当科では、ともに循環器センターを構成する心臓血管外科をはじめ、臨床検査技術部 生理検査部門、放射線技術部、臨床工学技術部、リハビリテーション技術部、薬剤部、看護部など数多くの部署との協同により、日々、心臓・血管疾患に対する質の高い診療を行うように心がけています。近年、大動脈弁狭窄症へのカテーテル治療(TAVI)や心臓リハビリテーションに代表されるように、内科、外科の垣根や職種の垣根を越えて患者さんにより良い医療を提供するという共通の目的を持つハートチームによって診療を行うという姿勢が益々重要となっていますが、我々も実践し心臓・血管疾患の内科的治療から外科手術までをスムーズに提供しています。対象となる疾患の特徴からも、また、本院が神戸市の基幹病院、救命救急センターであることからも救急患者、重症患者を多く診療しており、循環器内科への年間入院患者のかなりの割合を、CCUなどへの緊急入院患者が占めています。循環器疾患の診断においては、冠動脈造影に比べてより低侵襲的な検査としての320列MDCTによる冠動脈病変の評価、心疾患診療に必須である質の高い経胸壁心エコー図、経食道心エコー図検査、さらには心臓MRIや心臓核医学検査など、さまざまな検査機器と手法を駆使し、正確な診断と病態の評価、治療方針の決定に役立てています。
冠動脈疾患や不整脈の診療では、クリニカル・パスを積極活用し1泊2日、または日帰りでの冠動脈造影診断、2泊3日の冠動脈インターベンション治療(PCI)、3泊4日の心房細動アブレーション治療などを行い、短い入院期間で安全に効果的な診療を行うよう努めています。
さらに、上述したTAVIのほか、ペースメーカー、植え込み型除細動器、心不全に対する心臓再同期治療(両心室ペーシング)、僧帽弁狭窄に対する経皮的バルーン拡張術、僧帽弁閉鎖不全症に対する経皮的僧帽弁接合不全修復術、経皮的心房中隔欠損閉鎖術、経皮的左心耳閉鎖術など、さまざまな非薬物治療にも積極的に取り組んでいます。このように当科では、循環器疾患の広い分野の診療を高いレベルで行なっていますが、これら最新の医療機器による治療の前提として、冠動脈疾患や心不全における生活習慣の改善や患者さんごとの最適な薬物治療がまず必須であり、その点では心臓リハビリテーションによる総合的な患者指導などが大いに役立っています。
また、先進的な医療を早くから提供できる体制と意識を常に維持するよう、臨床研究の成果を国内外の学会や論文で発表することにも積極的に取り組んでおり、将来の循環器診療の進歩のために多くの多施設共同研究にも参加しています。
当科では、各分野のエキスパートからなるチーム体制を整えています。
循環器内科医、心臓血管外科医、麻酔科医,画像診断専門医、看護師、放射線技師、臨床工学技士など多職種にわたるスタッフが、「ハートチーム」を形成し、それぞれの専門分野の知識や技術を持ち寄って、患者さんにとって最適と思われる治療法を選択し、治療を行っています。

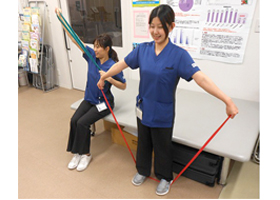
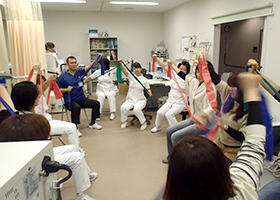
医師、看護師、理学療法士、栄養士、薬剤師、臨床心理士などの多くの職種が参加して、「心リハチーム」を形成し、患者さんにとって最適な心臓リハビリを行っています。

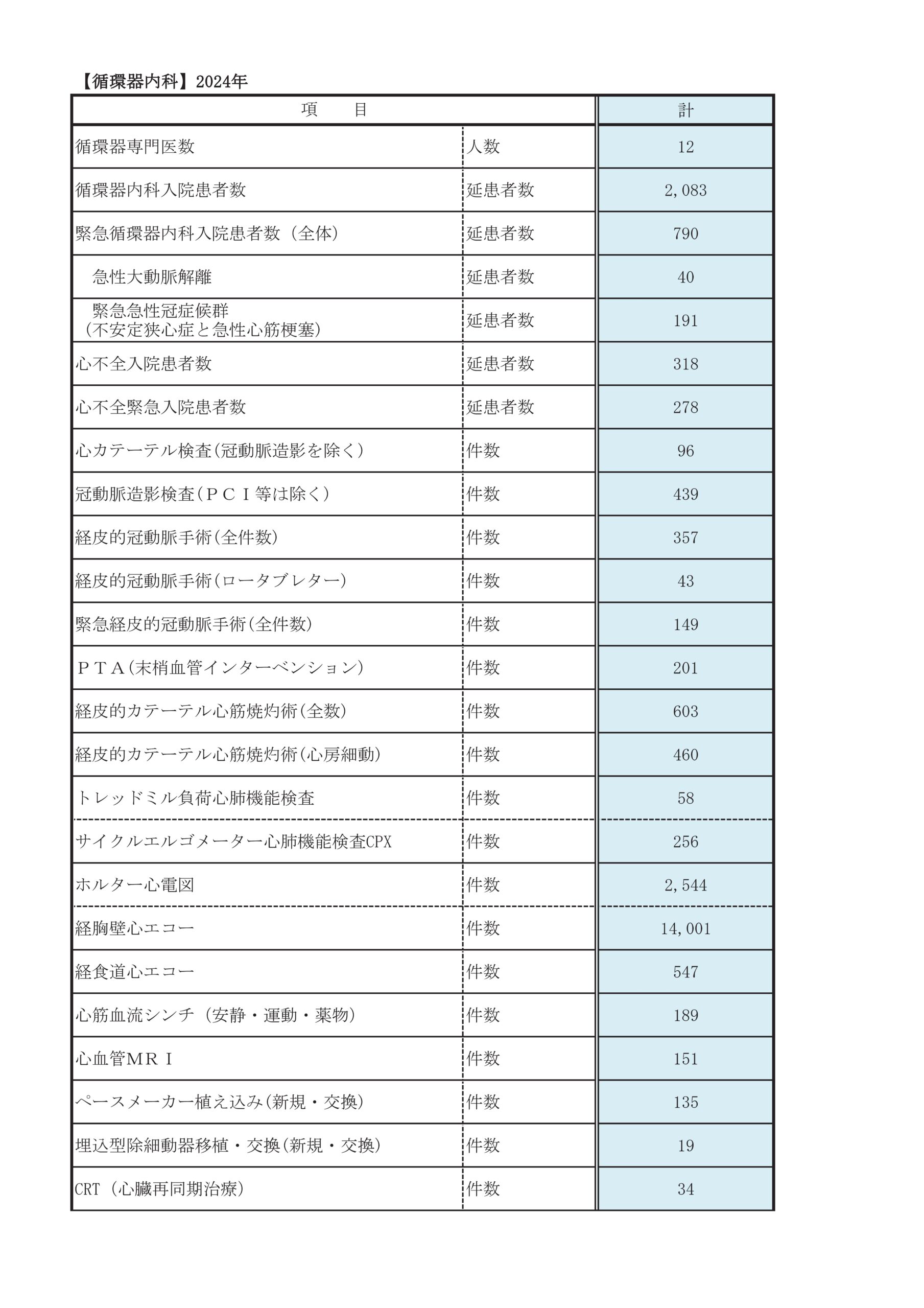
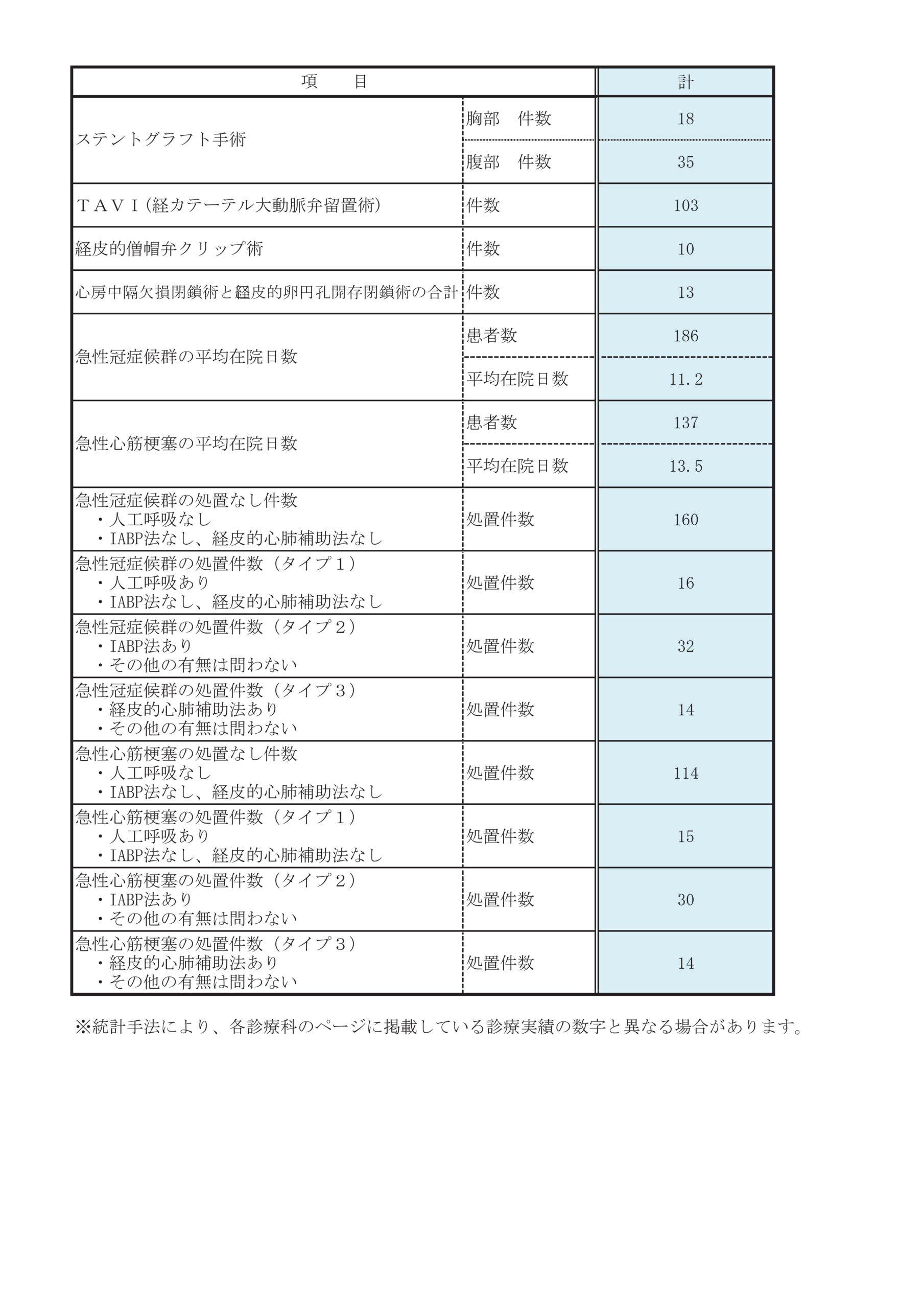
診療実績
主な疾患・治療法
患者さんとそのご家族、一般の方へ
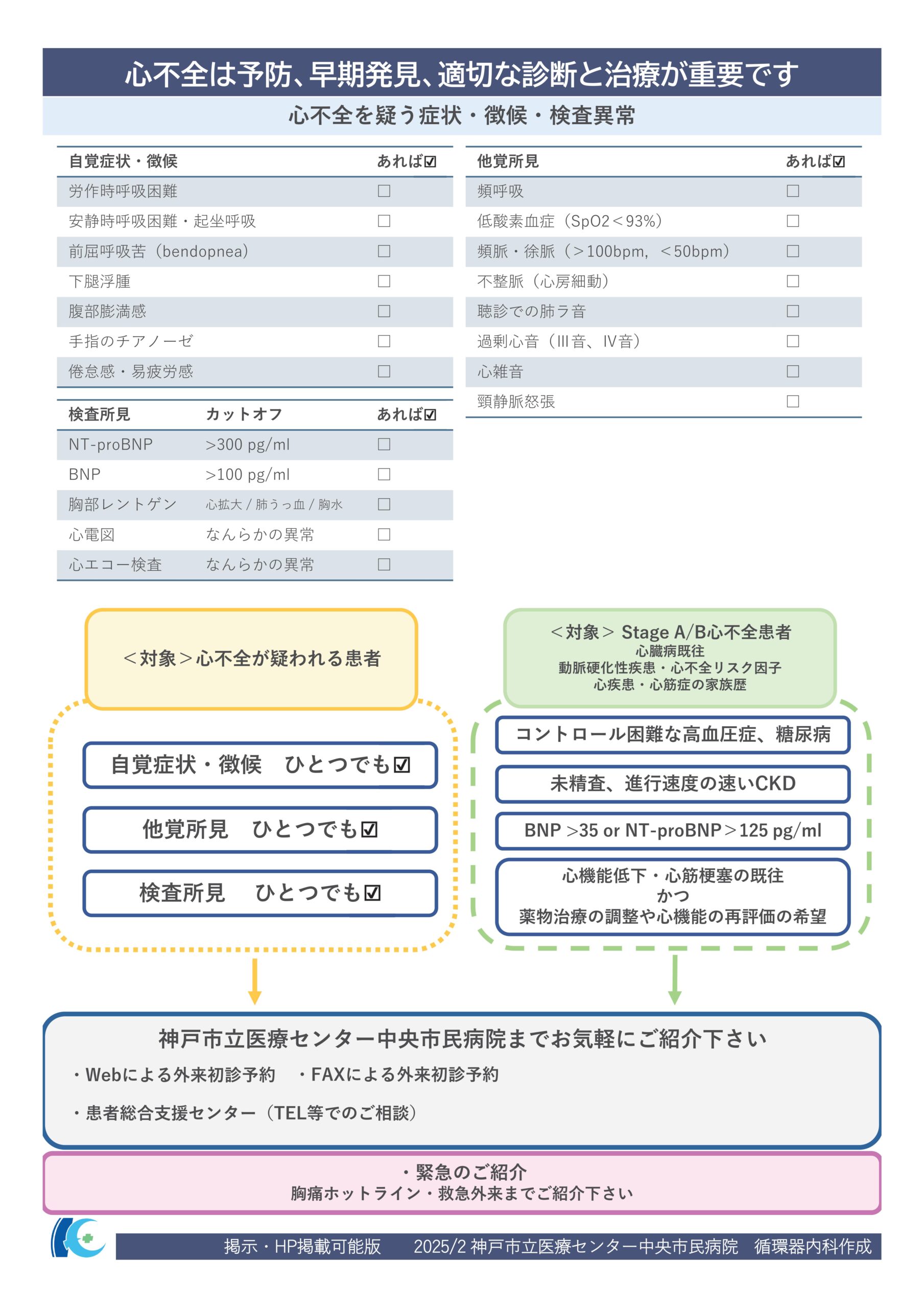
「心不全とは、心臓が悪いために、息切れやむくみが起こり、だんだん悪くなり、生命を縮める病気です。」(日本循環器学会 2025年改訂版心不全診療ガイドラインより)
心不全の症状によって、患者さんの生活の質や健康を損なう可能性があります。当院では、心不全の患者さんの診断を行い、一人ひとりの病状に応じた最適な治療計画を提案いたします。また、多くの職種で構成されるチームで、患者さんに寄り添いながら、最適な治療とケアを提供する包括的診療体制を整えております。
当院の心不全診療の特徴
- 専門的なチーム医療: 循環器専門医、心臓外科医、看護師、薬剤師、栄養士、理学療法士・作業療法士、臨床心理士、医療ソーシャルワーカーなど、複数の専門職が連携し、患者さんの状態に合わせた最適な治療と生活習慣改善や心理的サポート、希望に沿った生活が継続できるよう支援を行います。
- 最新の診断・治療技術: 当院は複数の画像診断機器やカテーテル検査などを用いて、心不全の原因疾患や状態の評価を精密に行うことが可能です。また、一人ひとりの病状に応じた、薬物治療や手術(カテーテル治療や心臓手術)、リハビリテーションなどの非薬物治療を組み合わせた治療計画を行うことが可能です。
予防と早期発見
過去に心臓病と診断された方や現在、生活習慣病で治療中の方は心不全発症の危険性があります。心不全は発症を予防することが重要であり、最新の薬物療法などを含む治療計画の見直しを行い、心不全の発症を予防します。また、心不全の早期発見と適切な治療を行うことで、心不全の進行予防を行います。
私たちの願い
心不全の診療は、単なる病気の治療ではなく、患者さん一人ひとりが希望に沿った生活を送ることを治療の目標にしています。当院のスタッフ一同が全力でサポートいたします。心不全に関するご相談は、どうぞお気軽にお問い合わせください。
医療従事者の方、地域の医療機関の方向け
心不全の予防・診断・治療の最適化を行います
当院では、最新の知見に基づき、心不全の予防や早期の診断、個別化された治療の最適化を積極的に行っています。
下記にあてはまる患者様がおられましたら、お気軽にご相談・ご紹介を頂けますと幸いです。
心臓カテーテル検査
1泊2日検査
当院で現在、主に行っている方法です。
1泊2日検査の流れ
- 検査当日は朝8時過ぎに来院していただき、医師やスタッフから検査の説明をお聞きになった後、午前中に検査を行います。
- 検査は局所麻酔で手首(場合により肘)や太ももの血管から行い、検査終了後は病室にてお過ごしいただきます。
- 太ももから検査をした場合には、4時間ほどベッドで横になって安静にしていただく必要がありますが、手首や腕から検査をされた場合には検査終了後は歩行や食事をとっていただくことが可能です。
- 査後、お昼か夕方に担当医からの結果の説明があります。
日帰り検査
心臓カテーテル検査は従来少なくとも1泊2日の入院を必要としていましたが、過去に手首あるいは腕からのカテーテル検査を受けたことがある患者さん限定で火曜日と金曜日に日帰り検査を実施しております。このシステムは患者さんの仕事や日常生活への支障を最小限にすることができ、入院費用も軽減できます。
日帰り検査の流れ
- 検査当日は朝8時過ぎに来院していただき、医師やスタッフから検査の説明をお聞きになった後、午前中に検査を行います。
- 検査は局所麻酔で手首(場合により肘)の血管から行い、検査終了後は待機室にてお過ごしいただきます。
- 検査終了後は歩行や、食事をとっていただくことが可能です。
- 検査後に担当医からの結果の説明があります。
- 同日16時頃、カテーテルを入れた傷口に問題がないことを確認後帰宅となります。なお、これらの1泊あるいは日帰りの冠動脈造影検査は、腎臓の機能障害がある患者さんなど、検査前後に数日の入院が必要な場合には、適用できないことがありますので、ご留意ください。
- 翌朝9時頃、カテーテルを入れた傷口に問題がないことを確認後退院となります

心エコー図検査

検査機器
- EPIQ7 (フィリップス エレクトロニクス)
- iE33 (フィリップス エレクトロニクス)
- SC2000 (シーメンス ヘルスケア)
- Artida (東芝メディカル)
- Aplio (東芝メディカル)
- Vivid S6 (GEヘルスケアジャパン)
経胸壁心エコー図検査

経食道心エコー図検査
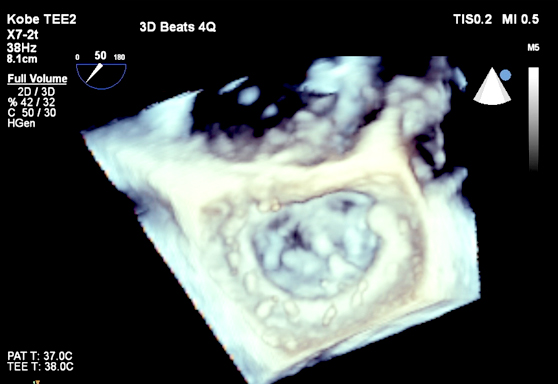
胃カメラと同じような太さの超音波プローブ(探触子)を口から飲んで頂き、食道・胃から心臓を詳しく観察する検査です。経胸壁心エコー図より高精細な画像が得られるため、正確な診断や治療方針の決定に役立ちます。心臓内血栓や弁膜症の術前術後、人工弁、感染性心内膜炎、塞栓症、先天性心疾患(心房中隔欠損症など)の患者さんが適応となります。
当院では検査を安全かつ楽に受けていただくため、鎮静剤を使用して眠っていただいている間に検査を行います。検査時間は約10〜20分と短時間ですが、経験豊富な心エコー医が迅速に検査を行い、3Dエコーも含めて詳細な評価を行っています。安全第一を心がけており、2015年度に検査室・手術室で行われた約700件において重篤な合併症は1例もありません。
術中経食道心エコー図検査
手術室における経食道心エコー図検査は、心臓手術を安全に行うための重要なツールです。当院では僧帽弁形成術や大動脈弁置換術などの弁膜症手術において、修復されたばかりの心臓弁を手術室で心エコー医がチェックしており、より安全で精度の高い手術ができるようにサポートしています。
負荷心エコー図検査

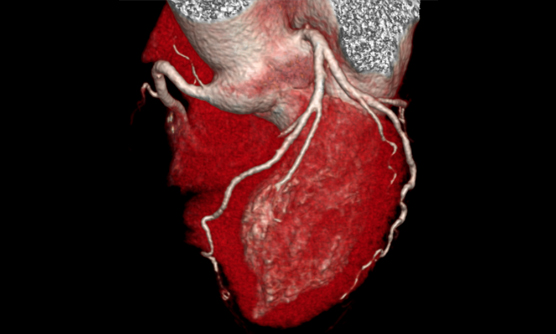
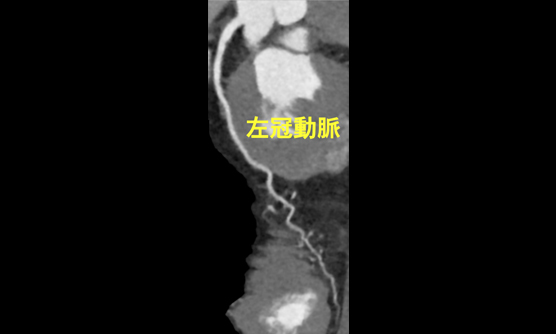
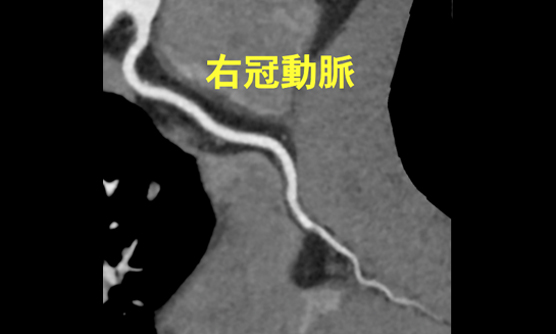
心臓CT検査
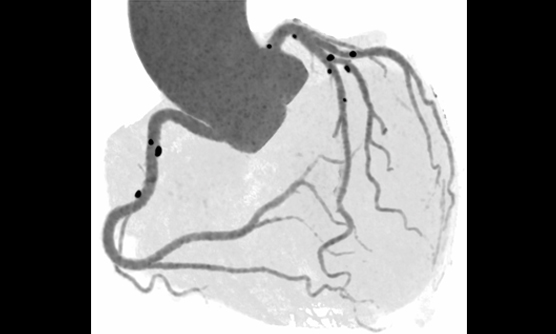
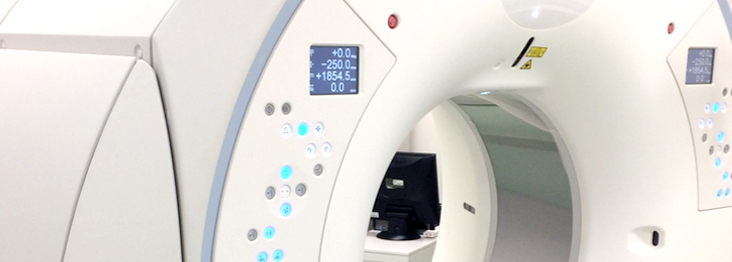
心臓CT検査では、2016年4月から東芝社製の最新型面検出器CT装置Aquilion One Genesis editionが導入されましたので、この装置を使用して検査を行っています。この装置では、320列の検出器が0.5mm間隔で面のように並んでおり、体幹部を16cm幅で1回転0.275秒で撮像出来ます。また従来の装置にくらべて格段に進化したFIRSTという逐次近似再構成法(撮像後の画像処理法)を採用しているため、少ない被曝量で鮮明な画像が得られるようになりました。この二つの特徴により、非常に高画質な画像が、低被爆で得られるようになりました。心臓CTは主には冠動脈病変の評価に使用されますが、弁膜症や先天性心疾患などの心臓の解剖評価にも有用と考えられています。また心臓以外にも大動脈や血管病変の評価にも役立ちます。
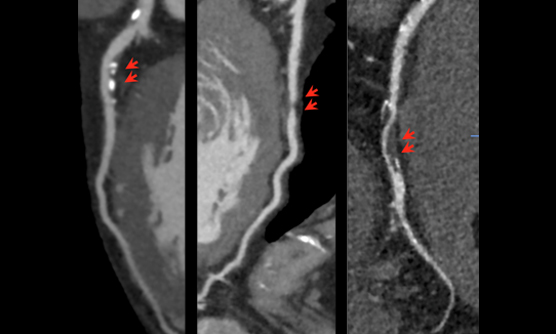
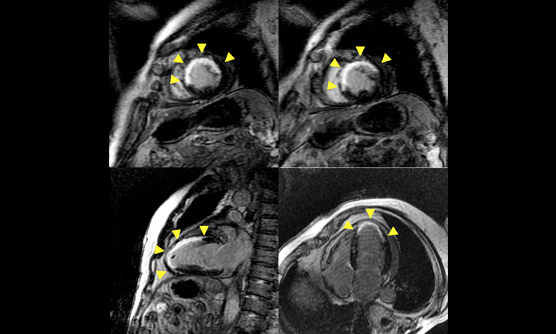
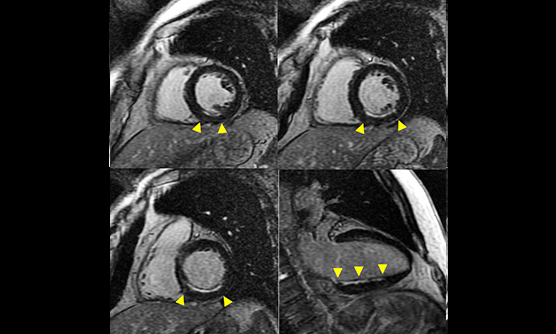
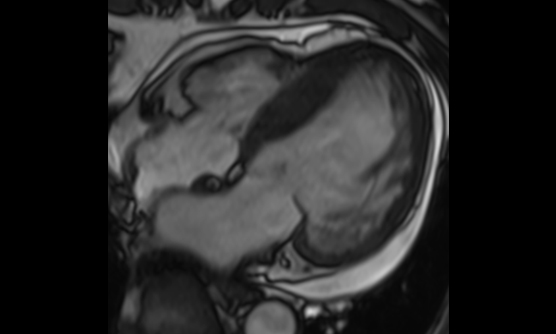
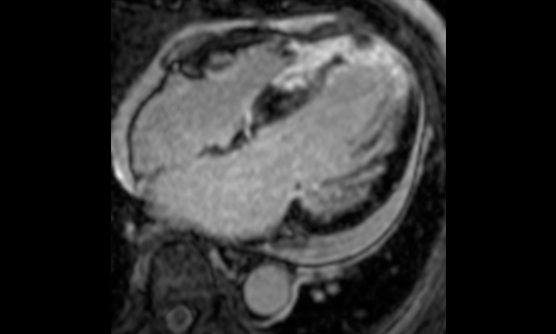
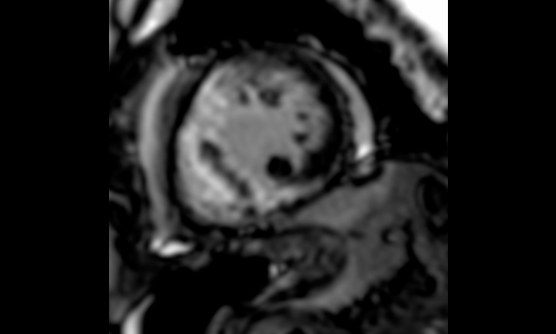
心臓MRI検査
心臓MRI検査では、1.5Tと3.0Tの二つの装置で施行しています。心臓MRIは心機能評価や心臓の筋肉(心筋)の評価に有用です。シネ撮像では、心臓の動きを動画で評価することが出来ます。この撮像法による心機能評価は各種の画像診断検査のなかで、最も正確とされています。また、ガドリニウム造影剤を使用した遅延造影撮像では、心筋梗塞後の梗塞範囲の評価や心筋が変性しておきる心筋症の診断に役立ちます。
(加地修一郎)
MRI装置
遅延造影による心筋梗塞範囲の評価
心筋症における遅延造影
低被曝量(0.61mSv)での冠動脈撮像

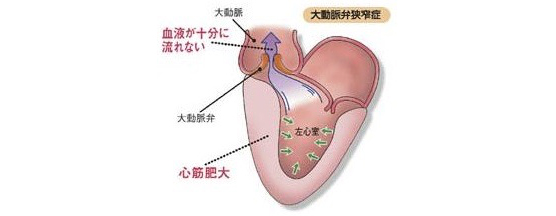
大動脈弁狭窄症とは?
心臓は全身に血液を送るポンプのような働きをしています。左心室が収縮して大動脈に血液を送り出しますが、左心室の出口に大動脈弁という血液の逆流を防止する弁が付着しています。弁の変性や動脈硬化などが原因でこの弁の出口が狭くなる病態を大動脈弁狭窄症といいます。労作時の息切れや失神などの原因となります。重症の大動脈弁狭窄症を放置すると、心臓の筋肉が肥大し、心不全、狭心症発作、失神、不整脈、突然死などが起こりえます。
経カテーテル的大動脈弁植え込み術(TAVI)
これまで大動脈弁狭窄症に対する手術としては、人工心肺使用下に、胸を開けて人工弁を植え込む外科手術が行われてきました。経カテーテル大動脈弁植え込み術 (Transcatheter Aortic Valve Implantation: TAVI)は、症状を伴う重症の大動脈弁狭窄症があるけれども、人工心肺を使用する外科手術のリスクが高い患者さんに対する低侵襲治療です。日本では2013年10月に保険診療可能となりました。厳しい施設基準が定められておりますが、当院は2013年12月に兵庫県初の認定施設承認を取得して以来、2016年10月末までに72例の埋め込みを施行しました。
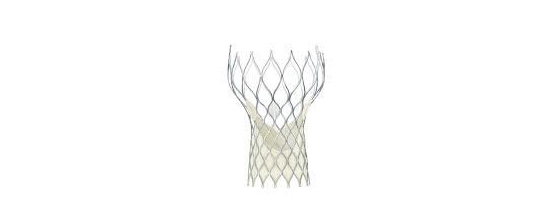
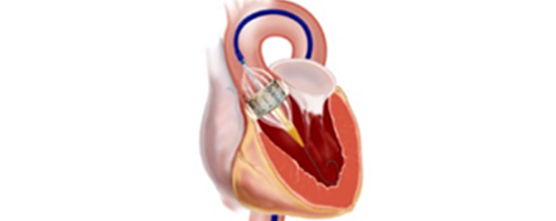
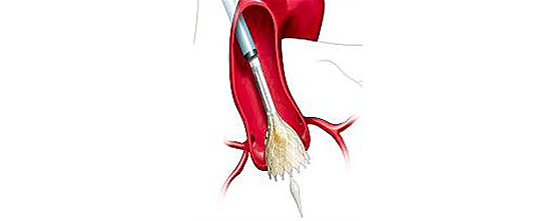
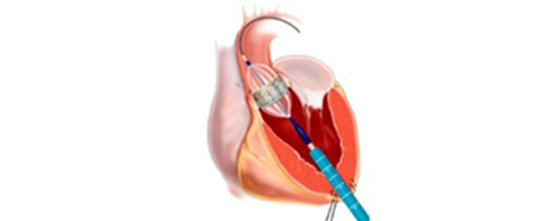
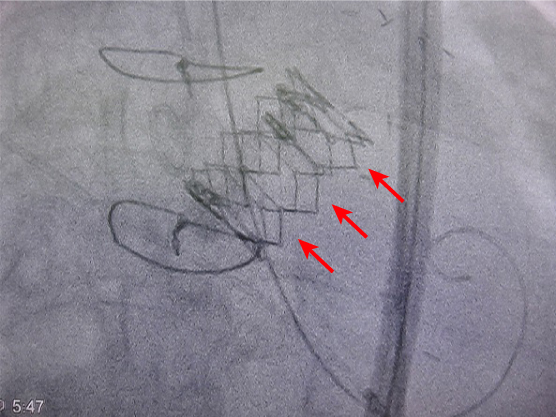
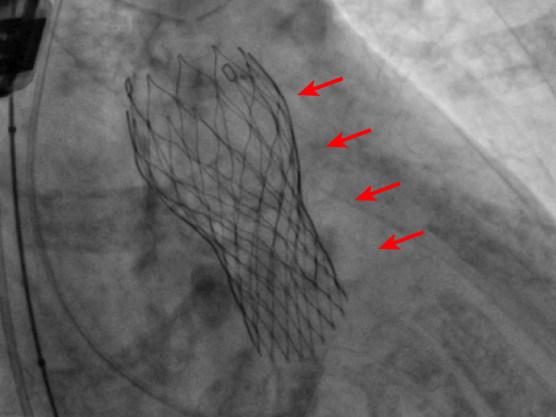
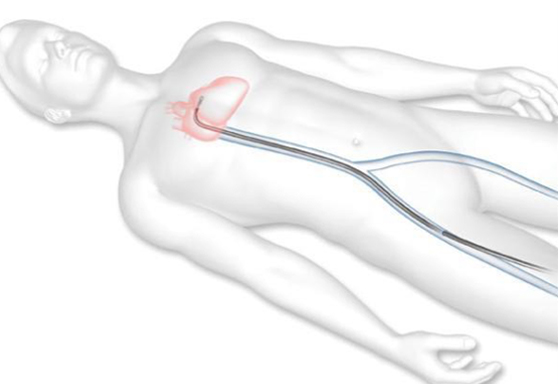
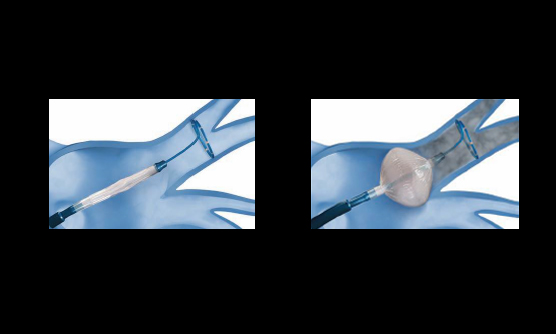
全身麻酔後に、カテーテルとよばれる細長い管を足の付け根の動脈に挿入します。足の血管の性状がよくないなどの理由で、足からアプローチできない場合は、肋骨の間の胸壁を数センチ切開し、直接心臓にカテーテルを挿入したり、あるいは鎖骨下動脈や上行大動脈からカテーテルを挿入します。カテーテルを経由して、折りたたまれた人工弁を心臓まで持ち込み、大動脈弁の位置に植込みます。2016年10月時点では、エドワーズライフサイエンス社とメドトロニック社の製造する2種類の弁が使用できますが、患者さんの弁の性状に合わせて使い分けています。
植え込む人工弁
足の血管からの治療
胸壁からの治療
人工弁(赤矢印)が植え込まれた直後の様子
ハートチーム
TAVI治療は、循環器内科医、心臓血管外科医、麻酔科医,画像診断専門医、看護師、放射線技師、臨床工学技士など多職種にわたるスタッフが,それぞれの専門分野の知識や技術を持ち寄って、患者さんにとって最適と思われる治療法を選択し、治療を行う事で初めて可能になります。このTAVI治療を担うグループを「ハートチーム」と呼びます。当院では、各分野のエキスパートからなるハートチーム体制を整えています。
TAVIの対象となる患者さんは?
症状を伴う重症の大動脈弁狭窄症があり、
- ご高齢(おおむね80歳以上)の方
- 過去にバイパス手術などの開胸手術をしたことがある方
- 肺気腫などの呼吸器疾患のある方
- 肝硬変などの肝疾患のある方
- 悪性疾患合併のある方(1年以上の予後が期待できること)
- 胸部の放射線治療を受けたことがある方
- 大動脈の動脈硬化が強い方
などの理由で外科手術のリスクが高い患者さんがTAVIの適応となります。ただし、リスクが低く安全に外科手術が行われると判断された方や、透析患者さんはTAVIの対象になりません。
ハイブリッド手術室
TAVI認定施設となるためにはハイブリッド手術室が必要とされています。ハイブリッド手術室とは、手術台と心・脳血管X線撮影装置を組み合わせた治療室のことで、手術室と同等の空気清浄度の環境下でのカテーテルによる血管内治療が可能です。当院では新病院移転時の2011年7月にハイブリッド手術室を導入しました。TAVIだけではなく、両心室ペースメーカー手術、大動脈ステントグラフト手術などでも使用しています。
TAVIを希望される患者さん、医療関係者の方々へ
TAVIの適応となるかどうかは、詳細な術前検査(冠動脈造影、経食道エコー、冠動脈造影、呼吸機能検査など)を行って決定する必要があります。まずは、かかりつけ医からの紹介状持参の上で、当院外来受診をお願いします。
| 相談窓口 | 循環器内科医長・心臓センター長 江原 夏彦 (外来日:火曜) 心臓血管外科主任部長 小山忠明(外来日:月~金曜。但し月、水、木、金曜は9-10時のみ) 病院代表番号: 078-302-4321 地域医療センター: 078-302-4458 FAX: 078-302-4424 FAX予約: 078-302-6031 FAX: 078-302-2251 |
|---|
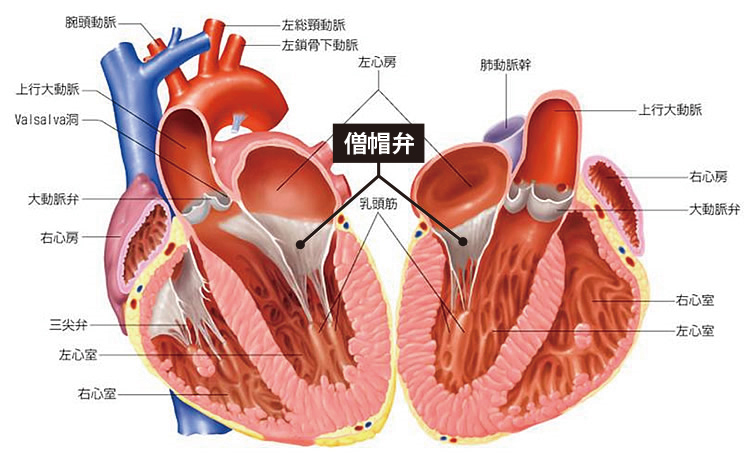
僧帽弁閉鎖不全症(逆流症)と心不全
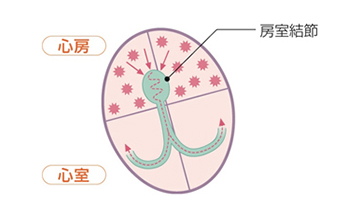
心臓には4つの部屋があります(図1)。上側の二つを左心房、右心房と呼び、下側の二つを左心室、右心室と呼びます。この4つの部屋が拍動を繰り返すことで、心臓は効率的に血液を送り出すことができます。肺で酸素化された血液は左心房に送られ、左心房と左心室の間にある僧帽弁を通って左心室に送られます。左心室は心臓のポンプとして働き、左心室から駆出された血液は大動脈弁を通って大動脈から全身に送られます。左心房と左心室の間には僧帽弁があり、左心室から左心房へ血液が逆流するのを防いでいます。
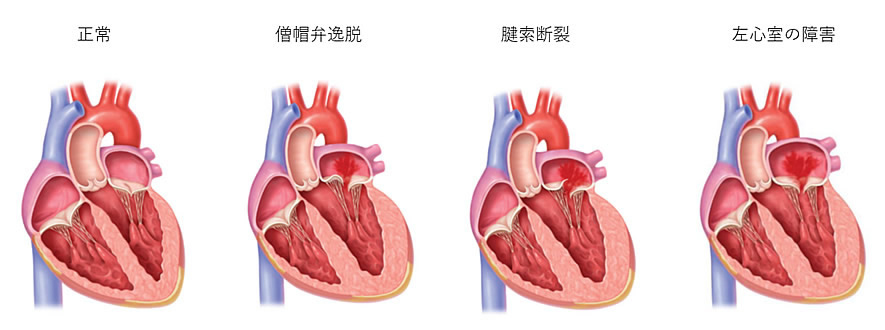
僧帽弁閉鎖不全症(逆流症)は、様々な原因(図2)により僧帽弁が完全に閉じなくなり、左心室が収縮した際に血液が左心室から左心房に逆流してしまう病気です。重症になると息切れやむくみなどの心不全症状が出現し、命に関わることがあります。
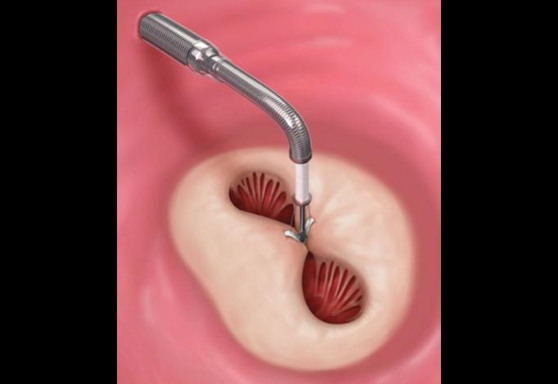
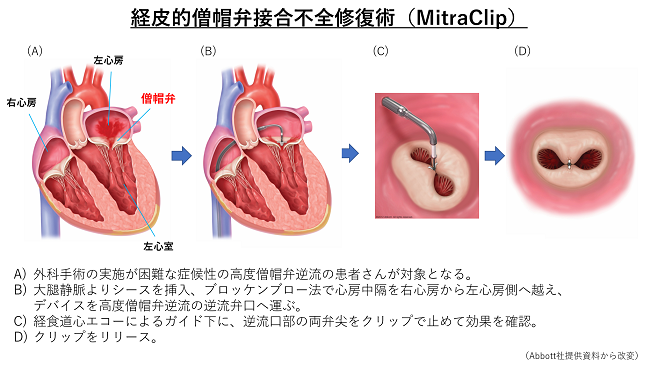
経皮的僧帽弁クリップ術(MitraClip®:マイトラクリップ)とは
重症の僧帽弁閉鎖不全症は動悸、息切れ、倦怠感、入院が必要な心不全の原因となります。これまでは胸を切開し、人工心肺を使用する外科手術(弁置換術・弁形成術)が根本的な治療とされてきました。しかし、心臓の動きが悪い、あるいは他の病気をかかえている、高齢である、などの理由で、手術を断念する、もしくは積極的にお勧めできない患者さんが少なくありませんでした。
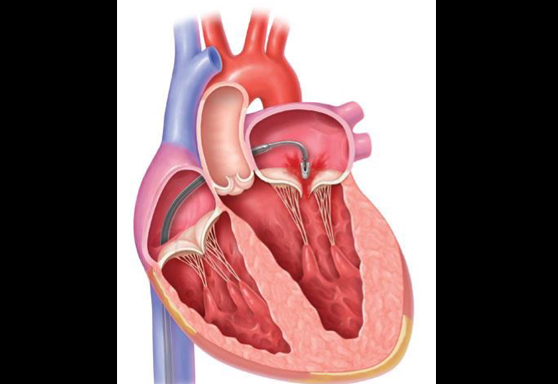
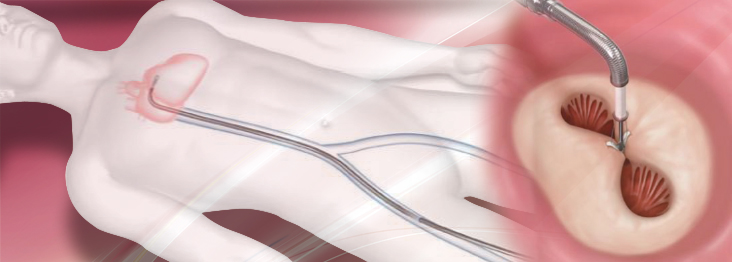
MitraClip®システムを用いた経カテーテル僧帽弁クリップ術は外科手術に比べ安全性が高く、手術の危険が高い患者さんでも治療可能です(図3)。外科手術よりも体への負担が少ないため、手術を受けることが難しかった患者さんに対しても治療が可能となりました。2003年にヨーロッパで始まり、日本でも2018年4月から保険診療開始となりました。
MitraClip®の適応
MitraClip®は外科的弁置換術・形成術の危険性が高い、もしくは不可能と判断された場合に適応になります。具体的には、高齢である、心臓手術の既往がある、心臓の動きが悪い、悪性腫瘍の合併がある、免疫不全の状態である、虚弱である、などが挙げられます。ただし、クリップで僧帽弁を閉じるという性質上、僧帽弁の形態によりMitraClip®の治療が困難な場合もあります。全身状態の評価とともに、心臓超音波画像等で僧帽弁の評価を行い、循環器内科医、心臓血管外科医、麻酔科医などの多職種からなるハートチームで議論し、MitraClip®の適応と治療方針について決定します。
お問い合わせ
MitraClip®に関するご相談、ご質問につきましては、かかりつけの先生と相談の上、当院循環器内科までご連絡ください。
相談窓口
循環器内科 江原夏彦(火曜日)、北井 豪(月曜日)
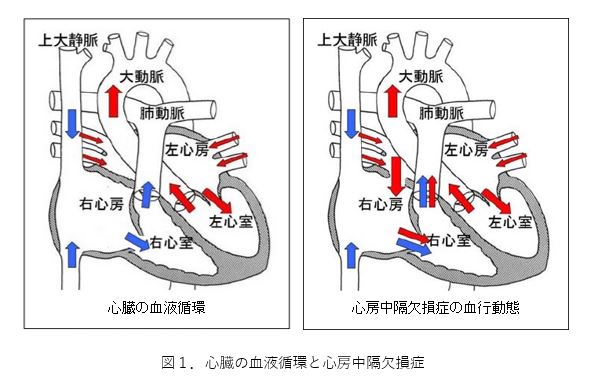
心房中隔欠損症とは
心臓には4つの部屋があります(図1)。上側の二つを左心房、右心房と呼び、下側の二つを左心室、右心室と呼びます。この4つの部屋が拍動を繰り返すことで、心臓は効率的に血液を送り出すことができます。肺で酸素化された血液は左心房に送られ、左心房と左心室の間にある僧帽弁を通って左心室に送られます。左心室は心臓のポンプとして働き、左心室から駆出された血液は大動脈弁を通って大動脈から全身に送られます。
心房中隔とは、右心房と左心房を隔てる壁(隔壁)です。様々な原因により、心房中隔にあな(孔)が開いていると、左心房に帰ってきた血液が、右心房に流れ込み、右心室から肺へと流れる血流が増えてしまいます。そのため、右心房、右心室にかかる負担(右心負荷)が大きくなり、心不全症状をきたすことがあります。また、強いいきみなどにより、体内に圧がかかる状態になると、右心房から左心房に血流が流れ込む場合があります。右心房に血栓などがあった場合に、脳梗塞など塞栓症の原因となることがあります。
右心負荷や塞栓症を認めた場合、心房中隔欠損孔を閉鎖することが症状の進展や予防に有効とされています。幼少期を過ぎてから孔が自然閉鎖することはまれであり、カテーテルや外科手術により孔を閉鎖することが選択肢となります。
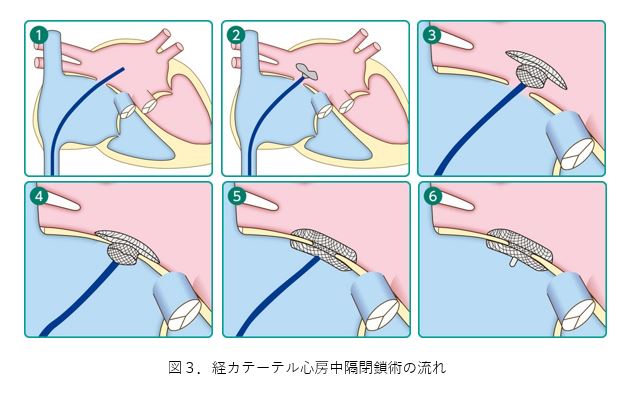
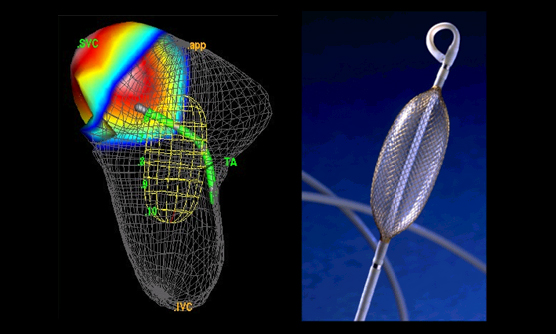
カテーテル治療に用いる閉鎖栓
カテーテル閉鎖栓は2枚の円盤が連なった形をしています。形状記憶合金であるナイチノール製のワイヤーを編んで形作られ、ワイヤーの網目は不織布の布で覆われています。閉鎖栓は柔らかく作られており、伸ばしてカテーテル内に収納することができます。カテーテルから1枚ずつ円盤を出し、心房中隔欠損孔を両側から2枚の円盤で挟み込み、孔を閉鎖します。
経カテーテル心房中隔欠損孔閉鎖術の実際の流れ
全身麻酔または局所麻酔を行い治療の準備を行います。食道や血管内から超音波検査で孔の状態を観察します。次に足のつけねから静脈を穿刺し、シースを挿入します。シースを通してガイドワイヤーを血管内にすすめ、右心房、心房中隔を通過し、左心房、肺静脈までワイヤーを進めます。その状態でワイヤーをガイドにしてデリバリーシース(閉鎖栓を運ぶカテーテル)を左心房に進めます(①)。デリバリーシースの先端より閉鎖栓を展開し(②)、左心房側のディスクと右心房側のディスクで欠損孔をしっかりと閉鎖できていることを確認し(③~⑤)、閉鎖栓をデリバリーシステムから外します(⑥)。この状態で、超音波画像により残存している短絡血流や閉鎖栓の留置状態を評価します。もし留置状況が好ましくなければ、閉鎖栓を回収して再度留置、もしくは治療を断念することがあります。孔の状態に応じて、複数の閉鎖栓を用いて治療する場合があります。閉鎖栓がしっかりと固定され、血液の短絡がきちんと改善されたことを再度確認したら、デリバリーシースを抜去し、太ももの付け根の部分を圧迫又は縫合して止血を行い、手術は終了となります。手術時間は、前後の準備を含めて、おおよそ2~3時間です。
術後は麻酔から覚め、足の付け根の止血に問題がなければ、起き上がって歩くことができます。また治療後に麻酔や経食道超音波検査の影響でのどの痛みが出ることがありますが、数日で軽快することがほとんどです。数日間、閉鎖栓の脱落などがないか経過を診て、退院となります。
カテーテルによる心房中隔欠損孔閉鎖術は、体への負担が少なく安全性が高い治療とされていますが、孔の形態や他の併存疾患により、外科手術の方が良い選択肢となる場合があります。当院では循環器内科・心臓血管外科によるハートチームで相談の上、個々の方に合わせた治療方針を検討しています。 カテーテルを用いた心房中隔欠損孔閉鎖術は日本でも2005年より施行されており、多くの方に治療が行われています。国内では施行できる施設は限られていますが、当院では日本心血管インターベンション学会・日本先天性心疾患インターベンション学会の認定を受け、治療を行っています。
お問い合わせ
心房中隔欠損孔閉鎖術に関するご相談、ご質問につきましては、かかりつけの先生と相談の上、当院循環器内科までご連絡ください。
相談窓口
循環器内科 江原夏彦(火曜日)、豊田俊彬(金曜日)
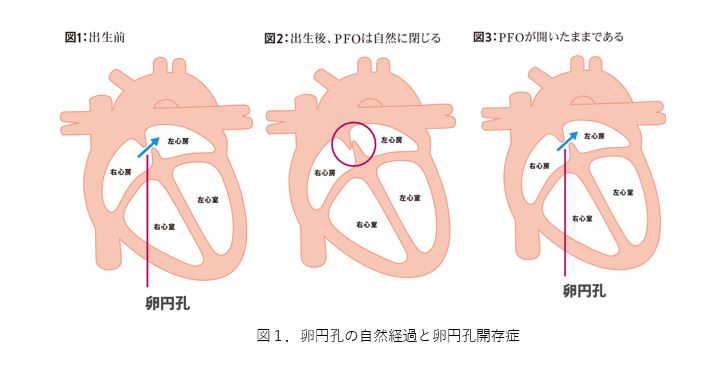
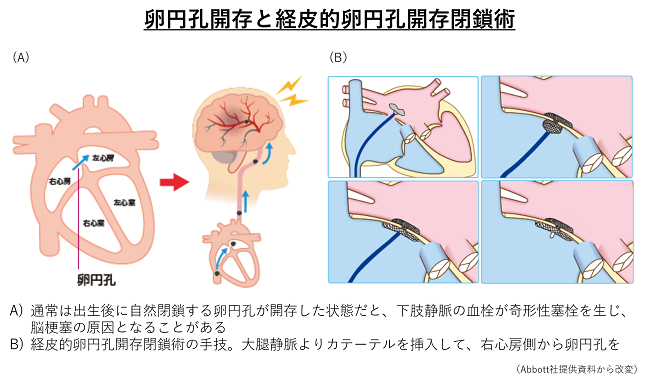
卵円孔開存症とは
心臓には4つの部屋があります(図1)。上側の二つを左心房、右心房と呼び、下側の二つを左心室、右心室と呼びます。この4つの部屋が拍動を繰り返すことで、心臓は効率的に血液を送り出すことができます。肺で酸素化された血液は左心房に送られ、左心房と左心室の間にある僧帽弁を通って左心室に送られます。左心室は心臓のポンプとして働き、左心室から駆出された血液は大動脈弁を通って大動脈から全身に送られます。
卵円孔とは、右心房と左心房を隔てる壁(心房中隔)にある孔で、胎児のときに、胎盤からの血液を胎児の全身に循環させるためにあります(図1)。通常は、出生後数か月以内に自然に閉じますが、成長しても閉じずに残っている場合があります。この状態を卵円孔開存症(Persistent Foramen Ovale: PFO)といい、健康な成人のおよそ4人に1人に存在しているといわれています。この穴を通じた血流を認めることもありますが、通常は症状もなく、治療の必要もないとされています。ただ、運動や咳などで静脈圧が高まると、卵円孔を通じて右心房から左心房に血液が流れ込むことがあります。その際に血栓などが卵円孔を通過し右心房から左心房、動脈系の血管に流れ、脳に達することで脳梗塞になることがあります。卵円孔開存症が脳梗塞の原因と考えられた場合に、孔を閉鎖する治療が選択肢となります。
卵円孔開存症の治療について
卵円孔開存症に対して治療が必要かどうかは、脳梗塞の原因となっているか、また穴の大きさや血液の短絡量(穴を通じて流れる血液の量)、心不全や塞栓症などの合併症の有無によって判断されます。
卵円孔開存症に対するカテーテル治療は、本邦では2019年よりアンプラッツアー卵円孔開存症閉鎖栓(Amplatzer PFO occluder)による治療が施行可能となり、以後認定を受けた施設でのみ治療が行われています。
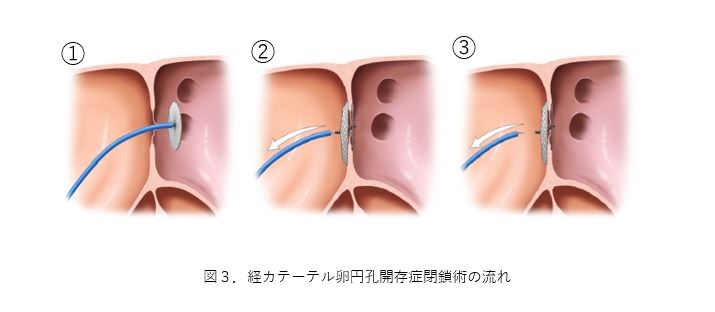
カテーテル治療に用いる閉鎖栓
カテーテル閉鎖栓は2枚の円盤が連なった形をしています。形状記憶合金であるナイチノール製のワイヤーを編んで形作られ、ワイヤーの網目は不織布の布で覆われています。閉鎖栓は柔らかく作られており、伸ばしてカテーテル内に収納することができます。カテーテルから1枚ずつ円盤を出し、卵円孔を両側から2枚の円盤で挟み込み、孔を閉鎖します。
経カテーテル卵円孔開存症閉鎖術の実際の流れ
全身麻酔または局所麻酔を行い治療の準備を行います。食道や血管内から超音波検査で孔の状態を観察します。次に足のつけねから静脈を穿刺し、シースを挿入します。シースを通してガイドワイヤーを血管内にすすめ、右心房、卵円孔を通過し、左心房、肺静脈までワイヤーを進めます。その状態でワイヤーをガイドにしてデリバリーシース(閉鎖栓を運ぶカテーテル)を左心房に進めます。デリバリーシースが卵円孔を通過すると、ケーブルに接続した閉鎖栓を先端から展開し(①)、左房側のディスクと右房側のディスクで孔をしっかりと閉鎖できていることを確認し(②)、閉鎖栓をケーブルから外します(③)。この状態で、超音波画像により残存している短絡血流や閉鎖栓の留置状態を評価します。もし留置状況が好ましくなければ、閉鎖栓を回収して再度留置、もしくは治療を断念することがあります。孔の状態に応じて、複数の閉鎖栓を用いて治療する場合があります。閉鎖栓がしっかりと固定され、血液の短絡がきちんと改善されたことを再度確認したら、デリバリーシースを抜去し、太ももの付け根の部分を圧迫又は縫合して止血を行い、手術は終了となります。手術時間は、前後の準備を含めて、おおよそ1~2時間です。術後は麻酔から覚め、足の付け根の止血に問題がなければ、起き上がって歩くことができます。また治療後に麻酔や経食道超音波検査の影響でのどの痛みが出ることがありますが、数日で軽快することがほとんどです。数日間、閉鎖栓の脱落などがないか経過を診て、退院となります。
カテーテルによる卵円孔開存症閉鎖術は、体への負担が少なく安全性が高い治療とされていますが、その主な目的は卵円孔開存症による脳梗塞の再発予防です。当院では循環器内科・脳神経内科によるブレイン・ハートチームで相談の上、個々の方に合わせた治療方針を検討しています。
カテーテルを用いた卵円孔開存症閉鎖術は日本でも2019年より施行されており、多くの方に治療が行われています。国内では施行できる施設は限られていますが、当院では日本心血管インターベンション学会・日本先天性心疾患インターベンション学会の認定を受け、治療を行っています。
お問い合わせ
卵円孔開存症閉鎖術に関するご相談、ご質問につきましては、かかりつけの先生と相談の上、当院循環器内科までご連絡ください。
相談窓口
循環器内科 江原夏彦(火曜日)、豊田俊彬(金曜日)

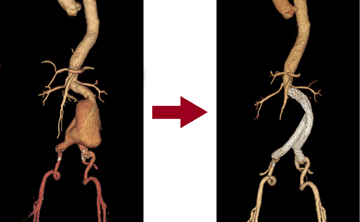
大動脈瘤に対するステントグラフト治療
大動脈瘤とは
血管の一部が拡張し、通常動脈径の1.5倍以上になったものを動脈瘤といいます。腹部大動脈が瘤化したものを腹部大動脈瘤、胸部大動脈が瘤化したものを胸部大動脈瘤といいます。原因は多くは、動脈硬化によるものであり、ほとんどは無症候性です。
大動脈瘤は大きさ(直径)が、腹部で50mm、胸部で60mm以上になると破裂しやすいといわれており、治療の対象となります。これらの大きさに満たない場合でも、瘤の形状が破裂しやすい場合や、瘤の拡大スピードなどにより治療の適応となる場合もあります。
ステントグラフト治療とは
人工血管にステント(金属の網、バネのようなもの)を組み合わせたものをステントグラフトといいます。これを大腿動脈(足の付け根の動脈)から挿入し、患部で広げて、瘤への血流を遮断させることにより、大動脈瘤の破裂を予防するのが、ステントグラフト治療です。
この治療法は、従来から行っている開胸あるいは開腹の人工血管置換術に比べて、体の負担が軽いという利点があります。しかし、血管の解剖学的条件(血管の蛇行の程度や、大動脈からでている枝と大動脈瘤との距離など)によっては、ステントグラフト手術が困難な場合もありますので、患者さんの状態や、血管の状態を総合的に判断して、治療法を選択します。
また、ステントグラフト治療特有の問題として、将来的にリーク(血流の漏れ)が生じる場合があります。したがって、ステントグラフト治療を行った後は、定期的に、CT等で検査をしていく必要があります。
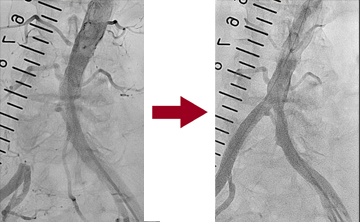
末梢動脈疾患に対するカテーテル治療
近年、高齢化や、食生活の欧米化等により、動脈硬化性疾患は増加傾向にあり、末梢動脈疾患(特に下肢閉塞性動脈硬化症)も、増加傾向にあります。
下肢閉塞性動脈硬化症は、主に下肢の動脈が狭窄または閉塞することにより、下肢に虚血症状が起きる疾患です。症状は、間欠性跛行(歩くと下肢が痛くなる)から、重症になると、安静時下肢疼痛、虚血性潰瘍、壊疽を認めるようになります。
上肢下肢血圧比(ABI)検査をすることにより、下肢虚血のスクリーニングを行うことができます。下肢虚血が疑われる場合は、より正確に狭窄、閉塞部位および血流の状態を調べるために、血管エコー検査、CT検査、皮膚灌流圧検査(SPP)等を行います。最終的に血行再建治療を検討する場合は、血管造影検査(カテーテル検査)を行うことが多いです。
症状を改善する目的、あるいは重症下肢虚血で潰瘍が難治性の場合は血行再建治療(カテーテル治療あるいはバイパス手術)を検討します。どちらの治療が良いかは病変の部位や形態等により異なりますので、患者さんごとに検討する必要があります。
カテーテル治療は、通常、大腿動脈(足の付け根の動脈)から管を入れて、狭窄、閉塞部位を造影剤で確認し、バルーンで広げ、必要に応じてステントを留置します。この治療では、治療が成功しても、6ヶ月〜1年後に再閉塞、再狭窄をきたす可能性もあります。手術の後は、抗血小板剤の内服が必要となります。
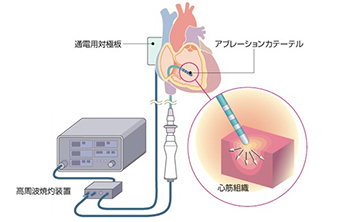
カテーテルアブレーション
カテーテルアブレーションとは、頻脈性不整脈の原因となっている心臓の一部の筋肉を焼き固める(心臓の壁にヤケドを作る)治療法です。日本語の正式名称は経皮的カテーテル心筋焼灼術(K-5951, K-5952)で、1980年代から急速に進歩し広く行われるようになってきています。まず局所麻酔の後、足の付け根(主に右股関節部)や右の首もとや肩口から、電極カテーテル(直径3mm、長さ1mほどの電気コード様の器具)を複数本挿入します。
これらの電極カテーテルを心臓の内側に留置して、不整脈の様子を観察します(心臓電気生理検査)。これにより不整脈の種類と原因が判明すれば、直ちに治療(アブレーション)を行います。異常な電気信号に関わる心筋に対して、カテーテルの先端から高周波電流を1分ほど通電します。電流が流れた心筋は50-60℃の熱を発生し、細胞がつぶれて固まります(たんぱく変性と凝固壊死)。こうして固まった心筋は、異常信号を発生したり異常な電気回路を作ったりできなくなります。つまり不整脈の原因が無くなり、完治します。
入院期間と費用
現在までにほとんど全ての頻脈性不整脈が、カテーテルアブレーションにより根治させることができるようになってきています。当院での一般的なアブレーション治療は2泊3日の入院で行っております。2泊3日のスケジュールで行える不整脈は、発作性上室性頻拍症(WPW症候群、房室結節リエントリー性頻拍症、心房頻拍)、心房粗動、心室性期外収縮、(特発性)心室頻拍です。心房細動と(器質性)心室頻拍は3泊4日から5泊6日の入院スケジュール(下記参照)となります。
不整脈アブレーションは健康保険の適応であり、多くの生命保険・医療保険で手術給付金の対象となっています。入院治療費は、高額医療申請の手続きをしていただくと約10万円の自己負担です。
合併症について
動悸発作の不安や生涯にわたる薬の呪縛から解放され、多くの方に喜んでいただけると期待される治療法ですが、合併症もわずかですがみられます(合計1-3%程度)。主なものは、カテーテル挿入部の再出血や血腫、血管損傷や心タンポナーデ(心臓からの出血により血圧低下すること)、塞栓症(脳梗塞や肺塞栓)、感染症、房室ブロックなどの新たな不整脈出現などが挙げられます。当院ではアブレーション治療をお受けいただく全ての方に、これらの合併症の可能性とともに、予防対策などについても十分にお話させていただき、ご理解いただくように努めています。
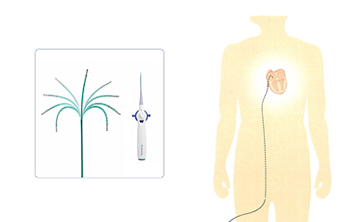
心房細動アブレーション
カテーテルアブレーションは専門の知識と技量が必要ですので、不整脈専門医のいる病院でしか行えません。中でも心房細動に対するアブレーション治療は高度な技術が要求されますが、当院では積極的に治療を行っております。
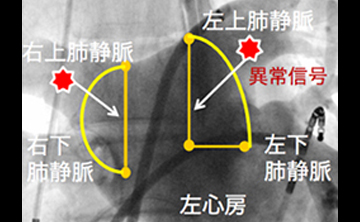
心房細動は、時に不整脈発作が出現する発作性心房細動と、不整脈が1週間以上持続する持続性心房細動、さらには1年以上持続する長期持続性(慢性)心房細動に分けられます。発作性心房細動では、頻脈発作の引き金となる異常信号の多くが、肺静脈(肺できれいになった血液を左心房へ戻す血管)の周囲から発現することが分かってきました。この異常信号を心房へ伝わらせないようにするために、肺静脈と左心房の接合部へ通電し円周状の焼灼線を作成します。これにより異常信号を肺静脈の中に閉じこめるアブレーション法(肺静脈隔離術)が基本的な心房細動アブレーションです。当院では、左右上下で4本ある肺静脈を上下2本ずつ一括で隔離することで、更に有効性を高めた方法(拡大同側肺静脈隔離術)を行っております。発症早期型(発作性)の心房細動の場合は、この方法により80%の患者さんが1回の治療で効果がみられます。更に複数回の治療では93%の患者さんに効果がみられています。
心房細動の病歴が長くなると病状が徐々に進行し、不整脈の状態が持続してしまいます。このような持続性心房細動や慢性心房細動に対しては、上記の拡大同側肺静脈隔離に加え、上大静脈隔離術や、左心房の線状アブレーション、細動基質アブレーションなどのオプションとなる治療法も組み合わせた方法を行っております。これらの方法により持続性心房細動では60%が1回の治療で成功しています。
心房細動でお困りの方の中でも「薬物治療にても動悸発作が治まらない」場合や、「脳梗塞発症リスクを減少させたい」などの希望をお持ちの方には、この心房細動アブレーションが良い治療法と思われます。心房細動アブレーションは3泊4日間~5泊6日間の入院スケジュールで行っています。
アブレーション治療技術の進歩
カテーテルアブレーションは20年程の歴史しかない治療法ですが、急速な早さで進歩してきています。当院では有用な新規治療機器を積極的に導入し、治療成績の向上に役立てています。
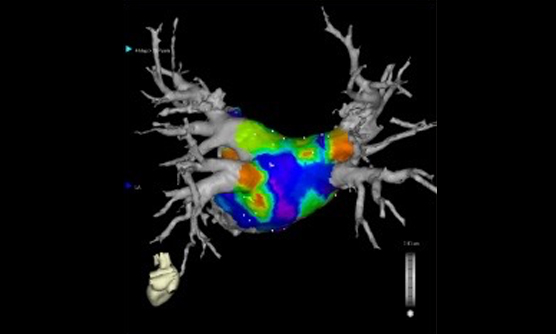
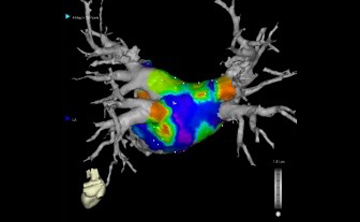
CARTO
磁場情報によるナビゲーション機能をもとに不整脈の原因部分を詳細に立体的に検索し、更にCT画像や心腔内超音波画像と組み合わせた3次元の不整脈マップを作成できる「CARTO」システム
EnSite Array
不整脈の一瞬の変化を捉えることができ、その動きを3次元的に表示可能な「EnSite」システム。
コンタクトフォース・カテーテル
アブレーションカテーテルの先端圧を感知することで、今まで以上に治療効果と安全性が高まった「コンタクトフォース・カテーテル」。
新しい心房細動アブレーション治療方法
さらに新しい心房細動アブレーション治療方法として「冷凍凝固バルーンアブレーション」や日本発の「ホットバルーンアブレーション」も導入しています。
これらの最新器具を適切に使用することで、これまで以上に多くの不整脈でお困りの方の治療に効果を発揮しております。
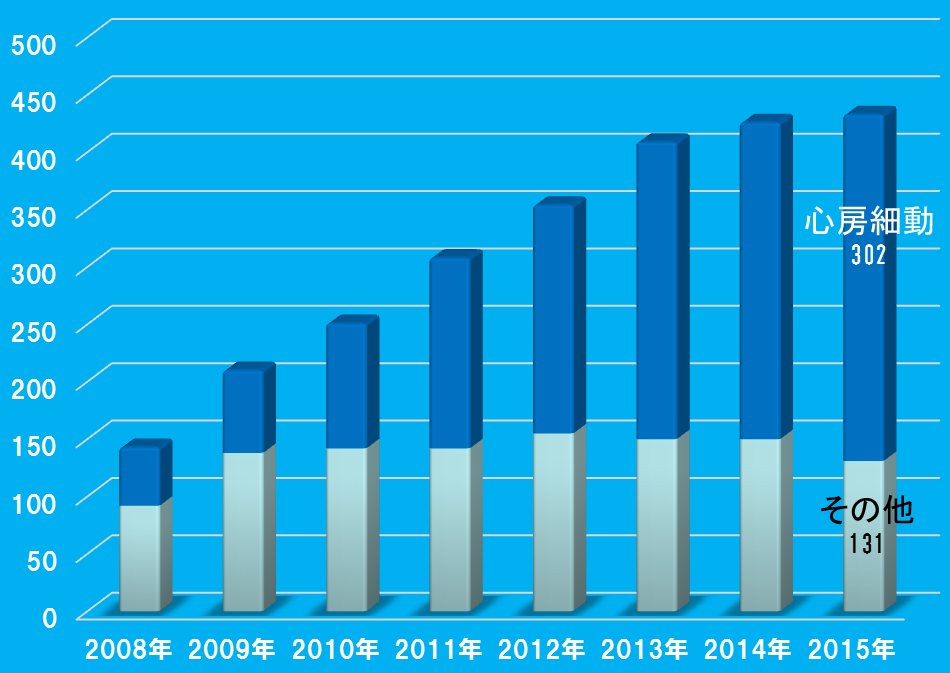
治療実績
年間アブレーション治療実施症例数
治療成績
一般的に発症早期型である発作性心房細動では治療成績が良く、不整脈の持続期間が長くなるにつれ治療効果が低下します。以下のように当院での治療成績(正常脈維持効果)も同様の傾向を示しています。心房細動は早期発見と早期治療が大切です。
| 初回治療後 | 複数回治療後 | |
| 発作性心房細動 (1週間以内に心房細動が停止するもの) |
80.2% | 93.1% |
|---|---|---|
| 持続性心房細動 (1週間以上持続するもの) |
62.3% | 90.7% |
| 慢性心房細動 (1年間以上持続しているもの) |
40.3% | 68.3% |
お問い合わせ
動悸や脈の乱れなどでお困りの患者様やカテーテルアブレーション治療をご希望の患者様は、かかりつけの先生にご相談の上、循環器内科 不整脈外来(水曜日:小堀、金曜日:佐々木)を受診下さい。
また不整脈全般についてのご質問などは、メール(メールマーク)にても対応させていただいております。お気軽にご利用下さい。
不整脈に対するデバイス治療
ペースメーカー治療
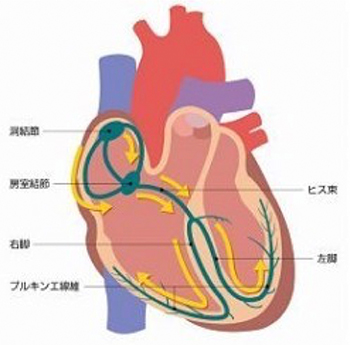
心臓は、筋肉の壁(心筋)によって4つの部屋(左右の心房、左右の心室)に仕切られています。4つの部屋が規則正しく1日に約10万回の収縮と拡張を行うことで、全身へ血液を送り出すポンプの働きをしています。心臓の規則正しい拍動(心臓の動き)は、心筋を流れる「電気信号」の刺激によってコントロールされています。この心臓を動かす「電気信号」は、心臓の中の発電所(洞結節)で作られ、1分間に60-100回程度の規則正しさで発信されています。そして心臓の壁を上(心房)から下(心室)に向かって一方通行で流れ、心筋を規則正しく刺激し収縮させています。
ペースメーカーが必要な心臓の病気は、「徐脈性不整脈」といって、不整脈により脈が異常に遅くなる状態です。代表的なものに、洞不全症候群(拍動の信号を出す洞結節の機能が低下する状態)、房室ブロック(洞結節から出た拍動の信号が途中でブロックされて心室にうまく伝わらない状態)があります。徐脈性不整脈により、脳や全身に十分に血液を送り出せなくなり、一時的に意識を失ったり、意識がもうろうとすることがあります。
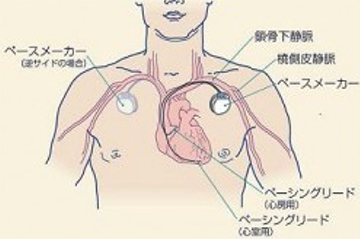
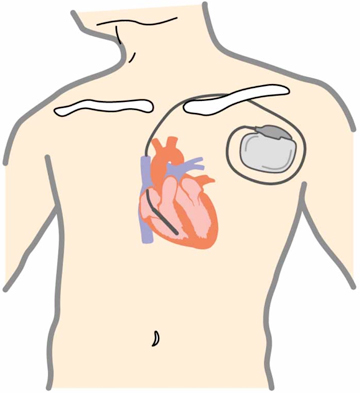
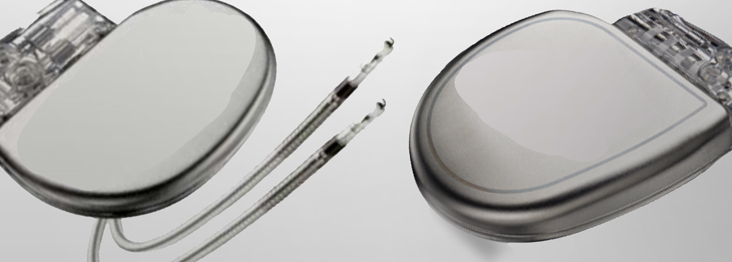
ペースメーカーは患者さん自身の脈拍や電気信号を常に監視し、脈拍が少なくなりすぎないように、心臓に電気刺激を与えます。患者さん自身の脈拍が十分保たれている場合は、電気刺激を与えません。ペースメーカーは電気回路と電池からなる本体と、心臓に電気信号を伝える電線(リード)から構成されます。本体の大きさは、幅約5センチ、暑さは8ミリ程度です。
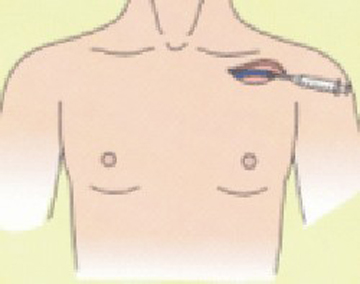
ペースメーカー本体は、鎖骨の少し下の皮膚を数センチ切開して、皮下に植え込みます。電線は1本、もしくは2本、鎖骨の奥にある血管を通して、心臓まで到達させて植え込みます。手術は局所麻酔で行い、1時間〜2時間程度かかります。手術後は、経過が良好であれば約1週間程度の入院が必要です。
退院後はペースメーカー植込み前と同等の生活が送れます。ただし、家庭にあるごく一部の電気製品や、病院での医療機器による検査には注意が必要なものがあります。
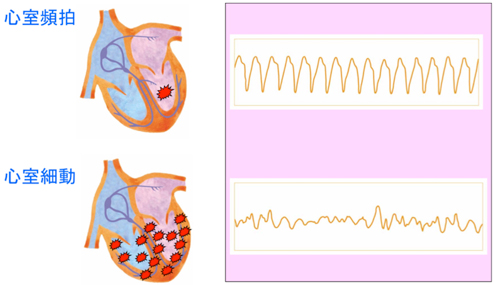
植込み型除細動器、完全皮下植込み型除細動器、着用型除細動器
植込み型除細動器(ICD、アイシーディーともいいます。Implantable Cardioverter Defibrillatorの頭文字をとったものです。)は、命にかかわる重症不整脈(心室細動や心室頻拍)による突然死を予防するための体内植込み型治療装置です。
健康な心臓では、右心房の上の方に洞結節という部位で電気刺激が作られ、その刺激が心房を通過し、房室結節と呼ばれる心臓の中心部を通って心室に伝えられ、心室の筋肉が収縮します。その結果、全身(脳や胃腸、腎臓や筋肉など)へ血液が拍出され、生命が維持されます。ところが心臓に何らかの障害が起こり、突然に、心室の筋肉が勝手に興奮してしまい、異常に速く収縮したり、不規則に震えてしまう状態が起こることがあります。この状態を、心室頻拍や心室細動といいます。心室頻拍や心室細動の状態では、全身に十分な血液を拍出することはできず、失神や突然死の原因となります。
植込み型除細動器が体内に植込まれていると、突然発生したこのような命にかかわる不整脈(心室頻拍や心室細動)を自動的に検出し、即座に電気治療を行って、不整脈を停止させることができます。植込み型除細動器は、電池とマイクロコンピューターが搭載された金属製の「本体」と、血管を通って心臓の中に留置して心臓からの電気情報を本体に伝える「リード」からできています。一般的には、本体は左右どちらかの胸部(鎖骨のやや下)の皮膚と筋肉の間に植込みます。リード線は、鎖骨下静脈という心臓につながる太い静脈から、右心室という心臓の部屋に1本、必要により、右心房という心臓の部屋にも1本、留置します。不整脈が起こっていない状態では、植込み型除細動器は不整脈の監視だけを行っています。植込み型除細動器はペースメーカーの機能も持っているため、普段から脈がおそい人(徐脈といいます)に対しては、ペーシングを行って、心拍数を補うことも可能です。もし、不整脈が発生した場合、心臓の中に留置されたリード線が電気信号を本体に伝えます。本体が、治療が必要な不整脈であると判断した場合には、治療が行われます。治療は主に2種類あり、「抗頻拍ペーシング」といって、通常のペースメーカーのような刺激を速い頻度で行い不整脈を停止させるものと、「カルディオバージョン」、「除細動」といって、心臓に電気ショックを与えて不整脈を停止させるものがあります。患者さん1人1人の病気にあうように、不整脈の検出の判断や電気治療の方法をあらかじめ本体にプログラミングします。
手術の際には、鎖骨の下3センチくらいのところに局所麻酔剤を注射します。通常は局所麻酔なので手術中も意識は保たれますが、気持ちを楽にしていただくため鎮静剤を使用することもあります。麻酔が効いてから、鎖骨の下3センチくらいのところの皮膚を数センチ切り、皮膚の下に植込み型除細動器が入る小さなポケットをつくります。 鎖骨の下を走る太い静脈(鎖骨下静脈)に、植込み型除細動器の本体と心臓を結ぶ電線(リード)を1〜2本入れ、リードが心臓内の目的とする場所へ適切に入ったかどうかを、X線透視で確認します。リードを植込み型除細動器の本体に接続し、皮膚の下に収納し、切開した部分を縫い合わせます。その後、場合によっては、麻酔薬を静脈から点滴し眠っていただいた後で、実際に心室性不整脈を誘発し、適切に作動する事を確認する場合があります。手術時間は2時間〜3時間程度です。術後は数時間の安静のみで、約1週間で退院、日常生活への復帰が可能です。
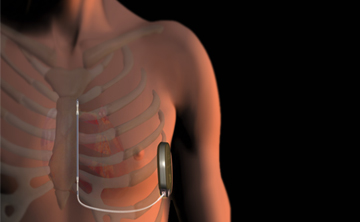
これまでは、血管を通して心臓の中に電線を留置するタイプの植込み型除細動器のみ使用可能でしたが、2016年から、わきの下に植込まれた本体と、皮下に留置された1 本のリードを使って、電気ショックによる治療を行う、完全皮下植込み型除細動器(S-ICD)が使用可能になりました。このシステムは、本体と電線が心臓や血管に触れないため、植込み手術の際の合併症だけでなく、リードや本体に細菌が感染してリード抜去をしなければならない場合の合併症の可能性が少なくなること等が期待されています。植込み手術は、原則的に全身麻酔で行われます。また、患者さんの不整脈の種類、心臓の病状によっては使用できないこともあります。
また、植込み型除細動器を植え込む必要があるかどうか未確定の場合や、患者さんの状態によってすぐに植込み型除細動器の植込み手術が施行できない場合に、期間を限定して、着用型自動除細動器を使用することもあります。
植込み型心電計(植込み型ループレコーダー)
失神の原因は様々な可能性がありますが、その中には、不整脈が原因で発生するものがあります。失神が不整脈によって起こっているかどうかの診断には、失神時の心電図を確認することが最も確実です。このため、ホルター心電図といって、24時間の心電図を記録する検査がよく行われますが、不整脈はいつ発生するかわからないため、ホルター心電図記録中に失神の原因となる不整脈が発生可能性はあまり高くありません。そこで、原因不明の失神の患者さんに対して、原因を明らかにする目的で植込み型心電計を使用することがあります。植込み型心電計は、長期間(最長約3年間)にわたり、心電図を記録することが可能ですので、失神などの症状が起きた時の心電図が記録できる可能性が高くなります。
植込み型心電計は、非常に小さな機械で、左胸の皮下に植え込みます。手術は局所麻酔で30分程度です。傷が治れば、入浴や運動など、いつも通りの生活をすることができます。
ペースメーカー外来
ペースメーカーや植込み型除細動器を植え込んだ患者さんは、定期的にペースメーカー外来に通院していただき、電池消耗やリードの不具合がないか、設定は適切か、治療の必要な不整脈の発生がないか等を点検します。またペースメーカーなどにまつわる日常生活上の疑問点や不安に対してのご質問をお受けし、より快適な生活を送っていただくお手伝いをさせていただいています。
最近では、遠隔モニタリングによる管理も行っています。ペースメーカーや植込み型除細動器を植え込んだ患者さんの自宅に送信機を設置すれば、自動的にペースメーカー外来で行っている点検と同様の情報が電話回線を通じてウェブサイトに反映されます。当院の臨床工学技士、医師がインターネットを通じてその情報を得ることができます。これにより、ペースメーカー外来への通院の頻度を安全に減らすことができ、また、リードや本体の異常、治療が必要な不整脈の早期発見が可能となっています。
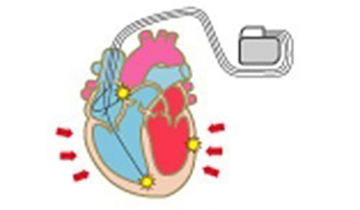
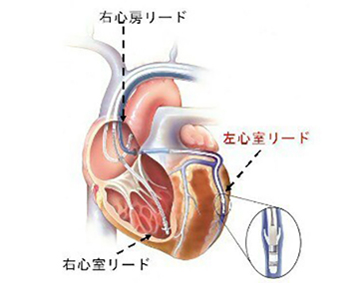
心臓再同期療法とは
心不全の新しい治療「心臓再同期療法」とは、ペースメーカーをつかって心臓のポンプ機能を改善させる方法です。
心臓には4つの部屋があります(右房、右室、左房、左室)。全身から戻ってきた血液は右房、右室を通ってから肺に行き、肺で酸素をもらったのち左房、左室を経て、全身へと流れていきます。心臓は4つの部屋に電気信号が伝わることによって動いています。健康な心臓では、この電気信号は、順序よく伝わっています。ところが心臓に何らかの障害が起こり、心臓の中で電気信号の伝わる順序にずれが起きてしまうことがあります。本来ほぼ同時に全体に伝わるはずの心室の電気信号が早く伝わる部分と遅く伝わる部分ができてしまうといったようなずれかたをした場合、心臓もいびつな動きをすることになります(心室同期障害)。心機能が低下している状態で、心室同期障害があると、さらに心機能が低下し、血液を十分送り出せなくなって心不全の状態を引き起こすことがあります。
このような場合、人工的に電気信号を出して規則正しくリズムを作る器械(ペースメーカー)で、左室の離れた・二カ所に電気を送り、心臓に伝わる電気信号の順序を整え(再同期)、心機能を改善させる治療をすることがあり、心臓再同期療法といいます。心臓の4つの部屋のうち、最も重要な役割を果たしているのが左室ですので、主に左室内でのタイミングのずれを改善させることが主な目的ですが、心房と心室の収縮のずれ、左室と右室の収縮のずれを改善させることもできます。電気信号を休みなく心臓に送りつづけるために、ペースメーカーを胸の皮膚の下に植込む必要があります。
心臓再同期療法が適応となるのは以下の条件に該当する方です。
- 軽い労作でも息切れが出るなど中等度~重度の心不全の方
- 心電図や心エコー検査で、電気信号の伝わりかたに異常があって心室の収縮がうまくいかない「心室同期障害」のある方
- 心機能が非常に低下している方(左室駆出率35%以下【正常値:55%以上】)
- いろいろな薬で治療しているが症状が改善しない方
この治療が受けられるのは、厚生労働省が定めた「両室ペースメーカー移植術の施設基準」を満たした病院で、この手術の認定医が行うのが原則です。当院では2004年から心臓再同期療法を行っています。2008年9月までに31名の方が新規埋め込み手術を受けられました。手術による死亡、心破裂などの重篤な合併症は認めておりませんが、術後にリードがはずれてしまい再手術となった症例が1例ありました。不整脈に対する一般的なペースメーカー治療と違い、心臓再同期療法は重症の心不全の方を対象としているため、手術を受けても症状が改善しない可能性も約30%あると報告されています。当院での成績では、治療が有効であった(左室駆出率の5%以上の改善を認めた)方の割合は65%でした。生命にかかわる危険な不整脈を発症するリスクが高い方の場合は、電気ショックを心臓に与えて危険な不整脈を停止させる除細動機能の付いた両心室ペースメーカーを埋め込む場合もあります。
心臓再同期療法は薬物療法を補うために行われるものであり、これまでと同様に薬は飲んでいただくことになりますので、主治医の先生の指示に従ってください。また、ペースメーカーの定期的な点検を受けていただく必要があります。
心臓再同期療法の手術
手術は、胸の皮膚の下にぺースメーカーを入れるというものです。鎖骨の下3センチくらいのところに局所麻酔剤を注射します。通常は局所麻酔なので手術中も意識は保たれます。除細動機能の付いた両心室ペースメーカーを埋め込む場合は全身麻酔で行う場合もあります。
麻酔が効いてから、皮膚を数センチ切り、皮膚の下にペースメーカーが入る小さなポケットをつくります。 鎖骨の下を走る太い静脈に、ペースメーカー本体と心臓を結ぶ電線(リード)を3本(心房細動の方の場合は2本)入れ、リードが心臓内の目的とする場所へ適切に入ったかどうかを、X線透視で確認します。 リードをペースメーカー本体につなぎ、皮膚の下にしまい、切開した部分を縫い合わせて終了します。手術後に植込んだ部分の皮膚が少し膨らむことがあります。
心臓リハビリテーションの取り組み
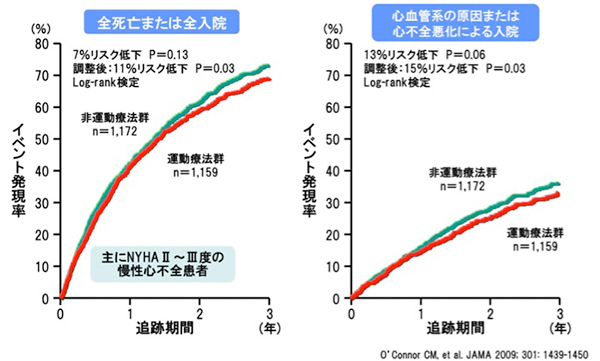
心臓リハビリテーションは、心臓病にかかられた患者さんが退院後の日常生活を安全、快適に送っていただくために行うものです。心臓リハビリテーションは運動療法が中心となりますが、将来の心血管病を予防するための教育やカウンセリングなども含まれます。心臓リハビリテーションは心臓病の患者さんの運動能力、症状、動脈硬化危険因子、心理状態の改善に効果があるとされ、ひいては死亡率の低下が得られるとされています。心臓病に対する治療は、手術やお薬のみでは不十分であり、最大の治療効果を挙げるよう、それを補うのが心臓リハビリテーションということになります。
従来、心臓リハビリテーションは、病気による長期間の安静臥床の結果生じる筋力低下などからの回復を目指す運動療法が主に考えられていましたが、最近では、これらに加えて患者さんや患者さんの御家族に対する病気についての教育・啓蒙、食事指導、禁煙指導、ストレス管理等の生活指導など、多くの要素を含め、包括的心臓リハビリテーションと呼ばれるようになってきました。包括的心臓リハビリテーションを行うには、医師、看護師のみでは不十分であり、当院では理学療法士、栄養士、薬剤士、臨床心理士などの多くの職種が参加してチーム医療を実践し、多方面から患者様のお役に立てるように努力しています。
心臓リハビリテーションの対象疾患
- 急性心筋梗塞
- 心臓手術後
- 狭心症
- 大血管疾患(大動脈解離、大動脈瘤、大血管術後)
- 慢性心不全
- 下肢閉塞性動脈硬化症
心臓リハビリテーションの効果
心臓リハビリテーションは、運動療法と、心臓病やその予防のための講義、多職種によるカウンセリングなどが中心となります。ここでは、心臓病の方が運動療法を行うことで、どのようなよい効果が得られるかについて説明します。
1940年頃は、急性心筋梗塞の患者さんは治療のためしばらくの間絶対安静を強いられていました。しかしその後、絶対安静が長く続けることによる筋力の低下などの問題が指摘されるようになり、1970年代には心筋梗塞後の運動療法が広く行われるようになりました。また、同様に、慢性心不全の患者さんも、1980年頃までは治療として安静や活動の制限が行われていました。しかし、慢性心不全の患者さんの運動耐容能(どのぐらいの強さの運動ができるか)は、心臓の機能とはあまり関係がなく、むしろ筋肉の量や、血管内皮(血管の内側の壁にある細胞で、血管を広げるのに重要な働きをする)の機能が重要であることがわかってきました。このようなことから、慢性心不全の患者さんにも、運動療法が行われるようになってきました。
これから、運動療法が、具体的に体と心にどのような変化をもたらすか、細かくみていきます。
心臓リハビリテーションは、運動療法と、心臓病やその予防のための講義、多職種によるカウンセリングなどが中心となります。ここでは、心臓病の方が運動療法を行うことで、どのようなよい効果が得られるかについて説明します。
1940年頃は、急性心筋梗塞の患者さんは治療のためしばらくの間絶対安静を強いられていました。しかしその後、絶対安静が長く続けることによる筋力の低下などの問題が指摘されるようになり、1970年代には心筋梗塞後の運動療法が広く行われるようになりました。また、同様に、慢性心不全の患者さんも、1980年頃までは治療として安静や活動の制限が行われていました。しかし、慢性心不全の患者さんの運動耐容能(どのぐらいの強さの運動ができるか)は、心臓の機能とはあまり関係がなく、むしろ筋肉の量や、血管内皮(血管の内側の壁にある細胞で、血管を広げるのに重要な働きをする)の機能が重要であることがわかってきました。このようなことから、慢性心不全の患者さんにも、運動療法が行われるようになってきました。
これから、運動療法が、具体的に体と心にどのような変化をもたらすか、細かくみていきます。
(1) 運動耐容能の改善
運動することにより、筋肉量の増加や、筋肉内の毛細血管の増加がおこり、体がたくさんの酸素を取り込めるようになるため、運動耐容能が改善します。運動耐容能がいい人(より強い運動を軽い症状で行える人)ほど、心臓病による死亡が少ないと言われていますので、運動療法を行うことで、心臓病患者さんの寿命がのびることが期待できます。
(2) 心臓の機能の改善
運動療法により、心臓の広がる機能がよくなること、血圧が下がること、などから、心臓から拍出される血液の量が増加すると言われています。また、以前は運動療法を行うと心臓が大きくなって、機能が落ちると考えられていた時期がありましたが、現在ではそのような心配はないことが分かっています。
(3) 血管の機能の改善
血管の壁の内側は、内皮細胞という細胞で覆われています。この細胞は、一酸化窒素(NO)などの血管を広げる物質を産生していて、血管が必要に応じて広がったり収縮したりするのを調節する非常に重要な働きを持っています。運動療法により、この血管内皮細胞の機能がよくなり、心臓や筋肉で運動時に血管が広がりやすくなり、血流が増加することで、症状を改善すると言われています。
(4) 筋肉の量や質の改善
運動療法により、筋肉の量や質が改善します。また筋肉の量や収縮する力が増加することで、静脈から心臓に血液がかえりやすくなりますので、心臓から拍出される血液の量も増えると言われています。
(5) 自律神経のバランスの改善
自律神経は、交感神経(激しい活動をした時に活性化する神経)と、副交感神経(ゆったりと落ち着いている時に活性化する神経)があります。心臓病の患者さんは、常に交感神経が優位となり、副交感神経が減弱している傾向があると言われています。交感神経が不必要に優位になると、安静にしていても心拍数があがったり、不整脈が出やすくなり、動悸を感じることもあります。逆に運動時には、心拍数が適切に上がらなかったり、過剰な呼吸が起こったりすることで、疲れやすくなります。運動療法により、交感神経と副交感神経のバランスを改善させることができますので、これらの症状の改善が期待できます。また交感神経の活性が強いほど心臓病患者さんの寿命が短くなると言われていますので、運動療法により交感神経の活性がおさえられれば、寿命をのばす効果も期待できます。
(6) 精神的な効果
心臓病の患者さんは、動悸や息切れ、疲れやすい、胸痛などの症状のため、日常生活が制限されています。このような状態が続くと、精神的にも、落ち込みやすくなってしまいます。運動をすることで、気分転換になり、また運動療法により症状の改善が期待できますので、さらに精神的によい影響を及ぼすと考えられています。
以上のように運動療法には様々な効果があり、ある研究によれば、運動療法を行うことにより、心臓病による死亡や入院のリスクを低下させることができたと報告されています。
また、心臓リハビリは運動療法だけではありません。さまざまな職種(医師、看護師、理学療法士、薬剤師、栄養士など)が包括的に一人の患者さんの治療に関わるため、生活上の注意点、食事や内服薬に関する注意点など、様々なことを学ぶことができます。
日常生活では下記のような症状がないか注意してください。
心臓リハビリテーションって何をするの?
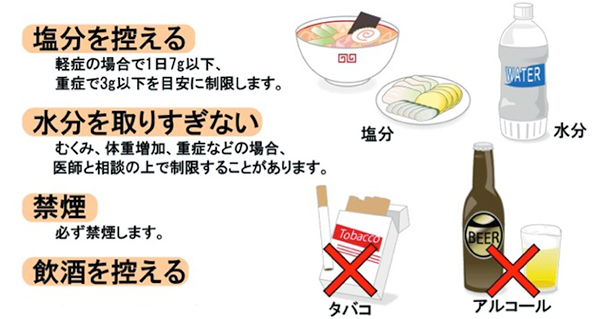
生活指導
心臓リハビリテーションの目的は、病気によって一時的に低下した体力を取り戻し、社会復帰を目指すということだけではありません。患者さんが退院後も健康を保ち、より質の高い生活を継続して行えるようにすることが一番の目的です。そのためには、患者さん自身が正しい知識を習得し、その知識に基づいた健康行動を継続して行う必要があります。
心臓リハビリテーションの目的は、病気によって一時的に低下した体力を取り戻し、社会復帰を目指すということだけではありません。患者さんが退院後も健康を保ち、より質の高い生活を継続して行えるようにすることが一番の目的です。そのためには、患者さん自身が正しい知識を習得し、その知識に基づいた健康行動を継続して行う必要があります。
生活指導の目的
心臓病の多くは生活の不摂生によるものといわれています。また、心臓病は繰り返す病気です。一度回復した病気が再び悪化する要因として、生活の不摂生が挙げられることも少なくありません。生活指導の目的は、入院をきっかけに、患者さん自身が過去の生活習慣を見直し、退院後の新たな生活習慣を具体的に考え、それを長い期間行うことができるようになることです。
心臓リハビリテーションで行うこと
生活指導は主に看護師が担当します。看護師が患者さんと一緒に入院前の生活習慣を振り返ります。そして患者さんと共に退院後の生活を考え、よりその人らしく健康行動が実施できるようにお手伝いをしています。また、退院後も長い期間に渡り健康行動が行えるようにサポートしています。患者さんとは入院中だけでなく、外来心臓リハビリテーションや定期外来受診時にも個別の健康相談の機会を設けさせて頂いています。
心臓病と上手につきあうために
1.自分で体調を観察する
体調管理に最も重要な項目です。体重・血圧・脈拍・自覚症状の有無などを自分で観察できるようになると、体調を管理しやすくなります。また、問題をいち早く発見することができ、早期に医療機関を受診することにもつながります。その結果、健康を逸脱した状態になっても体へのダメージを最低限にとどめることができます。患者さん自身が自分の体調を観察できるようになるために、看護師と共に体重・血圧・脈拍測定の方法、自覚症状観察の方法を確認していきます。
2.減塩・水分管理
心臓病と付き合うために避けられない項目です。過剰な塩分は血圧を上昇させます。また塩分は水分を体内に貯留させる働きがあるため、水分が過剰な状態を引き起こし、心不全を生じる要因になります。心臓病食(減塩食)については管理栄養士が詳しく説明しますが、食生活の工夫は生活指導の中でも時間をかけて実施しています。
3.運動習慣の確立
運動療法は、心臓病に対して非常によい影響を及ぼします。運動習慣を確立できた患者さんは血圧・血糖値・コレステロール値などを安定させ、心臓病の再発を予防するだけでなく、生命予後・健康予後の延長が期待できます。しかし、過剰な運動は心臓にとって負担となり、病状の悪化や、発作の誘因ともなります。適切な運動の強度は個人によって様々ですが、心臓リハビリテーションでは、各個人に合わせた運動強度を選択して運動療法を実施します。さらに、退院後も同等の運動強度で運動療法が実施できるように理学療法士が中心となり、個別で運動療法を指導しています。
4.日常生活における心臓への負担の予防
過剰な心臓への負担とは、運動時のみならず、日常生活においても、その危険性を秘めています。例えば、食事の後すぐにお風呂に入る、家事を連続して行う、内服を済ませずに運動療法を行う、などです。何気ない行動が思わぬところで、心臓にとって過剰な負担となることがあるため、生活指導を通じて、日常生活における心臓への負担の予防について説明しています。
このように、心臓病と上手に付き合うためには、知っておかなければならない項目がたくさんあります。さらに、これらを長期間継続して行うことは非常に労力を必要とし、すべてを実行することは患者さんの負担も大きくなります。そこで、私たちが行う生活指導は、患者さんが健康を維持するために、継続して実施するべき行動を、負担が少ない方法で提案するように心がけています。自らの健康を維持し、より質の高い生活を継続するために、是非心臓リハビリテーションを活用してください。
一般的な運動プログラムについて
快適な日常生活を送るためには、適切な運動の選択と継続が大切です。
Step1 体力をUPしよう
運動の種類
有酸素運動
体内に酸素を十分に取り込みながら行う運動
- 散歩、自転車こぎ、水泳(水中ウォーキング)等
無酸素運動
酸素が足りなくなるような状態で行われる運動
短距離走、懸垂、腕立て伏せ、重量挙げ等
心臓病の方は、軽度から中等度の強さで、心臓に負担をかけずに行う『有酸素運動』を行う事が勧められています。開始から3分間はウオーミングアップとして少しずつペースを上げ、終了時も最後の3分間はクールダウンとして徐々にペースを落とします。これはけがの予防にもなります。
運動の強さ
脈拍数
心臓に負担をかけない脈拍数を目標にします。
自覚症状
自覚的運動強度(ボルグ指数)を用いています。
11(楽である)~13(ややきつい)を目安に運動しましょう。軽く汗ばむもしくは、運動しながら会話が出来る程度の運動です。
運動の時間
無理のない時間から始めて少しずつのばしていきます。一般的に目標は30~40分です。
運動の頻度
できれば毎日が良いですが、週3回~5回でもかまいません。
Step2 筋力を強化しよう
レジスタンストレーニング
負荷をかけて行う筋トレ
効果
筋力・筋肉量・筋持久力の向上、基礎代謝の向上
方法
*息を止めない、反動をつけない
回数
軽い重りで多めの回数
頻度
週2~3回
運動療法の注意点
- 他人と競う、いきむ運動はやめましょう。
- 極端に寒い日や、炎天下での運度は避けましょう。
- 心臓外科手術後の方は極端に「胸を反らせる」「体をねじる」「重いものを持つ」動作は避けましょう。
- 汗をかくことで血液の粘調度が高まり、血管がつまりやすくなります。運動の前後に、水分をとりましょう。
実際、私ってどれぐらい動いても大丈夫なの?
それを知るためには「下肢筋力測定」「心肺運動負荷試験(CPX)」が必要となってきます。
下肢筋力測定
下肢筋力は運動耐容能や日常生活をおくるために重要です。生存率にも関係しているといわれています。下肢筋力を客観的に評価しましょう。
心肺運動負荷試験
CPxは日常生活のどの程度まで動くことができるのか把握でき、生活指導に役立てることができます。
食事療法
食事・栄養について
集団栄養教室
循環器疾患には高血圧、狭心症、心筋梗塞、心不全、動脈硬化症などがありますが、これらの予防・治療のためには、身体にとって望ましい食習慣、生活習慣を身につけることが必要です。教室では主に、食事のリズム、適正体重、塩分量や脂肪の質についてお話します。普段の食生活の中で何に気をつければ良いのかを、一緒に考えましょう。また、毎日の食生活の中での減塩方法のポイントや、その他の調理法についても説明します。
個別栄養相談
集団栄養教室を受講された方を対象に、退院後の生活に繋がるように、それぞれの患者様の生活に合った食事療法について、より具体的に、フードモデルなどを使用して管理栄養士が個別にお話します。
実際に使う資料
薬物療法
集団教室
循環器疾患に使用されるお薬には様々な種類がありますが、一般的によく使用されるお薬についてお話しします。どのような目的でお薬を処方されているのか正しく理解しておくことは大変重要です。お薬は容態に応じて変わることもあります。今服用されているお薬以外にもどのようなお薬があるのか知っておくと、今後の参考にもなりますので、一緒に勉強しましょう。
個別説明
各個人のお薬についてより細かくお話しします。
よくある質問
Q1:1「食後約30分」、2「食直前」、3「食直後」はいつ飲むの?
それぞれ①食事が終わってから30分以内、②食事の10分前、③食事の10分後、に服用して下さい。
Q2:「食後」のお薬は食事を摂らずに飲んでもいいの?
一般的には食事を摂らずに飲んでも問題ないお薬が多いですが、種類によっては副作用予防の観点から食事摂取が好ましい場合や、効果の観点から必ず食事の摂取が必要な場合や、逆に空腹時でなければいけないお薬もありますので、必ず薬剤師に相談して下さい。
Q3:薬が多くて飲み方がよくわからない!錠剤が大きくて飲みにくい!何か良い方法はないの?
1回服用量毎に一袋に包装する「一包化」やお薬を砕いて粉薬にする「粉末化」が出来ます。ただし、一包化や粉末化にすると質が悪くなるお薬もありますので、必ず主治医・薬剤師に相談して下さい。
Q4:症状がなくなったら薬をやめてもいい?
自己判断でお薬を中止すると病状の悪化につながる恐れがありますので、用法用量は必ず主治医の指示を守って下さい。他にも日頃困っている事・疑問に思っている事などを一緒に解決しましょう!!
心理療法
ストレスについての講義
日常生活の中で、いろいろ苦労したり緊張することも心身には影響を与えているようです。その「いろいろ」を現代人は「ストレス」と名付けて、なんとかそれに負けないように取り組んでいます。「ストレス」に対しては、あなどらず、しかしおそれず、という姿勢で対したい。その中身を少しでもお伝えできたら、と考えています。
心理テスト
ひと本来のユニークさはなかなか数字や図には表せません。そういう限界を承知した上で大づかみに自分の性格やこころの状態を知る道具に心理テストがあります。興味のある方はご相談してください。
自立訓練法
気がつくとイライラしている。リラックスしていい時にも緊張がとけない。そんなときに自分を落ち着かせるための手順が自立訓練法です。練習して身につけたい、という方に練習の進め方をご説明します。
心臓リハビリテーションの風景
心臓リハビリテーションに参加した患者さんの声
Q:外来心臓リハビリテーションに参加しようと思ったきっかけはなんですか?
『入院中にリハビリを十分に出来ていないと感じていて、このまま退院するのがすごく不安だった。また退院後の事を考えると運動習慣が少ないと感じていたので参加しようと思った。』(60歳代 男性)
Q:外来心臓リハビリテーションに参加してよかったことはありますか?
『リハビリに来ることで自分の体調を看護師にチェックしてもらえたり、心配なことを聞けるのはすごくよかった。リハビリに来ることを目標に体調を整えようと思うし、自分の体力が回復したなと実感できるので参加してよかったと思う。』(80歳代 女性)
心臓リハビリテーション指導士資格取得者一覧
- 古川 裕(ふるかわ ゆたか) 医師
- 北井 豪(きたい たけし) 医師
- 山根 崇文(やまね たかふみ) 医師
- 金 基泰(きむ きて) 医師
- 村井 亮介(むらい りょうすけ) 医師
- 小椋 由美子(おぐら ゆみこ) 看護師
- 仲村 直子(なかむら なおこ) 看護師
- 鯰谷 雅志(なまずだに まさし) 看護師
- 田頭 美沙(たがしら みさ) 看護師
- 岩田 健太郎(いわた けんたろう) 理学療法士
- 門 浄彦(かど きよひこ) 理学療法士
- 下雅意 崇亨(しもがい たかゆき) 理学療法士
- 田内 都子(たのうち みやこ) 理学療法士
- 佐々木 康介(ささき こうすけ) 理学療法士
- 若田 恭介(わかた きょうすけ) 理学療法士
- 高橋 祐介(たかはし ゆうすけ) 理学療法士
臨床研究
| 研究課題名 | 主任研究者 | 当院責任者 | 承認日 | 研究期間 | 説明文 (PDF) |
| 炎症性心血管疾患に対するマルチモダリティ心血管イメージングに関する国際共同前向き観察研究 | 順天堂大学医学部附属順天堂医院循環器内科 鍵山暢之 | 循環器内科 佐野 円香 |
2026/2/5 | 承認日~2036/3/31 | |
|---|---|---|---|---|---|
| 骨折の有無が心不全患者の予後等に与える影響 | 順天堂大学医学部附属順天堂医院 循環器内科 末永祐哉 | 循環器内科 古川裕 | 2025/12/18 | 承認日~2029/3/31 | |
| 静脈血栓塞栓症患者のマルチオミクスデータを収集する多機関共同遺伝子解析研究 | 京都大学医学部附属病院 循環器内科 助教 山下 侑吾 | 循環器内科 安積 佑太 | 2024/8/14 | 2027/3/31 | |
| 循環器疾患のための画像検査の実態と予後調査 | 神戸市立医療センター中央市民病院 循環器内科 古川 裕 | 同左 | 2024/10/7 | 承認日~2026/7/31 | |
| 植込み型心臓電気デバイス治療に関する登録調査[New JCDTR 2023] | 一般社団法人 日本不整脈心電学会 三橋 武司 | 循環器内科 古川 裕 |
2024/12/10 | 承認日~2028/3/31 | |
| 経カテーテル的心房中隔欠損閉鎖術における心臓の形態的リスク因子の検討 | 京都大学医学部附属病院 循環器内科 助教 塩見 絋樹 | 循環器内科 医長 豊田 俊彬 | 2025/6/5 | 承認日~2027年3月31日 | |
| 本邦における心臓リハビリテーション実施状況のレジストリー(Japanese Cardiac Rehabilitation Registry: J-CARRY研究) | 順天堂大学医学部附属順天堂医院 循環器内科 代表者名:横山 美帆 | 循環器内科 古川 裕 | 2025/5/26 | 承認日~2030年1月31日 | PDF 別紙 |
| 循環器疾患診療実態調査(JROAD)のデータベースと CRT 患者の予後に関わる因子に関する研究(研究 B:JROAD-DPC データベースの二次調査による CRT 患者の予後に関する全国的調査研究(JPN-CRT 研究)) | 国立循環器病研究センター心臓血管内科部門不整脈科 草野研吾 | 循環器内科 医長 江原夏彦 | 2025/3/11 | 承認日~2030年 3 月 31 日 | PDF 別紙 |
| 人工知能を利用した心筋症の心臓MRI画像自動診断システムの開発:AICM‐CMR Study |
関西電力病院 循環器内科 代表者名:加地 修一郎 |
循環器内科 村井 亮介 | 2025/4/23 | 承認日~2027 年 3 月 31 日 | |
| 難治性心房細動に対するパルスフィールド・アブレーション治療付加に関する研究(ADVANCED PFA研究) |
神戸市立医療センター中央市民病院 循環器内科 大岡 順一 |
同左 | 2025/4/1 | 承認日~2033年3月31日 | |
| 冠動脈3枝疾患に対する定量的冠血流比(QFR)に基づく機能的虚血評価の意義: CREDO-Kyoto Registry Cohort-3 QFR Study |
京都大学大学院医学研究科循環器内科 田村 章憲 |
循環器内科 江原 夏彦 |
2025/3/6 | 承認日~2026年9月30日 | |
| 免疫チェックポイント阻害薬関連心筋炎の診断、治療、予後についての多機関共同観察研究 |
明石医療センター 循環器内科 西川 達哉 |
循環器内科 村井 亮介 | 2025/2/21 | 承認日~2027年3月31日 | |
| 陳旧性心筋梗塞に伴う持続性心室頻拍の不整脈基質、アブレーション成績に関する多施設後ろ向き研究 |
東京科学大学病院 循環器内科 |
循環器内科 小堀 敦志 |
2025/1/15 | 承認日~2029年7月31日 | |
| 連合弁膜症の疫学および予後に関する多施設前向き観察研究 |
順天堂大学医学部附属順天堂医院 循環器内科 |
循環器内科 佐野 円香 |
2024/1/14 | 承認日~2030/3/31 | |
| 僧帽弁形成術後の長期予後調査 |
神戸市立医療センター中央市民病院 循環器内科 |
同左 | 2023/11/2 | 承認日~ | PDF 別紙 |
| 左室駆出率の低下した急性心不全入院患者における至適薬物療法についての多施設後向きレジストリー研究 |
順天堂大学医学部附属順天堂医院 末永 祐哉 |
循環器内科 村井 亮介 |
2024/7/23 | 承認日~2027/4/30 | |
| 心臓サルコイドーシスの画像検査と遺伝的要因に関する多施設レジストリ研究 |
順天堂大学医学部附属順天堂医院 循環器内科 |
循環器内科 村井 亮介 |
2024/5/2 | 承認日~2028/3/31 | PDF 別紙 |
| 腫瘍関連肺高血圧症レジストリ研究 |
東京大学医学部附属病院 |
循環器内科 佐野 円香 |
2024/4/12 | 承認日~2029/1/31 | |
| 心エコーデータを用いた循環器病患者の心機能・予後評価に関する検討 |
手稲渓仁会病院・循環器内科 |
循環器内科 佐野 円香 |
2024/3/26 | 承認日~2030/3/31 | |
| レセプトおよびDPCデータを用いた循環器疾患における医療の質に関する研究 |
日本循環器学会 IT/Database 部会長 |
循環器内科 古川 裕 |
2020/10/27 | 承認日~ 2030/3/31 |
|
| 左室駆出率保持型心不全の正確な診断アルゴリズムの確立に向けた多施設共同研究 |
名古屋市立大学大学院 |
神戸市立医療センター中央市民病院 循環器内科 佐野 円香 |
2023/11/20 | 承認日~ | |
| 循環器疾患診療実態調査(JROAD)のデータベースとCRT患者の予後に関わる因子に関する研究 (研究B:JROAD-DPCデータベースの二次調査によるCRT患者の予後に関する全国的調査研究(JPN-CRT研究) |
国立循環器病研究センター心臓血管内科部門不整脈科 草野 研吾 |
循環器内科 江原 夏彦 |
2023/10/19 | 承認日~ | PDF 別紙 |
| 構造的心疾患、大動脈疾患における診療、治療情報データベース |
神戸市立医療センター中央市民病院 循環器内科 |
同左 | 2023/9/13 | 承認日~ | |
| 経皮的僧帽弁接合不全修復システムを用いた僧帽弁閉鎖不全に対する治療介入の有効性と安全性に関する多施設レジストリー研究 |
神戸大学大学院医学研究科循環器内科 |
循環器内科 江原 夏彦 |
2023/7/6 | 承認日~ | |
|
肥大型心筋症患者における診療の実態調査および突然死/拡張相への移行に関する新規予測プログラムの開発とその検証のための多施設後向き登録研究 |
京都大学医学部附属病院 循環器内科 先端医療研究開発機構准教授 |
循環器内科 古川 裕 |
2022/12/22 | 承認日~2026/12/31 | |
|
一般社団法人 National Clinical Database (NCD)における手術・治療情報データベース事業 |
一般社団法人 National Clinical Database (NCD) |
循環器内科 古川 裕 |
2025/1/29 | 承認日~2029/12/31 | |
|
ピロリン酸シンチグラフィ陽性の予測因子の探索
|
兵庫県立淡路医療センター 藤本 恒 |
循環器内科 村井 亮介 |
2022/11/17 | 承認日~2023/3/31 | |
|
循環器疾患診療実態調査(JROAD)のデータベースによる心臓サルコイドーシスの診療実態調査と二次調査に基づく診断・治療プロトコールの策定に関する研究 |
国立循環器病研究センター 代表者名 泉 千里 |
循環器内科 古川 裕 |
2022/11/15 | 承認日~2028/12/31 | |
|
A型偽腔閉塞型急性大動脈解離の治療と予後に関する国際多施設共同観察研究 |
University of Ulsan College of Medicine Asan Medical Center Heart Institute 代表者名:Jae-Kwan Song | 循環器内科 村井 亮介 |
2022/9/1 | 承認日~2023/6/30 | |
| カテーテルアブレーション施行患者を対象としたTMDU 多施設レジストリ研究 | 東京医科歯科大学循環器内科 笹野哲郎 |
循環器内科 小堀 敦志 |
2022/3/23 | 承認日〜2026/8/31/ | |
| 急性大動脈症候群患者における予後規定因子を検討する後方視的観察研究 | 神戸市立医療センター中央市民病院 循環器内科 金 基泰 |
同左 | 2021/2/1 | 承認日〜2023/3/31 | |
| カテーテルアブレーション全国症例登録研究[J-AB 2022] | 一般社団法人 日本不整脈心電学会 研究代表者 山根 禎一 |
循環器内科 小堀敦志・佐々木 康博 |
2021/12/28 | 2022/1/1〜2030/3/31(予定) | |
| 肥大型心筋症患者における診療の実態調査および突然死/拡張相への移行に関する新規予測プログラムの開発とその検証のための多施設後向き登録研究 | 国立循環器病研究センター 泉 知里 |
循環器内科 古川 裕 |
2021/11/29 | 承認日〜2026/12/31 | |
| 心房性機能性僧帽弁逆流の疫学及び治療の意義に関する多施設後方視的観察研究 | 順天堂大学医学部附属順天堂医院 循環器内科 鍵山 暢之 |
循環器内科 佐野 円香 |
2021/11/26 | 承認日〜2027/3/31 | |
| 第1世代レーザーバルーンを用いた手動ドラッキングレーザー照射による肺静脈隔離術の有効性の比較検討 | 神戸市立医療センター中央市民病院 循環器内科 佐々木 康博 |
同左 | 2021/11/22 | 承認日〜2022/10/31 | |
| 経カテーテル大動脈弁植込み術症例における大動脈弁狭窄症の病型ならびにその予後に関する調査 | 筑波大学付属病院病院 循環器内科 家田 真樹 |
循環器内科 佐野 円香 |
2019/10/4 | 承認日〜2024/12/31 | |
| SARS-CoV-2感染症における心臓バイオマーカーを用いた予後予測法の探索(COVID-MI) | 神戸市立医療センター中央市民病院 循環器内科 豊田 俊彬 |
同左 | 2021/10/12 | 承認日〜2027/2/28 | |
| 静脈血栓塞栓症患者の診療実態とその予後を検討する多施設ヒストリカルコホート研究 COMMAND VTE Registry 2 | 京都大学医学部附属病院 循環器内科 山下 侑吾 |
循環器内科 金 基泰 |
2021/9/17 | 承認日~2024/7/31 | |
| NEXT Trial: Extended Follow-up Study | 京都大学大学院医学研究科循環器内科 尾野 亘 |
循環器内科 江原夏彦 |
2021/7/26 | 承認日~2021/12/31 | |
| 経皮的左心耳閉鎖システムを用いた非弁膜症性心房細動患者の塞栓予防の有効性と安全性に関する多施設レジストリー研究-J-LAAO- | 千葉大学大学院医学研究院 循環器内科学 小林 欣夫 |
循環器内科 小堀 敦志 |
2021/5/12 | 承認日~2035/3/31 | |
| エベロリムス溶出性コバルトクロムステント留置後の抗血小板療法をP2Y12阻害薬単剤とすることの安全性を評価する研究(STOPDAPT-3) | 京都大学医学部附属病院 循環器内科 木村 剛 |
循環器内科 木下 愼 |
2021/1/19 | 承認日~2025/1/13 | |
| 補助循環用ポンプカテールに関するレジストリ事業 | 大阪大学医学部附属病院 心臓血管外科 澤 芳樹 |
循環器内科 古川 裕 |
2020/10/27 | 承認日〜2025/12/31 | |
| HeartLight内視鏡アブレーションシステム市販後調査に関する後ろ向き観察研究 | 東京医科歯科大学医学部附属病院循環器内科・不整脈センター 合屋 雅彦 |
循環器内科 小堀 敦志 | 2020/10/5 | 承認日〜2022/6/30 | |
| 実地臨床におけるエベロリムス溶出性ステント(XIENCE V™)とシロリムス溶出性ステント(CYPHER SELECT™+ステント)の有効性および安全性についての多施設前向き無作為化オープンラベル比較試験:長期追跡試験 | 神戸市立医療センター中央市民病院循環器内科 木下 愼 |
循環器内科 木下 愼 | 承認日〜2021/7/31 | ||
| 人工知能を利用した肥大型心筋症の心臓MRI画像自動診断システムの開発(AIHCM2) | 神戸市立医療センター中央市民病院 循環器内科 村井 亮介 |
同左 | 2022/8/25 | 承認日~2026/3/31 | |
| 3種のバルーンカテーテルによる心房細動治療の臨床的特徴の検討 | 神戸市立医療センター中央市民病院循環器内科 小堀 敦志 |
同左 | 2020/5/15 | 承認日〜2021/3/31 | |
| 新規我が国における心臓植込み型デバイス治療の登録調査-New Japan Cardiac Device Treatment Registry(New JCDTR)- | 山口大学医学部付属病院 清水 昭彦 |
循環器内科 金 基泰 | 2020/4/27 | 承認日〜2023/3/31 | |
| 心房細動に対するカテーテルアブレーション周術期に発症する冠攣縮性狭心症の原因と予防に関する研究 | 神戸大学大学院医学研究科内科学講座 循環器内科学分野不整脈先端治療学部門 特命准教授 福沢 公二 |
循環器内科 河野 裕之 | 2019/11/12 | 承認日〜2019/12/31 | |
| 急性大動脈解離発症前造影CT画像の解析 | 杏林大学医学部第二内科 吉野 秀朗 |
循環器内科 加地 修一郎 | 2019/1/26 | 承認日〜2020/3/31 | |
| 心房細動例における薬物療法および非薬物療法による脳卒中、全身性塞栓症、認知症および生命予後についての調査」(兵庫心房細動ネットワーク) | 神戸大学大学院医学研究科内科学講座 循環器内科学分野不整脈先端治療学部門 特命准教授 吉田 明弘 |
循環器内科 小堀 敦志 | 2015/3/25 | 承認日~2021/4/30 | |
| 関西におけるレーザーバルーン心房細動アブレーションの治療効果と安全性の検討 | 循環器内科 小堀 敦志 | 2018/9/11 | 承認日~2021/ 3/31/ | ||
| 日本におけるクライオバルーンアブレーションの安全性の検討 | 福井大学 医学部附属病院 循環器内科 夛田 浩 | 循環器内科 小堀敦志 | 2018/5/14 | 承認日~2020/3/31 | |
| クライオバルーンおよび高周波アブレーションの効果と安全性についての性差特異性メタ解析研究 | スイス・バーゼル大学病院 Professor Michael Kühne | 循環器内科 小堀 敦志 | 2018/11/9 | 承認日~2020/3/31 | |
| SATAKE・HotBalloonカテーテル使用症例に対する全国観察研究 | 筑波大学 医学医療系 循環器内科学 青沼 和隆 | 循環器内科 小堀 敦志 | 2018/3/13 | 承認日~2019/8/31 | |
| 心房細動アブレーション後の飲酒量と心房細動再発率の関連を検討する多施設コホート研究(ALCOHOL-AF study) | 東京医科歯科大学医学部付属病院 循環器内科 平尾 見三 | 循環器内科 小堀 敦志 | 2017/11/28 | 承認日~2020/3/31 | |
| 冠動脈疾患診断およびリスク層別化における冠動脈CTの新規機能的指標の意義の性差と費用効果分析(NADESICO-FFRCT study) | 国立循環器病研究センター 副院長 安田 聡 |
循環器内科 古川 裕・北井 豪 | 2018/1/ | 進行中 | |
| 生体弁置換術後心房細動患者の抗血栓療法に関するレジストリー(後向き観察研究) | 国立循環器病研究センター 心臓血管内科部門 心不全科 泉 知里 |
循環器内科 古川 裕 | 2018/8/25 | 承認日~2019/9 | |
| 天理よろづ相談所病院 循環器内科 三宅 誠 |
|||||
| 心房細動合併患者における冠動脈インターベンション施行後の抗血栓療法の実態調査 | 京都大学大学院以下研究科 循環器内科 木村 剛 |
循環器内科 古川 裕 |
2016/8/16 | 承認日〜2023/9/24 |
お知らせ
医師、医師を目指す方向け当科のご紹介
※本コンテンツは、医師の方を対象とし、当医療機関についての理解を深めていただけるよう作成しているものであり、一般の方を対象とする宣伝・広告等を目的としたものではありません。
こんにちは、神戸市立医療センター中央市民病院 循環器内科部長の古川 裕(ふるかわ ゆたか)です。
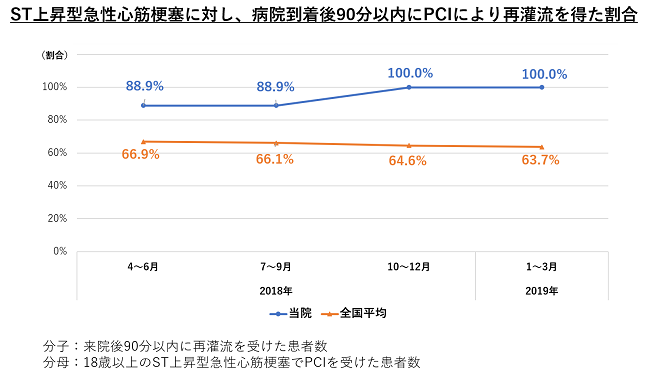
当院は、神戸市とその近郊の患者さんやかかりつけ医の先生方に信頼される高度医療機関・救命救急センターとしての役割を果たすべく、日々診療に取り組んでいます。循環器診療の領域では、次々と新しい治療法が開発・改良されています。当科でも常に先進的な治療を取り入れるとともに、それら治療法の適応を慎重に判断するよう心がけています。また、ST上昇型心筋梗塞、急性大動脈解離など循環器疾患の救急患者では迅速な治療が求められるため、必要な体制と設備を整えて診療を行っています。
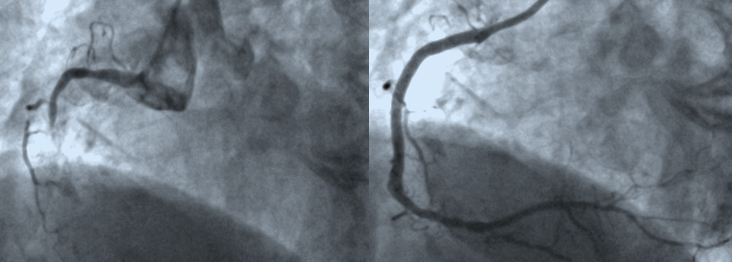
今回は、前者の1例として弁膜症などの構造的心疾患に対するカテーテル治療、後者の1例としてST上昇型心筋梗塞に対する急性期治療における当科の取り組みをご紹介します。ぜひご一読いただき、患者さんのご紹介に際しての参考にしていただければと思います。
古川 裕
循環器内科 部長
構造的心疾患のカテーテル治療
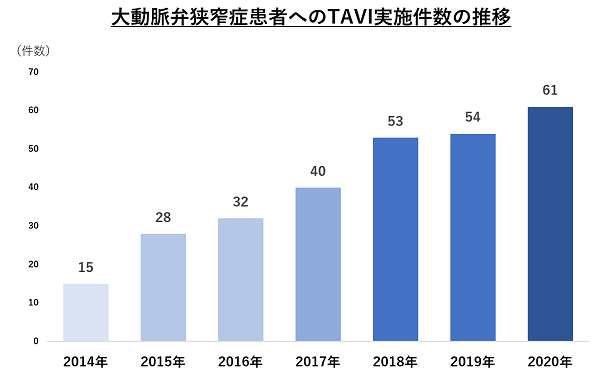
構造的心疾患とは、Structural Heart Disease(SHD)の訳語であり、弁膜症や先天性心疾患など心臓の構造に異常がみられる疾患群のことをいいます。この領域の疾患の多くは、以前は外科手術のみが根本治療の選択肢でしたが、最近、大動脈弁狭窄症に対する経カテーテル大動脈弁置換術(Transcatheter Aortic Valve Implantation; TAVI)を始め、より低侵襲なカテーテル治療が次々と導入されています。TAVIは臨床の場にすっかり定着した感があり、よくご存じの方も多いと思います。
当院では当科、心臓血管外科のほか院内各部署との協働でTAVIハートチームを作り、2014年2月に兵庫県下で最初の実施施設として治療を開始しました。以来、実施件数は年々増加し、2020年12月の記事掲載時までに計283例の大動脈弁狭窄症患者さんにTAVIを行っています 。
新たな臨床試験の結果が明らかになるにつれ、開始当初は外科手術禁忌例や高リスク例に限られていたTAVIの適応は、より低リスク・低年齢層の患者さんへと拡大しつつあります。一方で、外科手術で用いる生体弁に比してのTAVI弁の長期耐久性への懸念や構造的にTAVIに不向きな病変もあるため、治療に際しては当科と心臓血管外科の医師で議論し、それぞれの患者さんにとって外科手術、TAVI、内科的な経過観察のどれが最適なのか慎重に判断しています。これまで30日死亡例は無く、当院での全体的な成績は非常に良好です。 また、2019年3月より、当院で開始した治療として僧帽弁閉鎖不全症に対する経皮的僧帽弁接合不全修復術 (MitraClip)があります。
この治療法は、僧帽弁の逆流弁口部の弁尖をクリップで留めて逆流を制御するというもので、現在のように僧帽弁形成術が洗練される前には、同様のコンセプトに基づいた外科手術の術式もありました(Alfieri法)。また、正常では一つのはずの僧帽弁口が先天的に二つに分離している重複僧帽弁口という先天異常が稀に見られますが、他に併存する異常がなければ、必ずしも僧帽弁機能に狭窄や逆流などの異常を来すとは限りません。このため、治療前の僧帽弁口が十分大きければ、治療後に僧帽弁狭窄を生じることなくMitraClipの実施が可能です。 僧帽弁閉鎖不全症に対する根本的な治療として僧帽弁形成術や置換術が有効ですが、患者の年齢や合併症などにより外科手術の実施が不可能または高リスクである症例に対してMitraClipを用いることで低侵襲な治療を行っています。MitraClipに関しても、その適否の判断にはハートチームによる検討を行っており、患者さんの全体像を踏まえてMitraClipがよいか外科手術を十分実施可能なのか慎重に判断していますので、治療が必要かもしれないと思われる僧帽弁閉鎖不全症の患者さんがおられましたら、両方の選択肢を持つ当院へ是非ご紹介ください。
そのほか、わが国でも以前から行われてきた心房中隔欠損症に対するカテーテル閉鎖術に加え、その延長線上にある経皮的卵円孔開存閉鎖術も最近保険診療下で実施できるようになりました。
当院ではこれらの構造的心疾患の診療に際して、これまでのエビデンスやガイドラインの推奨も十分考慮しつつ、各患者さんに必要な、しかし、過剰ではない最も適した治療の提供を心がけています。治療の適応の判断から実施まで責任を持って行いますので、紹介すべきか悩ましい症例も含めて、遠慮なくご紹介いただければ幸いです。
循環器救急医療
当院は約9年前に現在の場所へ新築移転しましたが、現病院の設計に際して、この医療圏での救急医療と高度医療を担うという当院の役割を機能的に果たせるよう繰り返し検討が重ねられました。循環器救急診療に関しては、搬入された重症救急患者を迅速に治療できるよう1階の救急部門に隣接して緊急カテーテル検査・緊急PCIを行う血管造影室が配置されています。これにより、患者さんの搬入から治療までの時間を短縮させることができました。
このことや従事する医療スタッフ皆の意識の向上により、ST上昇型急性心筋梗塞の患者さんの搬入から冠動脈責任病変の治療までの「Door to Balloon」時間も短縮し、現在では全てのST上昇型急性心筋梗塞で「Door to Balloon」時間90分以内を達成しています。
また、急性心筋梗塞などの循環器疾患による心肺停止症例に対して、体外循環式心肺蘇生法(Extracorporeal Cardiopulmonary Resuscitation: ECPR)を救急部との協働で行っております。ECPRは、経皮的な人工心肺装置(Percutaneous Cardiopulmonary Support:PCPS、または、Veno-Arterial Extracorporeal Membrane Oxygenation:VA-ECMO)を用いた侵襲的心肺蘇生法のことで、大腿静脈から右房まで挿入した脱血管から体外の閉鎖回路に設置した遠心ポンプにより静脈血を脱血し、同じ回路内の膜型人工肺で血液を酸素化、大腿動脈から挿入した送血管から患者さんの体循環へ送血するもので、治療中一時的に心肺機能を代行させて全身の重要臓器の機能を維持しつつ、原疾患の治療を行い、患者さん自身の循環機能の回復を待つというものです。
その実施には、来院時心肺停止症例を最初に診る救急医と、脱血管・送血管の挿入、その後のPCIなどの治療とPCPSの管理を行う循環器内科医とのチームワークが必要になります。治療適応とするには循環機能の回復が見込めるだけで無く、脳機能の回復が見込めることなどが必要となるため、適応となる条件は事前に定めて両診療科で共有しています。もちろん、院内で急変した患者さんも急変時対応のコード次第で同様の治療法の適応となります。
来院時心肺停止症例への当院の対応は、かかりつけ医の先生方には直接目に触れにくいところかもしれませんので、当院の取り組みとしてこの機会に紹介させていただきました。
先生方へのメッセージ
循環器疾患の急性期医療における当科の現状・取り組みを、最近導入した治療と救急診療の2つの面から紹介させていただきました。
今回の記事に登場した弁膜症などの構造的心疾患や冠動脈疾患の他にも、実績を多くの先生方に認知していただいている頻脈性不整脈へのカテーテル・アブレーション治療や各種心筋疾患など、当院では循環器疾患全般を広くカバーする急性期医療を提供しています。
当院はCOVID-19診療の拠点病院でもあり、現在の病院機能について先生方にご心配いただいたり、患者さんの受診控えに繋がったりということもあるのではないかと思います。重症COVID-19診療には多大なる人的な医療資源の投入が必要ですし、当院も“コロナ前”に比べると急性期医療を行う上での様々な困難に直面しているのは事実です。そのような状況において、当院はCOVID-19第一波のときの教訓を生かし、本来の高度医療機関・救命救急センターとしての役割を果たすべくCOVID-19以外の重症患者さんの急性期診療と重症COVID-19患者さんの診療の両立に努めております。本稿が、神戸市と近隣の医療圏での地域医療にご貢献いただいている先生方に当科についてのご理解を深めていただき、先生方の大切な患者さんを少しでも安心してご紹介いただく一助になれば幸いです。