放射線治療センター
当院の放射線治療センターは高精度放射線治療装置3台を有し、様々な悪性腫瘍を対象に、通常の外部照射から強度変調放射線治療(IMRT)・定位放射線治療(いわゆるピンポイント照射)などの高精度治療まで、幅広く行っています。2008年の開設以降、治療件数も増加しており、現在の年間新規治療患者数は約600人です。
年間の診療実績はこちら放射線治療センターのスタッフ
専門職として、放射線治療医6人(うち放射線治療専門医4人)・放射線治療専任技師9人・専従医学物理士1人・看護師3人(がん放射線療法看護認定看護師 1人)が在籍しています。この他に事務スタッフ等を含めたチームで治療にあたります。
放射線治療について
放射線治療は、手術、薬物療法(抗がん剤治療)と並ぶがんの3大治療法の1つです。単独で行われることもありますが、局所に進行した腫瘍では手術や薬物療法など他の治療法と組み合わせた、いわゆる集学的治療法のひとつとして放射線治療が広く行われています。また、放射線治療は根治療法のみならず、骨転移の疼痛緩和など対症療法としても有用です。副作用の程度が他の治療法と比べて軽いことが多く、合併症や体力低下により手術や薬物療法に耐えられない患者さんにも広く適応できる治療法です。
主な疾患とその治療法についてはこちら放射線治療の流れ
- 受診
- 治療計画
- 放射線治療
- 経過観察
01 受診
放射線治療科を初めて受診される際は、当院の他の診療科や他の医療機関からの紹介が必要です。
⇩
予約時間の少し前に当院にお越しの上、受付をお済ませ下さい。放射線治療科を初めて受診される方は、診察の前に問診票の記入をお願いしております。受診が初めてでない場合も、前回の診察から間隔が空いた場合には記入をお願いしております。
⇩
順番が来ましたら診察室に入ります。診察室は1階Gブロックと2階Cブロックの2か所にございます。受付時にお渡しする携帯端末機に診察室番号の表示が出ますのでご確認ください。診察室では放射線治療医が放射線治療について説明いたします。放射線治療の必要性があり、患者さんの同意をいただきましたら、放射線治療の日程を決定いたします。
02 治療計画(CTシミュレーション)
放射線治療の治療計画のためのCT撮影を行います。放射線治療用に決まった方法で撮影しますので、直近に診断用のCTを撮影された方でも治療計画用のCT撮影を改めて行う必要があります。この時、ヨード造影剤を注射したり、固定具の作成をしたりすることがあります。実際の治療の際はCT撮影時と同じ体位で治療を行いますので、位置合わせのために皮膚にインクで印をつけます。
⇩
CTの撮影後に看護師が日常生活の注意点などを説明いたします。
⇩
CT撮影から放射線治療開始まで2日~2週間程度お時間をいただきます。この間、放射線治療医や技師が放射線を照射する範囲や方向、方法などを検討し、検証を行った上で治療計画を最終決定します。
03 放射線治療
放射線治療中は決められた日時に本館1階Gブロックまたは南館1階にお越しください。入院での治療か、通院での治療かは、疾患と患者さんの状態に応じて該当する診療科と相談し決定いたします。入院の際は該当する診療科での入院となります。放射線治療期間中に放射線治療の副作用により通院が難しくなることはほとんどありません。副作用が生じた場合には、外来診察で診療対応いたします。また、放射線治療の回数は疾患や患者さんにより大きく異なります(1回~40回)。治療は基本的に毎日1回行い、多くの場合、1回あたり10分程度です。強度変調放射線治療や定位放射線治療などの特殊な治療を行う場合は20-30分時間程度かかり、腔内照射を行う場合は2-2.5時間程度かかります。また通常の照射でも1回目の放射線治療の際は30分~1時間程度かかります。
⇩
治療期間中、困ったことがありましたらスタッフにお声がけ下さい。必要に応じ放射線治療医や看護師が対応致します。症状に変化がなくても、治療期間中、週1回は必ず放射線治療医の診察を受けていただきます。
04 経過観察
予定された放射線治療が終了しましたら、基本的に紹介いただいた診療科や医療機関での経過観察をお願いしております。放射線治療科で引き続き経過観察をお願いすることもございます。
放射線治療機器
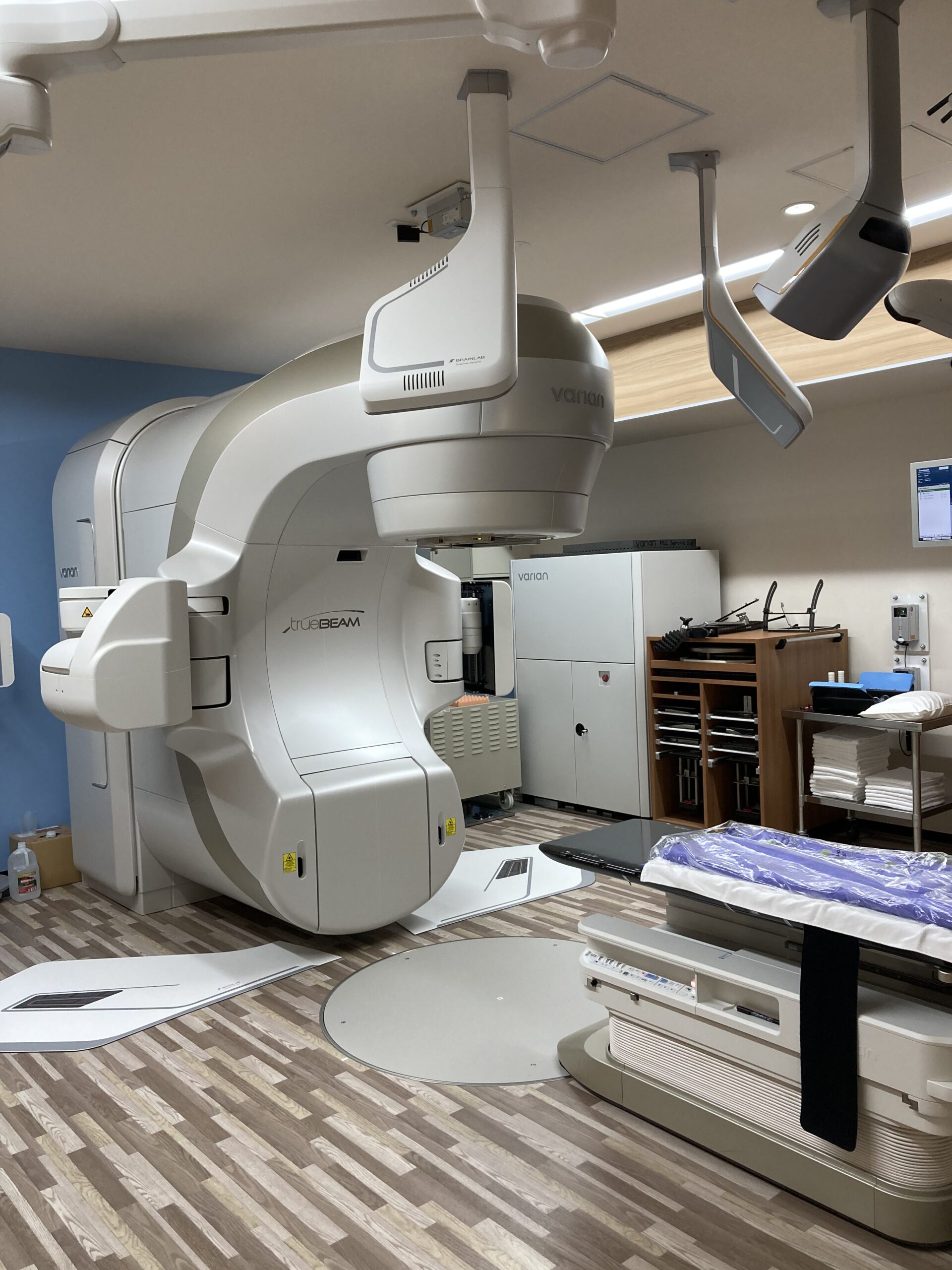
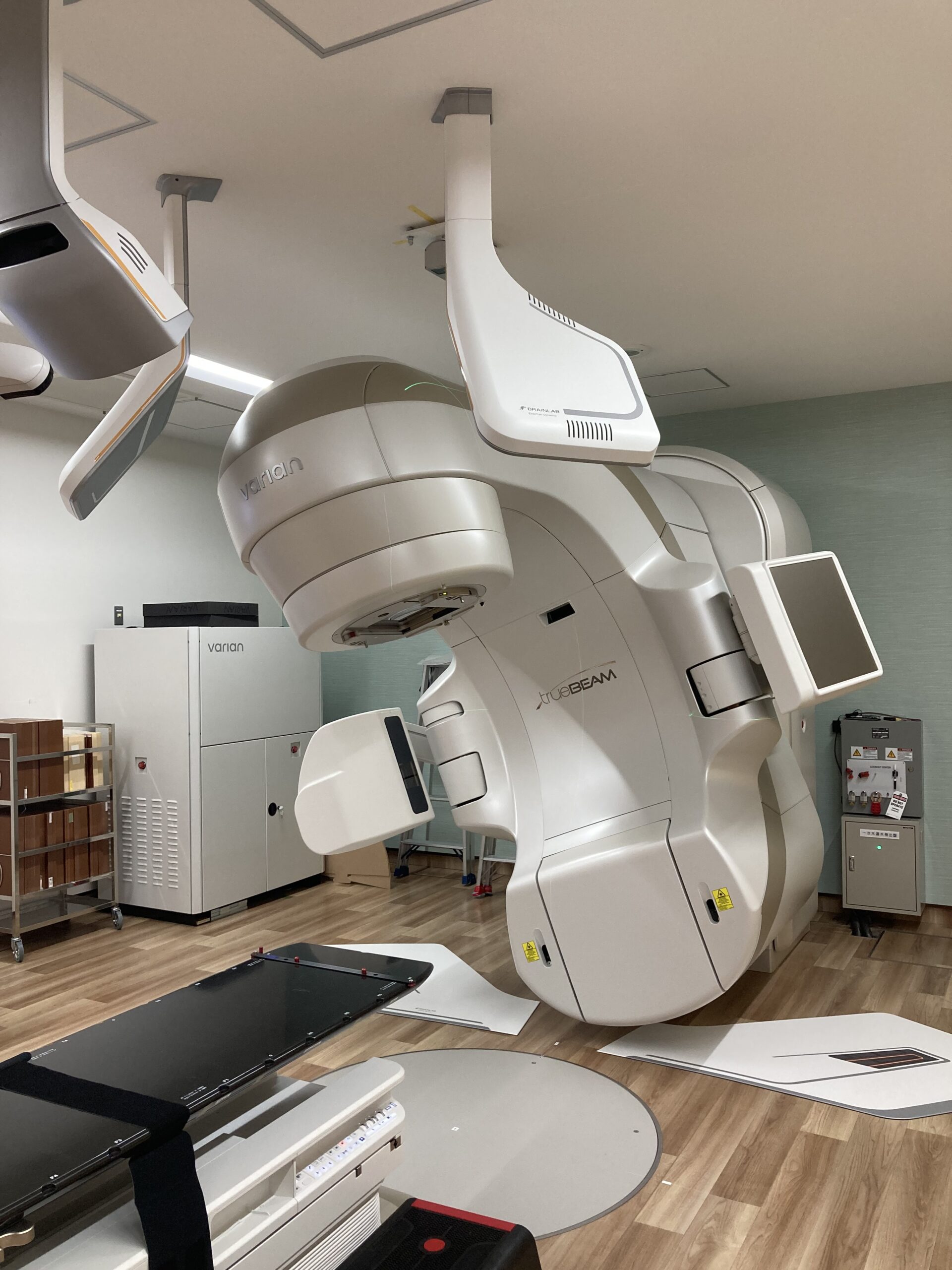
直線加速器
外部照射装置を計3台保有しています。定位放射線治療(SRS/SRT)・強度変調放射線治療(IMRT)・画像誘導放射線治療(IGRT)など、様々な高精度放射線治療に対応しています。
高線量率密封小線源治療装置
組織内、管状器官内にアプリケーターを留置して、内部から照射し、治療を行います。子宮頸癌、膣癌などで使用します。

放射線治療効果の例
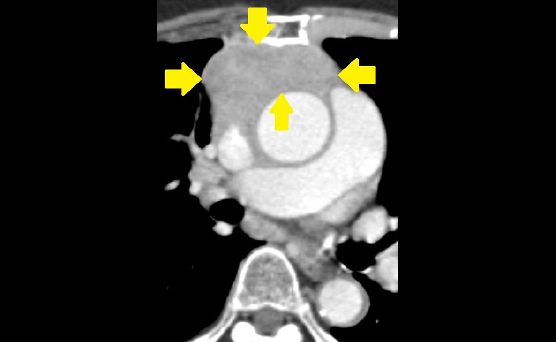
症例1
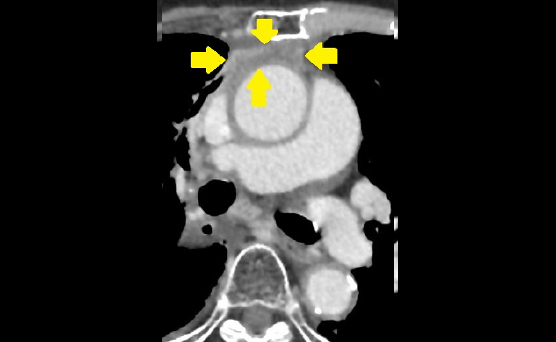
- 80歳代女性
- 胸腺がんに対して放射線治療(IMRT 66Gy/33fr)を施行
- 抗がん剤併用は難しく、放射線治療のみで治療
- 1年後、腫瘍はほぼ消失し、再発なく経過良好
症例2
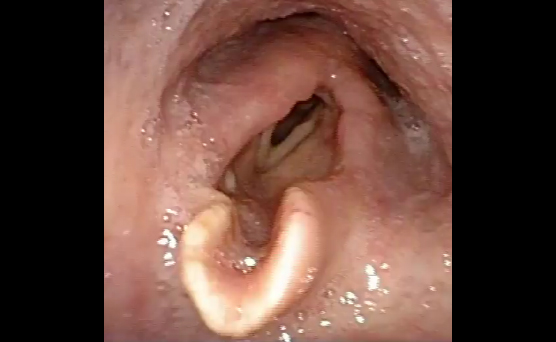
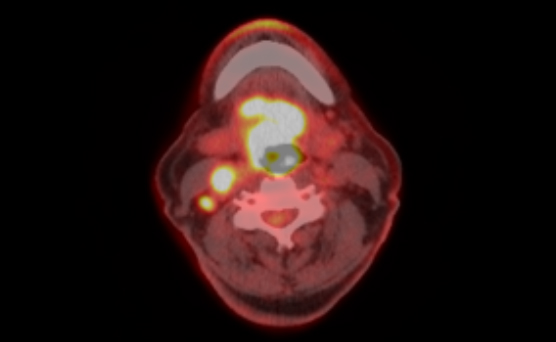
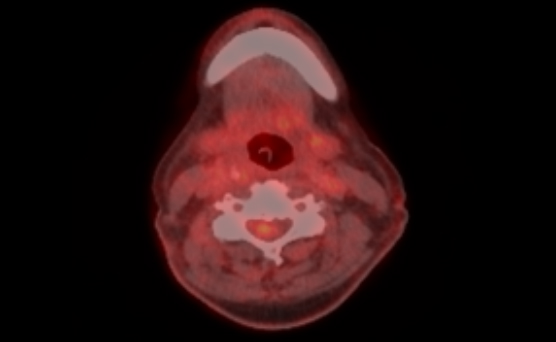
- 70歳代男性
- 局所進行下咽頭癌に対して放射線治療(IMRT 70Gy/35fr)を施行
- 抗がん剤としてシスプラチンを併用
- 治療後腫瘍は消失し、1年半後も再発なく経過良好
放射線治療Q&A
放射線治療の照射回数と照射線量は患者さんの疾患により大まかには決まっており、治療効果・副作用などを考慮し、放射線治療科の初回診察日に担当医と相談して細かい内容を決定します。治療が始まってからの回数や線量の変更は基本的には行いませんが、患者さんの健康状態や個々の事情により変更になることもあります。照射線量や照射回数に質問がある場合には、お気軽に放射線治療スタッフにお尋ねください。
放射線を腫瘍に対して照射していますが、がん細胞のみが照射されているわけではありません。CTなどの画像上に腫瘍は認めなくても、微小な腫瘍の存在が疑われる場合にはその領域に照射することもあります。また放射線の性質上、腫瘍に放射線を照射した場合、どうしても周囲の正常臓器にもいくらかの放射線はあたってしまします。照射方法を工夫することでできるだけ正常臓器には放射線をあてないようにしますが、放射線による副作用が将来的に予想される場合には事前に説明致します。
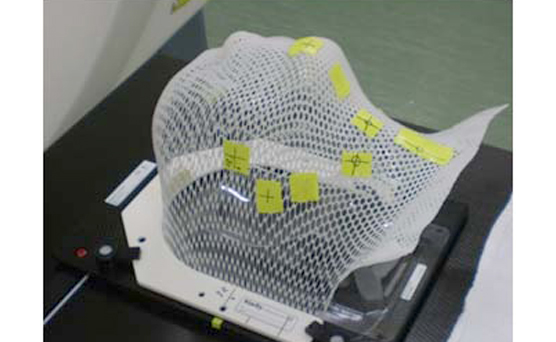
定位放射線治療と呼ばれる治療で、患者さんを治療用のシェルなどでしっかり固定した後、様々な方向から腫瘍に集中させて放射線を照射する方法になります。腫瘍への放射線集中性が向上するため、1回高線量での照射が可能となっており、高い局所制御が得られます。
その一方で照射範囲が腫瘍局所にとどまるため、周りにあるかもしれない眼に見えないような癌細胞の制御は不得手です。定位放射線治療ではなく通常の放射線治療の方が適している疾患も多いです。当院では主に脳転移や肺癌、肝臓癌や脊椎転移に対して定位放射線治療を施行しています。
定位放射線治療には当院の治療装置であるTrueBeamやガンマナイフやサイバーナイフといった装置が使われ、装置ごとに得手不得手があります。腫瘍の大きさや形状によって当院での治療が不向きであると考えられる場合は積極的に他の治療装置を持つ施設へ紹介しております。
当院にはありません。ただ、ガンマナイフもしくはサイバーナイフが適していると考えられる症例は積極的に該当装置を有する施設(神戸低侵襲がん医療センターなど)に紹介しております。
神戸低侵襲がん医療センター ホームページはこちら疾患や腫瘍の存在する部位によって異なります。放射線を外から照射する治療の中には当院で行っているX線を用いるものと粒子線(重粒子線・陽子線)を用いるものがあります。粒子線はX線と放射線の進み方や放射線自体の強さが異なるため、疾患や腫瘍の部位によってはより高い治療効果や、副作用を少なくすることが期待できます。ただ、X線の方が適しているような疾患も多く、必ずしも粒子線が優れているというわけではありません。また、粒子線治療が保険適応となる疾患は限られています。当院では粒子線治療が適していると考えられる症例は積極的に粒子線治療可能な施設に紹介しております。
当院では行っておりません。当院での放射線治療はX線を用いて行っております。ただ、粒子線治療が適していると考えられる症例は積極的に粒子線治療可能な施設(神戸陽子線センターなど)に紹介しております。
神戸陽子線センター ホームページはこちら放射線治療に関するリンク集
がん情報サービス (放射線治療)国立がん研究センターが提供する放射線治療に関するサイトです
日本放射線腫瘍学会(公式サイト)一般の方向けに放射線治療について説明しているサイトです
放射線治療Q&A日本放射線腫瘍学会が提供する患者さんからよくある質問をまとめています
京都大学医学部附属病院 放射線治療科当科と緊密に連携している京大病院放射線治療科のホームページです