロイドーシスの一例.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- 髙折克至 他:Infliximab抵抗性irAE腸炎に対してTofacitinibが著効した一例.日本消化器病学会近畿支部第120回例会,神戸,2024/1/27
- Yabuuchi Y et al.: Effective Endoscopic Delineation With Acetic Acid Spray and Narrow Band Imaging in Underwater Endoscopic Mucosal Resection for Sessile Serrated Lesion. The American Journal of Gastroenterology 117:840, 2022
- Aoyama N et al.: A case of neuroendocrine neoplasm of the minor duodenal papilla. Clinical Journal of Gastroenterology:2022
- Aoyama N et al.: Olmesartan-associated sprue-like enteropathy. BMJ 2022;15:e254189: 2022
- Tanaka K et al.: Endoscopic submucosal dissection for a superficial esophageal squamous cell carcinoma located in a Rokitansky diverticulum. Endoscopy E-Videos CC BY-NC-ND 4.0 ・ Endoscopy 2022; 54(S 02): E986-E987:2022
- Hosotani K et al.: Endoscopic submucosal dissection for complete removal of a residual colorectal tumor involving a diverticulum. Endoscopy E-Videos CC BY-NC-ND 4.0 ・ Endoscopy 2022; 54(S 02): E908-E909:2022
- Yabuuchi Y et al.: A novel technique to improve endoscopic accessibility in laparoscopic endoscopic cooperative surgery for a duodenal lesion. Endosc Int Open 2022; 10(12): E1597-E1598:2022
- Hosotani K et al.: Detecting remnant sessile serrated lesion after piecemeal cold snare polypectomy using acetic acid with narrow-band imaging. Endosc Int Open 2022; 10(12): E1595-E1596:2022
- Aoyama N et al.: Pancreatic metastasis from lung adenocarcinoma. Journal of General and Family Medicine:2023
- 今村大智 他: IgA血管炎174例の臨床像.第119回日本内科学会・講演会, 京都/Web, 2022/4/16
- 丹家元祥: 当院におけるEPBD/EPLBDによる総胆管結石治療の検討.第108回日本消化器病学会総会,東京/Web, 2022/4/21
- 秋山慎介 他: 膵癌術前の悪性胆道狭窄に対する内視鏡的胆道ドレナージ治療戦略.第108回日本消化器病学会総会,東京/Web, 2022/4/23
- 田中晃輔 他: Rokitansky憩室内に存在する食道表在癌に対するESDにおける工夫.第108回日本消化器内視鏡学会近畿支部例会,京都, 2022/6/11
- 籔内洋平 他: 表在性非乳頭部十二指腸上皮性腫瘍に対するD-LECS:安全で確実なESDから縫縮まで. 第108回日本消化器内視鏡学会近畿支部例会,京都, 2022/6/11
- 丹家元祥 他:当院における腫瘤を伴わない膵管狭窄に対する膵液連続細胞診の成績.第108回日本消化器内視鏡学会近畿支部例会,京都, 2022/6/11
- 森久芳樹 他: 成人発症で特徴的な消化管病変を呈したIgA血管炎の一例.第108回日本消化器内視鏡学会近畿支部例会,京都, 2022/6/11
- 長尾宗一郎 他: 市中病院におけるJNET分類の有用性と今後の課題について. 第108回日本消化器内視鏡学会近畿支部例会, 京都, 2022/6/11
- 押川大介 他: クローン病に合併した十二指腸副乳頭部神経内分泌腫瘍の一例. 第108回日本消化器内視鏡学会近畿支部例会, 京都, 2022/6/11
- 藤尾行恵 他: 十二指腸水平部の憩室出血に対して経口的ダブルバルーン内視鏡で止血し得た1例. 第108回日本消化器内視鏡学会近畿支部例会, 京都, 2022/6/11
- 下川岳人 他: 単4電池を多数誤飲し、内視鏡的に摘出した1例. 第108回日本消化器内視鏡学会近畿支部例会, 京都, 2022/6/11
- 竜野稜子 他: 当院における小型膵神経内分泌腫瘍に対するEUS-FNAの診断能. 日本消化器病学会近畿支部第117回例会,大阪, 2022/10/8
- 南條俊也 他: 小腸閉塞を発症した小腸MALTリンパ腫の1例. 日本消化器病学会近畿支部第117回例会, 大阪, 2022/10/8
- 押川大介 他: 成人腸重積37例の検討. 日本消化器病学会近畿支部第117回例会, 大阪, 2022/10/8
- 塚本和之 他: フェノフィブラート不耐の原発性胆汁性胆管炎に対してペマフィブラートが奏功した2例. 日本消化器病学会近畿支部第117回例会, 大阪, 2022/10/8
- 下川岳人 他: 巨大肝細胞癌に対してTAE後レンバチニブ投与中に腫瘍内出血を合併した一例. 日本消化器病学会近畿支部第117回例会, 大阪, 2022/10/8
- 小川健仁 他: CTで食道の浮腫性壁肥厚を契機に指摘された急性壊死性食道炎の2例. 日本消化器病学会近畿支部第117回例会, 大阪, 2022/10/8
- 藤尾行恵 他: 食道癌に対するNivolmab投与により下垂体炎をきたした1例. 日本消化器病学会近畿支部第117回例会, 大阪, 2022/10/8
- 曽根明日香 他: 免疫チェックポイント阻害薬投与中に発症したirAE(immune-related adverse event)胆管炎の1例. 日本消化器病学会近畿支部第117回例会, 大阪, 2022/10/8
- 勝山苑香 他: 腹痛を契機に発見され、外科的切除により診断された膵MiNENの一例. 日本消化器病学会近畿支部第117回例会, 大阪, 2022/10/8
- 秋山慎介 他: 切除可能膵体尾部癌に対する術前EUS-FNABの必要性と予後に関する検討. JDDW2022, 福岡/Web, 2022/10/28
- 丹家元祥 他: 当院の造影結節を有する膵管内乳頭粘液性腫瘍に対する膵液連続細胞診の成績. JDDW2022, 福岡/Web, 2022/10/28
- 山本健太 他: 当院における悪性胆道閉塞に対するドレナージ治療の現状. JDDW2022, 福岡/Web, 2022/10/29
- 長尾宗一郎 他: 高齢者の大腸憩室出血についての検討. 第109回日本消化器内視鏡学会近畿支部例会, 京都/Web, 2022/11/5
- 藤尾行恵 他: 血便を契機に診断し得たメトトレキサート関連リンパ増殖性疾患の1例.第109回日本消化器内視鏡学会近畿支部例会, 京都/Web,2022/11/5
- 井上聡子 他: クローン病の腸管狭窄に対する内視鏡的バルーン拡張術の効果と展望.第109回日本消化器内視鏡学会近畿支部例会, 京都/Web, 2022/11/5
- 細谷和也 他: Japan Endoscopy Databaseを活用した大腸内視鏡Quality indicatorの評価と今後の課題. 第109回日本消化器内視鏡学会近畿支部例会, 京都/Web, 2022/11/5
- 押川大介 他: 潰瘍性大腸炎増悪による血便との鑑別を要した二次性大動脈十二指腸瘻の一例. 第109回日本消化器内視鏡学会近畿支部例会, 京都/Web, 2022/11/5
- 小川健仁 他 : 遠位胆道癌による胆管狭窄に対する術前内視鏡的ドレナージの検討. 第109回日本消化器内視鏡学会近畿支部例会, 京都/Web, 2022/11/5
- 秋山慎介 他: 膵周囲液体貯留に対する内視鏡的step-up approachの現状と課題. 第109回日本消化器内視鏡学会近畿支部例会, 京都/Web, 2022/11/5
- 南條俊也 他: 当院における悪性胆道狭窄に対して胆管金属ステント留置後に胆嚢炎を発症した症例の検討.第109回日本消化器内視鏡学会近畿支部例会, 京都/Web, 2022/11/5
- 曽根明日香 他: 早期食道癌への内視鏡的治療時にオーバーチューブによる食道穿孔を来した1例. 第109回日本消化器内視鏡学会近畿支部例会, 京都/Web, 2022/11/5
- 長尾宗一郎 他: 市中病院での肝細胞癌に対するアテゾリズマブ・ベマシズマブ併用療法の成績について. 日本消化器病学会近畿支部第118回例会, 京都, 2023/1/21
- 井上聡子 他: 潰瘍性大腸炎に対するベドリズマブの寛解維持効果.日本消化器病学会近畿支部第118回例会, 京都, 2023/1/21
- 曽根明日香 他: 当院における胆管癌による胆道狭窄に対する経乳頭的病理診断能の現状. 日本消化器病学会近畿支部第118回例会, 京都, 2023/1/21
- 塚本和之 他: 出血性ショックを呈したアメーバ性大腸炎の一例. 日本消化器病学会近畿支部第118回例会, 京都, 2023/1/21
- 竜野稜子 他: メッケル憩室の術前診断についての検討~当院の20例の経験から~. 日本消化器病学会近畿支部第118回例会, 京都, 2023/1/21
- 有野寛人 他: 正中弓状靭帯症候群を背景に異時性に膵十二指腸動脈瘤破裂をきたした一例. 日本消化器病学会近畿支部第118回例会, 京都, 2023/1/21
- 藤尾行恵 他: 術前経皮的胆道ドレナージにより播種再発を来したと考えられる肝内胆管癌の一例. 日本消化器病学会近畿支部第118回例会, 京都, 2023/1/21
- 南條俊也 他: 悪性肝門部胆管閉塞に対してEUS下ドレナージ術を行った1例. 日本消化器病学会近畿支部第118回例会, 京都, 2023/1/21
- 長尾宗一郎 他: 後出血ハイリスク患者における胃ESD後粘膜欠損の予防的縫縮術について. 第95回日本胃癌学会総会, 札幌, 2023/2/24
- 細谷和也 他: 胃ESD後サーベイランス発見胃癌の検討. 第95回日本胃癌学会総会, 札幌, 2023/2/25
- Morita S: Multicenter prospective in vivo study of an endocytoscope system(ECS) for superficial esophageal cancer. Journal of Gastroenterology 56, pages808–813, 2021
- Ueda T et al.: Shaggy white lesion with morphological changes in the oesophagus. Gut DOI:10.1136/gutjnl-2021-326643, 2022
- 秋山慎介: 胃粘膜下腫瘍に対する腹腔鏡内視鏡合同手術の有用性. 第107回日本消化器病学会, 東京/Web, 2021/4/15
- 丹家元祥: 当院の膵管癌診療における初期症状についての検討. 第107回日本消化器病学会, 東京/Web, 2021/4/15
- 唐渡修一郎 他: 消化管原発濾胞性リンパ腫の治療、予後についての検討. 第101回日本消化器内視鏡学会総会, 広島/Web, 2021/5/14
- 上田智也 他: 胃ESD後出血の予測因子に関する検討. 第101回日本消化器内視鏡学会総会, 広島/Web, 2021/5/15
- 秋山慎介 他: 表在性非乳頭部十二指腸上皮性腫瘍に対するEMR、UEMRの現状と課題. 第101回日本消化器内視鏡学会総会, 広島/Web, 2021/5/14
- 長尾宗一郎 他: 当院における電気水圧衝撃破砕術(EHL)の検討. 第101回日本消化器内視鏡学会総会, 広島/Web, 2021/5/14
- 細谷和也 他: 85歳以上の超高齢者に対する胃ESDの短期成績及び長期成績の検討. 第101回日本消化器内視鏡学会総会, 広島/Web, 2021/5/16
- 鄭 浩柄: 肝 reactive Lymphoid hyperplasia の7症例-長期自然経過を含めた報告-. 第57回日本肝臓学会総会, 札幌/Web, 2021/6/18
- 唐渡修一郎 他: (追加発言1)当院においてCold snare polypectomy後病理的に癌と診断された11病変についての検討. 第106回日本消化器内視鏡学会近畿支部例会, 大阪/Web, 2021/7/10
- 安藤徳晃 他: 高齢者に対する早期胃癌内視鏡的粘膜下層剥離術(ESD)の検討 -機能評価の側面から-. 第106回日本消化器内視鏡学会近畿支部例会, 大阪/Web, 2021/7/10
- 上田智也 他: 十二指腸穿破による消化管出血を契機に診断し得た解離性肝動脈瘤の一例. 第106回日本消化器内視鏡学会近畿支部例会, 大阪/Web, 2021/7/10
- 森久芳樹 他: 当院で経験した腸管AVM9例に対する内視鏡的考察. 第106回日本消化器内視鏡学会近畿支部例会, 大阪/Web, 2021/7/10
- 秋山慎介 他: (追加発言1)ERCP関連手技に伴う難治性出血、穿孔に対するOTSCの使用経験. 第106回日本消化器内視鏡学会近畿支部例会, 大阪/Web, 2021/7/10
- 鄭 浩柄 他: 増加しつつあるメタボ肝癌の臨床的特徴について. 日本消化器病学会近畿支部第115回例会, Web, 2021/9/18
- 上田智也 他: 長期にわたり食道癌との鑑別に苦慮した食道epidermizationの一例. 日本消化器病学会近畿支部第115回例会, Web, 2021/9/18
- 下山雅之 他: 術前に診断可能であった早期胃神経内分泌癌の1例. 日本消化器病学会近畿支部第115回例会, Web, 2021/9/18
- 唐渡修一郎 他: 長期経過観察中に形質転化を来した治療介入に至った消化管濾胞性リンパ腫の1例. 日本消化器病学会近畿支部第115回例会, Web, 2021/9/18
- 森久芳樹 他: 妊娠中に高TG血症を原因とする急性膵炎を発症した1例. 日本消化器病学会近畿支部第115回例会, Web, 2021/9/18
- 小林拓哉 他: 術後診断目的に施行したEUS-FNA後にneedle tract seedingをきたした膵体尾部癌の1例. 日本消化器病学会近畿支部第115回例会, Web, 2021/9/18
- 安藤徳晃 他: 18年の経過で悪性転化した粘液性嚢胞腫瘍の一例. 日本消化器病学会近畿支部第115回例会, Web, 2021/9/18
- 今村大智 他: 強い腹痛で発症したIgA血管炎の一例. 日本消化器病学会近畿支部第115回例会, Web, 2021/9/18
- 田中晃輔 他: ステロイド単独投与にて再活性化を認めたHBV既往感染例の報告. 日本消化器病学会近畿支部第115回例会, Web, 2021/9/18
- 長尾宗一郎 他: 10mm以下の表面型大腸腫瘍に対するUEMRの有用性・安全性についての検討. JDDW2021, 神戸/Web, 2021/11/4
- Hosotani K et al.: Optimized optical stratification by JNET classification with chromoendoscopy for colorectal lesions ?10 mm. JDDW2021,Kobe/Web, 2021/11/5
- 丹家元祥 他: 当院の膵管癌診療におけるPETについての検討. JDDW2021, 神戸/Web, 2021/11/6
- 井上聡子: オルメサルタン関連スプルー様腸疾患3例の報告. 第59回日本小腸学会学術集会, 東京/Web, 2021/11/27
- 秋山慎介 他: 膵癌による遠位胆管狭窄に対する術前胆道ドレナージの検討. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 上田智也 他: 胃ESD後発見胃癌の臨床病理学的特徴に関する検討. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 籔内洋平 他: Sessile serrated lesionに対する酢酸散布後NBI観察下でのUnderwater EMRの可能性. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 丹家元祥 他: 当院における治療困難な胆管結石に対する胆道鏡下電気水圧衝撃波結石破砕術(EHL)の使用経験. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 井上聡子 他: カプセル内視鏡がクローン病診療に果たす役割. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 細谷和也 他: 10mm未満の非有茎性大腸腫瘍に対するUnderwater EMRとConventional EMRの短期成績の比較. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 森久芳樹 他: 消化管出血を契機に診断に至ったirAE胃炎・十二指腸の1例. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 安藤徳晃 他: 当院で経験した二次性大動脈十二指腸瘻. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 唐渡修一郎 他: 虫垂開口部に存在する腫瘍に対してUnderwater EMRで一括切除を得た1例. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 小林拓哉 他: EUS-FNAにて乳腺葉状腫瘍膵転移の確定診断に至った一例. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 田中晃輔 他: 当院で経験した乳癌胃転移の4例. 第107回日本消化器内視鏡学会近畿支部例会, 神戸/Web, 2021/12/11
- 秋山慎介 他: 膵体尾部癌術前のEUS-FNABに伴うneedle tract seedingと予後に関する検討. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- 安藤徳晃 他: COVID-19陽性患者における消化管出血の現状. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- 森久芳樹 他: 大腸憩室出血に対する内視鏡的止血難渋例の検討. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- 森田周子 他: 当院における食道癌に対するNivolumab投与症例の検討. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- 高折克至 他: 特異な形態を示し術前診断が困難であった小腸GISTの一例. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- 押川大介 他: 慢性特発性偽性腸閉塞に対するPEG-Jを用いた減圧療法の経験. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- 唐渡修一郎 他: 直接作用型抗ウイルス薬によるC型慢性肝炎治療後に自己免疫性肝炎および原発性硬化性胆管炎を発症した1例. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- 長尾宗一郎 他: 内視鏡的に治療し得たgangliocytic paragangliomaの一例. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- 上田智也 他: 急性胆管炎を契機に診断に至った膵Leiomyomaの一例. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- 田中晃輔 他: 虫垂原発MALTリンパ腫の一例. 日本消化器病学会近畿支部第116回例会, 大阪/Web, 2022/2/5
- Kitamoto H et al.:Successful Endoscopic Removal of a Large Pancreatic Stone in a Patient After Pancreaticoduodenectomy.Clinical Gastroenterology and Hepatology Volume18,Issue5:A30-A31,2020/5
- Hosotani K et al.:A case of anal intraepithelial neoplasia resected by endoscopic submucosal dissection after magnifying narrow-band imaging evaluation.Gastrointestinal Endoscopy GIE :Published 2020/6/9/li\u003e
- Okubo Y et al.:Recurrence of pembrolizumab-induced severe gastritis after tapering steroid therapy.Journal of Gastroenterology and Hepatology:Published 2020/9/18/li\u003e
- Hosotani K et al.:Underwater endoscopic mucosal resection for complete R0 removal of colorectal polyp in a patient with ulcerative colitis.Endoscopy : doi:10.1055/a-1346-8769,2021/2/16
- 田中由香里 他:オルメサルタン関連スプルー様腸疾患の内視鏡像.第104回日本消化器内視鏡学会近畿支部例会,Web,2020/6/27
- 森久芳樹 他:血友病患者に発症し、大量出血を来したカンピロバクター腸炎の一例.第104回日本消化器内視鏡学会近畿支部例会,Web,2020/6/27
- 長尾宗一郎 他:ワルファリン内服中に生じた亜全周性大腸粘膜下血腫の一例.第104回日本消化器内視鏡学会近畿支部例会,Web,2020/6/27
- 秋山慎介 他:十二指腸憩室出血に対する内視鏡治療の現状.第104回日本消化器内視鏡学会近畿支部例会,Web,2020/6/27
- 秋山慎介:表在性非乳頭部十二指腸上皮性腫瘍(SNADET).日本消化器病学会第106回総会,Web,2020/8/11-13
- 和田将弥:当院切除例からの膵粘液性嚢胞腫瘍(MCN)の手術適応の検討.日本消化器病学会第106回総会,Web,2020/8/11-13
- 占野尚人:当院における中・下咽頭表在癌に対する経口切除の現状.日本消化器病学会第106回総会,Web,2020/8/11-13
- 田中由香里 他:当院における免疫チェックポイント阻害薬による肝障害を発症した症例の検討.日本消化器病学会第106回総会,Web,2020/8/11-13
- 森田周子:経過観察した早期胃癌7症例の経過.第99回日本消化器内視鏡学会総会,京都/Web,2020/9/2-3
- 森田周子:Endocytoは食道扁平上皮癌の診断に有効か?-エビデンスを踏まえて-.第99回日本消化器内視鏡学会総会,京都/Web,2020/9/3
- 秋山慎介 他:当院における胃粘膜下腫瘍に対する腹腔鏡内視鏡合同手術の現状.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 井上聡子:潰瘍性大腸炎に対するトファシチニブの短期および長期治療効果.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 谷口洋平 他:TS1膵癌切除例における腫瘍サイズ10mm以下での検討.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 田中由香里 他:当院における免疫チェックポイント阻害薬関連腸炎の臨床像.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 安藤徳晃 他:EUS-FNAで組織診断を行った十二指腸NETの1例.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 上田智也 他:十二指腸穿破による消化管出血を契機に診断し得た解離性肝動脈瘤の一例.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 鄭 浩柄 他:sequential therapyを念頭に置いた分子標的治療薬による進行肝細胞癌治療戦略.日本消化器病学会近畿支部第113回例会,大阪,2020/10/3
- 小久保結未 他:進行肝細胞癌に対するソラフェニブ投与中に脳梗塞を発症した1例.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 竜野稜子 他:高度の肝機能障害とネフローゼ症候群を契機に診断された原発性アミロイドーシスの一例.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 長尾宗一郎 他:肝動脈瘤破裂を初発症状とした結節性多発動脈炎の一例.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 丹家元祥 他:当院の進行膵管癌における術後肝転移再発についての検討.日本消化器病学会近畿支部第113回例会,大阪/抄録,2020/10/3
- 安藤徳晃 他:当院における十二指腸NET9例の検討.JDDW2020,神戸/Web,2020/11/5
- 谷口洋平 他:膵癌術前ドレナージにおけるMetallic Stent vs Plastic Stentの比較.JDDW2020,神戸/Web,2020/11/5
- 森田周子:局注針を使用しないステロイド粘膜下層局注.第74回日本食道学会学術集会,徳島/Web,2020/12/10-11
- 長尾宗一郎 他:後出血ハイリスク患者におけるESD後粘膜欠損の予防的縫縮術について.第105回日本消化器内視鏡学会近畿支部例会,京都/Web,2020/12/19
- 田中由香里 他:超拡大内視鏡による観察が診断に有用であった表在食道癌の一例.第105回日本消化器内視鏡学会近畿支部例会,京都/Web,2020/12/19
- 秋山慎介 他:十二指腸憩室出血に対する止血術の現状.第105回日本消化器内視鏡学会近畿支部例会,京都/Web,2020/12/19
- 谷口洋平 他:当院における総胆管結石採石困難例における電気水圧衝撃破砕療法(EHL)の検討.第105回日本消化器内視鏡学会近畿支部例会,京都/Web,2020/12/19
- 唐渡修一郎 他:食道裂孔ヘルニアに伴う胃軸捻転症に対して内視鏡的整復を施行後、待機的に外科手術を行った1例.第105回日本消化器内視鏡学会近畿支部例会,京都/Web,2020/12/19
- 安藤徳晃 他:十二指腸Brunner腺過誤腫の内視鏡的切除にS-O clip が有用であった一例.第105回日本消化器内視鏡学会近畿支部例会,京都/Web,2020/12/19
- 竜野稜子 他:自己免疫性膵炎に合併した十二指腸GISTの一例.第105回日本消化器内視鏡学会近畿支部例会,京都/Web,2020/12/19
- 和田将弥:膵神経内分泌腫瘍診断におけるソマトスタチン受容体シンチグラフィ,FDG-PETの成績.第51回日本膵臓学会大会,神戸/Web,2021/1/8
- 竜野稜子 他:高度の肝機能障害を契機に診断された生体肝移植後のde novo自己免疫性肝炎の一例.日本消化器病学会近畿支部第114回例会,Web,2021/2/27
- 長尾宗一郎 他:診断に難渋した、正常肝に発生した肝外発育型肝細胞癌の一例.日本消化器病学会近畿支部第114回例会,Web,2021/2/27
- 安藤徳晃 他:PDL-1高発現を認めたLymphocyte-rich HCCの1切除例.日本消化器病学会近畿支部第114回例会,Web,2021/2/27
- 田中由香里 他:免疫チェックポイント阻害薬長期使用中にirAEとして小腸炎を発症した一例.日本消化器病学会近畿支部第114回例会,Web,2021/2/27
- 唐渡修一郎 他:腸重積症にて発症した小腸Burkittリンパ腫の1例.日本消化器病学会近畿支部第114回例会,Web,2021/2/27
- Kitamoto H et al.:A Rare Tumor Disseminated to the Gastrointestinal Tract After Treatment for HIV-Associated Lymphoproliferative Disease.Gastroenterology 2019 Volume156 Issue8 Pages2136–2138,2019/6/1
- Kitamoto H et al.:Chronic GI bleeding in a middle-aged woman.Gut Aug 2019, Volume68 Issue8,1385-1429,2019/8/1
- Kitamoto H et al.:Scanning early catches the worm:abdominal ultrasound as a possible screening method for intestinal cestodes.Lancet Vol.394 No.10205,2019/10/5
- 文原大貴 他:当院におけるレゴラフェニブ不応例に対するレンバチニブの使用経験.第55回日本肝臓学会総会,東京,2019/5/30
- 和田将弥:膵周囲液体貯留に対する超音波内視鏡下膵嚢胞.第97回日本消化器内視鏡学会総会,東京,2019/5/31
- 森田周子:表在咽頭腫瘍における深達度の内視鏡診断.第97回日本消化器内視鏡学会総会,東京,2019/5/31
- 谷口洋平:中下悪性胆道狭窄に対する術前full covered metallic stent(fCSEMS)の検討.第97回日本消化器内視鏡学会総会,東京,2019/6/1
- 占野尚人:胃癌ESD非治癒切除例の検討.第97回日本消化器内視鏡学会総会,東京,2019/6/1
- 森田周子:壁深達度T4b症例の臨床経過.第73回日本食道学会学術集会,福岡,2019/6/6
- 田中由香里 他:内視鏡的止血が困難であった非静脈瘤性上部消化管出血に対する緊急IVRの検討.第102回日本消化器内視鏡学会近畿支部例会,大阪,2019/7/6
- 井上聡子 他:潰瘍性大腸炎に伴うcolitic cancerの臨床像.第102回日本消化器内視鏡学会近畿支部例会,大阪,2019/7/6
- 上田智也 他:腹腔鏡下胆嚢摘出術後の難治性胆汁瘻に対してFully Covered Self Expandable Metallic Stent留置が有用であった一例.第102回日本消化器内視鏡学会近畿支部例会,大阪,2019/7/6
- 長尾宗一郎 他:腎細胞癌膵転移との鑑別にEUS-FNAが有用であった微小PanNETの一例.第102回日本消化器内視鏡学会近畿支部例会,大阪,2019/7/6
- 大久保佑樹 他:ステロイドにより軽快したペムブロリズマブ関連胃炎の一例.第102回日本消化器内視鏡学会近畿支部例会,大阪,2019/7/6
- 池田結香 他:急激な進行をたどった消化管アミロイドーシスに対してトシリズマブが著効した一例.第102回日本消化器内視鏡学会近畿支部例会,大阪,2019/7/6
- 文原大貴 他:通常内視鏡観察での発見、全貌観察が困難であった下咽頭癌の2例.第102回日本消化器内視鏡学会近畿支部例会,大阪,2019/7/6
- 秋山慎介 他:食道顆粒細胞腫に対するESDの経験.第102回日本消化器内視鏡学会近畿支部例会,大阪,2019/7/6
- 唐渡修一郎 他:当院における上部消化管内視鏡的異物除去症例の検討.第102回日本消化器内視鏡学会近畿支部例会,大阪,2019/7/6
- 谷口洋平 他:膵癌に対する術前胆道ドレナージの検討-Metallic Stent vs Plastic Stent-.第50回日本膵臓学会大会,東京,2019/7/12
- 和田将弥 他:ペムブロリズマブによる免疫関連有害事象と思われる膵炎の一例.第50回日本膵臓学会大会,東京,2019/7/12
- 和田将弥 他:当院における膵粘液性嚢胞腫瘍(MCN)切除例の検討.第50回日本膵臓学会大会,東京,2019/7/13
- 秋山慎介 他:胃粘膜下腫瘍に対するEUS-FNAの有用性の検討.日本消化器病学会近畿支部第111回例会,大阪,2019/10/5
- 細谷和也 他:胃癌ESD後eCuraC-2例の検討.日本消化器病学会近畿支部第111回例会,大阪,2019/10/5
- 唐渡修一郎 他:Gemcitabine+nab-Paclitaxel併用療法が奏功し、Conversion surgery可能となった局所進行切除不能膵癌の1例.日本消化器病学会近畿支部第111回例会,大阪,2019/10/5
- 長尾宗一郎 他:下行結腸狭窄に対して外科的治療を要した潰瘍性大腸炎の一例.日本消化器病学会近畿支部第111回例会,大阪,2019/10/5
- 文原大貴 他:レゴラフェニブ不応の肝細胞癌に対して長期間レンバチニブが有効である一例.日本消化器病学会近畿支部第111回例会,大阪,2019/10/5
- 田中由香里 他:抗PD-1抗体によるステロイド抵抗性の高度肝障害に対してミコフェノール酸モフェチルが著効した一例.日本消化器病学会近畿支部第111回例会,大阪,2019/10/5
- 上田智也 他:びまん性肝内動門脈シャントに伴う門脈圧亢進症に対して肝動脈塞栓術が有用であった一例.日本消化器病学会近畿支部第111回例会,大阪,2019/10/5
- 大久保佑樹 他:出血を契機に診断しえた肝細胞癌胃転移の1例.日本消化器病学会近畿支部第111回例会,大阪,2019/10/5
- 森田周子:消化管領域における内視鏡医療 診断から治療まで.第64回日本口腔外科学会総会・学術大会,北海道,2019/10/27
- 田中由香里:当院における免疫チェックポイント阻害薬による肝障害を発症した症例の検討.第43回日本肝臓学会西部会,下関,2019/12/12
- 細谷和也 他:抗血栓薬内服例における2nd lookの意義に関する検討.第103回日本消化器内視鏡学会近畿支部例会,大阪,2020/1/18
- 秋山慎介 他:当院における表在性非乳頭部十二指腸上皮性腫瘍に対するEMRの現状.第103回日本消化器内視鏡学会近畿支部例会,大阪,2020/1/18
- 大久保佑樹 他:出血を契機に診断しえた肝細胞癌胃転移の2例.第103回日本消化器内視鏡学会近畿支部例会,大阪,2020/1/18
- 戸田 潤 他:多彩な内視鏡像を呈した腸管濾胞性リンパ腫の1例.第103回日本消化器内視鏡学会近畿支部例会,大阪,2020/1/18
- 唐渡修一郎 他:NBI拡大観察によりAIN(Anal intraepitherial neoplasia)と診断した病変に対してESDを施行した1例.第103回日本消化器内視鏡学会近畿支部例会,大阪,2020/1/18
- 重里徳子 他:内視鏡像と病理所見が乖離した好酸球性胃腸炎の一例.第103回日本消化器内視鏡学会近畿支部例会,大阪,2020/1/18
- 長尾宗一郎 他:腸管空腸吻合部完全閉塞に対して経皮胆道鏡とシングル-ン内視鏡(SBE)によるランデブー法が有用であった一例.第103回日本消化器内視鏡学会近畿支部例会,大阪,2020/1/18
- 上田智也 他:Mirizzi症候群に対して経口胆道鏡下での電気水圧衝撃波破砕術(EHL)が有用であった1例.第103回日本消化器内視鏡学会近畿支部例会,大阪,2020/1/18
- 文原大貴 他:膵管、胆管拡張を来した、術前診断に難渋したNET-G3の一例.第103回日本消化器内視鏡学会近畿支部例会,大阪,2020/1/18
- 井上聡子:潰瘍性大腸炎に対するトファシチニブの当院の使用経験.日本消化器病学会近畿支部第112回例会,京都,2020/2/29
- 杉之下与志樹 他:日本消化器病学会近畿支部第112回例会.京都,2020/2/29
- 鄭 浩柄 他:ソラフェニブの治療効果を踏まえた分子標的治療薬による進行肝細胞癌治療戦略.日本消化器病学会近畿支部第112回例会,京都,2020/2/29
- 大久保佑樹 他:当院におけるTS1膵癌の臨床および画像的特徴についての検討.日本消化器病学会近畿支部第112回例会,京都,2020/2/29
- 文原大貴 他:レンバチニブ中止後に急速進行を認めた進行肝細胞癌の2例.日本消化器病学会近畿支部第112回例会,京都,2020/2/29
- 重里徳子 他:PBC・AIHの病態を異時性に示したPBC-AIH Overlap症候群の1例.日本消化器病学会近畿支部第112回例会,京都,2020/2/29
- 上田智也 他:バスケット嵌頓の解除に経口胆道下での電気水圧衝撃波破砕術(EHL)が有用であった1例.日本消化器病学会近畿支部第112回例会,京都,2020/2/29
- 和田将弥 他:膵内分泌腫瘍診断においてソマトスタチン受容体シンチグラフィは有用か?.日本消化器病学会近畿支部第112回例会,京都,2020/2/29
- 占野尚人 他:(追加発言)高齢者における中・下咽頭癌の経口的切除.日本消化器病学会近畿支部第112回例会,京都,2020/2/29
- 戸田 潤 他:当院で経験した日本海裂頭条虫の4例.日本消化器病学会近畿支部第112回例会,京都,2020/2/29
- Ueno Y:CORRELATION BETWEEN ENDOSCOPIC FEATURES AND HISTOLOGICAL SUBTYPES OF SMALL INTESTINAL LYMPHOMAS ESGE2019,Prague,2019/4/5
- Morita S:ENDOSCOPIC SUBEPITHELIAL DISSECTION FOR SUPERFICIAL PHARYNGEAL CANCER: A CASE SERIES OF 44 SUPERFICIAL CANCERS.ESGE2019,Prague,2019/4/5
- Toyonaga H et al.:Traumatic bile duct neuroma diagnosed by boring biopsy with cholangioscopy.Gastrointestinal EndoscopyVolume87, Issue 5, p1361–1362,May2018(published online 2017/11/1),2018/5/1
- 谷口洋平 他:当院におけるTS1膵癌の検討.第104回日本消化器病学会総会,東京,2018/4/20
- 谷口洋平 他:悪性胆道狭窄に対するMetallic stent胆管内留置法の検討.第95回日本消化器内視鏡学会総会,東京,2018/5/10
- 井上貴裕 他:中・下咽頭表在癌における局所切除術の治療成績.第95回日本消化器内視鏡学会総会,東京,2018/5/10
- 大久保佑樹 他:メッケル憩室診断におけるバルーン内視鏡の有用性.第95回日本消化器内視鏡学会総会,東京,2018/5/10
- 井上聡子 他:小腸および大腸狭窄に対する内視鏡的バルーン拡張術.第95回日本消化器内視鏡学会総会,東京,2018/5/10
- 文原大貴 他:当院における自己免疫性膵炎に対してのEUS-FNAによる病理診断能について.第95回日本消化器内視鏡学会総会,東京,2018/5/11
- 福島政司 他:当院における消化管出血に対する緊急バルーン内視鏡の現状.第95回日本消化器内視鏡学会総会,東京,2018/5/11
- 和田将弥 他:膵癌動体追尾強度変調放射線治療のための金マーカー留置方法としてのEUS下留置術の有用性.日本消化器内視鏡学会第100回近畿支部例会,大阪,2018/5/26
- 占野尚人 他:胃ESDにおける抗血栓薬の取り扱い.日本消化器内視鏡学会第100回近畿支部例会,大阪,2018/5/26
- 井上貴裕 他:けん引クリップを用いた大腸ESDの治療成績、およびESD初学者における同クリップの使用経験.日本消化器内視鏡学会第100回近畿支部例会,大阪,2018/5/26
- 上野由香里 他:当院で経験した乳癌胃転移4症例の検討.日本消化器内視鏡学会第100回近畿支部例会,大阪,2018/5/26
- 豊永啓翔 他:Cronkhite Canada症候群の胃病変における発症前後の所見.日本消化器内視鏡学会第100回近畿支部例会,大阪,2018/5/26
- 池田結香 他:当院で経験した虚血性小腸炎3症例の検討.日本消化器内視鏡学会第100回近畿支部例会,大阪,2018/5/26
- 大久保佑樹 他:バルーン内視鏡で止血し得た小腸多発inflammatory CAP polypの一例.日本消化器内視鏡学会第100回近畿支部例会,大阪,2018/5/26
- 文原大貴 他:乳頭部出血に対してfully covered metallic stent留置後に仮性動脈瘤破裂を合併して一例.日本消化器内視鏡学会第100回近畿支部例会,大阪,2018/5/26
- 青山直樹 他:著明な主膵管拡張をきたし、膵管鏡が診断に有用であった膵管癒合不全の1例.日本消化器内視鏡学会第100回近畿支部例会,大阪,2018/5/26
- 鄭 浩柄 他:核酸アナログ投与中のHBs抗原およびコア関連抗原低値例に対してPeg-INFα2aによるsequential therapyを行った2症例.第54回日本肝臓学会総会,大阪,2018/6/14
- 杉之下与志樹 他:C型肝炎ウイルス(HCV)抗体陽性症例に対する当院の取り組み.第54回日本肝臓学会総会,大阪,2018/6/14
- 井上貴裕 他:初学者における大腸ESDの治療成績についての検討.日本消化器病学会近畿支部第109回例会,大阪,2018/9/29
- 鄭 浩柄 他:当院におけるC型肝炎に対するDAA治療後発癌例に関する検討.日本消化器病学会近畿支部第109回例会,大阪,2018/9/29
- 谷口洋平 他:悪性胆道狭窄に対する術前full covered metallic stentの使用について.日本消化器病学会近畿支部第109回例会,大阪,2018/9/29
- 文原大貴 他:ソラフェニブ、レゴラフェニブ不応性の肝細胞癌に対してレンバチニブが有効であった一例.日本消化器病学会近畿支部第109回例会,大阪,2018/9/29
- 上野由香里 他:ダブルバルーン内視鏡で診断したオルメサルタン関連スプルー様腸疾患の一例.日本消化器病学会近畿支部第109回例会,大阪,2018/9/29
- 豊永啓翔 他:繰り返し専攻をきたしたtrisomy8陽性骨髄異形成症候群併発腸管ベーチェット病の1例.日本消化器病学会近畿支部第109回例会,大阪,2018/9/29
- 池田結香 他:当院における過去8年間の急性E型肝炎に関する検討.日本消化器病学会近畿支部第109回例会,大阪,2018/9/29
- 大久保佑樹 他:小腸癌術後に腹膜転移により小腸穿孔を来した一例.日本消化器病学会近畿支部第109回例会,大阪,2018/9/29
- 青山直樹 他:肺腺癌治療中にEUS-FNAで診断しえた転移性膵腫瘍の1例.日本消化器病学会近畿支部第109回例会,大阪,2018/9/29
- 杉之下与志樹:超音波の未来を切り拓く.日本超音波医学会第45回関西地方学術集会,神戸,2018/10/20
- 鄭 浩柄:超音波の未来を切り拓く.日本超音波医学会第45回関西地方学術集会,神戸,2018/10/20
- 青山直樹 他:当院における膵神経内分泌腫瘍(PNET)50例の画像所見についての検討.JDDW2018,神戸,2018/11/3
- 和田将弥 他:当院における膵周囲液体貯留に対する超音波内視鏡下水嚢胞ドレナージ術(EUS-CD)の工夫.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 占野尚人 他:残胃癌のESD -縫合線上の切除-.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 井上貴裕 他:当院における咽頭癌早期診断への内視鏡的アプローチ.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 青山直樹 他:繰り返す腸閉塞をきっかけに診断された非特異性多発性小腸潰瘍の1例.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 文原大貴 他:小腸NETの2例.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 池田結香 他:当院で経験した肺癌小腸転移の4例.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 上野由香里 他:胃粘膜に炭酸ランタンの沈着を認めた透析患者の一例.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 大久保佑樹 他:小腸癌診断におけるダブルバルーン内視鏡の有用性.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 上田智也 他:乳癌術後21年経過して、胃・十二指腸・大腸に多発転移をきたした1例.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 豊永啓翔 他:十二指腸閉塞を来した膵悪性リンパ腫の1例.第101回日本消化器内視鏡学会近畿支部例会,大阪,2018/11/10
- 福島政司 他:当院で経験したオルメサルタン関連スプルー様腸疾患の検討.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- 谷口洋平 他:当院における膵神経内分泌腫瘍(PNET)の診療の現況.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- 鄭 浩柄 他:当院における進行肝細胞癌に対するレゴラフェニブ投与例の検討.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- 豊永啓翔 他:咽頭、食道、大腸にmultiple lymphomatous polyposisを呈したマントル細胞リンパ腫の1例.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- 大久保佑樹 他:悪性幽門狭窄の診断に超音波内視鏡下穿刺吸引法(EUS-FNA)が有用であった一例.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- 上野由香里 他:小腸悪性リンパ腫の診断におけるダブルバルーン内視鏡検査の有用性.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- 青山直樹 他:IVRによって治療しえた回腸動静脈奇形の1例.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- 池田結香 他:生体肝移植後の高度黄疸を伴ったC型肝炎再発に対してSOF/LDVが奏功した1症例.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- 文原大貴 他:当院における難治性腹水に対するトルバプタン治療効果に関する考察.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- 平井達基 他:胆管内乳頭状腫瘍の一切除例.日本消化器病学会近畿支部第110回例会,京都,2019/2/23
- Taniguchi Y:Intraductal vs. transpapillary fully covered self-expandable metal sent placement for malignant biliary stricture .DDW2018,Washington,DC,2018/6/2-5
- Okubo Y et al.:Usefulness of double-balloon enteroscopy for diagnosis of Meckel’s diverticulum.UEG2018,Vienna,2018/10/20-24
- Toyonaga H et al.:Preoperative biliary drainage using plastic stents versus self-expandable metal stents for periampullary cancer.UEG2018,Vienna,2018/10/20-24
- Fukushima M:Investigation of cases of obscure gastrointestinal bleeding and small bowel bleeding that led to rebleeding.Gastro2018,Bangkok,2018/12/5-8
- Hatamori H,Wada M,Taniguchi Y,Inokuma T:Pancreatic pseudocyst localized in the gastric wall after EUS-guided FNA of type 1 autoimmune pancreatits.Gastrointestinal Endoscopy Vol.86 Issue5 P919-921,2017/6/2
- Ogawa S , Imai Y , Inokuma T : Mimicking Gastric Natural Killer/T-Cell Lymphoma . Gastroenterology Vol.153 Issue1 e22-e23,2017/6/2
- Toyonaga H,Masashi F,Inokuma T,Imai Y:Mantle cell lymphoma involving the esophagus evaluated by magnifying endoscopy with narrow-band imaging.Gastrointestinal Endoscopy Volume87 Issue1 P305-306,January2018,published online 2017/7/15
- Toyonaga H,Taniguchi Y,Inokuma T:Traumatic bile duct neuroma diagnosed by boring biopsy with cholangioscopy . Gastrointestinal Endoscopy Volume87 Issue 5 P1361 – 1362,May2018,published online 2017/11/1
- Toyonaga H,Morita S,Inokuma T,Ezoe Y(Ishikawa Gastrienterology Clinic):Cricoid pressure to prevent gastric deflation during esophagogastroduodenoscopy.VIDEOGIE Volume3 Issue3 P102-105,March2018,published online 2017/12/12
- 谷口洋平:膵腫瘍性病変に対するコイル型シースを有する EZ Shot 3 plus の使用経験について.第 103 回日本消化器病学会,東京,2017/4/22
- 森田周子:ポスター会場 3(大阪国際会議場 3 階 イベントホール)ポスター14 胃-ESD 後出血.第 93 回日本消化器内視鏡学会総会,大阪,2017/5/11
- Taniguchi Y,Wada M,Inokuma T:Cross-wired metallic stents for bilateral endoscopic stent placement for malignant hilar biliary obstruction(非切除悪性肝門部胆管狭窄に対する stent in stent での Metallic stent 留置について).第 93 回日本消化器内視鏡学会総会,大阪,2017/5/11
- 福島政司,井上聡子,猪熊哲朗:【追加発言】再出血を来した原因不明消化管出血、小腸出血症例の 検討.第 93 回日本消化器内視鏡学会総会,大阪,2017/5/11
- 占野尚人:80 歳以上の高齢者の胃癌に対する ESD.第 93 回日本消化器内視鏡学会総会,大阪, 2017/5/11
- 青山直樹,占野尚人,大久保佑樹,文原大貴,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,谷口洋平, 福島政司,和田将弥,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:当院における上部 消化管内視鏡的異物除去症例の検討.第 93 回日本消化器内視鏡学会総会,大阪,2017/5/11
- 豊永啓翔,谷口洋平,青山直樹,奥村 圭,畑森裕之,伊藤卓彦,松本一寛,北本博規,福島政司, 占野尚人,森田周子,井上聡子,和田将弥,鄭 浩柄,杉之下与志樹,猪熊哲朗:消化管穿孔、瘻孔 に対する OTSC system の治療成績と安全性の検討.第 93 回日本消化器内視鏡学会総会,大阪, 2017/5/11
- 和田将弥,谷口洋平,青山直樹,豊永啓翔,奥村 圭,畑森裕之,伊藤卓彦,松本一寛,北本博規, 福島政司,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,今井幸弘,猪熊哲朗:当院に おける転移性膵腫瘍に対する EUS-FNA の成績.第 93 回日本消化器内視鏡学会総会,大阪,2017/5/11
- 畑森裕之,福島政司,大久保佑樹,文原大貴,青山直樹,豊永啓翔,奥村 圭,井上貴裕,谷口洋平, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:緊急ダブルバルー ン内視鏡下 ERCP の有用性、安全性についての検討.第 93 回日本消化器内視鏡学会総会,大阪, 2017/5/12
- 森田周子,占野尚人,猪熊哲朗:80 歳以上の早期胃癌内視鏡的粘膜下層剥離術施行症例における予 後の検討.第 93 回日本消化器内視鏡学会総会,大阪,2017/5/12
- 鄭 浩柄,杉之下与志樹,谷口洋平,福島政司,和田将弥,猪熊哲朗:当院におけるジェノタイプ1 型 C 型肝硬変症例に対する DAAs 治療効果について.第 53 回日本肝臓学会総会,広島,2017/6/8- 6/9
- 占野尚人,福島政司,森田周子,猪熊哲朗,今井幸弘:当院における咽頭腫瘍の内視鏡切除.第 98 回日本消化器内視鏡学会近畿支部例会,神戸,2017/6/17
- 和田将弥,谷口洋平,猪熊哲朗:当院における膵疾患に対する診断的EUS-FNAの現状.第98回日 本消化器内視鏡学会近畿支部例会,神戸,2017/6/17
- 畑森裕之,谷口洋平,福島政司,和田将弥,猪熊哲朗:術後再建腸管の総胆管結石症例に対するダブ ルバルーン内視鏡 EPLBD の有用性、安全性についての検討.第 98 回日本消化器内視鏡学会近畿支 部例会,神戸,2017/6/17
- 豊永啓翔,占野尚人,青山直樹,奥村 圭,畑森裕之,伊藤卓彦,松本一寛,北本博規,谷口洋平, 福島政司,和田将弥,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗,上原慶一郎:メト トレキサート関連リンパ増殖性疾患の一例.第 98 回日本消化器内視鏡学会近畿支部例会,神戸, 2017/6/17
- 青山直樹,福島政司,豊永啓翔,奥村 圭,畑森裕之,伊藤卓彦,松本一寛,北本博規,谷口洋平, 和田将弥,森田周子,占野尚人,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗,上原慶一郎:オル メサルタン内服が原因と考えられるスプルー様腸疾患の 1 例.第 98 回日本消化器内視鏡学会近畿支 部例会,神戸,2017/6/17
- 奥村 圭,井上聡子,青山直樹,豊永啓翔,畑森裕之,伊藤卓彦,松本一寛,北本博規,谷口洋平, 福島政司,和田将弥,森田周子,占野尚人,鄭 浩柄,杉之下与志樹,猪熊哲朗:診断に難渋し急速 に病状が進行した小腸 T cell lymphoma の一例.第 98 回日本消化器内視鏡学会近畿支部例会,神 戸,2017/6/17
- 大久保佑樹,占野尚人,文原大貴,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,谷口洋平, 福島政司,和田将弥,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗,今井幸弘:EMR にて切除しえた十二指腸 Brunner 腺癌の 2 例.第 98 回日本消化器内視鏡学会近畿支部例会,神戸, 2017/6/17
- 井上貴裕,谷口洋平,松本一寛,青山直樹,豊永啓翔,奥村 圭,畑森裕之,福島政司,和田将弥, 占野尚人,森田周子,鄭 浩柄,井上聡子,杉之下与志樹,猪熊哲朗:経乳頭的ドレナージ術が有用 であった門脈内穿破を来した膵仮性嚢胞の 1 例.第 98 回日本消化器内視鏡学会近畿支部例会,神 戸,2017/6/17
- 文原大貴,森田周子,大久保佑樹,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,谷口洋平, 福島政司,和田将弥,占野尚人,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗,貝原 聡:胆嚢十 二指腸瘻の 2 例.第 98 回日本消化器内視鏡学会近畿支部例会,神戸,2017/6/17
- 片山宜郎,和田将弥,大久保佑樹,文原大貴,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕, 谷口洋平,福島政司,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:十二指 腸NETの4例 -当院での治療経験の検討-.第98回日本消化器内視鏡学会近畿支部例会,神戸, 2017/6/17
- 森田周子:内視鏡的胃全層切除の現状と可能性.ENDOSCOPY FORUM JAPAN 2017,小樽, 2017/8/5-6
- 杉之下与志樹,鄭 浩柄,和田将弥,猪熊哲朗:ジェノタイプ 1b 型 C 型肝炎に対する DAAs 治療 効果と治療後肝細胞癌発症例の検討.日本消化器病学会近畿支部第 107 回例会,大阪,2017/9/23
- 和田将弥,谷口洋平,猪熊哲朗,今葷倍敏行:局所進行切除不能膵癌に対する動体追尾 IMRT のた めの EUS 下金マーカー留置術.日本消化器病学会近畿支部第 107 回例会,大阪,2017/9/23
- 奥村 圭,杉之下与志樹,大久保佑樹,文原大貴,青山直樹,豊永啓翔,畑森裕之,井上貴裕,谷口 洋平,福島政司,和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,猪熊哲朗:当院における難 治性腹水に対するトルバプタンの有効性の検討.日本消化器病学会近畿支部第 107 回例会,大阪, 2017/9/23
- 文原大貴,谷口洋平,大久保佑樹,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,福島政司, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:術後難治性胆汁瘻 に対して fully covered self expandable metallic stent 留置が有用であった一例.日本消化器病学会 近畿支部第 107 回例会,大阪,2017/9/23
- 青山直樹,福島政司,大久保佑樹,文原大貴,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,谷口洋平, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗,今井幸弘:当院に おける小腸濾胞性リンパ腫についての検討.日本消化器病学会近畿支部第 107 回例会,大阪, 2017/9/23
- 大久保佑樹,福島政司,文原大貴,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,谷口洋平, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:メッケル憩室診断 におけるバルーン内視鏡の有用性.日本消化器病学会近畿支部第 107 回例会,大阪,2017/9/23
- 城田祥吾,井上聡子,大久保佑樹,文原大貴,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕, 谷口洋平,福島政司,和田将弥,占野尚人,森田周子,鄭 浩柄,杉之下与志樹,猪熊哲朗:大量出 血を繰り返し、小腸内視鏡が有用であった若年発症の空腸動脈瘤.日本消化器病学会近畿支部第 107 回例会,大阪,2017/9/23
- 福島政司,井上聡子,猪熊哲朗:オルサルメタン関連スプルー様腸疾患の臨床像.JDDW2017,福 岡,2017/10/13
- 谷口洋平,青山直樹,豊永啓翔,奥村 圭,畑森裕之,福島政司,和田将弥,占野尚人,森田周子, 井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:当院における膵癌診療の現状について.JDDW2017, 福岡,2017/10/14
- 森田周子:パネルディスカッション 1 (第 2 会場 東館 3F 大会議場) 早期がん非治癒切除症例 の長期予後.第 99 回日本消化器内視鏡学会近畿支部例会,京都,2017/11/18
- 谷口洋平:肝・膵臓 (第 6 会場 東館 2F 視聴覚研修室).第 99 回日本消化器内視鏡学会近畿支部 例会,京都,2017/11/18
- 谷口洋平,和田将弥,猪熊哲朗:当院におけるTS1膵癌の臨床的および画像的特徴の検討.第99回 日本消化器内視鏡学会近畿支部例会,京都,2017/11/18
- 井上貴裕,森田周子,占野尚人,猪熊哲朗,前田紘奈:当院において局所切除術を施行した中・下咽 頭表在癌の長期予後.第 99 回日本消化器内視鏡学会近畿支部例会,京都,2017/11/18
- 豊永啓翔,福島政司,大久保佑樹,文原大貴,青山直樹,奥村 圭,畑森裕之,井上貴裕,谷口洋平, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:Upside-downstomach を呈した横隔膜傍裂孔ヘルニアの 1 例.第 99 回日本消化器内視鏡学会近畿支部例会,京都, 2017/11/18
- 大久保佑樹,谷口洋平,文原大貴,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,福島政司, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:通過障害を来し内 視鏡的に診断し得た乳癌転移の 2 例.第 99 回日本消化器内視鏡学会近畿支部例会,京都,2017/11/18
- 奥村 圭,占野尚人,大久保佑樹,文原大貴,青山直樹,豊永啓翔,畑森裕之,井上貴裕,谷口洋平, 福島政司,和田将弥,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:治療に伴う経過を 追えた胃・大腸 Kaposi 肉腫の 1 例.第 99 回日本消化器内視鏡学会近畿支部例会,京都,2017/11/18
- 青山直樹,和田将弥,大久保佑樹,文原大貴,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,谷口洋平, 福島政司,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗,今井幸弘:EUS- FNA で術前診断しえた胃 Glomus 腫瘍の一例.第 99 回日本消化器内視鏡学会近畿支部例会,京都, 2017/11/18
- 井上聡子,福島政司,猪熊哲朗:クローン病に対する内視鏡的バルーン拡張術の有効性と限界.第99 回日本消化器内視鏡学会近畿支部例会,京都,2017/11/18
- 畑森裕之,谷口洋平,大久保佑樹,文原大貴,青山直樹,豊永啓翔,奥村 圭,井上貴裕,福島政司, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:難治性胆管空腸吻 合部狭窄に対して fully covered self-expandable metal stent 留置が奏功した一例.第 99 回日本消 化器内視鏡学会近畿支部例会,京都,2017/11/18
- 文原大貴,井上聡子,大久保佑樹,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,谷口洋平, 福島政司,和田将弥,占野尚人,森田周子,鄭 浩柄,杉之下与志樹,猪熊哲朗:初回内視鏡で診断 に至らなかった大腸動静脈奇形の 2 例.第 99 回日本消化器内視鏡学会近畿支部例会,京都, 2017/11/18
- 上田智也,占野尚人,大久保佑樹,文原大貴,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕, 谷口洋平,福島政司,和田将弥,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:腹部超 音波検査(US)が診断に有用であった小腸アニサキス症の 1 例.第 99 回日本消化器内視鏡学会近畿支 部例会,京都,2017/11/18
- 占野尚人,福島政司,森田周子,猪熊哲朗:当院における胃癌ESD非治癒切除例の検討.日本消化 器病学会近畿支部第 108 回例会,京都,2018/3/17
- 福島政司,井上聡子,猪熊哲朗,今井幸弘:当院における小腸悪性腫瘍の診断と臨床像.日本消化器 病学会近畿支部第 108 回例会,京都,2018/3/17
- 鄭 浩柄,杉之下与志樹,猪熊哲朗:当院におけるC型肝炎に対するDAA治療成績とSVR後発癌. 日本消化器病学会近畿支部第 108 回例会,京都,2018/3/17
- 大久保佑樹,谷口洋平,文原大貴,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,福島政司, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:悪性胆道狭窄に金 属ステント留置後胆道出血をきたした 1 例.日本消化器病学会近畿支部第 108 回例会,京都, 2018/3/17
- 豊永啓翔,福島政司,大久保佑樹,文原大貴,青山直樹,奥村 圭,畑森裕之,井上貴裕,谷口洋平, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗:出血制御のため緊 急手術を要した小腸 GIST の 1 例.日本消化器病学会近畿支部第 108 回例会,京都,2018/3/17
- 文原大貴,杉之下与志樹,大久保佑樹,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,谷口 洋平,福島政司,和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,猪熊哲朗:慢性C型肝炎 に対する直接作用型抗ウイルス薬(DAA)治療後に自己免疫肝炎を発症した一例.日本消化器病学会 近畿支部第 108 回例会,京都,2018/3/17
- 青山直樹,谷口洋平,大久保佑樹,文原大貴,豊永啓翔,奥村 圭,畑森裕之,井上貴裕,福島政司, 和田将弥,占野尚人,森田周子,井上聡子,鄭 浩柄,杉之下与志樹,猪熊哲朗,今井幸弘:通常型 膵管癌との鑑別に EUS-FNA が有用であった NEC(neuroendocrine carcinoma)の一例.日本消化器 病学会近畿支部第 108 回例会,京都,2018/3/17
- 唐渡修一郎,井上聡子,大久保佑樹,文原大貴,青山直樹,豊永啓翔,井上貴裕,谷口洋平,福島政 司,和田将弥,占野尚人,森田周子,鄭 浩柄,杉之下与志樹,猪熊哲朗:限局性上部消化管アミロ イドーシスの 2 例.日本消化器病学会近畿支部第 108 回例会,京都,2018/3/17
- 長尾宗一郎,井上聡子,大久保佑樹,文原大貴,青山直樹,豊永啓翔,奥村 圭,畑森裕之,井上貴 裕,谷口洋平,福島政司,和田将弥,占野尚人,森田周子,鄭 浩柄,杉之下与志樹,猪熊哲朗:イ レウスで発症した回腸子宮内膜症の 2 例.日本消化器病学会近畿支部第 108 回例会,京都,2018/3/17
- Taniguchi Y:CROSS-WIRED METALLIC STENTS IN ENDOSCOPIC BILATERAL STENT-IN- STENT PLACEMENT FOR MALIGNANT HILAR BILIARY OBSTRUCTION.DDW2017, Chicago,2017/5/9
- HatamoriH,FukushimaM,InokumaT:Efficacyandsafetyofurgentdoubleballoonenteroscopy- assisted endoscopic retrograde cholangiopancreatography.APDW2017,Hong Kong,2017/9/23- 26
- InoueT,TaniguchiY,InokumaT:Endoscopicpapillarylargeballoondilationforlargeormultiple common bile duct stones: efficacy, safety, and stone recurrence.APDW2017,Hong Kong, 2017/9/23-26
- Taniguchi Y,Inokuma T:APDW2017.Hong Kong,2017/9/25,Toyonaga H,Taniguchi Y, Inokuma T:Treatment results and safety of over-the-scope-clip system for gastrointestinal tract perforations and fistulas.APDW2017,Hong Kong,2017/9/25
- Toyonaga H,Taniguchi Y,Wada M,Inokuma T:Unilateral versus bilateral stent-in-stent placement of metal stents for malgnant hilar biliary obstruction.UEG2017,Barcelona, 2017/10/28-11/1
- 福島政司 他:オルメサルタン関連スプルー様腸疾患の 1 例.胃と腸 第 51 巻 第 4 号 P497-502,2016/4/25
- 南出竜典 他:von Hippel-Lindau 病に合併した多発性膵神経内分泌腫瘍の一例.膵臓 V ol.31 No.2 P150-157,2016/4/25
- 北本博規 他:経皮内視鏡的胃瘻造設時に胃粘膜下血腫を来し、術後早期にバンパー埋没症候群を合併した 1 例.在宅医療と内視鏡治療 vol.20 No.1,2016/9/1
- 伊藤卓彦 他:NBI拡大観察により早期肛門扁平上皮癌と診断した病変に対しESDを施行した 1 例.Gastroenterological Endoscopy Vol.58(9),2016/9/20
- 森田周子 他:食道・Barrett 食道 症例アトラス 5 食道表在癌(0-IIa+IIc).新しい診断基準・分類に基づいた NBI/BLI/LCI 内視鏡アトラス 第 1 版第 1 刷 (株)日本メディカルセンター (東京),2016/10/20
- Ito T et al.:The prospect of endoscopic submucosal dissection for early anal canal squamous cell carcinoma.Clinical Journal of Gastroenterology Vol.9 Issue6 P384-388,2016/12/1
- 畑森裕之 他:胆嚢十二指腸瘻を形成した悪性胃十二指腸狭窄に対する内視鏡的十二指腸ステント留置術において側孔付バルーンカテーテルが有用であった 1 例.Gastrological Endoscopy Vol.59(1),2017/1/25
- 鄭 浩柄 他:当院におけるダクラタスビル・アスナプレビル併用療法の成績.第102回日本消 化器病学会総会,東京,2016/4/21
- 井上聡子:third line therapy としての抗 TNF-α抗体治療が有効であった潰瘍性大腸炎 3 例の検 討.第 102 回日本消化器病学会総会,東京,2016/4/21
- 谷口洋平 他:当院における内鏡的乳頭括約筋切除術(EST)+大口径バルーン拡張術(EPLBD)について.第 102 回日本消化器病学会総会,東京,2016/4/23
- 奥村 圭 他:当院における Helicobacter pylori の除菌における除菌率についての検討.第 102 回日本消化器病学会総会,東京,2016/4/23
- 北本博規 他:当院における高齢者に対する経皮内視鏡的胃瘻造設症例の検討.第91回日本消化 器内視鏡学会総会,東京,2016/5/12
- 畑森裕之 他:当院におけるS状結腸軸捻転症51例の臨床的検討.第91回日本消化器内視鏡学会総会,東京,2016/5/12
- 福島政司:当院における小腸悪性腫瘍診断のストラテジー.第91回日本消化器内視鏡学会総会, 東京,2016/5/13
- 谷口洋平:経下部消化管からの超音波内視鏡下穿刺吸引術(EUS-FNA)について.第91回日本消化器内視鏡学会総会,東京,2016/5/13
- 伊藤卓彦 他:当院における悪性腫瘍による Gastric Outlet Obstruction(GOO)に対するステント留置療法の有用性の検討.第 91 回日本消化器内視鏡学会総会,東京,2016/5/13
- 松本一寛 他:当院における大腸ステント留置症例の検討.第91回日本消化器内視鏡学会総会, 東京,2016/5/13
- 森田周子:ハンズオン 4 女性指導医による胃 ESD.第 91 回日本消化器内視鏡学会総会,東京, 2016/5/14
- Kitamoto H et al.:Clinical features of Cytomegalovirus enterocolitis(当院における CMV 腸炎症 例の検討).第 91 回日本消化器内視鏡学会総会,東京,2016/5/14
- 和田将弥 他:当院におけるジェノタイプ2型C型慢性肝炎・肝硬変に対するソホスビル/リバビリン併用療法の治療成績.第 52 回日本肝臓学会総会,千葉,2016/5/19
- 北本博規 他:当院における小腸悪性腫瘍に対する内視鏡的アプローチについて.日本消化器内視鏡学会近畿支部第 96 回支部例会,京都,2016/6/11
- 占野尚人 他:当院における胃体部大弯ESDにおけるアプローチ.日本消化器内視鏡学会近畿支部第 96 回支部例会,京都,2016/6/11
- 青山直樹 他:内視鏡的に観察・診断しえた食道 GIST の一例.日本消化器内視鏡学会近畿支部 第 96 回支部例会,京都,2016/6/11
- 伊藤卓彦 他:出血コントロールに難渋し、腹腔鏡下に切除した胃glomus腫瘍の1例.日本消化器内視鏡学会近畿支部第 96 回支部例会,京都,2016/6/11
- 畑森裕之 他:内視鏡像を確認出来た軽症腸管糞線虫症の1例.日本消化器内視鏡学会近畿支部 第 96 回支部例会,京都,2016/6/11
- 奥村 圭 他:当院における大腸憩室出血に対する EBL(Endoscopic Band Ligation)の検討.日 本消化器内視鏡学会近畿支部第 96 回支部例会,京都,2016/6/11
- 松本一寛 他:Choledochoceleの1例.日本消化器内視鏡学会近畿支部第96回支部例会,京都, 2016/6/11
- 北本博規:潰瘍性大腸炎に合併したCytomegalovirus腸炎の再発に関する検討.第7回日本炎症性 腸疾患学会学術集会,京都,2016/7/10
- 北本博規:急性発症の嚥下障害に対する経皮内視鏡的胃瘻造設術の検討.第 21 回 PEG・在宅医 療研究会学術集会,高松,2016/9/3
- 北本博規 他:チオプリン製剤の副作用と最適化.日本消化器病学会近畿支部第105回例会,大 阪,2016/9/17
- 鄭 浩柄 他:当院におけるダクラスタビル+アスナプレビル併用療法の成績.日本消化器病学会 近畿支部第 105 回例会,大阪,2016/9/17
- 谷口洋平 他:非切除悪性肝門部胆道狭窄に対するBONASTENTM-Hilar使用によるstentinstent について.日本消化器病学会近畿支部第 105 回例会,大阪,2016/9/17
- 豊永啓翔 他:急性肝不全を呈した Epstein-Barr Virus 関連血球貪食性リンパ組織球症の 1 例. 日本消化器病学会近畿支部第 105 回例会,大阪,2016/9/17
- 奥村 圭 他:肝硬変患者の難治性腹水に対する腹水濾過濃縮再静注療法(CART)の検討.日本消化器病学会近畿支部第 105 回例会,大阪,2016/9/17
- 畑森裕之 他:自己免疫性膵炎に対する EUS-FNA 施行後に特異的な形態を呈する膵液瘻を来した一例.日本消化器病学会近畿支部第 105 回例会,大阪,2016/9/17
- 伊藤卓彦 他:血を契機に発見され、EUS-FNAで診断することができた胃迷入膵の一例.日本消化器病学会近畿支部第 105 回例会,大阪,2016/9/17
- 青山直樹 他:小腸内視鏡で経過観察しえたII型腸管症関連T細胞リンパ腫(ESTL)の3例.日本消化器病学会近畿支部第 105 回例会,大阪,2016/9/17
- 松本一寛 他:内視鏡的硬化療法を行った十二指腸静脈瘤破裂の一例.日本消化器病学会近畿支部第 105 回例会,大阪,2016/9/17
- 和田将弥 他:当院における狭義の先天性胆道拡張症の検討.第52回日本胆道学会学術集会,横浜,2016/9/30
- 占野尚人 他:当院における胃癌ESD非切除例の検討.JDDW2016,神戸,2016/11/3
- 井上聡子 他:当院における好酸球性胃腸炎の臨床像.JDDW2016,神戸,2016/11/4
- 谷口洋平 他:当院における非切除悪性肝門部胆道狭窄に対する Self-expandable metallicstent(SEMS)について.JDDW2016,神戸,2016/11/5
- 和田将弥 他:当院におけるEUS-FNAの偶発症についての検討.JDDW2016,神戸,2016/11/5
- 占野尚人 他:高齢者早期胃癌に対するESD.日本消化器内視鏡学会近畿支部第97回支部例会,京都,2016/11/26
- 森田周子 他:[追加発言]拾い上げ困難な食道癌症例の検討 -過去 2 年以内に上部消化管内視鏡施行したが指摘できなかった当院での食道癌症例の検討-.日本消化器内視鏡学会近畿支部第97 回支部例会,京都,2016/11/26
- 和田将弥 他:当院における膵癌に対する EUS-FNA の現状.日本消化器内視鏡学会近畿支部第97 回支部例会,京都,2016/11/26
- 松本一寛 他:食道癌を侵入門戸としたリステリア菌血症の一例.日本消化器内視鏡学会近畿支部第 97 回支部例会,京都,2016/11/26
- 伊藤卓彦 他:重篤な出血をきたしたため外科的に切除した胃平滑筋腫の一例.日本消化器内視鏡学会近畿支部第 97 回支部例会,京都,2016/11/26
- 青山直樹 他:下部消化管内視鏡検査時に偶然発見、摘除した鞭虫症の1例.日本消化器内視鏡学会近畿支部第 97 回支部例会,京都,2016/11/26
- 畑森裕之 他:EUS-FNAで診断困難であった脱分化型脂肪肉腫の一例.日本消化器内視鏡学会近畿支部第 97 回支部例会,京都,2016/11/26
- 奥村 圭 他:大量出血を契機に発見された小腸悪性リンパ腫の1例.日本消化器内視鏡学会近畿支部第 97 回支部例会,京都,2016/11/26
- 北本博規 他:内視鏡的経過を追えている Lymphomatoid Gastropathy の 1 例.日本消化器内視鏡学会近畿支部第 97 回支部例会,京都,2016/11/26
- 豊永啓翔 他:胆道鏡(SpyGlassTMDS)による観察、生検が診断に有用であった胆管断端神経腫の1 例.日本消化器内視鏡学会近畿支部第 97 回支部例会,京都,2016/11/26
- 谷口洋平 他:膵腫瘍に対するEZShot3plusの使用経験について.日本消化器病学会近畿支部第106 回例会,大阪,2017/2/25
- 北本博規 他:全胃幽門輪温存膵頭十二指腸切除後の残膵膵石に対して内視鏡治療を行った1例. 日本消化器病学会近畿支部第 106 回例会,大阪,2017/2/25
- 奥村 圭 他:急激に進行した関節リウマチに伴う消化管アミロイドーシスの1例.日本消化器 病学会近畿支部第 106 回例会,大阪,2017/2/25
- 青山直樹 他:十二指腸副乳頭神経内分泌腫瘍の1例.日本消化器病学会近畿支部第106回例会, 大阪,2017/2/25
- 畑森裕之 他:当院におけるS状結腸軸捻転の検討.日本消化器病学会近畿支部第106回例会, 大阪,2017/2/25
- 豊永啓翔 他:過粘稠性 Klebsiella pneumoniae による侵襲性肝膿瘍症候群.日本消化器病学会近 畿支部第 106 回例会,大阪,2017/2/25
- Ito T et al.:Predictive Factors for Efficacy of Tolvaptan in Patients With Refractory Ascites in Decompensated Liver Cirrhosis.Digestive Disease Week 2016,San Diego,2016/5/21
- Ito T et al.:The Efficacy of an Endoscopic Self-Expandable Metal Stent for Gastric Outlet Obstruction by Malignancies.Digestive Disease Week 2016,San Diego,2016/5/23
- Taniguchi Y et al.:A Newly Designed Cross-Wired Metallic Stent for Unresectable Malignant Hilar Bile Duct Obstruction .Digestive Disease Week 2016,San Diego,2016/5/24
- KitamotoHetal.:Cytomega1ovirusenterocolitisinpatientswithulcerativecolitis.AOCC2016,Kyoto, 2016/7/7-9
- Matsumoto K et al.:Feasibility and safety of laparoscopic and endoscopic surgery for gastric submucosal tumors .UEG 2016,Vienna Austria,2016/10/15-19
- Hatamori H et al.:Efficacy and safety of urgent double balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography.UEG 2016,Vienna Austria,2016/10/15-19
- Morita S:Current status of GI women in Asia.APDW2016,Kobe,2016/11/5
- Kitamoto H et al.:Regorafenib-Induced Hyperammonemic Encephalopathy in Metastatic Colon Cancer.Journal of Cancer Prevention & Current Reseach,Vol.3 No.2 00076,2015/10/19
- Minamide T et al.:A case of arteriovenous malformation of the small intestine treated by endoscopic therapy.GASTROENTEROLOGICAL ENDOSCOPY Vol.57 No.10 P2448-2454,2015/10/29
- Ito T et al.:Gastric metastasis of pancreatic neuroendocrine tumor 5years after surgical resection of the primary lesion.Digestive Endoscopy Vol.27 No.7 P782,2015/11
- Matsumoto K et al.:Rupture of small intestinal varices treated by endoscopy. GASTROENTEROLOGICAL ENDOSCOPY Vol.57 No.11 P.2519-2523,2015/11/28
- Fukushima M et al.:Severe spruelike enteropathy associated whith olmesartan observed by double-ballon enteroscopy.GASTROINTESTINAL ENDOSCOPY Vol.83 No.1 P269-270,2016/1
- 北本博規 他:当院で小腸内視鏡で精査を行った小腸DLBCLの検討.第101回日本消化器病学会総会,仙台,2015/4/23
- 谷口洋平:当院における高齢者急性胆管炎についての検討.第101回日本消化器病学会総会,仙台,2015/4/23
- 鄭 浩柄 他:シメプレビル併用3剤治療市販後の実態と成績―当市内3施設における検討―.第51回日本肝臓学会総会,熊本,2015/5/21
- 伊藤卓彦 他:早期肛門管扁平上皮癌に対するESD治療の可能性.第89回日本消化器内視鏡学会総会,名古屋,2015/5/29
- 福島政司 他:当院における血管炎に起因する消化管病変の臨床的検討.第89回日本消化器内視鏡学会総会,名古屋,2015/5/29
- 北本博規 他:胆管空腸吻合部狭窄治療に対する通電ダイレーターの有用性について.第89回日本消化器内視鏡学会総会,名古屋,2015/5/29
- 北本博規 他:当院における悪性胃十二指腸狭窄症例に対するステント留置療法の現状について.第89回日本消化器内視鏡学会総会,名古屋,2015/5/29
- 和田将弥 他:当院における超音波内視鏡下膵嚢胞ドレナージ術(US-CD)の成績.第89回日本消化器内視鏡学会総会,名古屋,2015/5/30
- 占野尚人 他:バレット食道癌に対するESD.第89回日本消化器内視鏡学会総会,名古屋,2015/5/30
- 谷口洋平 他:当院での後期高齢者・超高齢者における総胆管結石に伴う急性胆管炎の治療について.第89回日本消化器内視鏡学会総会,名古屋,2015/5/30
- 和田将弥:当院における膵神経内分泌腫瘍(PNET)に対するEUS-FNAの検討.第46回日本膵臓学会大会,名古屋,2015/6/20
- 占野尚人 他:当院における大腸ESDの現状と治療の工夫.日本内視鏡学会第95回近畿支部例会,大阪,2015/6/20
- 谷口洋平 他:当院における後期高齢者・総胆管結石症についての検討.日本内視鏡学会第95回 近畿支部例会,大阪,2015/6/20
- 北本博規 他:当院における経皮内視鏡的胃瘻増設症例の検討.日本内視鏡学会第95回近畿支部例会,大阪,2015/6/20
- 畑森裕之:十二指腸ステント留置術の難渋例に対して結石除去用バルーンカテーテル(Bouncer)使用が有用であった1例.日本内視鏡学会第95回近畿支部例会,大阪,2015/6/20
- 細谷和也 他:小腸内視鏡が術前診断に有用であった小腸NETの一例.日本内視鏡学会第95回近畿支部例会,大阪,2015/6/20
- 松本一寛 他:門脈ガス血症をきたした虚血性小腸炎の一例.日本内視鏡学会第95回近畿支部例会,大阪,2015/6/20
- 奥村 圭 他:腸管嚢腫様気腫症(Pneumatosis cystoides intestinalis;PCI)を合併した潰瘍性大腸炎(Ulcerative Colitis;UC)の1例.日本内視鏡学会第95回近畿支部例会,大阪,2015/6/20
- 福島政司 他:オルメサルタン関連スプルー様腸疾患の1例.日本内視鏡学会第95回近畿支部例会,大阪,2015/6/20
- 伊藤卓彦 他:十二指腸乳頭癌術後19年後に肝門部胆管癌を認め、治癒しえた1例.日本内視鏡学会第95回近畿支部例会,大阪,2015/6/20
- 北本博規 他:Regorafenib療法中に肝性脳症を来したstageIV腸がんの2症例.第13回日本臨床腫瘍学会学術集会,札幌,2015/7/16
- 谷口洋平 他:胆管空腸吻合部狭窄に対する通電ダイレーターを用いた内視鏡治療の有用性について.第51回日本胆道学会学術集会,宇都宮,2015/9/17-18
- 伊藤卓彦 他:巨大肝嚢胞に対し、純エタノール注入療法が奏功した1例.第103回日本消化器病学会近畿支部例会,大阪,2015/9/26
- 北本博規 他:当院における便潜血検査陽性症例と大腸ポリープの関連について.第103回日本消化器病学会近畿支部例会,大阪,2015/9/26
- 奥村 圭 他:馬刺し摂取が原因と考えられた急性E型肝炎の1例.第103回日本消化器病学会近畿支部例会,大阪,2015/9/26
- 松本一寛 他:十二指腸に穿通したびまん性大細胞性B細胞リンパ腫(DLBCL)の一例.第103回日本消化器病学会近畿支部例会,大阪,2015/9/26
- 南出竜典 他:コーラ溶解法と内視鏡的砕石術が奏功した胃石の1例.第103回日本消化器病学会近畿支部例会,大阪,2015/9/26
- 畑森裕之 他:縦隔リンパ節腫大に対してEUS-FNA施行し結核性リンパ節炎と診断しえた一例.第103回日本消化器病学会近畿支部例会,大阪,2015/9/26
- 松本一寛 他:虚血性小腸炎の検討.JDDW2015,東京,2015/10/8
- 福島政司 他:当院における術後再建腸管に対するバルーン内視鏡を用いた緊急ERCPの現状.JDDW2015,東京,2015/10/8
- 細谷和也 他:当院における膵神経内分泌腫瘍(PNET)33例の検討.JDDW2015,東京,2015/10/8
- 南出竜典 他:当院における胃粘膜下腫瘍に対するLaparoscopy and endoscopy cooperative surgery(LECS) の現状 .JDDW2015,東京,2015/10/8
- 森田周子 他:表在咽頭腫瘍の深達度診断.JDDW2015,東京,2015/10/9
- 谷口洋平 他:当院における自己免疫性膵炎の臨床像と E U S – F N A の診断能について.JDDW2015,東京,2015/10/9
- 伊藤卓彦 他:当院における悪性腫瘍に伴うGastric outlet obstruction(GOO)に対するステント留置療法の有用性.JDDW2015,東京,2015/10/9
- 奥村 圭 他:腸管嚢腫様気腫症(PCI)の臨床的検討 ―慢性型と劇症型は同一疾患といえるか―.JDDW2015,東京,2015/10/9
- 北本博規 他:原因不明消化管出血症例に対する緊急カプセル内視鏡検査の有用性と限界について.JDDW2015,東京,2015/10/10
- 和田将弥 他:当院における消化管粘膜下腫瘍に対するEUS-FNAの成績.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 南出竜典 他:(追加発言2)当院における胃粘膜下腫瘍に対するLaparoscopy and endoscopy cooperative surgery(LECS)の現状.日本消化器内視鏡学会近畿支部第95回支部例会,大阪, 2015/11/7
- 谷口洋平 他:胆管空腸吻合部狭窄治療に対する通電ダイレーターの有用性について.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 福島政司 他:小腸悪性リンパ腫の内視鏡像の検討.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 北本博規 他:当院における急性GVHD腸炎の検討.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 奥村 圭 他:胸痛で発症した食道粘膜下血腫の1例.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 南出竜典 他:悪性リンパ腫化学療法後に発症した播種性糞線虫症の一例.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 松本一寛 他:診断に難渋した顕微鏡的多発血管炎による小腸潰瘍の一例.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 畑森裕之 他:びまん性変化を来した腸管MALTリンパ腫の一例.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 伊藤卓彦 他:悪性腫瘍による十二指腸狭窄に対するEvolutionの有用性.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 伊藤純子 他:カプセル内視鏡が滞留しダブルバルーン内視鏡で回収を行った小腸濾胞性リンパ腫の一例.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 辻坂勇太 他:胃潰瘍出血を契機に虚血性小腸炎を発症し、門脈ガス血症をきたした一例.日本消化器内視鏡学会近畿支部第95回支部例会,大阪,2015/11/7
- 北本博規 他:当院における経皮内視鏡的胃瘻増設症例の検討.第19回日本病態栄養学会学術集会,横浜,2016/1/9
- 細谷和也 他:当院における膵神経内分泌腫瘍(PNET)の検討.日本消化器病学会近畿支部第104回例会,大阪,2016/2/6
- 松本一寛 他:内臓逆位症に合併した膵性胸水の一例.日本消化器病学会近畿支部第104回例会,大阪,2016/2/6
- 畑森裕之 他:内視鏡所見の経時的変化を追えた好酸球性腸炎の一例.日本消化器病学会近畿支部第104回例会,大阪,2016/2/6
- 南出竜典 他:内視鏡的に観察しえた多発小腸血管腫の一例.日本消化器病学会近畿支部第104回例会,大阪,2016/2/6
- 伊藤卓彦 他:当院における肝硬変に伴う難治性腹水にたいするトルバブスタンの有効性の検討.日本消化器病学会近畿支部第104回例会,大阪,2016/2/6
- 奥村 圭 他:肝臓内に好酸球性肉芽腫を形成した1例.日本消化器病学会近畿支部第104回例会,大阪,2016/2/6
- 北本博規 他:粘膜下腫瘍の形態を呈した小腸動脈瘤の1例.日本消化器病学会近畿支部第104回例会,大阪,2016/2/6
- Ito T et al.:The Efficacy of an endoscopic self-expandable metal stent for gastric outlet obstruction by malignancies.23rd United European Gastroenterology Week,Barcelona,2015/10/24-28
- Fukushima M et al.:Usefulness of double-balloon enteroscopy for diagnosis of Meckel’s diverdiculum.Asian Pacific Digestive Week 2015,Taipei,2015/12/3-6
- Taniguchi Y:Evaluation of treatment for acute cholangitis in the elderly patients.Asian Pacific Digestive Week2015,Taipei,2015/12/3-6
- Kitamoto H et al.:Usefulness and Limitations of emergent capsule endoscopy in patients with obscuregastrointestinal bleeding.Asian Pacific Digestive Week2015,Taipei,2015/12/3-6
- Hosotani K et al.:Endoscopic removal of foreign bodies from the gastrointestinal tract: Retrospective analysis of 284 patients .Asian Pacific Digestive Week2015,Taipei,2015/12/3-6
- Minamide T et al.:Pancreatic Lesions with von Hippel-Lindau Disease.Asian Pacific Digestive Week 2015,Taipei,2015/12/3-6
- Matsumoto K et al.:The characteristics of ischemic enteritis.Asian Pacific Digestive Week 2015,Taipei,2015/12/3-6
- 福島 政司:ダブルバルーン内視鏡で経過観察しえたenteropathy-associated T-cell lymphomaの1例.胃と腸 第49巻第9号別刷,2014/8/25
- Fukushima M et al.:A case series of Meckel’s diverticulum:usefulness of double-ballon enteroscopy for diagnosis.BMC Gastroenterology 2014(Vol.14),2014/8/30
- Ogawa S et al.:Case of primary hepatic gastrinoma:Diagnostic usefulness of the selective arterial calcium injection test.Hepatology Research (Article first published online:18 Sep2014), 2014/9/18
- Fukushima M et al.:Granulocytic sarcoma of the small intestine in a prtient with chronic myelomonocytic leukemia ,Diagestive Endoscopy 2014(Vol.26:757-758), 2014/11/3
- 小川 智 他:MRI検査が診断に有用であった空腸異所性膵癌の1例.日本消化器病学会雑誌 Vol.112(2015) No.1 P70~77,2015/1/5
- 松本 知訓 他:II.各論 特殊な組織型(臨床病理学的特徴) 粘液癌/印環細胞癌.日本臨床 73巻増刊号3(2015年3月20日発行) P754~757,2015/3/20
- 藤田 幹夫 他:進行再発大腸癌に対する一次治療としての F O L F O X 6 /SOX+Cetuximab療法についての検討.第100回日本消化器病学会総会,東京,2014/4/24
- 小川 智 他:肝Reactive Lymphoid Hyperplasia 3症例における造影超音波検査所見の検討.日本超音波医学会第87回学術集会,横浜,2014/5/9-11
- 福島 政司 他:消化管濾胞性リンパ腫の診断、治療、予後.第87回日本消化器内視鏡学会総会,福岡,2014/5/15-17
- 北本 博規 他:当院における成人腸重積症の検討.第87回日本消化器内視鏡学会総会,福岡,2014/5/15-17
- 北本 博規 他:当院における悪性胃十二指腸狭窄症例に対するステント留置療法の現状について.第87回日本消化器内視鏡学会総会,福岡,2014/5/15-17
- 細谷 和也 他:当院における消化管異物の経験例.第87回日本消化器内視鏡学会総会,福岡,2014/5/15-17
- 占野 尚人 他:超高齢者に対する胃ESD.第87回日本消化器内視鏡学会総会,福岡,2014/5/15-17
- 谷口 洋平 他:胆管金属ステント留置後の急性胆嚢炎に対する胆嚢ドレナージ術(PTGBD)後、超音波内視鏡下胆嚢ドレナージ術(EUS-GBD).第87回日本消化器内視鏡学会総会,福岡,2014/5/15-17
- 谷口 洋平 他:内視鏡的乳頭切開術(EST)+大口径バルーン拡張術(FPLBD)の治療成績および再発のリスクと短期・中期経過についての検討.第87回日本消化器内視鏡学会総会,福岡,2014/5/15-17
- 和田 将弥 他:当院における胆管結石に対するEndoscopic papillary large balloon dilation(EPLBD)の検討.第87回日本消化器内視鏡学会総会,福岡,2014/5/15-17
- 占野 尚人 他:バレット食道腺癌に対するESD症例の検討.第92回日本消化器内視鏡学会近畿支部例会,大阪,2014/6/21
- 南出 竜典 他:虚血性小腸炎の検討.第92回日本消化器内視鏡学会近畿支部例会, 大阪,2014/6/21
- 福島 政司 他:当院における特発性腸間膜静脈硬化症の臨床的検討.第92回日本消化器内視鏡学会近畿支部例会,大阪,2014/6/21
- 和田 将弥 他:当院における消化管粘膜下腫瘍の診断と治療の現況.第92回日本消化器内視鏡学会近畿支部例会,大阪,2014/6/21
- 細谷 和也 他:粘膜下腫瘍様の形態を呈した食道癌の一例.第92回日本消化器内視鏡学会近畿支部例会,大阪,2014/6/21
- 松本 一寛 他:胃腺内分泌細胞癌と腺癌の同時多発胃癌の一例.第92回日本消化器内視鏡学会近畿支部例会,大阪,2014/6/21
- 伊藤 卓彦 他:膵神経内分泌腫瘍(P-NET)の切除5年後に転移性胃腫瘍として再発した1例.第92回日本消化器内視鏡学会近畿支部例会,大阪,2014/6/21
- 北本 博規 他:術前診断し得た主膵管進展したPNETの1例.第92回日本消化器内視鏡学会近畿支部例会,大阪,2014/6/21
- 藤田 幹夫 他:A Retrospective Study of HER2-status and Combined Chemotherapy with Trastuzumab in Advanced Gastric Cancer(当院におけるHER2 陽性進行再発胃癌の検討).第12回日本臨床腫瘍学会学術集会,福岡,2014/7/17-19
- 藤田 幹夫 他:消化器癌化学療法における部分的脾動脈塞栓術の有用性.第52回日本癌治療学会学術集会,横浜,2014/8/28-30
- 谷口 洋平 他:内視鏡的乳頭切開術(EST)+大口径バルーン拡張術(FPLBD)の治療成績および再発についての検討.第50回日本胆道学会学術集会,東京,2014/9/26-27
- 和田 将弥 他:当院におけるラージバルーンによる胆管結石除去術の試み.第101回 日本消化器病学会近畿支部例会,大阪,2014/10/4
- 北本 博規 他:膵癌との鑑別が困難であった限局性自己免疫膵炎の1手術例.第101回日本消化器病学会近畿支部例会,大阪,2014/10/4
- 畑森 裕之 他:EUS-FNAで診断し、胸腔鏡下切除しえた巨大食道平滑筋腫の1例. 第101回日本消化器病学会近畿支部例会,大阪,2014/10/4
- 細谷 和也 他:当院の胃静脈瘤出血に対するヒストアクリルを用いた胃静脈瘤硬化 療法の現状.第101回日本消化器病学会近畿支部例会,大阪,2014/10/4
- 南出 竜典 他:内視鏡的粘膜切除術によって診断し得た小腸動静脈奇形の一例.第 101回日本消化器病学会近畿支部例会,大阪,2014/10/4
- 松本 一寛 他:Sequential療法が奏功したB型肝炎の一例.第101回日本消化器病学会近畿支部例会,大阪,2014/10/4
- 伊藤 卓彦 他:回盲部炎を契機とした腸重責症を引き起こし回盲部切除術に至った1例.第101回日本消化器病学会近畿支部例会,大阪,2014/10/4
- 井上 聡子 他:潰瘍性大腸炎に対する当院のタクロリムス治療の検討.第101回日本消化器病学会近畿支部例会,大阪,2014/10/4
- 藤田 幹夫 他:Her2陽性治癒切除不能進行再発胃癌の検討.JDDW2014,神戸,2014/10/23
- 谷口 洋平 他:内視鏡的乳頭括約筋切除術(EST)+大口径バルーン拡張術(EPLBD)の治療成績および再発について.JDDW2014,神戸,2014/10/24
- 伊藤 卓彦 他:当院で経験した転移性胃腫瘍の検討.JDDW2014,神戸,2014/10/25
- 和田 将弥 他:当院におけるSolid-pseudopapillary neoplasm(SPN)7例の検討.JDDW2014,神戸,2014/10/25
- 松本 一寛 他:当院における胃内分泌細胞癌の検討.JDDW2014,神戸,2014/10/ 25
- 細谷 和也 他:当院における小腸GIST12例の検討.JDDW2014,神戸,2014/10/26
- 占野 尚人 他:抗血栓薬内服と胃ESDの偶発性.第93回日本消化器内視鏡学会近畿支部例会,大阪,2014/11/15
- 福島 政司 他:当院における術後再建腸管に対するバルーン内視鏡を用いたERCPの治療成績.第93回日本消化器内視鏡学会近畿支部例会,大阪,2014/11/15
- 北本 博規 他:当院における原因不明消化管出血例に対するカプセル内視鏡の有用性について.第93回日本消化器内視鏡学会近畿支部例会,大阪,2014/11/15
- 伊藤 卓彦 他:肛門管扁平上皮癌に対し、内視鏡的粘膜剥離術ESDにて治癒切除しえた一例.第93回日本消化器内視鏡学会近畿支部例会,大阪,2014/11/15
- 松本 一寛 他:EVLおよびAethoxysklerol血管外注入により止血を得た小腸静脈瘤破裂の一例.第93回日本消化器内視鏡学会近畿支部例会,大阪,2014/11/15
- 北本 博規 他:肝細胞腺腫との鑑別を要した巨大肝血管筋脂肪腫の1例.日本超音波医学会第41回関西地方会学術集会,京都,2014/11/22
- 鄭 浩柄 他:B型慢性肝炎・肝硬変に対する核酸アナログの有効性と限界について.第102回日本消化器病学会近畿支部例会,京都,2015/2/21
- 福島 政司 他:当院における消化管出血に対する緊急バルーン内視鏡の現状.第102回日本消化器病学会近畿支部例会,京都,2015/2/21
- 細谷 和也 他:経過中勞瘻孔形成を認めたが、集学的治療によりQOLの改善と比較的長期の生存が得られた切除不能進行食道癌の一例.第102回日本消化器病学会近畿支 部例会,京都,2015/2/21
- 南出 竜典 他:爪楊枝による胃壁内膿瘍の一例.第102回日本消化器病学会近畿支部例会,京都,2015/2/21
- 北本 博規 他:耳下腺MALTリンパ腫の治療後に小腸DLBCLを合併した1例.第102 回日本消化器病学会近畿支部例会,京都,2015/2/21
- 伊藤 卓彦 他:血栓塞栓用ビーズを用いて少ない副作用で治療できた巨大肝細胞癌の1例.第102回日本消化器病学会近畿支部例会,京都,2015/2/21
- 松本 一寛 他:遺残胆嚢肝癌の一例.第102回日本消化器病学会近畿支部例会,京都,2015/2/21
- Taniguchi Y et al.:Efficacy and Safety Endoscopic papillary large balloon dilation following with an Endoscopic sphincterotomy (EST+EPLBD) for large or multiple common bile duct stones(CBDS). APDW2014, Indonesia. 2014/11/22-25
- Inokuma T et al.:Clinical consideration of metastatic gastric tumor. APDW2014, Indonesia,2014/11/22-25
- Fujita M et al.:A phase II study of 5-FU/I-LV/oxaliplatin(mFOLFOX6)in patisnts with metastatic or unresectable small bowel adenocarcinoma: A post hoc analysis.ASCO-GI,San Francisco,2015/1/15-17