リンパ浮腫ケア外来の案内
リンパ浮腫でお悩みの患者さんに対し、医師の指示のもと、リンパ浮腫についての説明・日常生活についての注意点・セルフケアの方法の指導(マッサージ・バンテージ・スキンケア・運動療法)・弾性着衣とバンテージ用品の紹介、選択、採寸、使用法の説明などさせていただきます。患者さんご自身、またはご家族の方が上手くリンパ浮腫とむきあっていけるようセルフケアのお手伝いをさせていただきます。当外来では、マッサージは行なっていません。患者さんがご自身でマッサージができるよう指導を行なっています。
※患者さんの状態により、相談の上、他施設でケアを受けていただく場合があります。
診察の案内
| 診察日 | 火曜日、木曜日 |
|---|---|
| 場所 | A152 |
| 時間 | 9:30~11:30 13:00~17:00 |
| 診療 | 自由診療 完全予約制 初診は約2時間、再診は約1時間 |
| 対象疾患 | 静脈およびリンパ管の障害におけるリンパ浮腫 |
| ケア内容 | フェルディ式複合理学療法を基にしたセルフケア指導を中心に行います |
| 担当 | リンパ浮腫ケアの資格を有する看護師が交替で担当します |
予約の取り方と注意点
当院通院中の患者さんを対象としています。主治医に相談していただき、リンパ浮腫ケア外来の予約を取ります。足のリンパ浮腫の患者さんは、初診前に、エコー検査・血液検査(Dダイマー:静脈血栓症の活動があるかを示す値)を行っていただきます。この検査は保険適応です。
リンパ浮腫と付き合っていくために知っていただきたいこと
各項目をクリックすると詳細が表示されます
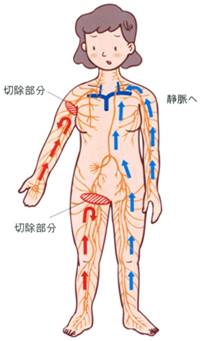
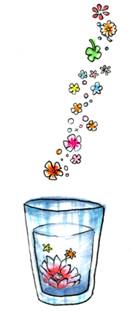
体の細胞で不要になったものやタンパク・脂肪などを運んでいるリンパ液は、リンパ管を使ってからだのすみずみから、首の下にある静脈角という場所に運ばれて静脈に流れ込みます。その後不要なものは腎臓を通り尿として体外に排出されます。口から食べたものが胃から腸に運ばれ排泄されるように、リンパ管にも自動運動能という働きがあり、また逆流防止弁があるため常に首の方に向かってのみ流れています。しかしリンパ管を切断するなど機能が損なわれると、そこから先にリンパ液が運ばれずにたまってしまいます。この状態をリンパ浮腫といいます。
わき道ができることもありますが、わき道がなければたまったリンパ液が、逆流防止弁を壊して逆流してしまいむくみ始めます。リンパ管は全身の皮下組織の中にあるため、皮膚や皮下組織の中にタンパクや脂肪の多いリンパ液がたまりリンパ浮腫を発症します。発症した直後のリンパ浮腫は、皮下組織には水分(リンパ液)が多く柔らかく、安静にしていると改善しやすいむくみです。リンパ液の逆流が皮膚の表面にまで及ぶと皮膚が硬くなり、長期間経過すると脂肪や繊維組織が多くなり改善しづらくなります。リンパ浮腫は一度起こしてしまうと、完治するのは困難ですが、ケアしだいで状態をコントロールすることができます。長期にわたり、リンパ液がうっ滞すると、免疫力が低下し、小さな傷や水虫など、細菌感染や過度な負担を原因として、蜂窩織炎(ほうかしきえんについては後で説明します)を合併しやすくなります。
複合理学療法とは
リンパ浮腫の保存的治療法です。医師による診断のもと、基本の4つの治療方法である、「スキンケア」・「医療徒手リンパドレナージ」・「圧迫療法」・「排液を促す運動療法」から構成されます。また、ご自宅でのセルフケアや自己管理の指導とともに、継続的なサポートをさせていただいております。むくみの程度や皮膚状態に応じて個別の治療構成を立て、患者様が継続して、自己管理できる方法を支援させていただくよう、心がけております。
スキンケア
清潔・保湿を心がけ、感染症を起こさないように皮膚を良い状態に保つことが大切です。リンパ液がうっ滞することにより、免疫力の低下につながり、皮膚の乾燥や傷があるとそこから細菌感染をおこし、炎症や蜂窩織炎をおこしやすくなります。強い日差しでの日焼けを避け、やけど、またはホットカーペットやカイロなどの低温やけどに気をつけましょう。腕のむくみがある方は採血や注射はむくんでいない方の腕で行うようにしてください。治療のためにやむを得ない場合は、医師、看護師に相談しましょう。水虫や巻き爪などの細菌感染や傷、皮膚症状は早めに治療します。また、保湿クリームを塗り皮膚を保護する、ペットに引っ掻かれないようにする、脱毛剤やカミソリで毛ぞリをしないようにする、発赤や熱感のある時は冷却を行う、などの対処が必要です。
医療徒手リンパドレナージ(マッサージ)
皮膚や皮膚組織にたまったリンパ液を柔らかいマッサージによって適切な方向(健康な皮膚やリンパ管、リンパ節など)に流していきます。これによって浮腫が軽減し、リンパ液のうっ滞が原因で硬くなった皮膚の状態を改善させることができます。
圧迫療法
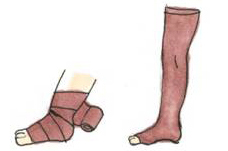
圧迫した状態での運動療法

蜂窩織炎とは、皮膚の下の組織の急性炎症のことを言います。かかり始めは、風邪などの症状に似ています。
おもな症状は
悪寒・・・体全体に寒気、だるさ、震え。
発赤・・・炎症を起こしている皮膚全体が赤くなる、または赤い発疹がみられる。
発熱・・・局所に継続的な熱感を感じる。38度以上の発熱。
このような症状の場合は、すぐに医療機関を受診して、医師の診察を受けましょう。保湿ケア以外のマッサージ・圧迫・運動は一時中止し安静にしましょう。悪寒があるときは毛布であたためましょう。熱感がある場合は冷却をしましょう(広範囲にまんべんなくしっかりと)。炎症を頻繁に起こす場合は日常生活を再度見直すことが必要です。炎症が治まってから、マッサージ・圧迫・運動は再開しましょう。
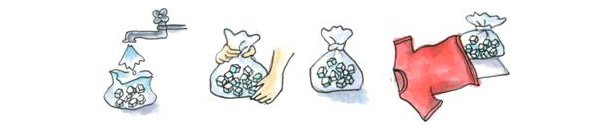
冷却方法(氷のうの作り方)
- ビニール袋に水道水3分の2と家庭用の氷20個くらいをいれ、空気を抜いて口を輪ゴムでしっかりと止める。
- Tシャツなどの柔らかい布で覆い大き目の氷嚢を作る。
- 一カ所に30秒くらい密着させながらゆっくりコロコロ転がしながら大きく全体を冷却する。
- 冷却をやめて2~3分たっても熱感がこみ上げてこなければ終了します。
- この熱っぽさがなくなるまで冷却を続けます。
リンパ漏(ろう)とは
リンパ液が表面に押し出されて小さな水ほうになり、破れてリンパ液がもれ出ることをいいます。きれいなガーゼを皮膚がじくじくしないように頻回に交換しましょう(リンパ液のもれが多い場合は生理用ナプキンなども使用するとよい。)。軽く圧迫包帯を巻いておきましょう。
- 無理をしない
- 負担をかけない
- 皮膚を傷つけない
衣類
- 下着や靴下は皮膚をしめつけない、ゆったりとした綿などの柔らかい素材を選びましょう。
- 足にむくみがある場合は、はきやすく、歩きやすい靴を選びましょう。
食
- 標準体重を維持するようにしましょう。
- アルコールは適量にしておきましょう。
- タバコは控えましょう。
就寝時
- 無理のない程度に、柔らかいクッションなどで、腕や脚を少し高く上げて寝ましょう。
- 弾性ストッキングは夜寝るときには脱ぎましょう。
仕事
スポーツ・娯楽
- 腕や脚を急激に伸ばすような動きを避け、身体に過度の負担をかけないようにしましょう。
- 長時間の温泉浴やサウナ浴は避けましょう。
旅行・移動
長時間の運転や長距離バス・飛行機での移動時は、時々体を動かしましょう。できれば圧迫療法を行いましょう。
弾性着衣の保険適用について
平成20年度診療報酬改定により、医師の指示に基づき購入する弾性着衣(スリーブ・ストッキングなど)が年に2回計4セットまで(1回の購入時2セットまで)を療養費として申請することが認められるようになりました。
*次回申請までには前回領収書発行日より6ヶ月以上の間隔が必要となります。
支給対象となる疾病
リンパ節郭清術を伴う悪性腫瘍(悪性黒色腫、乳腺をはじめとする腋窩部のリンパ節郭清を伴う悪性腫瘍、子宮悪性腫瘍、子宮附属器悪性腫瘍、前立腺悪性腫瘍及び膀胱をはじめとする泌尿器系の骨盤内のリンパ節郭清を伴う悪性腫瘍)の術後に発生する四肢のリンパ浮腫
申請の手順
申請前にすること
- 保険組合窓口に、『療養費支給申請書』を取りに行き、必要事項を記入する。
- 「弾性着衣など 装着指示書」作成してもらう。
- 着圧指示が30mmHg以上のもの
- 医師の特別な指示がある場合は20mmHg 以上の着圧でも可。
- 弾性着衣などの取扱機関にて、弾性着衣の処方や発注、支払い『領収書』を発行してもらう。
申請
保険組合窓口に以下のものを揃えて、提出する。
申請時の必要書類
- 療養費支給申請書
- 弾性着衣など 装着指示書(発行書類によっては作成料が必要)
- 領収書(装着指示書発行日以降の日付のもの)
- 保険証
- 印鑑
- 世帯主の口座番号
1~6を準備して、保険組合に提出すると、2~3カ月の審査の後に通知が手元に届きます。
※複合的理学療法を行うことで、ごく稀に以下の事が起こる可能性があります。以下のことが考えられる場合には、治療を行う前に医師にご相談ください。また、初診時の状態から体調に変化がみられた場合や新たな病気がみつかった場合、必ずセラピストにお申し出ください。
禁忌事項
- 感染症による急性炎症を生じている場合[炎症症状を悪化させるおそれがある]
- 心臓などの機能障害のある方[心臓に負担がかかり、胸水・腹水・心のう液貯留等を引き起こすおそれがある]
- 静脈疾患(血栓性静脈炎・静脈血栓症等)の可能性のある方[血栓がはがれて肺の血管等に塞栓症を引き起こすおそれがある]
- 閉塞性動脈硬化症の可能性のある方[圧迫の禁忌:循環障害の増悪を引き起こすおそれがある]
注意事項
- 頚動脈洞症候群の方[頚動脈に圧を加えることで、血圧に変動をきたすおそれがある]
- 不整脈のある方[頚動脈に圧を加えることで、心臓に負担をかけるおそれがある]
- 甲状腺機能亢進症の方[頚部の施術により甲状腺ホルモン分泌の急な増加を招き、症状を増悪させるおそれがある]
- 動脈硬化のある方[血管の硬化がある場合、血管障害を引き起こすおそれがある]
- 腎機能障害のある方[体液バランスの変調により、胸水・腹水等を引き起こすおそれがある]
- 腹部の急性・慢性疾患(腸カタル・潰瘍性大腸炎・クローン病等)の方[腹部に強い圧を加えることで炎症や出血、腹膜炎を誘発するおそれがある]
- 腹腔内の手術や照射療法を受け癒着の強い方[腹部に強い圧を加えることで、腸壁や膀胱壁を損傷する危険性があり腹膜炎に繋がるおそれがある]
- 大動脈瘤のある方[腹部に強い圧が加わることで大動脈瘤に支障をきたすおそれがある]
- 腸閉塞の既往がある方[腹部に強い圧を加えることで、腹膜炎を誘発するおそれがある]
- てんかんの既往がある方[腹部に強い圧を加える等で、てんかん発作を引き起こすおそれがある]
- 患肢に感覚障害のある方[血行障害や痛み等の症状を自覚できないおそれがある]
- 繊維に対して過敏症を起こす可能性のある方[接触性皮膚炎や湿疹を起こすおそれがある]
- 悪性腫瘍がリンパ管に浸潤し浮腫が発生した場合や転移や再発、病状の悪化等がみられた場合[まずは原疾患に関して主治医とよく相談し、全身状態を考慮のうえ場合によっては施術を休止する等、リンパ浮腫治療の継続と施術内容を再検討する必要がある]
- その他、肝臓疾患・腎臓疾患・循環器疾患(高血圧・狭心症・不整脈・多血症など)・強皮症・ズデック症候群・関節リウマチ・乳幼児等[リンパ浮腫治療を受ける前に主治医に相談する必要がある]