技師長あいさつ
- 当院が目指す救急医療・高度医療・患者さま中心の医療に貢献するため、専門能力を活かして正確で安全な検査を行い、患者さまや診療の要望に応える検査サービスを提供しています。
- チーム医療では、臨床検査技師もチーム医療の一員として、感染管理チーム (ICT) や栄養サポートチーム (NST) などさまざまなチームで知識や技術を提供しています。
- 教育では、最先端の検査技術やレジデント制度を導入するなど臨床検査の発展に貢献できる資質の高い人材の育成に努めています。
- 当検査室では、2019年にISO15189の認定を取得しました。ISO15189の要求事項に基づいた品質マネジメントシステムを構築して、マネジメントレビューを通じて品質方針を見直し、年度ごとに品質目標および品質指標を設定・検証して定期的な見直しや改善をするといったPDCAを回すことで臨床検査の品質を維持しています。
- 臨床検査技術部では、 “診断・治療に貢献する安心・安全・迅速な検査” をキャッチコピーに臨床検査業務に取り組んでいます。
部門紹介
検体検査部門
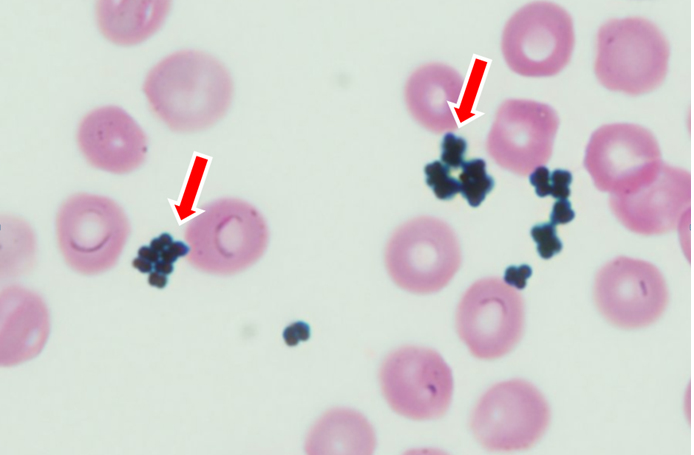
検体検査では、生化学・免疫検査(血中薬物・内分泌・腫瘍マーカー)、血液学検査(血算・凝固・形態)、一般検査(定性・沈渣・髄液検査)、緊急検査を実施しています。自動分析装置や顕微鏡などいろいろな方法で検査を行い、疾患の診断や治療、経過観察などに役立てるために、迅速に精度の高い検査結果を報告しています。
生化学・免疫検査
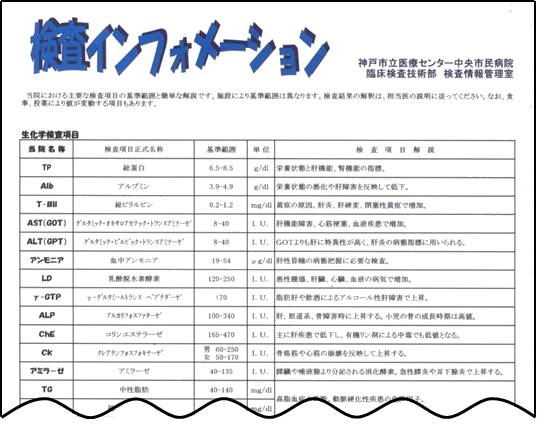
生化学・免疫検査では、患者さんから採取された血液(主に血清)や尿、胸水、腹水、髄液などに含まれる成分について検査しています。血液や尿などに含まれる糖、脂質、電解質、たんぱく質などの成分は、臓器の障害により変動します。測定する方法によって、酵素やたんぱく質、脂質、電解質などの生化学検査、ホルモンや腫瘍マーカーなどの免疫検査に分かれます。検体到着から約1時間以内に結果報告し、診察前に検査結果が分かるように努めています。
生化学・免疫検査の項目の一覧表
生化学検査
- 総たんぱく質
- アルブミン
- 総ビリルビン
- 間接ビリルビン
- AST (GOT)
- ALT (GPT)
- LDH
- ALP
- YGPT
- LAP
- Ch-E
- CK
- CK MB
- AMY
- LIP
- BUN
- CRE
- UA
- Na
- K
- Cl
- Ca
- IP
- Fe
- UIBC
- Mg
- TG
- T-CHO
- HDL
- LDL
- Glu
- グリコアルブミン
- HbA1c
- NAG
- UTP
- ハプトグロビン型判定なし
- 血液ガス
- エタノール
- アンモニア
- アンバウンドビリルビン
- ICG
- 浸透圧
- 血中薬物濃度
- フェニトイン
- フェノバルビタール
- カルバマゼピン
- バルプロ酸ナトリウム
- テオフィリン
- ジゴキシン
- アセトアミノフェン
- 炭酸リチウム
- サリチル酸
- メトトレキサート
免疫検査
- CRP
- IgG
- IgA
- IgM
- IgE
- C3
- C4
- pre ALB
- RF
- β2MG
- KL 6
- SP-D
- sIL 2R
- NGAL
- AFP
- CEA
- CA19-9
- CA15-3
- シフラ
- CA125
- インスリン
- CPR
- フェリチン
- プロラクチン
- コルチゾール
- TSH
- T3
- T4
- FT3
- FT4
- サイログロブリン
- TGAb
- TRAb
- TPOAb
- HCG
- GH
- プロカルシトニン
- NT Pro BNP
- PIVKA Ⅱ
- 高感度PSA
- SCC
- LH
- FSH
- トロポニンI
- ACTH
- iPTH
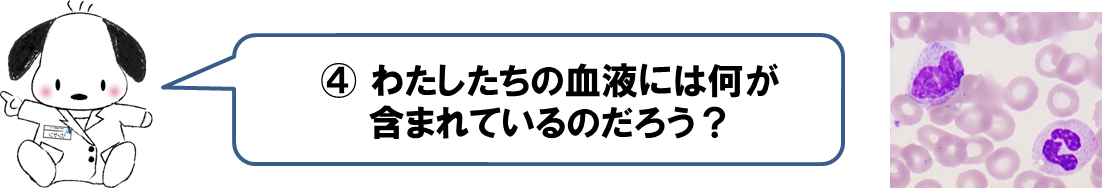
血液検査
血液検査室では、赤血球、白血球、血小板の数や大きさ、ヘモグロビン濃度などを調べる血液一般検査や、白血球の分類や形態、赤血球や血小板の形態を調べる血液像検査、また、出血しやすい病気や血栓のできやすい病気などを調べる凝固線溶検査を行っています。その他に、血小板機能をみる検査の1つである血小板凝集能、赤血球沈降速度などの検査を行っています。
血液一般・凝固等の項目の一覧表
血液一般・凝固等の項目の一覧表
- WBC
- RBC
- HGB
- HCT
- PLT
- RET
- 白血球分類
- 目視鏡検
凝固検査
- PT
- APTT
- フィブリノゲン
- Dダイマー
- ATⅢ
- クロスミキシング
その他
- 赤血球沈降速度
- βD-グルカン
- マラリア
- 赤血球抵抗試験
- 凝集能検査
- 好酸球
- 特殊染色
一般検査部門
一般検査室では、尿検査(定性、沈渣)、便検査(便潜血)など、腎臓をはじめ各臓器の疾病の補助診断、及び治療の経過観察に必要な検査を行っています。材料となる尿や便は、人体の排泄物として患者に苦痛を与えず、最も容易に採取できるため、基礎的な検査として用いられています。尿検査では、尿中正常成分の量的変化や異常成分の出現によって腎・尿路系疾患だけでなく、糖尿病などの他の各種疾患の診断にも役立ちます。
尿・便検査項目の一覧表
尿検査
- 尿定性
- 尿沈渣
- 尿中BTA
便検査
- 便中ヘモグロビン
- 便脂肪染色
その他
- 髄液検査
- 穿刺液Ph、比重
- 関節液結晶
- 尿素呼気試験
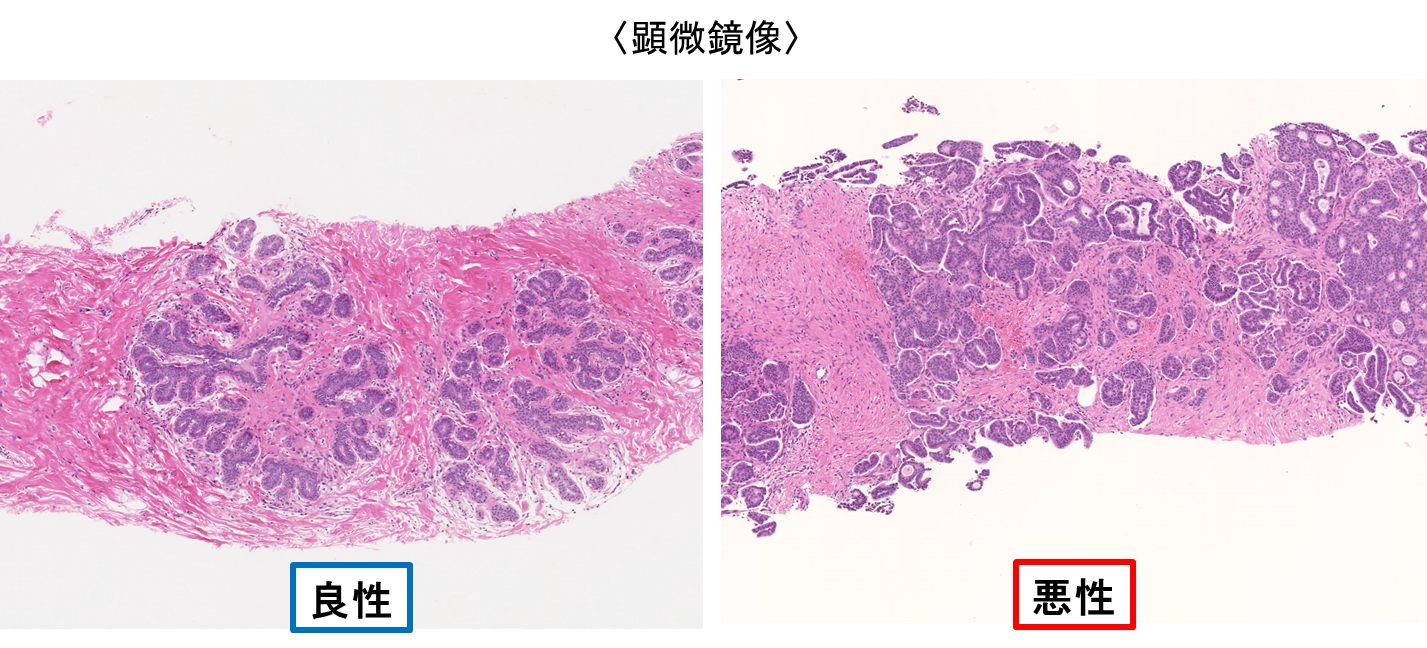
病理検査
病気の良性・悪性などを正確に診断するための病理組織検査と細胞診検査を、病理診断科の病理医(部長・原 重雄先生)の指導のもとで臨床検査技師10名(内 細胞検査士7名、認定病理検査士3名)が業務に携わっています。
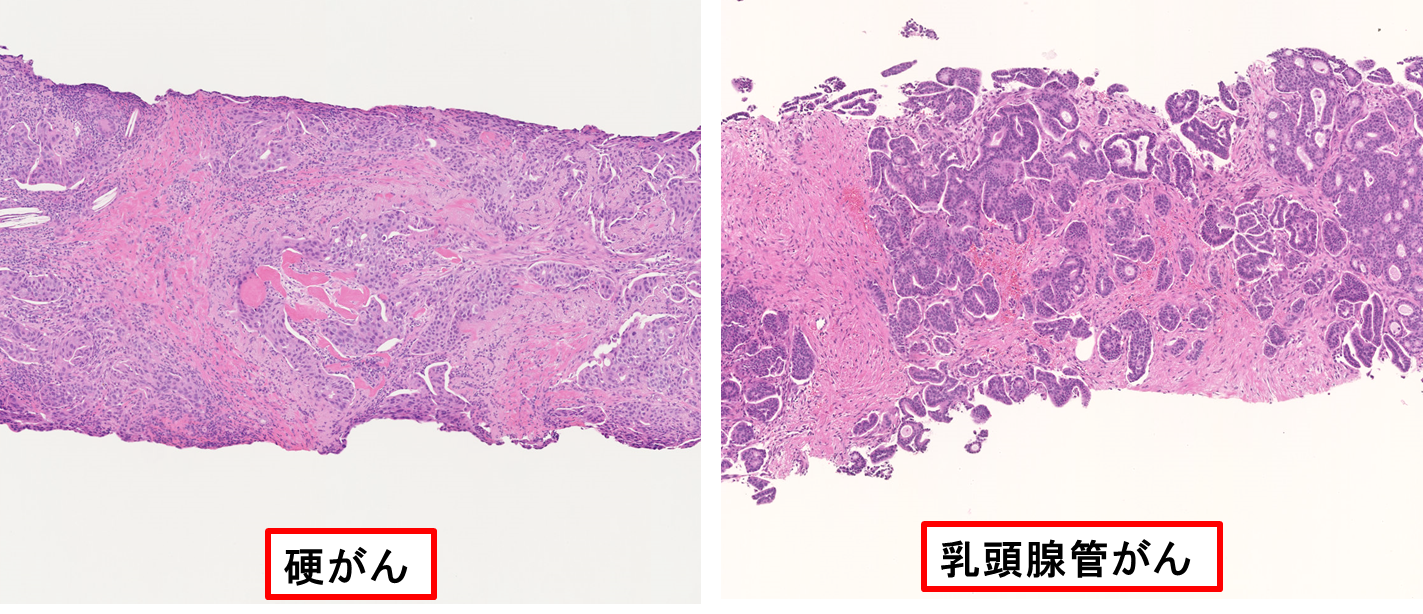
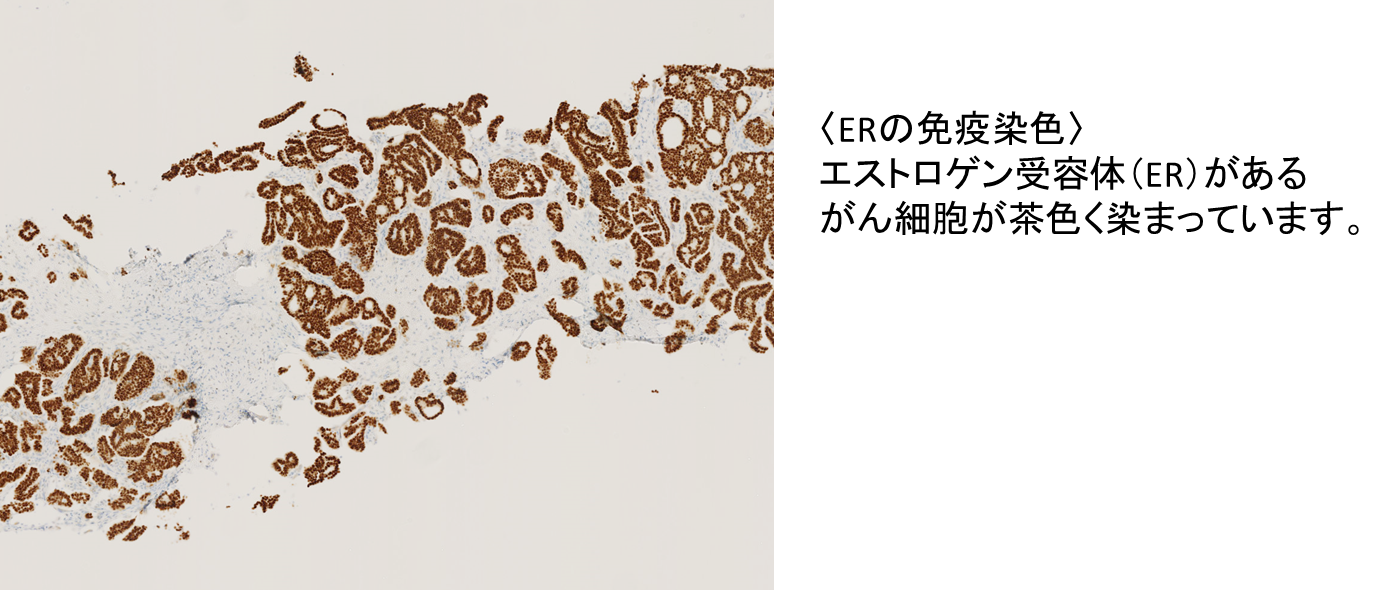
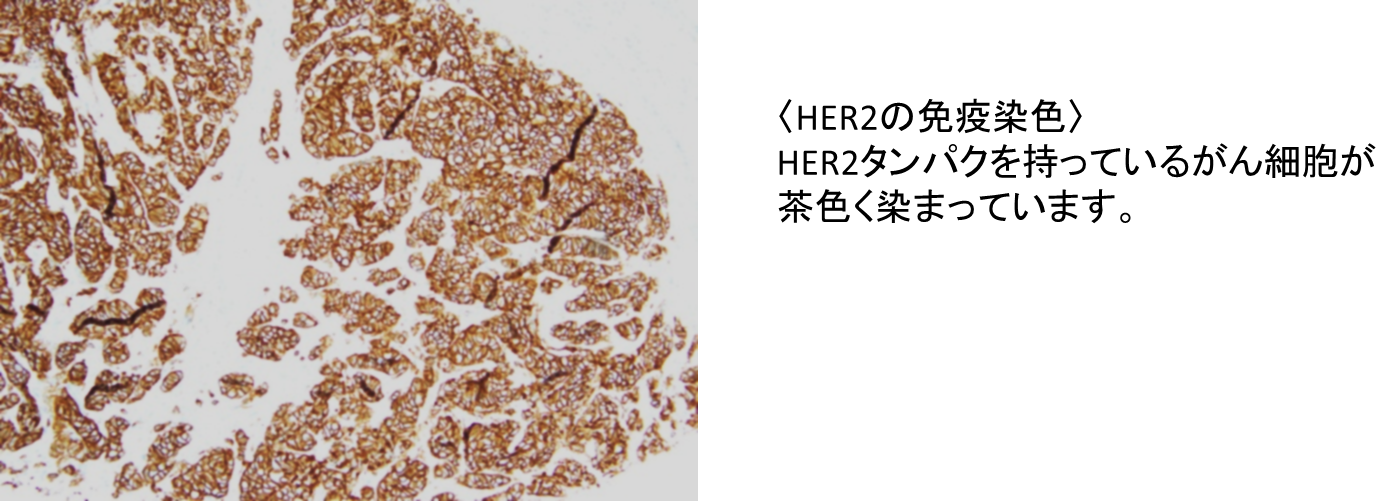
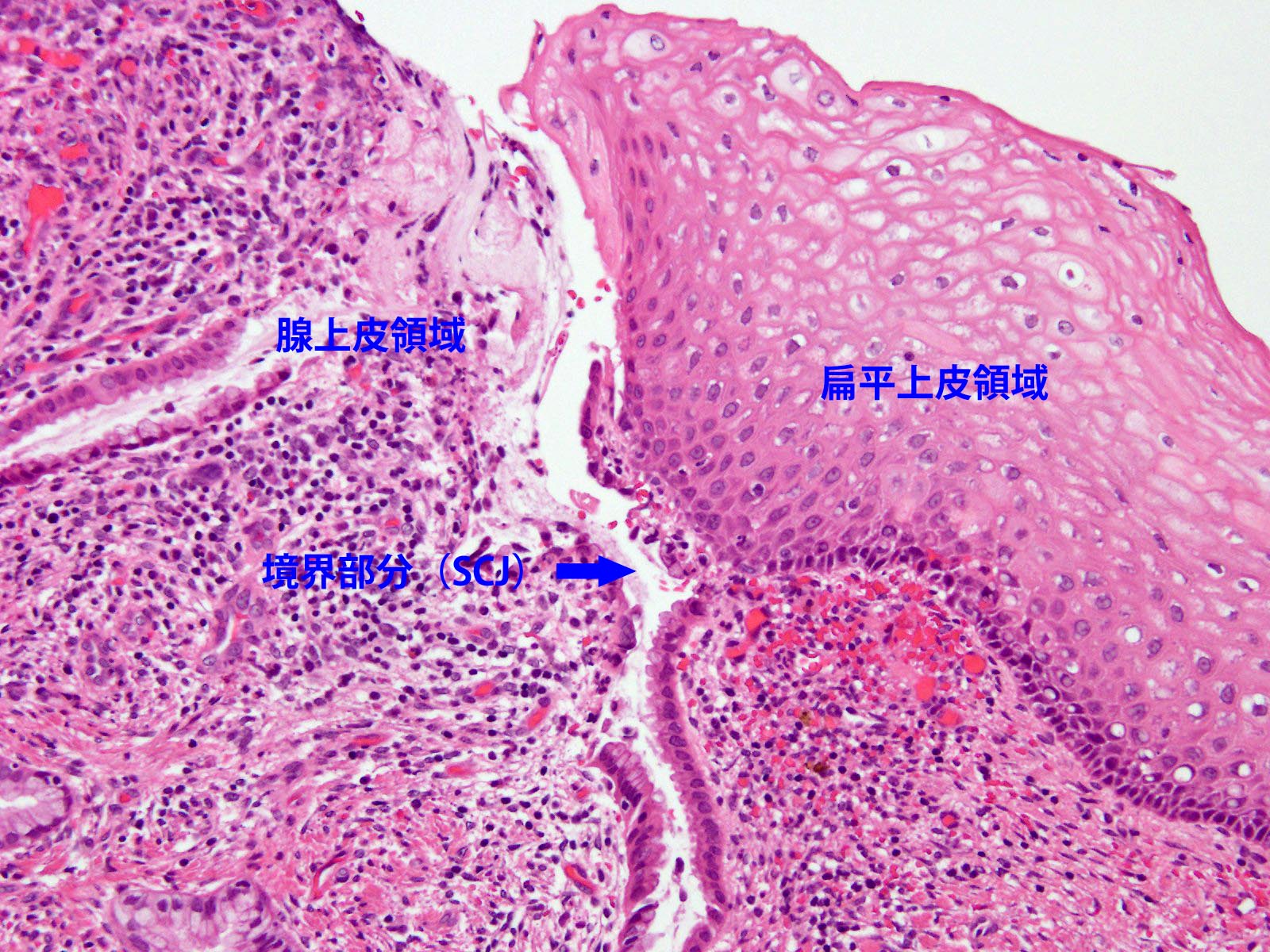
病理組織検査は、手術や生検で採取した組織片を一定の操作のあとにHE染色や免疫染色をして、病理医が顕微鏡で組織形態を調べる検査です。特殊な検査として、腎臓疾患などでの蛍光抗体検査、乳癌の薬物療法に関わる検査、分子標的薬の適合に関わる検査などもサポートしています。
細胞診検査は、子宮頚膣部や子宮体部、喀痰、尿、胸水、腹水、その他各種臓器由来の細胞を採取して、一定の操作のあとに染色を行い細胞検査士が顕微鏡で癌細胞などの有無を調べる検査です。当院では昨年2017年度から液状化細胞診(LBC)の方法を用いた検体処理法も導入して診断精度の向上を図っています。
また、術中迅速診断検査、病理解剖の介助、臨床病理カンファレンス(CPC)や臨床医の学会発表の支援、臨床治験なども積極的にサポートしています。さらに、がんゲノム医療連携病院としての病理検査室の役割も果たしています。
細胞遺伝子部門
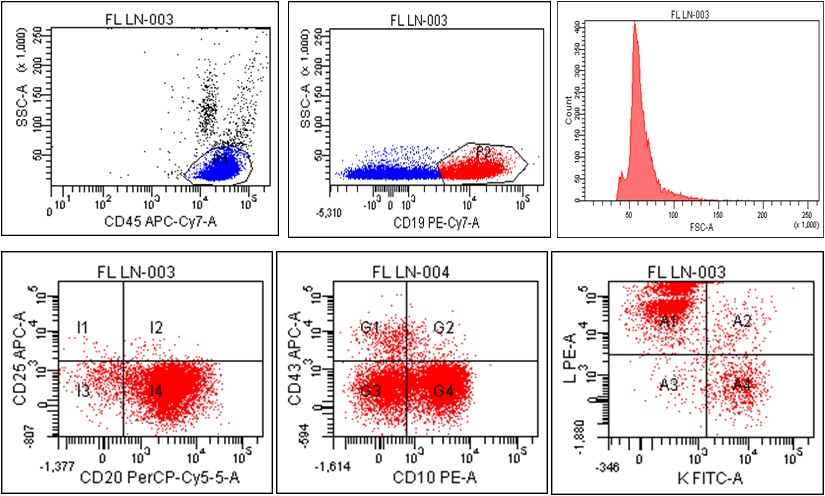
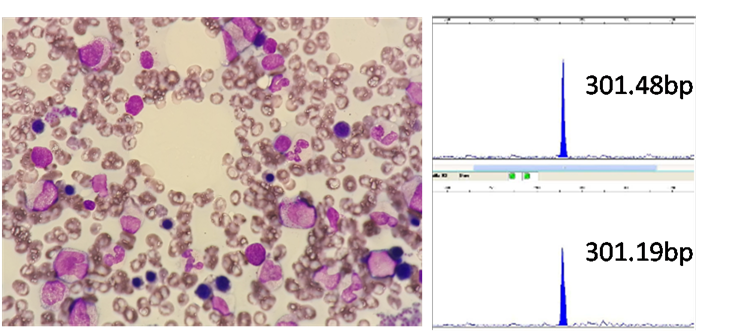
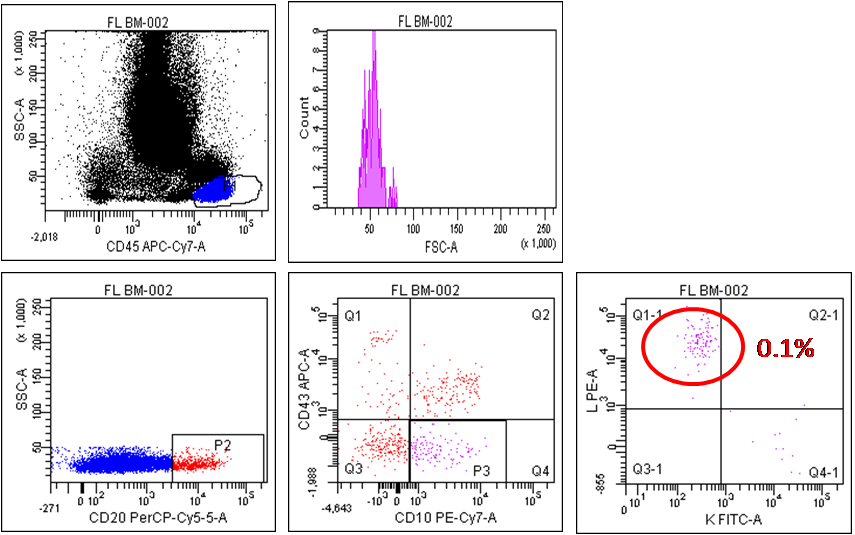
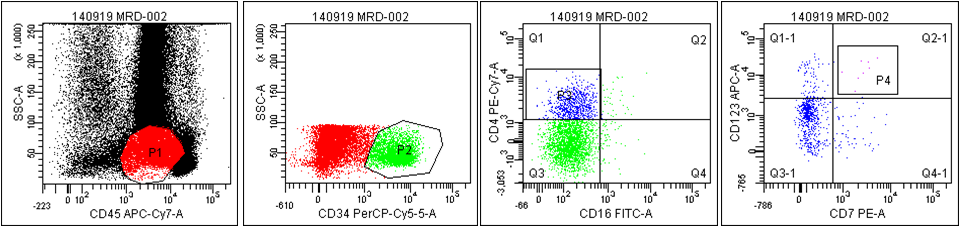
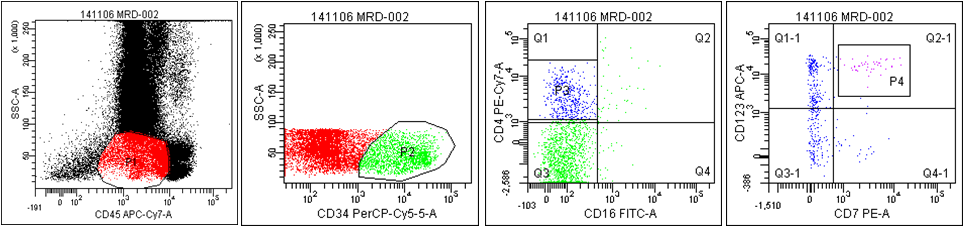
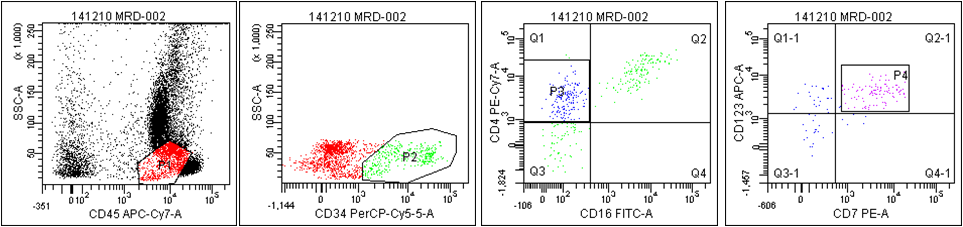
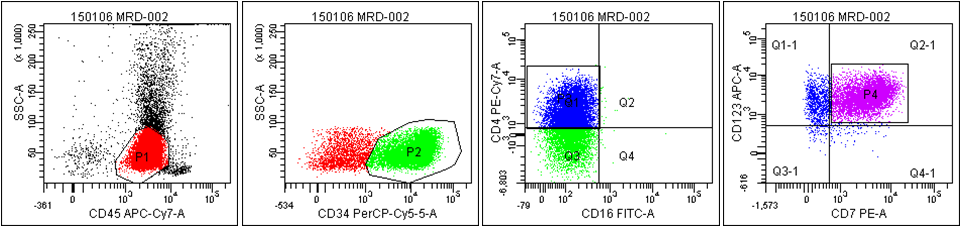
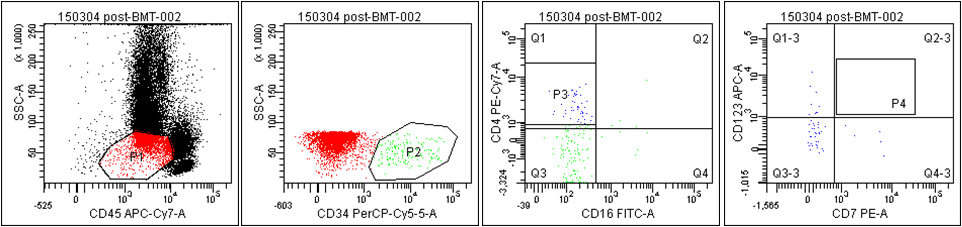
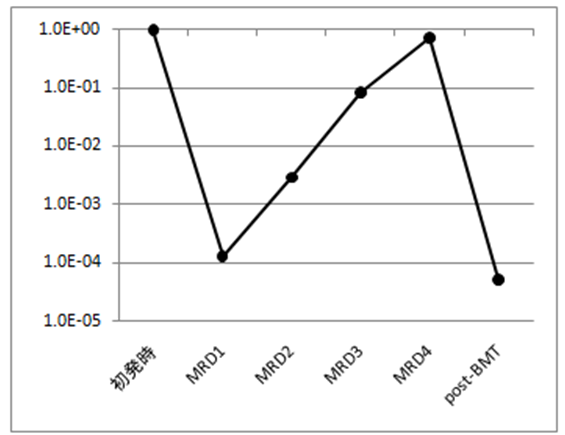
造血器腫瘍の病型診断や治療効果の判定・予後分類に重要な測定可能残存病変(MRD)の検出において、従来の形態学的検査や染色体検査に加え、フローサイトメトリー(FCM)検査や遺伝子検査の重要性がますます高まっています。
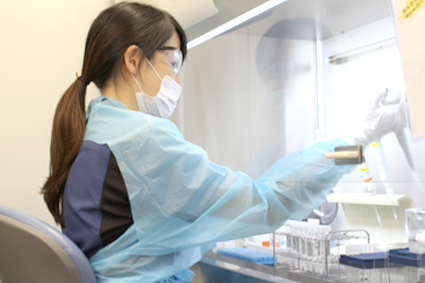
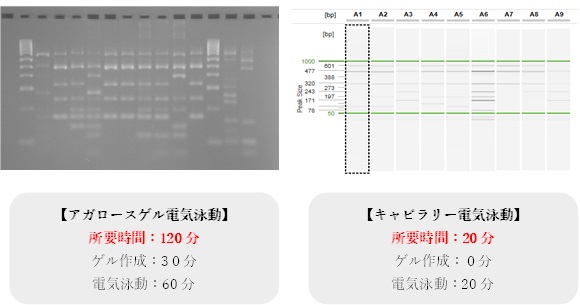
当部門では、骨髄像検査、FCMによる細胞検査、PCR法による遺伝子検査を同一部門内で実施している全国でも稀な検査体制をとっています。検査結果をいち早く報告することは勿論のこと、検査結果を総合的に解釈する能力を高めることができ、臨床医や他の検査部門との密なディスカッションを行うことが可能となっています。
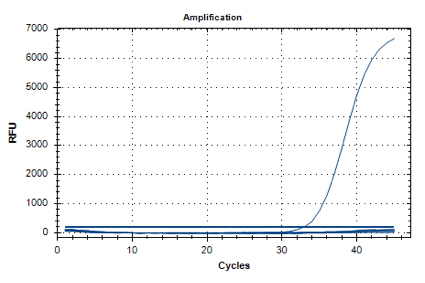
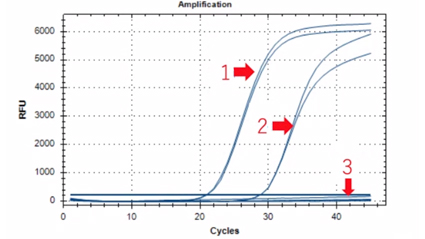
FCM検査では10カラー解析が可能な次世代型フローサイトメーターを導入し、EuroFlowから提唱されている解析法をベースに当院で開発したKobeFlowを実施し、精度の高い検査を提供しています。また、遺伝子検査においても、デジタルPCRなどの最新機器を導入し、多種多様な遺伝子異常の検出を実施しています。最近では、日和見感染症関連ウイルスPCR検査などを導入し、造血器腫瘍分野のみでなく感染症分野においても長年培ったノウハウを活用しています。
検査項目
骨髄像検査
- 骨髄像の判読
細胞検査(FCM)
- 末梢血リンパ球サブセット検査
- T細胞・B細胞・NK細胞百分率検査
- T細胞サブセット百分率検査
- 造血器腫瘍細胞抗原検査
- CCR4タンパク
- CD34陽性造血幹細胞数測定
- CD3陽性T細胞数測定
- 網状血小板比率
- 高感度PNH血球検査
遺伝子検査(PCR)
- 造血器腫瘍遺伝子検査
- Major BCR::ABL1 定量検査
- minor BCR-::BL1定量検査
- RUNX1::RUNX1T1定量検査
- PML::RARA定量検査
- CBFB::MYH11定量検査
- TCF3::PBX1定量検査
- FUS::ERG定量検査
- DEK::NUP214定量検査
- KMT2A再構成定量検査
- NPM1変異定量検査
- WT1 mRNA定量検査
- MYD88 L265P定量検査
- RHOA G17V定量検査
- BRAF V600E定量検査
- JAK2 V617F定量検査
- MPL変異検査
- CALR変異検査
- JAK2 exon12変異検査
- CD79B変異検査
- STAT3変異検査
- UBA1変異検査
- EZH2変異検査
- SF3B1変異検査
- KIT変異検査
- IGH::BCL2検査
- 網羅的AML遺伝子変異検査
(FLT3-ITD,FLT3-TKD,NPM1,KRAS,NRAS,IDH1,IDH2,TP53,DNMT3A,CEBPA,ASXL1,RUNX1) - 患者特異的FLT3-ITD定量検査
- 免疫関連遺伝子再構成
- IGH再構成検査
- IGL再構成検査
- TCRB再構成検査
- TCRG再構成検査
- TCRD再構成検査
キメリズム解析
- 移植前スクリーニング解析
- 移植後キメリズム解析
ウイルス検査
- 日和見感染症関連ウイルス定量検査
(HSV1,HSV2,VZV,CMV,EBV,HHV6,HHV7,HHV8,ParvoB19,BKV,JCV,ADV)
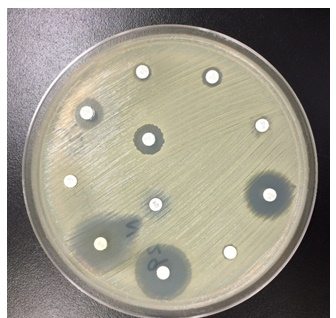
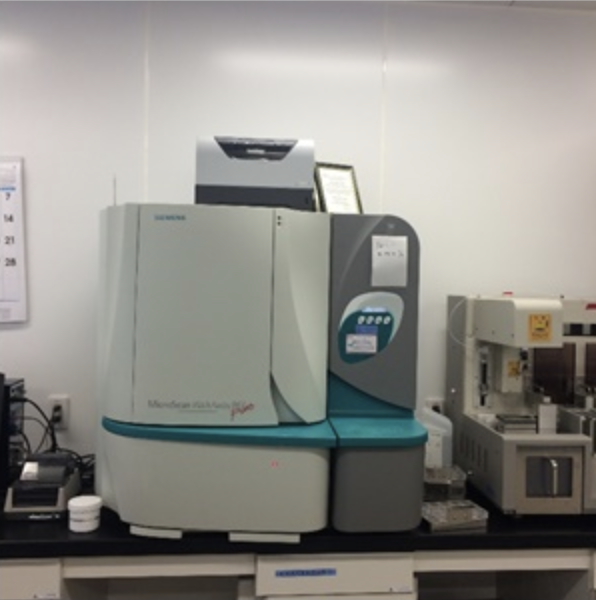
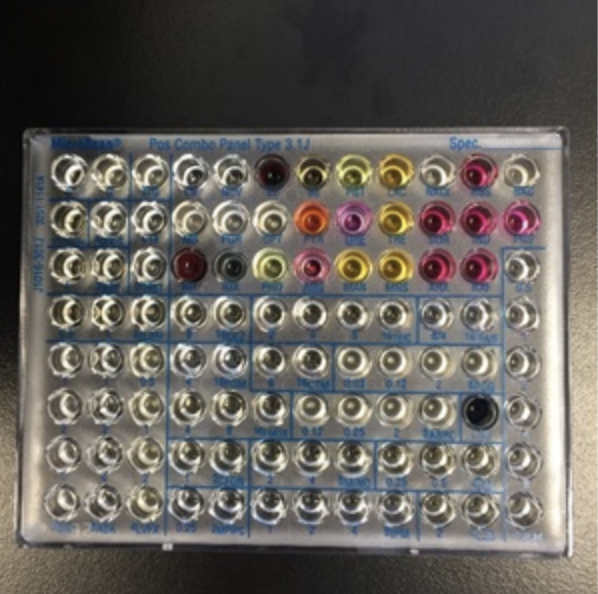
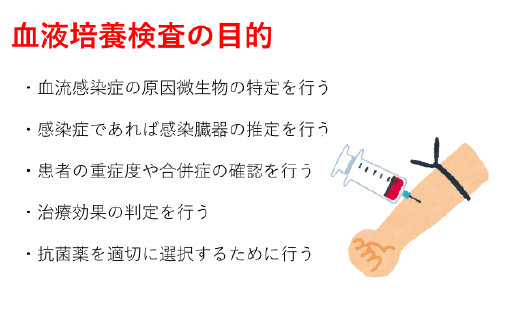
微生物検査部門
各種臨床検体の細菌培養、薬剤感受性検査および免疫学・遺伝子学的感染症検査を実施しています。種々の細菌・ウイルス迅速診断検査も常時行える体制をとっています。また、チーム医療としてICT及びAST活動に積極的に参画し院内感染予防対策に貢献しています。
検査項目
一般細菌検査
- 塗抹検査
- 培養
- 同定検査(質量分析など)
- 薬剤感受性検査
- 遺伝子検査
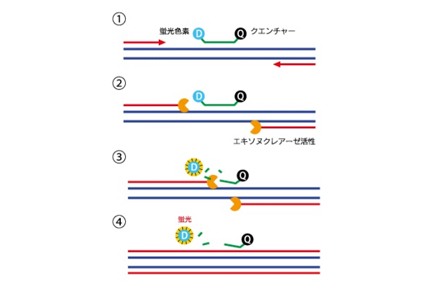
- PCR-Quenching Probe(QProbe)法によるマイコプラズマの検出
- 16S rRNA遺伝子PCR及びシーケンス解析
- ITS領域遺伝子PCR及びシーケンス解析
- D1/D2領域遺伝子PCR及びシーケンス解析
- 各種薬剤耐性遺伝子PCR
- 菌種特異的遺伝子PCR
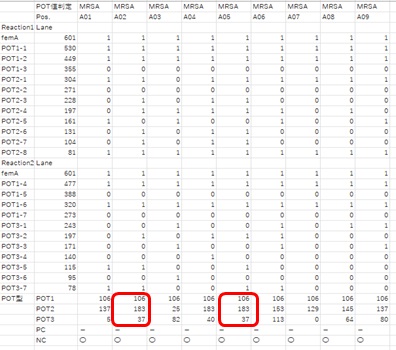
- POT法を用いた型別
抗酸菌検査
- 塗抹検査
- 培養・同定検査
- 薬剤感受性検査
- 遺伝子検査
- PCR-Quenching Probe(QProbe)法による結核菌群、Mycobacterium avium、Mycobacteriumin tracellulareの検出
迅速検査
- 抗原、抗体及び毒素検出検査(検査材料はそれぞれ異なる)
- 新型コロナウイルス
- インフルエンザウイルス
- アデノウイルス
- ロタウイルス
- ノロウイルス
- デングウイルス
- 肺炎球菌
- レジオネラ
- CDトキシン 等
- HBV-DNA定量検査
- HCV-RNA定量検査
感染症マーカー検査
- B型肝炎関連マーカー
- C型肝炎関連マーカー
- 梅毒検査
- HIV関連マーカー
- HTLV-1関連マーカー
免疫抑制剤
- タクロリムス血中濃度測定
- シクロスポリン血中濃度測定
抗MRSA薬
- バンコマイシン血中濃度測定
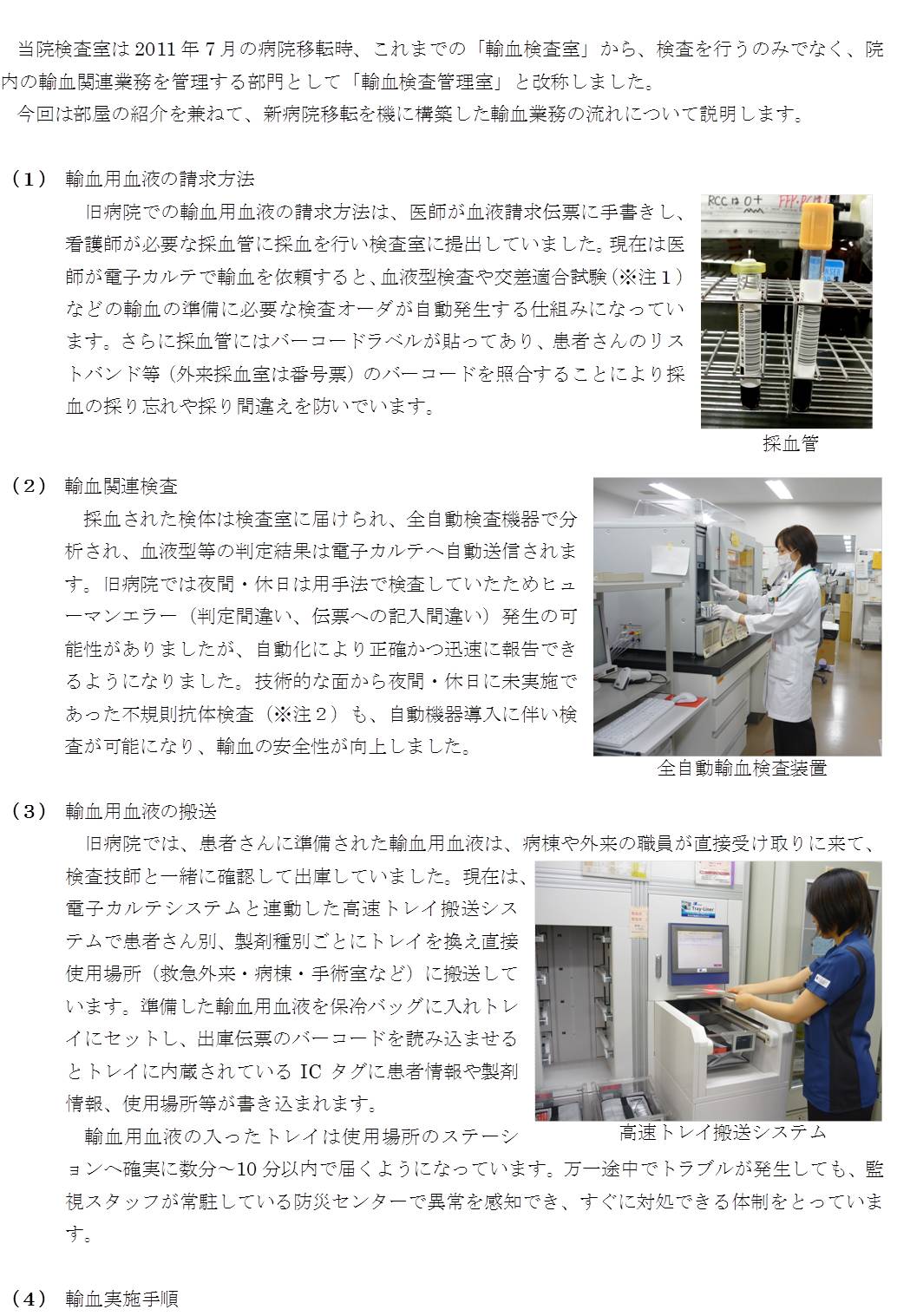
輸血検査管理室
血液型検査・不規則抗体検査・交差適合試験の実施や血液製剤・アルブミン製剤の一元管理を行い、輸血に関する業務を統括管理する部門です。救急外来には超緊急用の輸血製剤を常時設置し、緊急性の高い輸血に24時間365日対応できる体制を整えています。
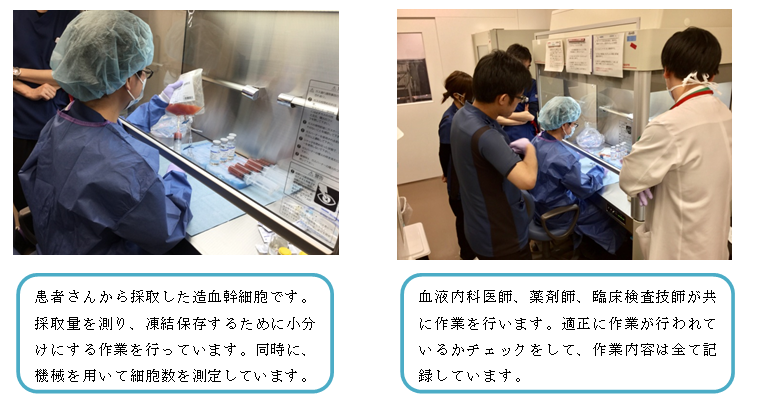
さらに、医師や薬剤師、臨床工学技士と協力し、CAR-T細胞療法をはじめ、末梢血幹細胞の調製、臍帯血・骨髄血の移植、顆粒球輸注やドナーリンパ球輸注など、造血幹細胞関連の一括管理も行っています。
検査項目
血液型検査
- ABO式血液型検査
- Rh(D)血液型検査
- ABO亜型検査
- 移植時血液型検査
不規則抗体検査
- 抗体スクリーニング検査
- 不規則抗体同定検査
交差適合試験
その他の検査
- 直接クームス検査
- 間接クームス検査
- D-L抗体
- 抗体価測定
特殊検査部門
今日、インターネット等の普及により中毒に関する情報や様々な薬物毒物を容易に入手する事が可能となりました、この為、中毒の起因となる物質は多種多様ではありますが、起因物質の検索は早急に対応しなければなりません。当部門では簡易測定試薬及び精密分析測定機器を用いて中毒起因物質の検索を実施しています。また、臨床からの要望により分離分析などによる精査も実施しています。
検査項目
- 簡易測定試薬による検査
- 尿中メタノール
- 尿中有機リン系農薬
- 尿中カーバメイト系農薬
- 尿中パラコート
- 尿中ヒ素化合物
- 血中青酸化合物
- 精密分析測定機器(ガスクロマトグラフ質量分析計:GC/MS)による検査
検査情報管理部門
PFI事業の検体検査業務に関して、委託業務の管理や運用の調整を行っています。検査システムの保守管理や医療の質の向上のため、各種チーム医療にも参画しています (NST、糖尿病教室、腎臓病教室など)。また、患者、臨床へのサービス業務として検査相談室を併設し、診療側へのすべての検査に係わる情報提供、相談対応、苦情対応やホームページ更新、患者向け検査インフォメーションの発行、データベース利用による診療支援、臨床研究治験業務の支援も行っています。
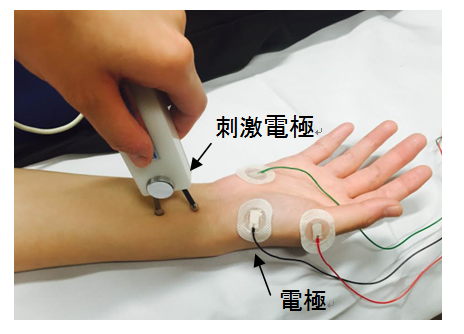
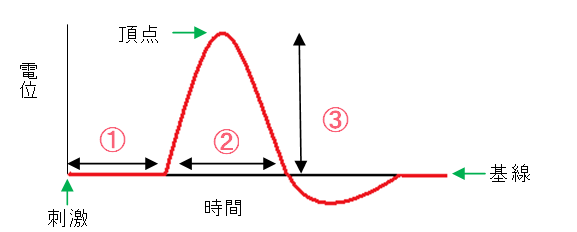
神経生理検査部門
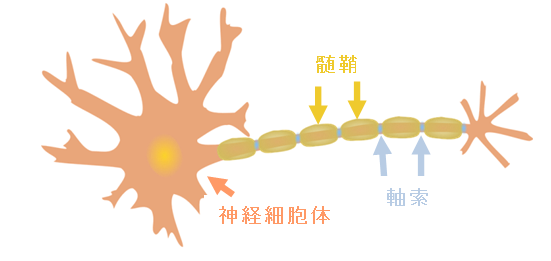
末梢神経系と中枢神経系の神経生理検査と頭頚部血管系の超音波検査を行っています。機能検査は脳波検査、神経伝道検査、誘発電位検査 (聴性脳幹反応、体性感覚誘発電位、視覚誘発電位)、針筋電図検査です。神経生理検査は末梢神経や中枢神経に刺激を与え、神経の電気活動を応用して神経機能を評価する検査法です。近年、この手法を用いた術中神経モニタリングが行われるようになってきており、当検査室でも術中麻酔下で脳機能、脊髄機能をリアルタイムにモニタリングを行い、神経機能温存を目指した手術での要望に応えています。また、人工内耳埋め込み術後の聴覚神経経路の確認のためE-ABRも行っています。
検査項目
神経伝導検査(NCS)
- 運動神経伝導検査(MCS,F波)
- 感覚神経伝導検査(SCS)
- 反復刺激試験
- 磁気刺激検査
大脳・脳幹誘発電位
- 聴性脳幹反応(ABR)
- 体性感覚誘発電位(SEP)
- 視覚誘発電位(VEP)
その他誘発電位
- 瞬目反射
- 磁気刺激運動誘発電位
術中神経モニタリング(IOM)
脳波検査(EEG)
終夜睡眠ポリソムノグラフィ(PSG)
頚動脈超音波検査
経頭蓋脳血管超音波検査
外来採血部門
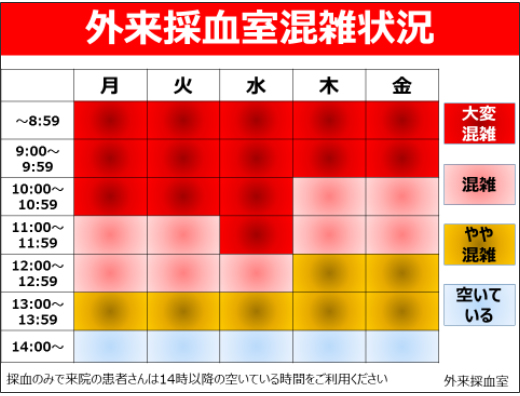
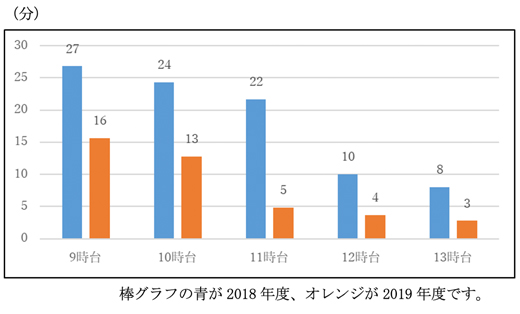
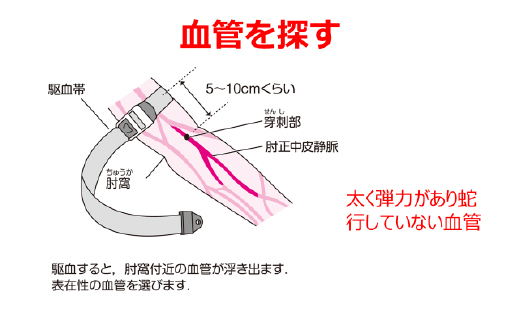
一カ月に10,000人を超える外来患者の採血を行っています。自動受付システムにより診察券を通すだけで採血整理券が発行され、その番号により採血ブースまで誘導される仕組みで、採血時には整理券と採血管のバーコードを照合するシステムを導入し患者確認を行っています。
採血ブースは8ブースあり、外来一般採血以外に血液培養の無菌採血や治験症例、癌ゲノム診療の採血も行っています。
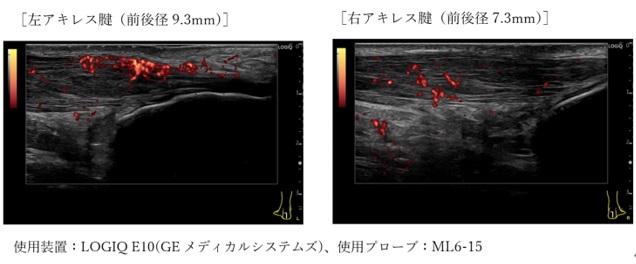
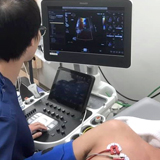
腹部体表超音波検査部門
腹部臓器全般、乳腺、甲状腺、耳鼻科系(耳下腺、顎下腺)、脈管系(大動脈、末梢血管など)を対象とした、スクリーニング検査・症状の原因究明の検査・経過観察の検査・術前術後の評価・急性腹症などの至急対応や超音波造影剤を用いた造影エコーなどにも対応しています。また、カラードプラ・パルスドプラ法を用いた臓器・病変の血行動態評価を行い、良悪性の鑑別、炎症ステージの分類など質的診断も行っています。
腹部体表超音波検査
超音波検査は体外から超音波をあてて、臓器などから跳ね返ってくる信号で画像を作り距離や形から病態を診る検査です。当検査室では腹部超音波検査、乳腺超音波検査、甲状腺超音波検査や上肢下肢の血管超音波検査、造影剤を使用した造影超音波などの特殊検査も実施しています。超音波検査は痛みや身体への害はなく安全な検査です。妊娠中の方も安心して受けて頂くことができます。
また、重症下肢虚血の血管再生治療(臨床試験)に係わる皮膚灌流圧測定や動脈超音波検査などを含めた精密検査も行っています。
検査項目
- 腹部超音波検査
- 乳腺超音波検査
- 甲状腺超音波検査
- 体表超音波検査
- 血管超音波検査(下肢動脈・静脈、上肢動脈・静脈)
- 腹部造影超音波検査(精査、スクリーニング)
- 乳腺造影超音波検査
下肢動脈精密検査
閉塞性動脈硬化症やバージャー病を対象としたCD34陽性細胞移植による血管再生治療の臨床試験の検査を行っています。これは、患肢の動脈性血行動態を毛細血管レベルの灌流圧や経皮酸素分圧、指尖の動脈圧などを測定して評価する精密検査です。専門的な検査を行い、下肢動脈血管の再生治療前後の評価を行っています。
検査項目
- 下肢動脈超音波検査
- 皮膚灌流圧測定
- 経皮酸素分圧測定
- 指尖動脈圧測定
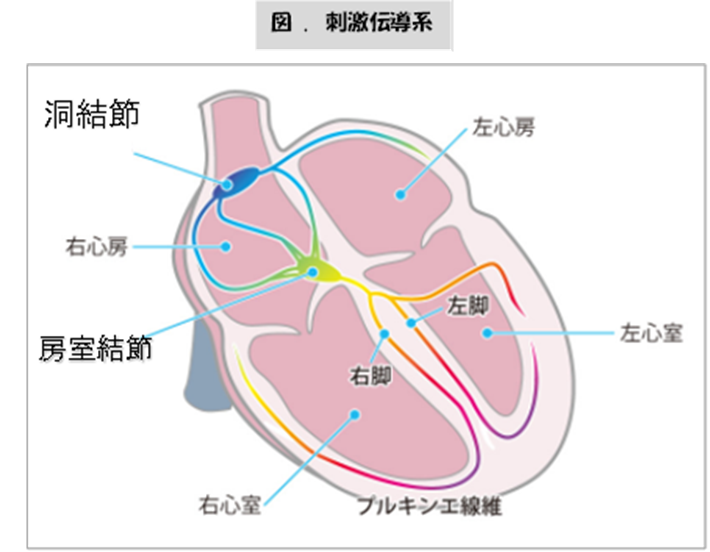
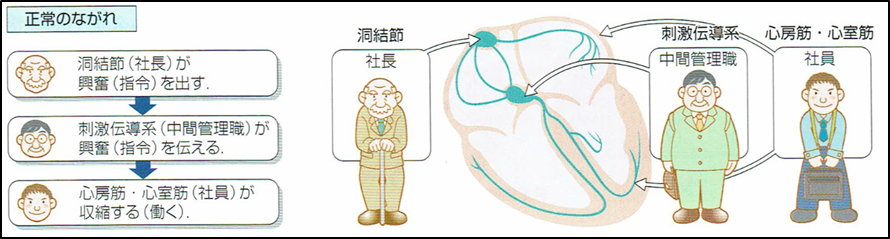
心肺機能検査部門
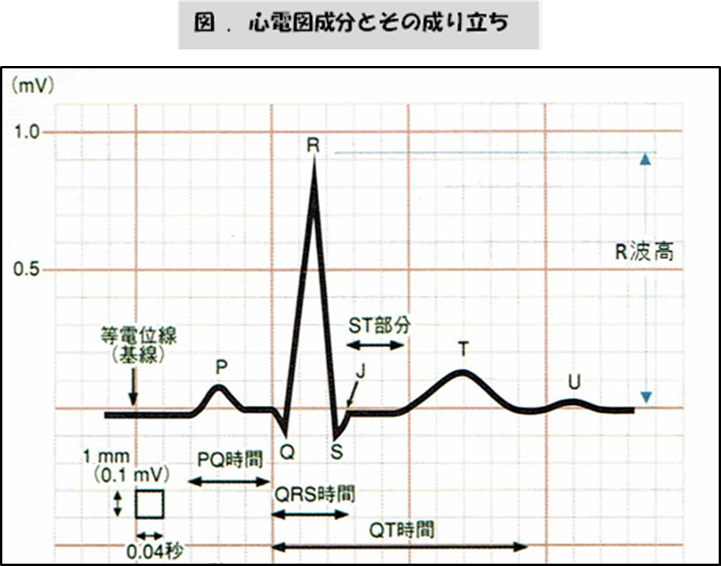
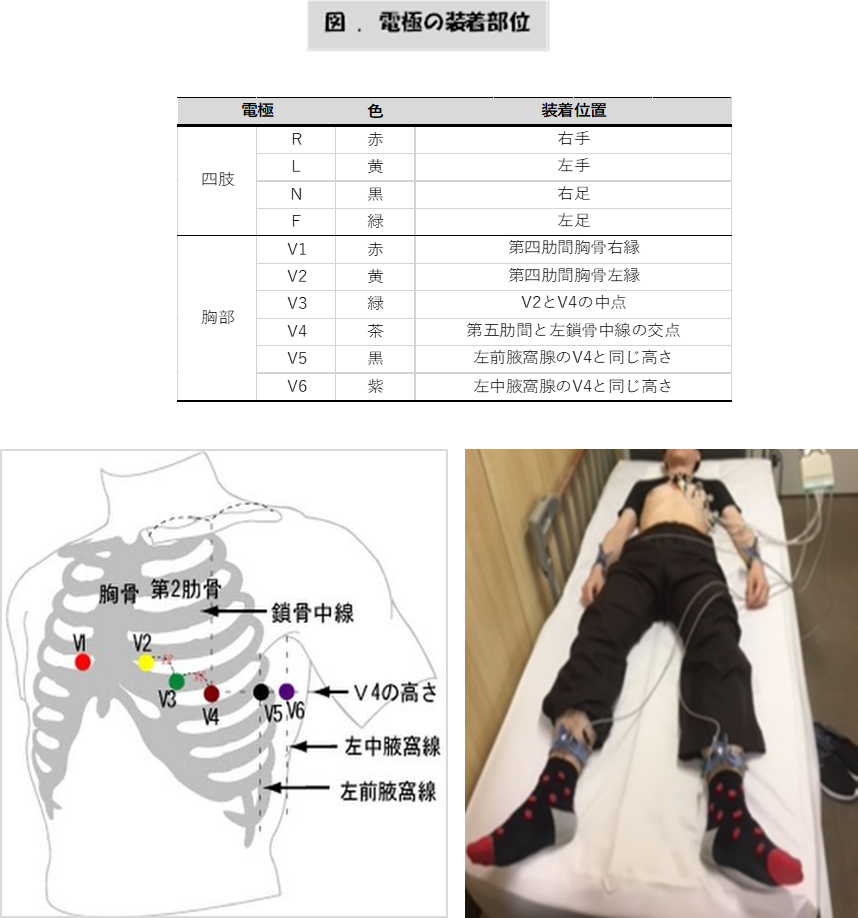
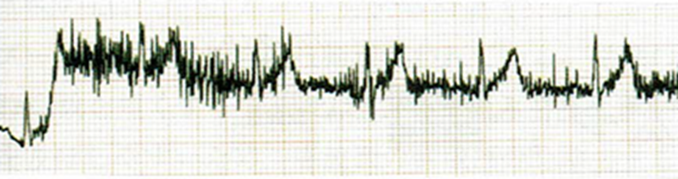
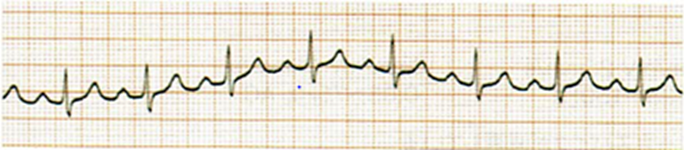
循環器 (主に心臓)と呼吸器 (主に肺や気管支)の機能について検査しています。循環器の検査には心電図検査 や心臓超音波(心エコー)検査などがあり、心臓の状態を調べます。一方、呼吸器の検査には肺機能検査や気道可逆性試験などがあり、換気機能 (肺の中への空気の換気状態)や酸素と二酸化炭素のガス交換機能を調べています。
検査項目
心電図検査
- 安静心電図検査
- 運動負荷心電図検査(トレッドミル負荷心電図検査)
- 携帯型発作時心電図検査
- 24時間・7日間・21日間心電図検査(ホルター心電図検査)
- 自律神経機能検査(CVRR)
血圧脈波図検査(PWV・ABI)
肺機能検査
- 肺活量(VC)
- %肺活量(%VC)
- 努力性肺活量(FVC)
- 1秒量(FEV1)
- 1秒率(%FEV1)
- 残気量(FRC)
- 肺拡散能力(DLCO)
- 気道可逆性試験
- 呼吸抵抗検査
心臓超音波検査
- 経胸壁心エコー図検査(TTE)
- 経食道心エコー図検査(TEE)
- 負荷心エコー図検査 (運動・薬物)
- マイクロバブルテスト
チーム医療
チーム医療とは、医師と看護師、臨床検査技師、薬剤師、管理栄養士、理学療法士などの他の医療スタッフがお互いの専門性を生かし、最大限の能力を引き出し合うことによって、患者さん中心の治療をおこなう医療現場の取り組みです。それぞれの専門分野のスタッフが所見を述べ、コミュニケーションを密にすることにより、患者さんにとって最も効果的な治療法や方針が検討されていきます。
臨床検査技師が関わる院内チーム医療
1.栄養サポートチーム

2.院内患者教室

3.感染管理チーム

4.フットケアチーム
下肢に血流障害や潰瘍のある患者さんに対し、「足を守ること」を目的として活動するチームです。皮膚科医、循環器内科医、慢性疾患看護専門看護師等と症例検討会を実施しています。臨床検査技師は、治療方針決定のために必要となる詳細な血流評価に関わる各種検査を行ないデータを提供しています。
5.医療安全管理チーム
病院で報告されるインシデントレポートは、統計的に“病床数×5”と言われています(当院の場合は年間約3,500事例)。技師長が医療安全管理室の副室長として医療安全管理チームに加わり、多職種と合同で院内の全ての部署から報告されるインシデント事例について原因を明確にして、各部門での対応、改善策の立案、再発防止に向けたPDCAの状況などを検証しています。 また、臨床検査技術部の医療安全文化を推進するために、検査部の事例を検証、改善対策の進捗を監視して検査部門の医療安全をコントロールしています。
6.クリニカルパス
クニニカルパスとは、入院患者さんの病気を治すうえで必要な治療、ケアや検査などの情報を記載した診療スケジュール表であり、医療の標準化と効率化を目的として作成されたものです。患者さんの検査に対する不安を緩和し、安心して検査を受けられるように検査の内容、必要性や注意事項を記載したパンフレットを作成しています。
7.検査相談室
検査相談室は、院内の医療従事者から検査に寄せられるさまざまな相談、問合せ、クレームや要望などの窓口を一元化し、病院業務が円滑に機能することを目指しております。患者さん向けの検査項目の説明を記載した“検査インフォメーション”を発行し、採血室や総合受付などで配布しています。
臨床研究
残余検体(診療後に残った血液、尿、組織などの検体)の研究利用について| 研究課題名 | 説明文 (PDF) |
| マルチモダリティを用いた心エコー検査における大動脈弁狭窄症の最適アプローチの考案 | |
|---|---|
| 急性骨髄性白血病患者におけるIDH1もしくはIDH2遺伝子変異を標的とした後方視的観察研究 | |
| 悪性リンパ腫細胞における抗原発現の解析 | |
| AMLにおけるフローサイトメトリー解析に有用な新規異常抗原発現の検索 | |
| 急性白血病における体細胞遺伝子変異、腫瘍細胞のCD25発現および血中sIL-2R値の関連に関する後方視的観察研究 | |
| 経カテーテル大動脈弁植え込み患者におけるABI/baPWV検査指標と心血管イベントの関連 | |
| 経胸壁心エコー検査の右室心拍出量と右室収縮能指標における関連性の検討 | |
| COVID-19 罹患後における肺機能検査指標の経時的変化と改善に関連する因子の検討 | |
| 急性白血病における体細胞遺伝子変異、腫瘍細胞のCD25発現および血中sIL-2R値の関連に関する後方視的観察研究 | |
| CAR-T療法後に発生するサイトカイン放出症候群の発症予測マーカーの検索 | |
| うっ血性心不全患者におけるエコーを用いた包括的うっ血評価と心血管イベント発症の関連 | |
|
経胸壁心エコー検査を用いた僧帽弁術後(形成術・置換術)症例における心血管イベント関連指標の検討 |
|
| 担がん患者における直接経口抗凝固薬(DOACs)による深部静脈血栓症の退縮・消失効果の検討:観察研究 | |
| 僧帽弁Barlow病におけるmitral annular disjunction(MAD)が心血管イベントに及ぼす影響の検討 | |
| オシロメトリック法およびパルスオキシメータ法による足趾血圧測定の比較 |
検査を受ける患者様へ
検査の説明・注意点など
採血・採尿検査

心電図検査

ホルター心電図検査
トレッドミル負荷心電図検査

脈波図検査
心臓超音波検査
経食道心臓超音波検査
胃カメラのように管を口に入れて食道から観察することで、経胸壁からでは観察できない部分や詳細に心臓の動きを評価できます。喉に局所麻酔をかけ、約30分の検査時間です。検査前6時間は絶飲食していただきます。
運動負荷心エコー検査

肺機能検査

気道可逆性検査
喘息のお薬を吸入する前と後で同じ肺機能の検査をして、お薬が効いているかを調べる検査です。
経皮的動脈血酸素飽和度測定

終夜睡眠ポリソムノグラフィ
就寝時の睡眠・呼吸・いびき・体内酸素濃度の状態などを調べます。検査の際に脳波や心電図、呼吸や血中酸素量を調べるためにたくさんの検査センサーを装着します。
痛みや危険性はなく安全な検査で、妊娠中の方でも安心して受けていただくことができます。
この検査は夕方からの一泊入院で行います。

腹部エコー検査
腹部臓器(肝臓・胆嚢・膵臓・腎臓・脾臓)を対象に、スクリーニングや経過観察、術前術後の評価や症状の原因究明のための検査を行っています。
急性腹症などに対しては至急対応も行っています。
超音波造影剤を用いた造影超音波検査も実施しています。
超音波造影剤は静脈注射で注入します。
検査時は、上半身は衣服を胸の下まで捲り上げ、腹部の観察ができるように準備していただきます。
検査所要時間は30分程度です。
乳腺超音波検査
乳腺超音波検査は、乳腺内のしこりや状態等を超音波で調べる検査です。
検査は乳房にゼリーを塗って行います。
痛みや危険性はなく安全な検査です。検査時間は20~30分程度です。
当院では女性技師が担当しています。
甲状腺超音波検査
甲状腺超音波検査は、甲状腺のしこりや状態等を超音波で調べる検査です。
検査は頚部にゼリーを塗って行います
痛みや危険性はなく安全な検査で、妊娠中の方でも安心して受けていただくことができます。
検査時間は10〜20分程度です。
血管超音波検査
血管超音波検査は、動脈や静脈の血流の流れを調べる検査です。検査はゼリーを塗って行います。
検査は四肢の必要部位にゼリーを塗って行います。
痛みや危険性はなく安全な検査で、妊娠中の方でも安心して受けていただくことができます。
下肢は広い範囲(ソケイ部から足首)が検査の対象になるためズボンやストッキングを脱いで頂きますのであらかじめご了承ください。
検査時間は30~60分程度です。
頚動脈超音波検査
頚動脈超音波検査は、頚動脈の血液の流れや、動脈硬化の程度を超音波で調べる検査です。
検査は頚部にゼリーを塗って行います。
痛みや危険性はなく安全な検査で、妊娠中の方でも安心して受けていただくことができます。
検査時間は15〜30分程度です。
聴力検査
聴力検査は、耳の「聞こえ」を調べる検査です。
必要に応じて数種類の検査を組み合わせる場合があります。
痛みや危険性はなく安全な検査で、妊娠中の方でも安心して受けていただくことができます。
平衡機能検査
平衡機能検査は、めまいの原因や程度を調べる検査です。
立位でのバランスや特殊なゴーグルを用いて目の動きを調べる検査、耳に冷風や温風を送り、内耳を刺激することでめまいを誘発する検査などを組み合わせて行います。
痛みや危険性はなく安全な検査ですが、めまいを誘発させるため気分不良が起きる場合もあります。
聴性定常反応(ASSR)検査
聴性定常反応(ASSR)検査は、耳から入った音に対する脳波を記録する聴力検査です。
ひたいと耳の裏に検査センサーを付けた後、イヤホンを装着させていただきます。
痛みや危険性はなく安全な検査で、妊娠中の方でも安心して受けていただくことができます。
検査時間は90〜120分程度です。
脳波検査
脳波検査とは、頭皮に電極をペーストを用いて装着します。脳波(脳が活動しているときに生じる非常に弱い電気活動を波形としてとらえたもの)を記録する検査です。
小児では睡眠状態の脳波記録が大切です。保護者のみなさんにもご協力いただくことがあります。
また、必要に応じて深呼吸をして頂いたり、目の前で光を点灯させて脳波の変化を観察することがあります。。
痛みや危険性はなく安全な検査で、妊娠中の方でも安心して受けていただくことができます。
検査時間は30~60分程度です。
神経伝導検査
神経伝導検査は、神経の伝わり方や筋肉の動きを調べる検査です。
電気刺激による多少の痛みは伴いますが、危険性はなく安全な検査で、妊娠中の方でも安心して受けていただくことができます。
検査時間は30~60分程度です。
視覚誘発電位検査

筋電図検査
筋電図検査は、「手や足に運動の低下」「筋力の低下」「やせ」「痛み」などの原因が神経によるものなのか筋肉によるものなのかを調べる筋肉の検査です。手や足に検査用の細い針を刺して、筋肉の活動を調べます。力を入れたときと安静にしたときの記録を行います。痛みを伴う検査ですが、危険性はなく安全な検査ですので、安心してお受けになってください。妊娠中の方も安心して受けて頂くことができます。また、心臓ペースメーカーに影響を与えることもありません。検査時間は検査内容によって異なりますが、30分から90分程度です。
下肢動脈精密検査
下肢に虚血症状がある場合に行う精密検査です。虚血症状とは間欠性跛行(歩くと脚が痛くなり、休むとまた歩ける)、安静時下肢疼痛、潰瘍、壊疽など様々です。原因(閉塞性動脈硬化症、バージャー病、血管炎、コレステロール塞栓症など)の検索および治療方針検討の一助となるよう、詳細な検査を行います。検査の内容は上腕と足首(足趾)の血圧測定、皮膚灌流圧測定(毛細血管の血圧)、経皮酸素分圧、血管超音波検査から選択します。これらの検査を組み合わせることにより、血管の狭窄・閉塞病変の有無や部位の特定、潰瘍の治癒予測等が行えます。また、難治性潰瘍に対して実施しているCD34陽性細胞移植による血管再生治療(臨床試験)の適格性や経過観察にも利用されています。複数の検査を同日に行いますので、所要時間は2時間以上となります。
検査室タイムズ“TEKARI”
”TEKARI” 名前の由来
「てかり」とは、布地の一部がこすれて光っていること、皮脂の分泌で額や頬がてかてか光って見えること等をいいます。「てかってるー!」って、言われるとあまりいい気持ちにはなれません。だいたい「てかり」は、避けられている言葉です。しかしながら、脂汗をかきながら頑張る姿にてかりがあって、一生懸命生きている証の一つが「てかり」とも言えます。
我ら検査部が日々切磋琢磨しボロボロになりながらも頑張ってコツコツと築き上げた実績、それは決してきらびやかで華々しいスマートな輝きではありません。しかしながら、この輝きは技術者としての匠(たくみ)の精神や技を彷彿させる、いとおしく尊い輝きとして、“TEKARI(てかり)”と表現できるのではないかと考えました。
検査部自体が自ら光を放つことはありません。臨床からの依頼があってこそ、”きらり”と、輝ける部門です。臨床からの光を受けて、てかてかと輝き続けたいと思っております。
我らが検査部のそれぞれの部門の旬の話題の特集や、最新の検査部ニュースを “TEKARI(てかり)” として紹介します。定期的に更新してゆきますので、是非、覗いてみてください。
”TEKARI”最新号
輸血検査管理室
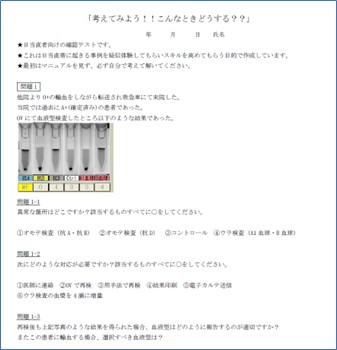
輸血を行なう際、一般的には血液型検査と不規則抗体検査を事前に実施し、患者さんの血液型に合わせた製剤を用意しますが、外傷や出産、大動脈解離などで危機的な大量出血を来した際、救命のために迅速に輸血を開始する必要があります。そのためにはマニュアルの策定や臨床との連携など、様々な事前準備が必要になります。今回は当院の超緊急輸血について詳しく解説していきます。
本題に入る前に、輸血検査室で管理している代表的な血液製剤について紹介します。
緊急輸血に使用する輸血や製剤の種類
《赤血球製剤(RBC)》

《血漿製剤(FFP)》

《血小板製剤(PC)》

《アルブミン製剤》

当院における超緊急輸血の紹介
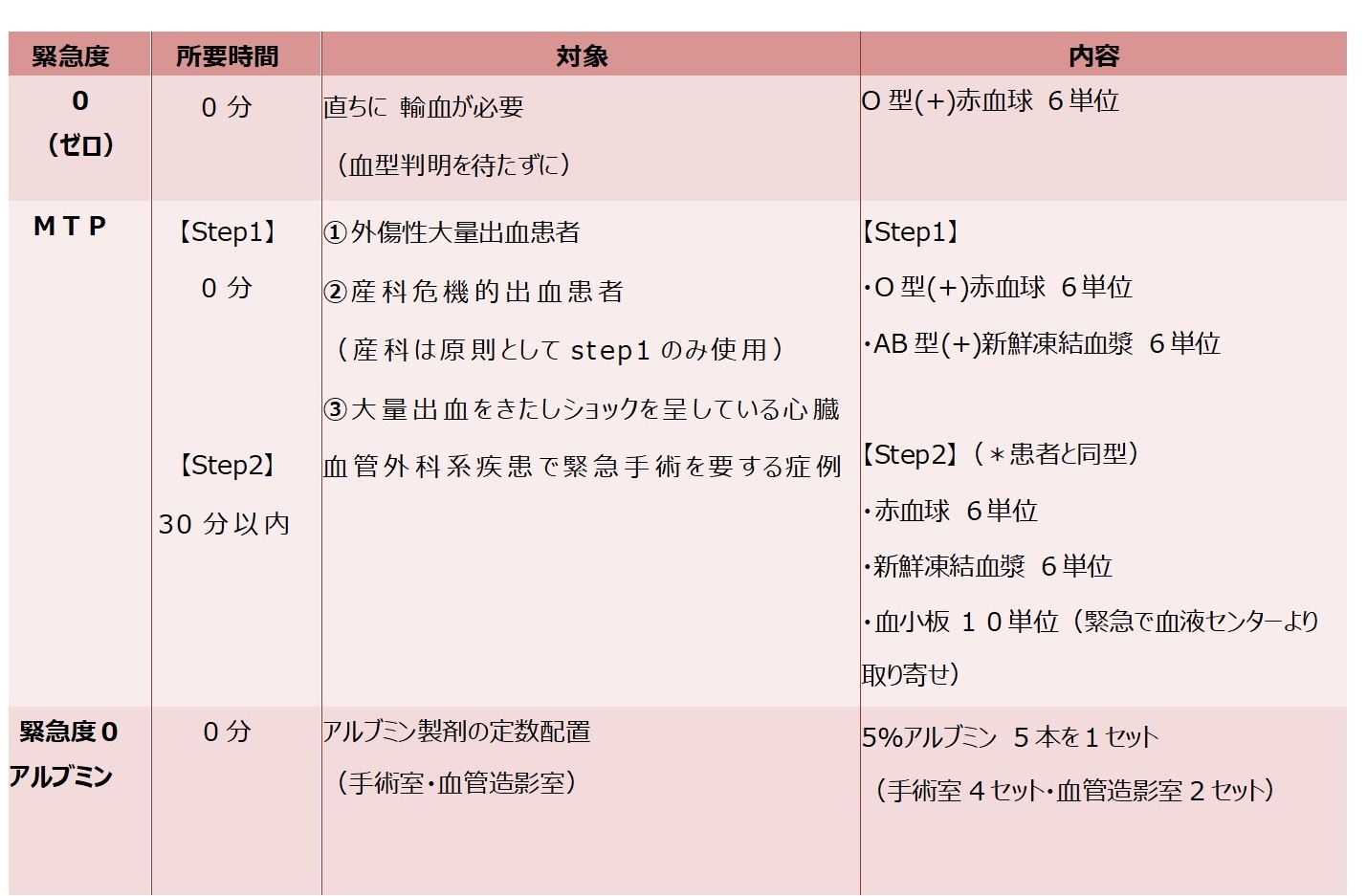
現在、当院で実施している超緊急輸血には、緊急度0(ゼロ)とMTP(Massive Transfusion Protocol )、そして緊急度0(ゼロ)アルブミンがあります。輸血を必要とする患者さんの状態を医師が判断し、輸血検査室と連携して救命のために迅速に輸血を実施できるように体制を常に整えています。
これらのO型赤血球やAB型新鮮凍結血漿を使用する超緊急輸血は、あくまで「出血性ショックのため血液型を判定している時間的余裕がない場合」、「血液型の判定が困難な場合」等の「例外的」な対応として救命のために実施されるもので、輸血過誤事例とは異なるものです。
参考文献:「輸血療法の実施に関する指針」厚生労働省医薬・生活衛生局血液対策課
http://www.mhlw.go.jp
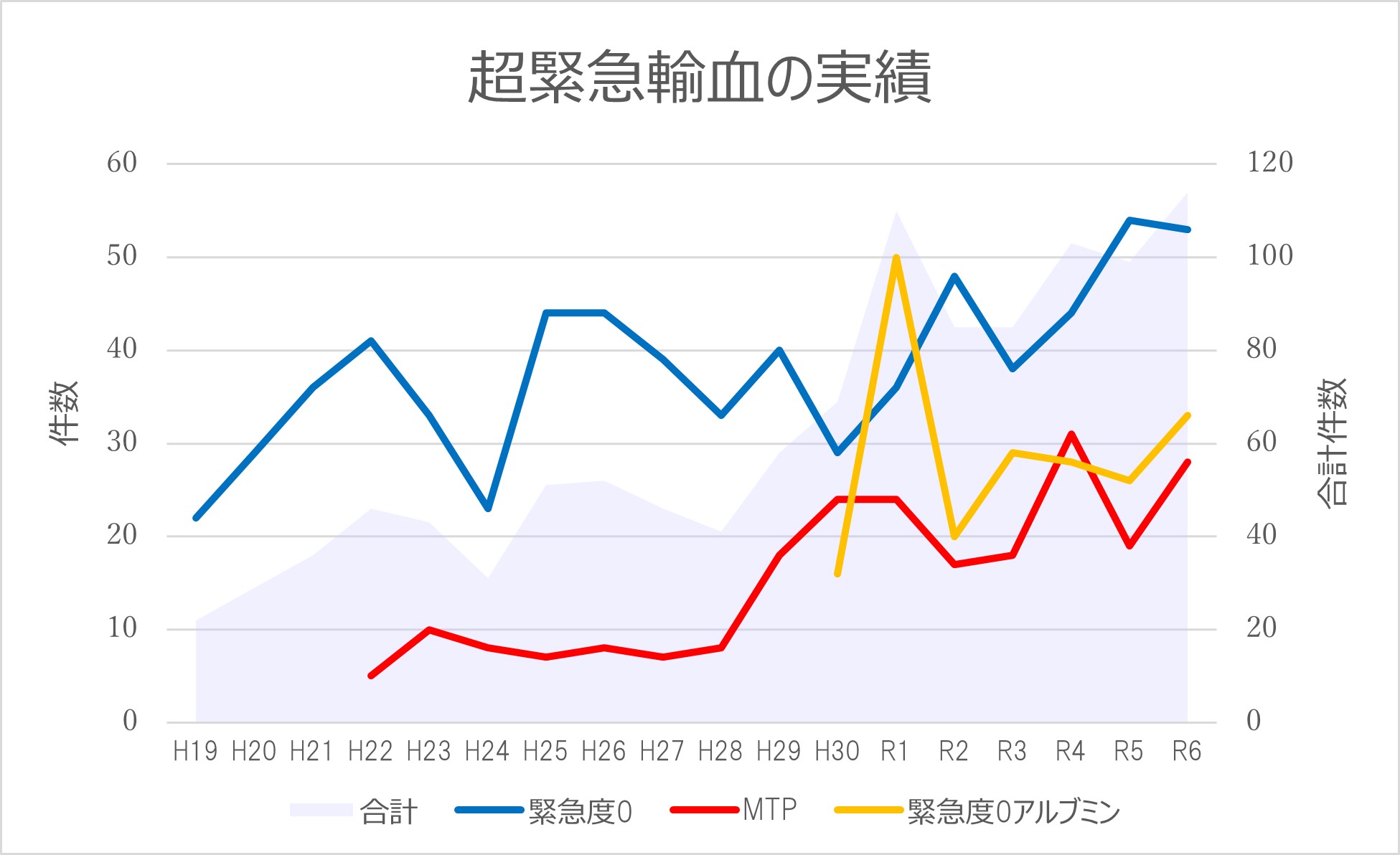
当院の超緊急輸血の実績
当院では3種類の超緊急輸血があり、その実績は以下の図のとおりです。
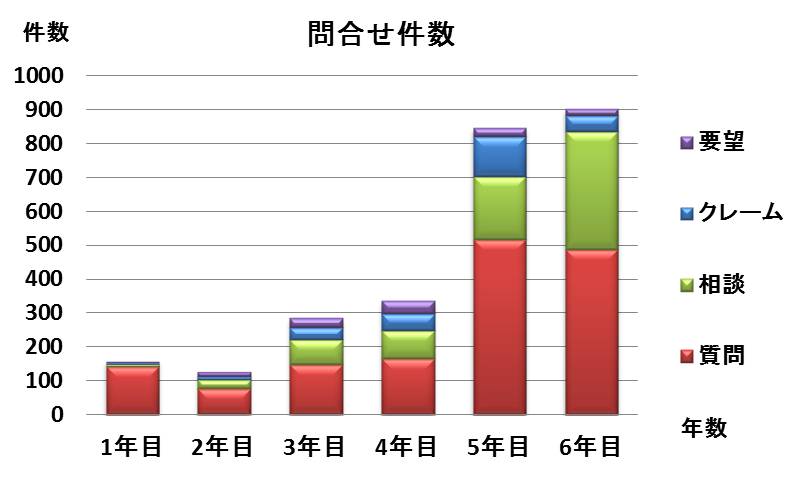
緊急度0は2007年、MTPは2010年、緊急度0アルブミンは2018年に運用開始しており、年々その数は増加傾向にあります。一定数のオーダーがある事により、定期的なシミュレーションを実施しなくても、スムーズに運用できるのが当院の特徴です。
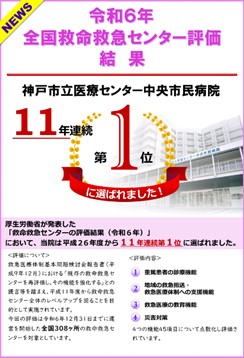
当院の救急救命の評価と検査部の取り組み
令和7年4月15日に厚生労働省から発表された「救急救命センターの評価結果(令和6年度)」において、当院の救急救命センターが、全国308の施設中、第1位の評価を獲得いたしました。今年で11年連続第1位に選出されております。
評価内容については、①重篤患者の診療機能、②地域の救急搬送・救急医療体制への支援機能、③救急医療の教育機能、④災害対策の4つの機能45項目について点数化し評価されています。
当院では「1年365日・24時間断らない救急医療」という理念のもと、安全で安心な医療の提供に努めており、神戸市民の「最後の砦」としての役割を果たしています。
この役割を実現するためにも、臨床検査技術部では救急患者が病院に到着後、迅速な検査や輸血用製剤の提供ができる体制を構築しています。患者さんから採取した検体はトレイ搬送システムを使用し、採取から検査までの時間を短縮しております。また、豊富に輸血用製剤を常備しているため、緊急で大量輸血が必要な患者さんへの対応も可能です。さらに輸血検査は臨床検査技師が24時間体制で実施しています。
上記の取り組みを始め、職員の教育やシステムの改善を行うなど、今後もより良い救急医療の提供に努めてまいります。
当院の教育体制
当院の臨床検査技術部は、検査室の国際規格であるISO15189を取得しています。
最後の砦として断らない救急を掲げ、365日・24時間体制で輸血検査や輸血製剤の準備を行っていることから、輸血検査に携わるすべてのスタッフは、教育を受け、高水準のスキルを常に維持する必要があります。
当輸血検査室では、日当直の臨床検査技師に対してのみでなく、救急医療に携わる医師に対しても教育体制を整え、以下のような形でスキルチェックを実施しています。

(臨床検査技師)》
この体制を維持・継続することで、緊急輸血時にもあわてることなく迅速で的確な対応が可能となります。
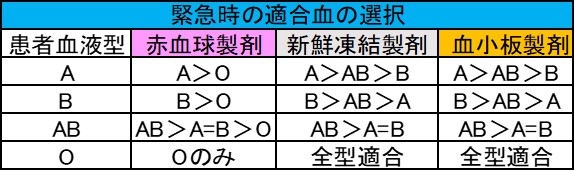
異型輸血に関するガイドライン
通常の輸血では患者さんの血液型と同型の製剤を輸血しますが、緊急の場合や、同型の製剤の供給に時間を有する場合は、異型適合輸血を行うことがあります。異型適合血を選択するときの血液型優先順位は下の表のとおりになっており、当院でもこの基準に従ってマニュアルを整備し、輸血を行うことがあります。
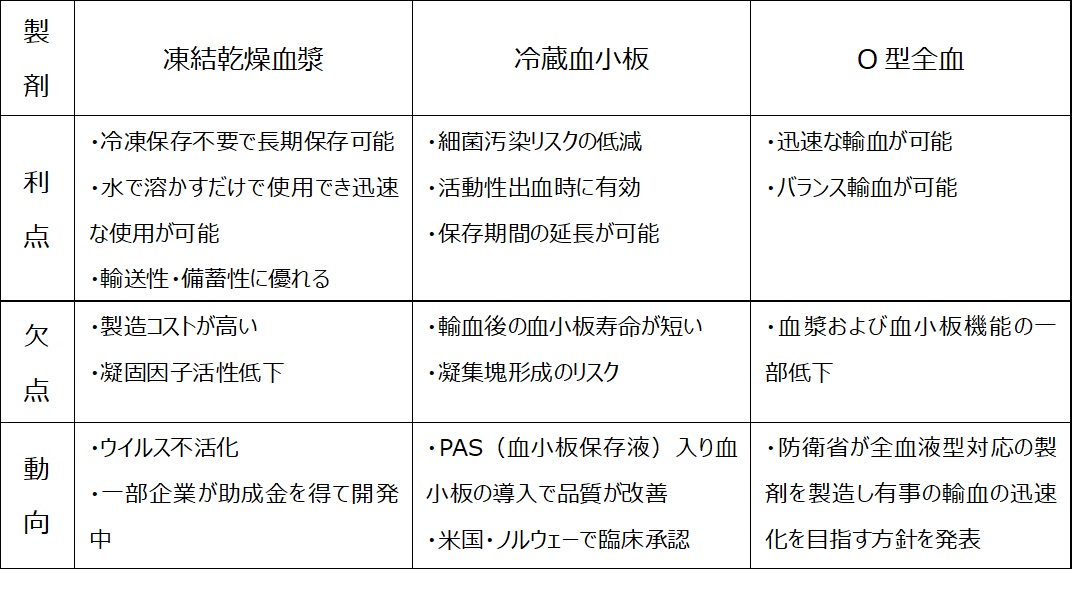
次世代に期待される製剤
緊急時の輸血では、患者さんの命を守るために迅速な対応が求められます。しかし、新鮮凍結血漿は使用できるまでに解凍の時間がかかり、血小板は保存期限が短いため院内に在庫がありません。そのため、必要な時にすぐに準備をするのが難しい場合があります。こうした問題を解決するため、次世代の血液製剤として「凍結乾燥血漿」「冷蔵保存血小板」「O型全血」などの開発や検討が進められています。以下、それぞれの製剤の特徴を紹介します。
これらの新しい血液製剤は現在日本では未承認ですが、緊急時にも安全かつ迅速な輸血治療を可能にする次世代製剤として期待されています。
”TEKARI”バックナンバー
生化学検査室 坪井 剛史
「正しい検査結果」を支える見えない工夫について
はじめに
体調が悪くて病院を受診したとき、健康診断を受けたとき、あるいは献血をしたときなど、採血をされた経験がある方は多いと思います。
血液検査には様々な項目があります。たとえば、肝臓の働きを調べるASTやALT、血糖値やHbA1c(ヘモグロビンA1c)、中性脂肪やコレステロールなどの脂質項目など、馴染みがある項目ではないでしょうか。
これらの検査結果は、病気の診断や治療方針を決めるうえで不可欠なため、検査結果は「正しい」ものでなければなりません。その「正しい検査結果」は、どのようにして得られているのかその取り組みを紹介します。
■ 検査結果の「正しさ」とは?
まず大前提として、機械で数値を測る「定量的検査」では、本当の正解(真の値)を誰も知ることはできません。なぜなら、検査は毎回まったく同じ条件で検査を行うことが不可能だからです。
たとえば、検査を実施する部屋の室温や湿度、機械の状態、使う試薬など、検査に関わるさまざまな要素は日々変化するため、どうしても検査結果にはわずかなばらつきが生じてしまいます。
そこで私たち臨床検査技師が行っているのは、「この検査結果はどれくらい信頼できるか?」を確認し、その信頼性を高めることで、「信頼できる結果」を報告できるようにしています。
このように、普段目にする検査結果の裏側では、見えないところで多くの工夫と努力が積み重ねられています。少しでもその背景を知っていただけたら嬉しいです。
■検査結果の信頼性とは?
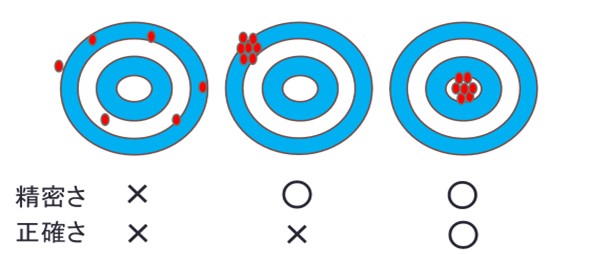
検査結果の信頼性は「精密さ」と「正確さ」の2つの要素で決定されます。
「精密さ」は値のばらつきの程度であり、「正確さ」は値のかたよりの程度を表します。
ここでは、的(ターゲット)を使って検査結果の信頼性をイメージとして説明します。
・左の的:同じ検体(試料)を何度も測定しても、結果がバラバラ。これは、検査結果に一貫性がなく、信頼性が低い状態です。(検査結果を報告できない状態)
・真ん中の的:結果は毎回ほぼ同じですが、的の中心から大きくズレています。つまり、安定しているけれど、間違った値を出している状態です。(検査結果を報告できない状態)
・右の的:いつ、誰が、何度測定しても、結果がほぼ同じで、しかも中心に近い。これが信頼性の高い検査結果です。(検査結果を報告できる状態)
■信頼できる検査結果を得るための「精度管理」とは?
右の的のような信頼性の高い検査結果を得るために行われるのが「精度管理」という取り組みです。
検査は毎日、同じ条件で行うことはできません。室温や湿度、機器の状態、使う薬品などが少しずつ変わるため、どうしても結果にばらつきが出てしまいます。
このばらつきをデータとして記録・分析し、管理することで、検査結果の信頼性を高めるのが精度管理です。
病院や検査機関では、血液や尿などの検査結果が正確であることがとても重要で、毎日同じ条件で検査ができないため、検査の「ばらつき(誤差)」を管理する仕組みがあります。
その仕組みである「内部精度管理」は自分の検査室の中での安定性を確認する方法であり、「外部精度管理」は他の検査室と比べてズレがないかを確認する方法です。
1. 内部精度管理
検査室の中で行う管理方法です。同じ検査室の中で、検査結果にどれくらいのばらつきがあるかをチェックしています。これは、同じ場所・同じ機器・同じ人が検査をしたときに、結果が安定しているかを確認するものです。
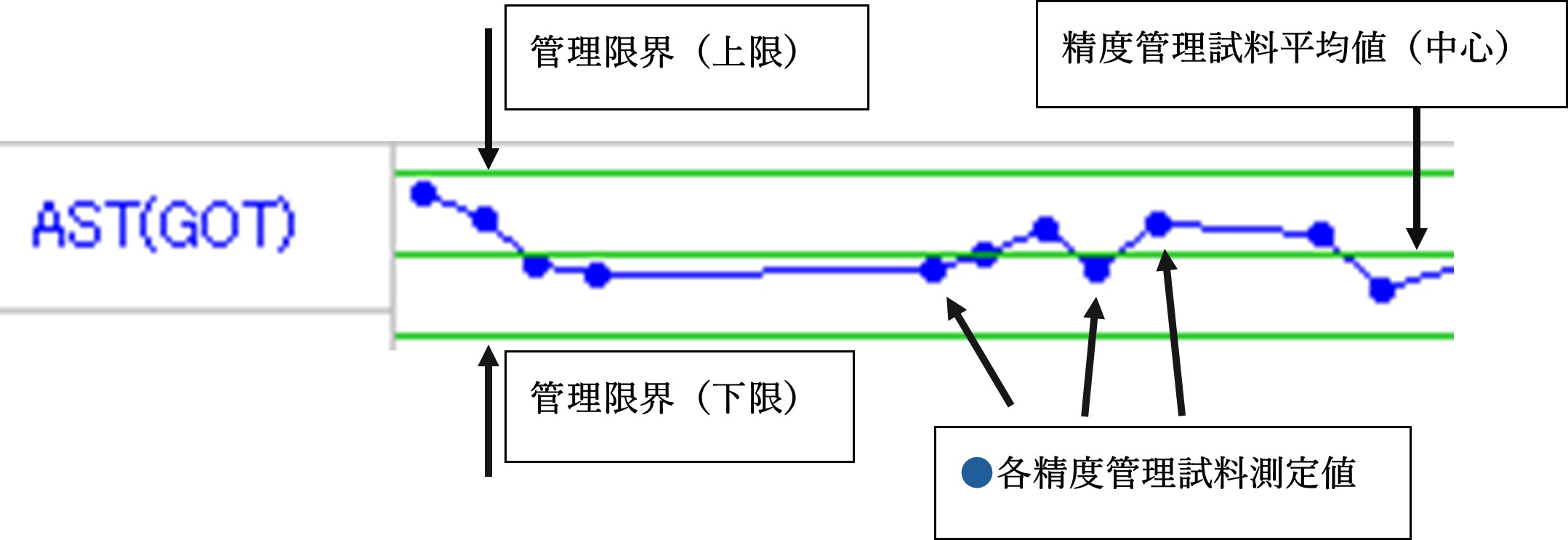
具体的には、あらかじめ値がわかっている試料、「精度管理試料」と呼ばれるものを使って、何度も測定を行います。その結果を統計的に分析し、「平均値」やこの値を超えると報告できないという目安である、「管理限界」を設定します。
そして、患者さんの検査を行う前後や、機器のメンテナンス後などに精度管理試料を測定し、結果が管理限界内にあるかを確認します。これにより、日々の検査が安定して行われているかをチェックできるのです。
●検査結果の信頼性を守る「管理限界」とは?
検査室では、検査結果が正しいかどうかを判断するために「管理限界」という基準を使っています。
たとえば、下図のように、検査項目ASTにおける精度管理試料を測定し、その結果が管理限界内にある場合は、「検査機器や測定方法に問題はない」と判断します。つまり、その状態で測定された患者さんの検査結果も信頼できる=正しい結果と考えられるのです。
●異常があった場合はどうするの?
もし精度管理試料の測定結果が管理限界を超えてしまった場合は、すぐにその機器の使用を中止します。そして、何が原因で異常が起きたのかを調べ、必要な対応を行います。
これにより、何かしらの異常が発生している状態で患者さんの検査をしてしまうことを防ぎ、誤った結果が報告されないようにする役割を果たしています。
●異常が出る前の「予兆」も見逃さない
精度管理試料の測定結果がたとえ管理限界内に収まっていても、注意が必要な場合があります。
・シフト現象:結果が急に中心からズレたまま続く状態
・トレンド現象:結果が少しずつ上がったり下がったりし続ける状態
こうした変化は、将来的に管理限界を超える可能性がある「予兆」としてとらえられます。検査室では、こうした傾向も見逃さず、早めに原因を調べて対応することで、検査ができなくなるといった問題が大きくなる前に防ぐよう努めています。
このように、検査室では日々の測定結果を細かくチェックし、異常が起きる前から対策を講じることで、常に信頼できる検査結果を提供できるようにしています。
しかし、これだけでは不十分です。なぜなら、病院や検査室ごとに環境も違うし、使っている機器や試薬が違うため、「検査室ごとの違い(ばらつき)」が生まれる可能性があるからです。
たとえば、同じ患者さんの血液を同じタイミングで検査したのに、A病院では「正常」と出て、B病院では「異常」と出ることもありえます。これは、検査室ごとの違いが原因かもしれません。
そこで登場するのが「外部精度管理」です。
2.外部精度管理
複数の検査室で同じ試料(検体)を検査して、その結果を集めて比較する方法です。
この比較には「SDI(標準偏差指数)」という数値を使います。SDIは、「あなたの検査結果が、全体の平均と比べてどれくらいズレているか」を示すものです。
このSDIの値を見れば、自分の検査室の結果が他の施設と比べてズレていないかがわかります。もしズレが大きければ、その原因を調べて、検査方法や機器の調整などを行い、精度を改善します。
■「検査結果」の裏側にある、見えない努力
病院などで受け取る「検査結果」は、一見するとただの数字や判定のように見えるかもしれません。ですが、その結果が正しく、信頼できるものであるために、検査室では日々さまざまな取り組みが行われています。
検査の精度を保つためには、統計学の知識や専門的な技術が必要です。さらに、検査結果がばらつく原因はとても多く、検査室の環境、機器の状態、試薬の違いなど、さまざまな要素が関係しています。そのため、もし異常な結果が出た場合には、原因を突き止めるのに時間がかかることもあります。
それでも、全国の検査室では「私たちが出した検査結果こそが正しい」と胸を張って言えるように、日々努力を重ねています。精度管理という仕組みを使って、検査の信頼性を高める工夫を続けているのです。
今回の説明を通して、普段は見えない検査の裏側に少しでも興味を持っていただけたら嬉しいです。検査結果の「正しさ」は、こうした地道な取り組みによって支えられています。
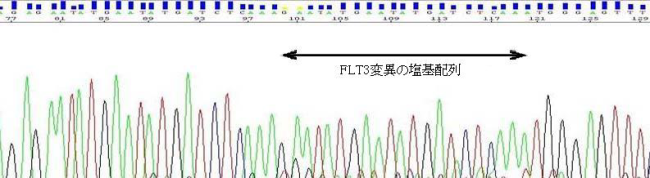
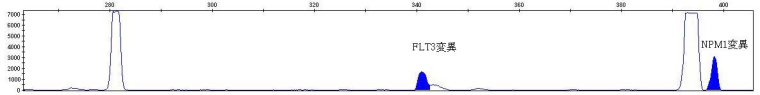
遺伝子検査:FLT3変異とNPM1変異”について
遺伝子検査:FLT3変異とNPM1変異”について
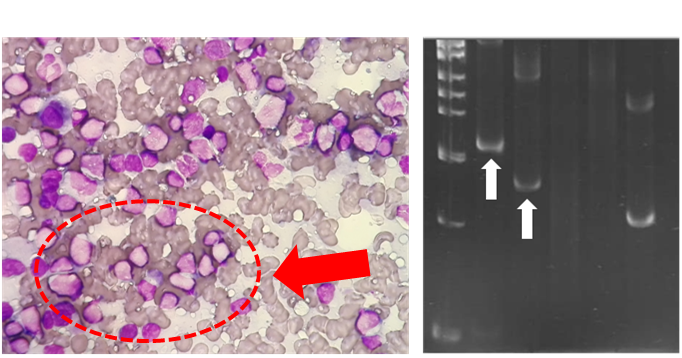
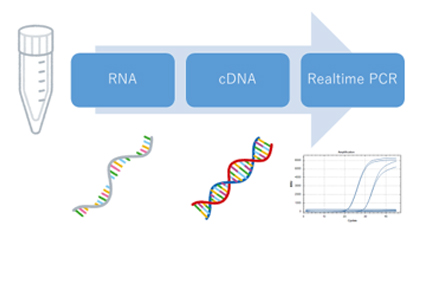
細胞遺伝子検査室では、フローサイトメトリー*1という手法を用いた細胞レベルの検査とPCR*2という手法を用いた遺伝子レベルの検査を実施しており、主に白血病や悪性リンパ腫などの血液腫瘍に関連する検査を担当しています。この10年間で血液腫瘍の分野における研究は目覚ましいものがあり、診断および治療は飛躍的な進歩を遂げました。白血病の確定診断において、今や遺伝子検査は不可欠なものとなっており、詳細な病型の分類に用いられています。そして、得られた検査結果は各病型に最適な治療方針を決定することに役立てられています。
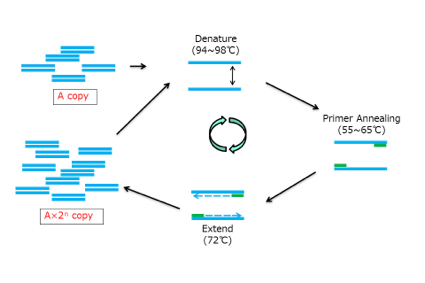
タイトルにある“FLT3変異とNPM1変異” *3は、急性骨髄性白血病との関連で注目されている遺伝子異常です。PCRという手法を用いて、急性骨髄性白血病の診断時における”FLT3変異とNPM1変異”の有無を検査することにより、化学療法に対する治療効果の予測をすることが可能となり、治療方針を決定する上で重要な情報を主治医に提供することができます。また、遺伝子異常が発見された場合は、遺伝子の詳細なパターン解析を行い、個々の患者さん毎に最適な検査方法を構築することで、微小残存病変*4 を検出することが可能となり、治療効果を正確に判定することができます。
現時点で”FLT3変異とNPM1変異”を検査することのできる医療機関は限られています。当検査室では全国に先駆けて2008年より検査を開始しており、100例以上の実績があります。今回ご紹介した検査のみならず、臨床医と密な連携を取りながら、常に最新かつ最良な検査方法の導入や新規開発に積極的に取り組み、得られた成果は国内外に発信していきたいと考えています。
*1:フローサイトメトリー
フローサイトメーターという機器と特殊な試薬を用いて、特定の細胞におけるタンパク質の有無を網羅的に測定し、細胞の特徴を解析する手法
*2:PCR
サーマルサイクラーという機器と特殊な試薬を用いて、極わずかな量の遺伝子を増幅させ、遺伝子異常の有無などを解析する手法
*3:FLT3変異とNPM1変異
FLT3変異とNPM1変異は急性骨髄性白血病の予後を予測する因子として注目されている。WHO分類第4版では遺伝子変異を伴う急性骨髄性白血病が独立した病型として設けられており、その中のひとつにNPM1変異が含まれている。一方、FLT3変異については一病型として定義されていないが、診断時に変異解析を行うことが推奨されている。
*4:微小残存病変
顕微鏡では発見できない極少数の白血病細胞の残存状態
検査部ニュース
新規検査項目
*平成23年11月 院内実施化となった検査項目
- グリコアルブミン
- マグネシウム
学術関係報告
論文発表
- 竹川 啓史:
真菌同定の実際 Ⅱ 糸状菌 Mucor,Rhizopus, Rhizomucor, Absidia, Cunninghamella, Syncephallastrum
臨床と微生物 38;551-557.2011.論文
発表・講演等 平成23年7月~12月
- 平成23年7月9日
京都府臨床検査技師会生理検査分野研修会 腹部超音波検査 ハンズオン&レクチャーコース
講師:岩崎 信広 「消化管―腫瘍性病変」 - 平成23年7月23日
日本消化器がん検診学会 近畿支部超音波部会 第12回 総会・学術集会
教育講演:岩崎 信広 「USと血流」 - 平成23年6月25日
第111回日本循環器学会地方会 研修医のための教育セッション
ハンズオン講師:紺田 利子 - 平成23年8月20日
和歌山県臨床検査技師会 生理検査分野研修会
教育講演:岩崎 信広 「ステップアップ消化管超音波」 - 平成23年9月20日
第111回 兵庫県臨床検査技師会 微生物検査研修会
講師:竹川 啓史 「シリーズ:真菌検査② ~マスターしよう真菌検査法~」 - 平成23年9月17日
消化管エコーライブセミナー
講師:岩崎 信広 「ステップアップ消化管超音波検査 -症例から学ぶ診断への道標-」 - 平成23年9月25日
兵庫県臨床検査技師会 腹部超音波実技講習会
講師:岩崎 信広 「装置の設定と検査における注意点、肝臓の解剖と生理」 - 平成23年10月9日
兵庫県臨床検査技師会 腹部超音波実技講習会
講師:岩崎 信広 「胆道系の解剖と生理」 - 平成23年10月16日
兵庫県臨床検査技師会 腹部超音波実技講習会
講師:岩崎 信広 「膵臓の解剖と生理」 - 平成23年10月23日
兵庫県臨床検査技師会 腹部超音波実技講習会
講師:岩崎 信広 「腎臓の解剖と生理」 - 平成23年10月15日
先端医療財団 CAS-CARE超音波検査講習会
講師:佐々木 一朗 - 平成23年10月29日
Echo Heart Izumo 2011
講演と実技指導:紺田 利子 「不明熱の精査」 - 平成23年10月29日
Echo Heart Izumo 2011
講演と実技指導:川井 順一 「胸痛の精査」 - 平成23年11月6日
兵庫県臨床検査技師会 丹但地区学術研究会
講師:岩崎 信広 「消化管腫瘍性病変の超音波診断」 - 平成23年11月13日
日本超音波医学会 第38回関西地方会学術集会
発表:岩崎 信広 「ドプラ検査が有用であった大腸angioectasiaの一例」 - 平成23年11月13日
日本超音波医学会 第38回関西地方会学術集会
発表:岩崎 信広 「リンパ管腫内出血の一例」 - 平成23年11月17日
第170回大阪腹部超音波研究会
発表:岩崎 信広 「消化管疾患の造影超音波検査 当院における現況」 - 平成23年11月27日
消化管エコーハンズオンセミナー
講師:岩崎 信広 - 平成23年11月13日
日本超音波医学会 第38回関西地方会学術集会
発表:竹林 真美子 「スクリーニング検査で発見された膵腫瘍の一例」 - 平成23年11月17日
第170回大阪腹部超音波研究会
発表:竹林 真美子 「スクリーニング検査で発見された膵腫瘍の一例」 - 平成23年11月5日
第17回神戸臨床フォーラム
教育講演:丸岡 隼人 「血液腫瘍診断におけるflow cytometryおよび遺伝子検査」 - 平成23年11月19日
第58回日本臨床検査医学会学術集会
発表:丸岡 隼人 「6-color flow cytometryを用いた成熟リンパ系腫瘍のimmunophenotyping」 - 平成23年12月7日
救急オープンセミナー
講師:岩崎 信広 「急性腹症における超音波検査」 - 平成23年12月21日
救急オープンセミナー
講師:佐々木 一郎 「救急医療における脳死対応セミナー」 - 平成23年12月18日
第111回超音波検査学会医用超音波講義講習会
講師:岩崎 信広 「急性腹症における超音波検査の進め方」
造影超音波検査の進歩
生理機能検査室 岩崎 信広
造影超音波検査
腫瘤性病変の血流動態的評価は診断や治療方針の決定においてきわめて重要である。超音波を用いた血流動態の評価法として、従来よりカラードプラ検査が用いられているが、血球からの反射音波のみを利用しているため、反射音波が弱ければ感度が低下する。しかし、造影超音波検査は造影剤が強い反射源となるため、より高感度に血流動態を評価することが可能である。
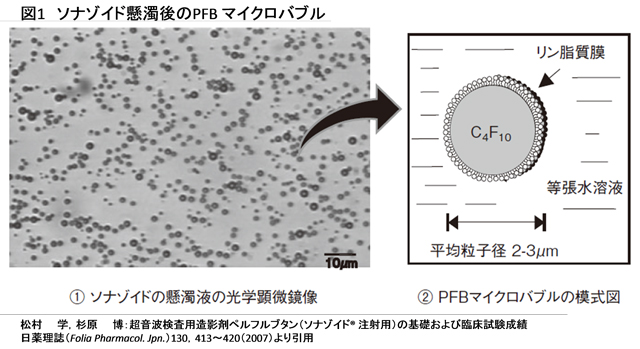
超音波用造影剤:SonazoidⓇ
SonazoidⓇは肝腫瘤性疾患の診断を目的とした超音波造影剤である。この造影剤は化学的に安定なガスであるペルフルブタン(PFB;図1)を内包させた製剤で、投与後は呼気中に排泄される。2007年1月の販売開始後5年が経過しているが重篤な副作用はほとんど報告されていない。CT検査・MRI検査など他の造影剤を用いる画像診断法では一定の割合で重篤な副作用があり、造影剤に対して過敏症が有る場合は施行できないが、造影超音波検査はこれらの患者様においても施行が可能であり、肝腫瘤性疾患における唯一の血流動態的診断法となる場合がある。
当院における造影超音波検査の現況
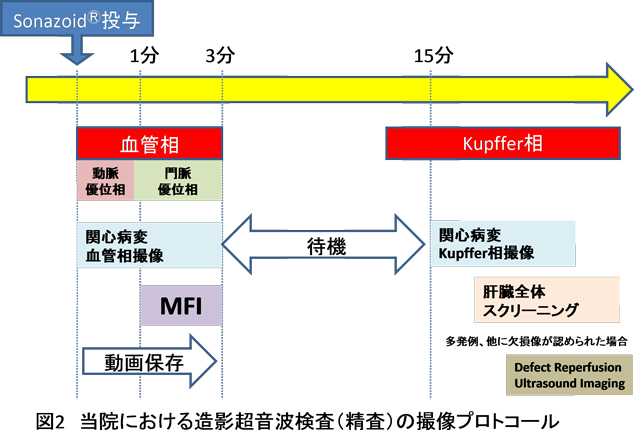
造影超音波検査は造影モードの搭載された専用機器が必要である。腹部超音波検査室にはハイエンド超音波検査診断装置*1が6台配置されており、造影剤販売当初から積極的に取り組んできている。また、検査には高度な技術と知識が必要とされるが、精通した複数の技師が常任し臨床からの様々な要望に対応している。当院では造影超音波検査をスクリーニング造影検査と精査造影検査に区分し実施している。スクリーニング造影検査は腫瘤の存在診断を主たる目的としている。造影剤の投与は外来中央処置室で行い、その後、超音波検査室に移動してKupffer相*2(post vascular phase)における欠損像の有無について観察している。一方、精査造影検査は主に腫瘤の質的あるいは鑑別診断を目的としている。造影剤投与直後の血管相*3(vascular phase)およびKupffer相の観察を行うため、造影剤投与から検査終了まですべてを腹部超音波検査室内で行っている。さらに、多発性に腫瘤が認められる症例や他部位に新たに欠損像が認められた場合、病変部血管相の評価のため、造影剤を再投与し工藤ら1)の提唱した「Defect Reperfusion Ultrasound Imaging*4」を行っている(図2)。したがって、スクリーニング造影検査に比べ、検査時間が1時間程度必要になる場合もあり、午後から1人/1時間の予約枠で施行している。また、肝細胞癌の治療ではラジオ波焼灼治療*5(Radiofreequency Ablation:RFA)時に病変部が認識困難な場合、「Defect Reperfusion Ultrasound Imaging」を用いて、安全かつ的確にRFAが施行できるよう治療支援として積極的に施行している。
*1 ハイエンド超音波診断装置:最新の技術を採用し、高機能・高性能を追求した超音波診断装置。
*2 Kupffer相:造影剤(マイクロバブル)の一部は細網内皮系(肝臓ではKupffer細胞)に取り込まれる。Kupffer細胞を有さない腫瘍は造影されず、腫瘍と正常肝組織のコントラストの差が明瞭化し、腫瘍の存在診断が可能となる造影剤投与後5~10 分以降の時相。
*3 血管相:肝腫瘤性病変内、辺縁及びその周辺の血管を造影することができる造影剤投与直後から3分までの時相。
*4 通常の超音波検査で検出不能の結節をKupffer相で欠損像(Defect)として検出した後、造影剤を再投与しDefectを呈した結節が動脈血流を有するか否か再灌流(Reperfusion)を判定する手法。
*5 ラジオ波焼灼治療:超音波ガイド下に電極針を体外から病変部まで穿刺し、ラジオ波を通電することにより発生する高熱で病変部を凝固壊死させる治療法。
造影超音波検査の応用
現在、造影超音波検査は肝腫瘤性疾患の診断だけでなく、治療支援として肝癌の局所治療の穿刺ガイドや治療評価にも応用されるようになってきた(研究レベルでは造影剤を加熱作用増強剤としてマイクロバブルを用いた強力集束超音波治療法(HIFU)の検討も行われている)。また、肝切除においては術中造影超音波検査も広がってきている。術中造影では肝臓に直接プローブをあてることができるため、より詳細な観察が可能となり、体外からでは検出できない小さな病変も検出できる。したがって、切除範囲など術式の決定や変更における有用な指標となっている。
症例
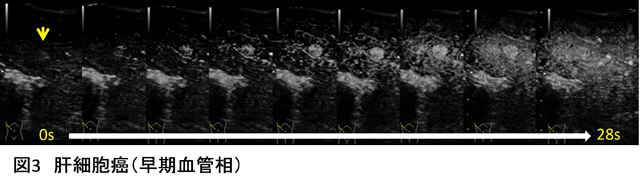
1. 肝細胞癌:早期血管相(図3)
肝S6に1㎝大の内部不均一な高エコー腫瘤(矢印)が認められる。造影剤投与10秒後から腫瘤全体が濃染している。
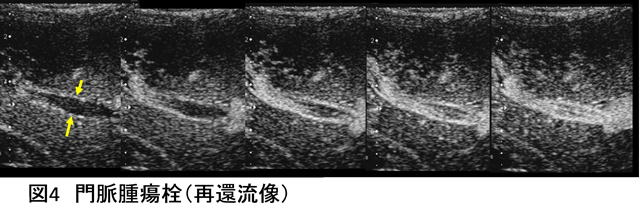
2. 門脈腫瘍塞栓:再還流像(MFI)(図4)
門脈(P6)内に淡い充実性エコーが認められる(矢印)。MFIで内部を走行する腫瘍内血管が明瞭に描出されている。
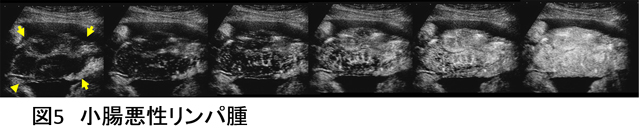
3. 小腸悪性リンパ腫:血管相(図5)
回腸に限局性の壁肥厚を認め、層構造は不明瞭化している(矢印)。早期濃染および腫瘍内を樹枝状に走行する血管構築が捉えられている。
4. 転移性肝癌:Kupffer相(図6)
肝S6に1.5㎝大の明瞭な欠損像が捉えられている(矢印)。
結語
当院では造影超音波検査の導入により、肝腫瘤性疾患における診断能が飛躍的に向上した。また、肝癌の治療支援における役割も大きく、今後は術者の育成をはじめ検査・治療体制を更に充実させていきたいと考えている。
1) Kudo M,Hatanaka K,Maekawa K:Newly developed novel ultrasound technique, defect reperfusion ultrasound imaging, using sonazoid in the management of hepatocellular carcinoma.Oncology, 2010 Jul;78 Suppl 1:40-5. Epub 2010 Jul 8.
検査部ニュース
新規検査項目
*平成24年4月 院内実施化となった検査項目
- 抗サイログロブリン抗体(Tg-Ab)
- 抗甲状腺ペルオキシダーゼ抗体(TPO-Ab)
学術関係報告
発表・講演等 平成24年1月~3月
- 杤尾人司、他:
アルコール禁患者におけるクロルヘキシジングルコン酸塩による静脈採血時の適正な消毒時間:採血シミュレーションを加えた細菌学的検討
医学検査Vol.61:374-379, 2012
発表・講演等 平成23年7月~12月
- 平成24年2月24日
第21回 腹部エコー実技講習会 「下肢静脈エコー」
講義:簑輪 和士 実技:黒田・浜田一・荒木・三羽
参加医師数18名 - 平成24年2月25日
兵庫県技師会腹部超音波実技講習会 「消化管エコー」
実技:簑輪 和士・岩崎 信広 - 平成24年3月3日 場所 京都テルサ
第5回 脳波・筋電図セミナー 講師
佐々木 一郎 : 「法的脳死判定」 - 平成24年3月15日 場所 中央市民病院 講堂
第109回 腹部超音波カンファレンス 発表
「消化管疾患診断のためのフローチャートを考える」
岩崎 信広:「当院における消化管疾患診断のフローチャートについて」
竹林 真実子:「典型的な消化管疾患のUS診断フローチャート」
三羽 えり子:「消化管疾患診断フローチャートの問題点」 - 平成24年3月24日 場所 但馬地域地場産業振興センター
第 10 回北近畿 Heart Imaging 研究会 発表
川井 順一:「経食道心エコー法および3次元心エコー法による僧帽弁閉鎖不全症の評価」
微生物検査室の紹介
微生物検査室 仁木 真理恵
微生物とは、細菌、酵母、ウイルスなど肉眼では観察できない生物のことで、人が生きていく上で必要不可欠な存在です。微生物と聞くと何となく嫌なイメージを抱きがちですが、人の体内にも100兆個以上存在しており、これらを常在菌とよんでいます。例えば、腸の中で生息している大腸菌などの腸内細菌は、食べ物の消化を助けたり、新たに侵入してきた菌を排除したりして私たちの体を守ってくれています。しかし、免疫力が低下している人にとっては、これらの常在菌が感染症の原因菌(病原微生物)になることもあります。また、病原性大腸菌O-157やカンピロバクターなど、体内に入り人に害を与える微生物(病原微生物)もいます。微生物検査室ではこのような病原微生物の情報を主治医に提供しています。
微生物検査室の役割は大きく分けて4つあります
①一般細菌検査
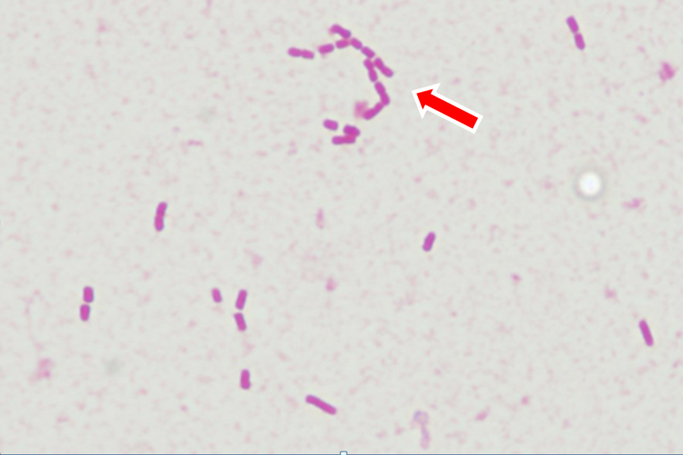
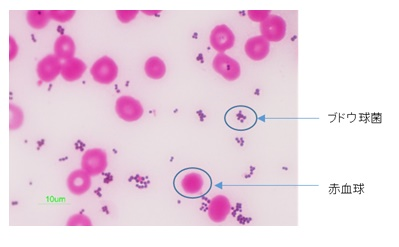
喀痰、尿、膿、血液など患者さんの検体を用いて病原微生物の有無を検査しています。まず、提出していただいた検体をスライドガラスに塗りグラム染色*1を行います。グラム染色により、濃紫色に染まるグラム陽性菌とピンク色に染まるグラム陰性菌に分けられます。これらを顕微鏡で観察し、染色された色や細菌の形態等から菌種の推測を行います。グラム染色は細菌の分類や同定をするうえで最も重要な工程になります。
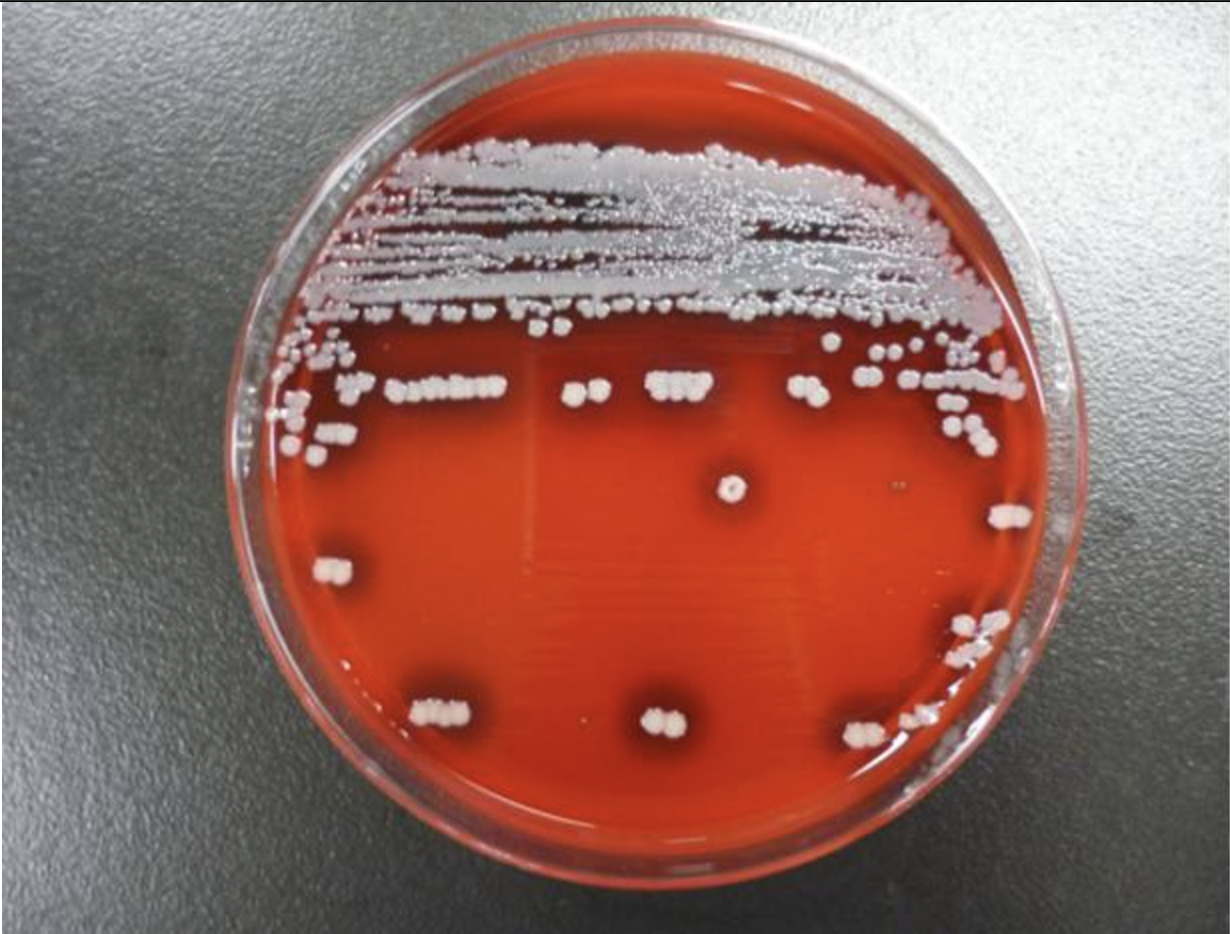
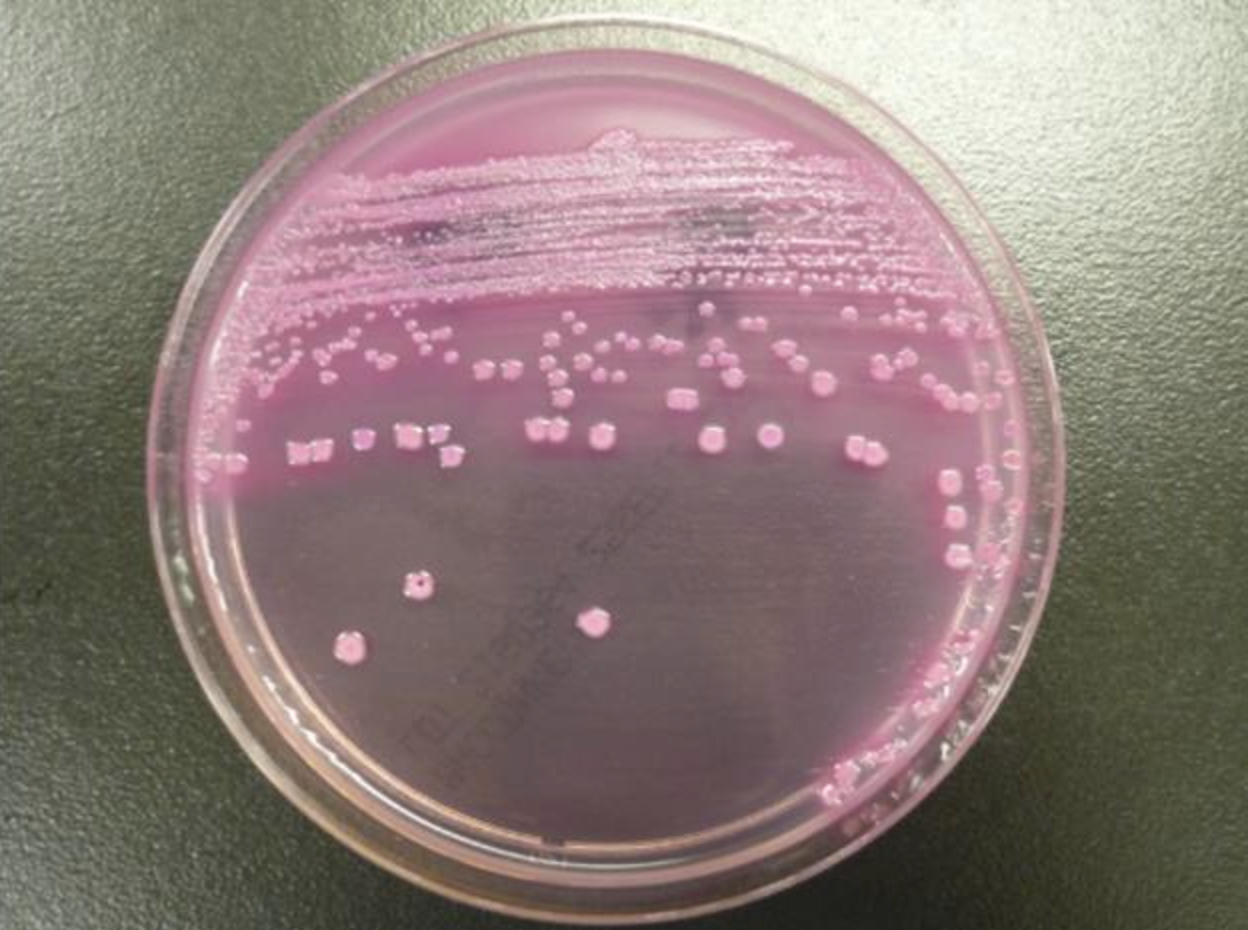
次に、検体を数種類の培地に塗布し、ふ卵器で培養させます。一晩培養させると、肉眼では見ることができなかった細菌が培地上で発育し、増殖して集落(コロニー)を形成し、目に見える大きさになります。数種類の培地に塗布することで、培地による発育の有無や集落の色、形状からある程度の菌名が推測できます。
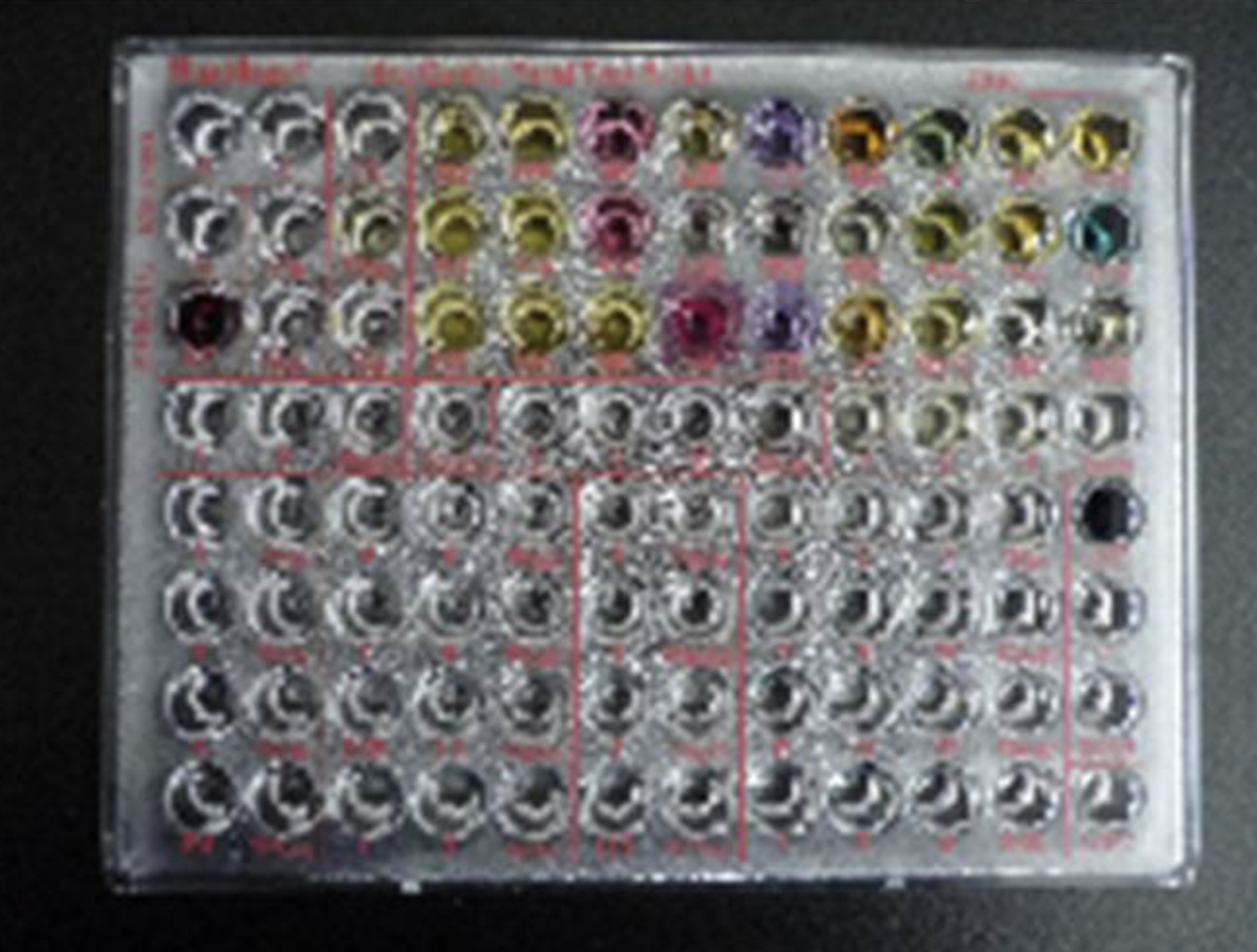
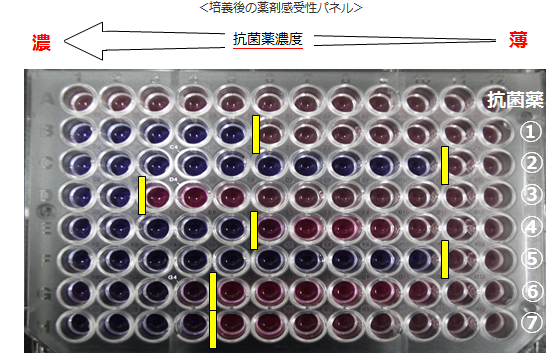
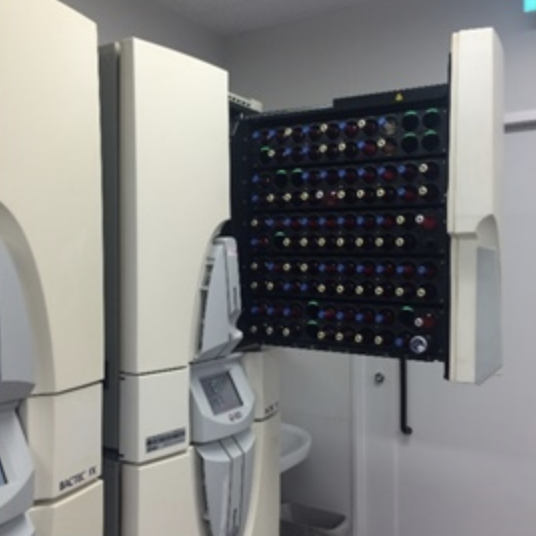
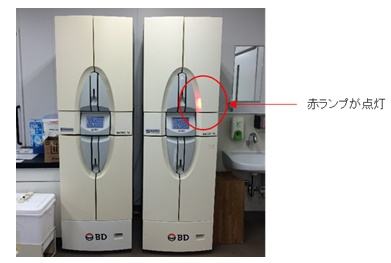
集落が形成されるとその細菌の同定と薬剤感受性検査を行います。同定検査ではブドウ糖や乳糖を分解できるかなど、細菌が持っている性質を調べることにより細菌の種類を決定します。一方、薬剤感受性検査では患者さんの検体から検出された病原微生物に効く薬剤を調べています。同定と薬剤感受性検査は一部の菌を除いて写真のような同定パネルを用いて全自動細菌分析装置により行っています。
②迅速抗原検査
便や尿中に排泄される病原菌の抗原*2を調べることで、病原菌の有無について迅速な報告が可能となっています。通常の培養検査による細菌の検出は2日以上かかりますが、迅速抗原検査の場合は15~30分以内に結果を報告することができます。当院では、インフルエンザウイルス抗原検査、便中ロタウイルス抗原検査、咽頭粘液アデノウイルス検査、尿中肺炎球菌抗原検査、尿中レジオネラ抗原検査などを行っています。
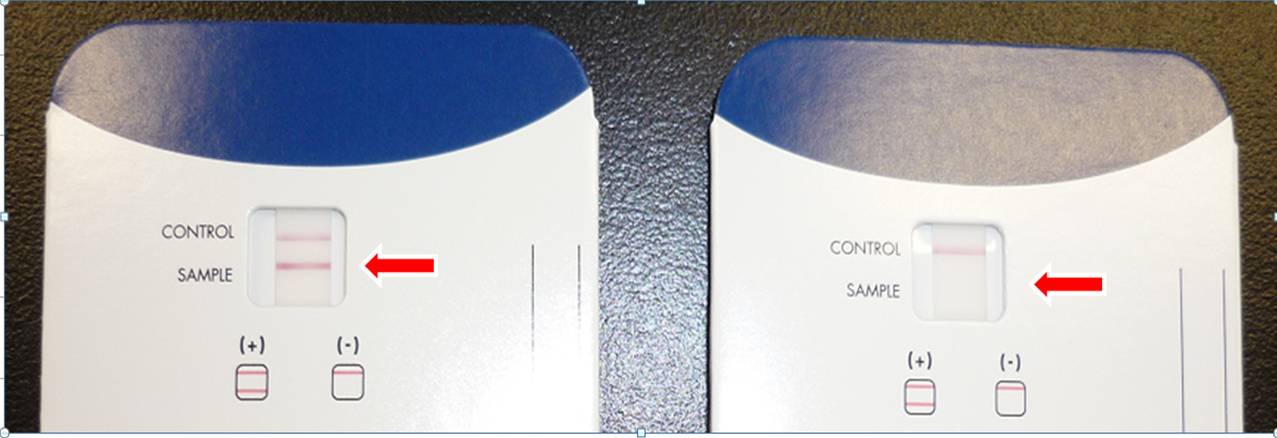
尿中肺炎球菌抗原検査:左が抗原陽性、右が抗原陰性
③抗酸菌検査
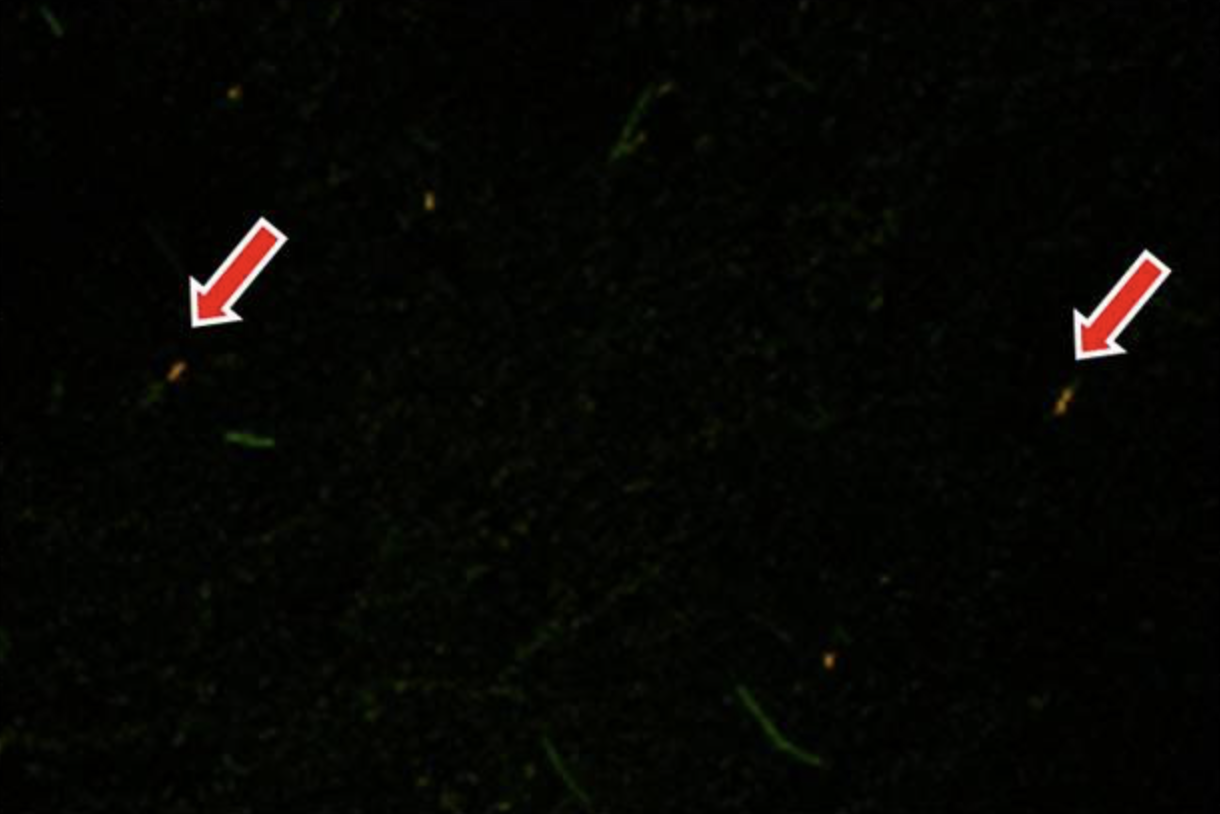
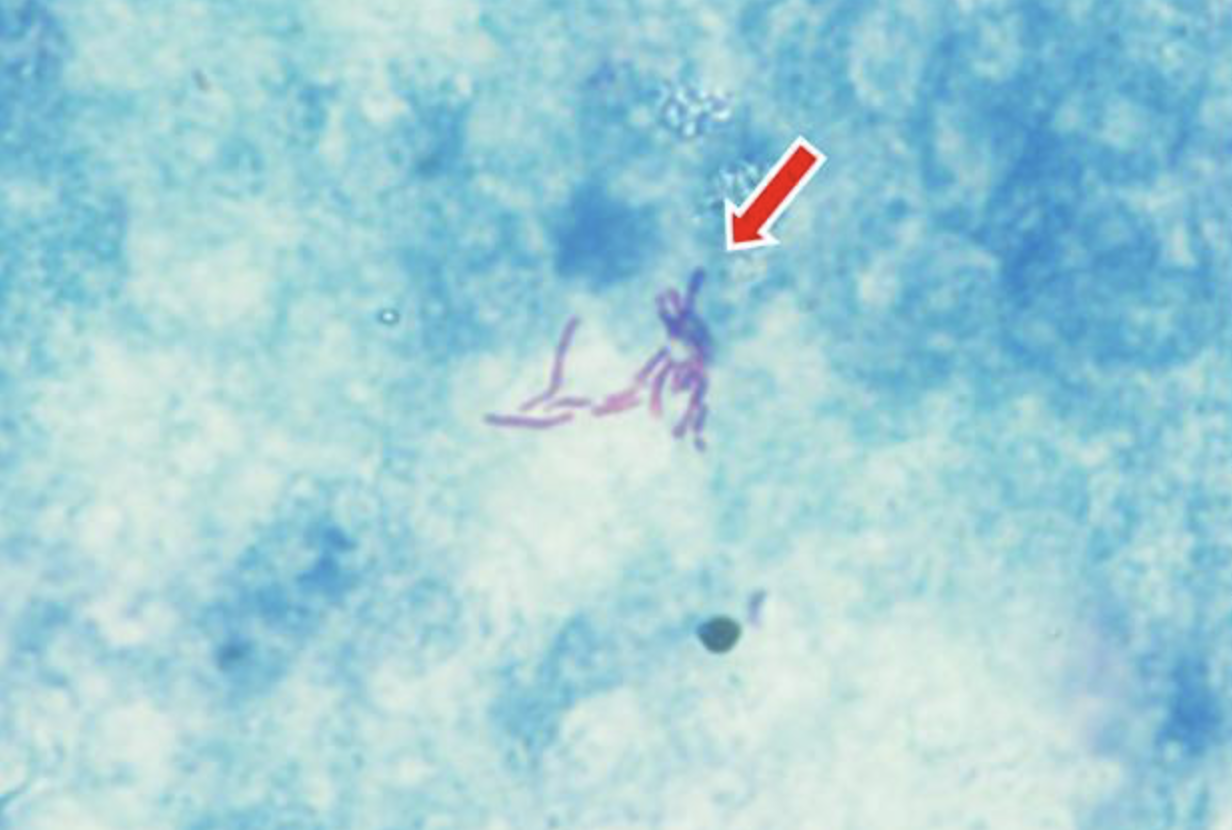
結核菌などの抗酸菌検査も当院で行っています。塗抹検査では蛍光染色とチール・ネンゼン染色を行います。これらの染色は抗酸菌以外の細菌は染色されないので、他の一般細菌と区別がつきます。
抗酸菌は発育が遅いものが多く培養には時間がかかるため、培養結果が出るのに1~2カ月かかることもあります。しかし、PCR法*3も同時に行うことで、半日以内に結果を報告することが可能になります。
④院内感染対策
感染制御チーム(ICT)の一員として、MRSA(メチシリン耐性黄色ブドウ球菌)、MDRP(多剤耐性緑膿菌)、ESBL(基質特異性拡張型βラクタマーゼ)産生菌などの院内感染の原因となる細菌の検出状況を調査し、院内感染防止に努めています。また、病棟内の水周りに院内感染の原因菌となる薬剤耐性菌がいないか環境調査を行い、アウトブレイク*4の防止にも努めています。
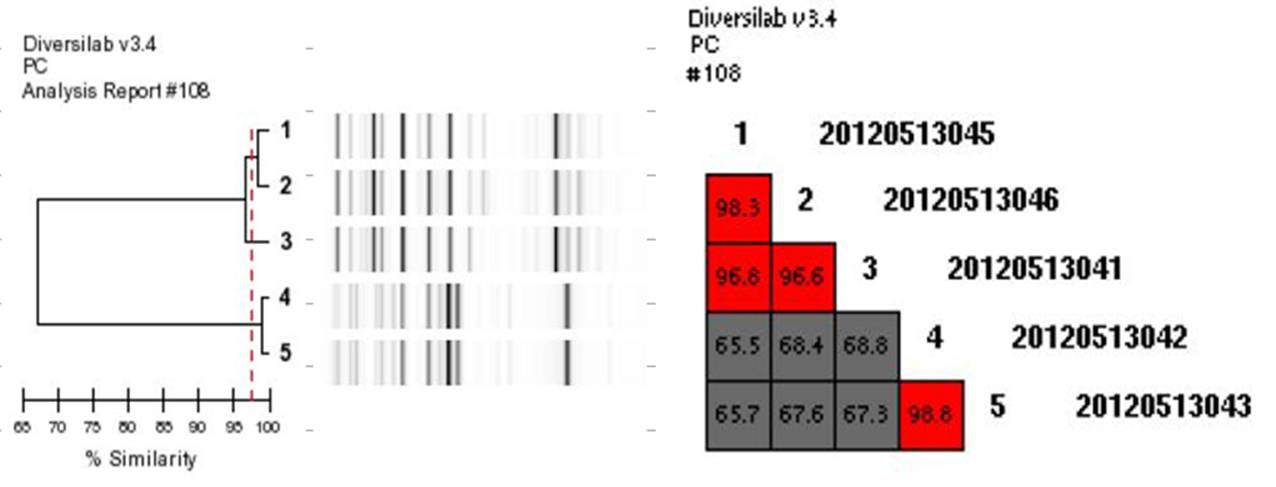
しかし、それでもアウトブレイクが発生した際には、遺伝子解析による疫学的調査を行っています。この遺伝子解析にはパルスフィールドゲル電気泳動法(PFGE)が広く用いられていますが、簡便性および迅速性に乏しいため、当院ではDiversiLabという特殊な機械による遺伝子解析を行い迅速に対応するようにしています。
1番と4番は別々の患者由来の菌。2と3は1番の患者の部屋の水周りにいた菌。5は4番の患者の部屋の水周りにいた菌。すなわち、右図では1と2は98.3%の相同性*5があり、ほぼ同一の菌株であると証明できますが、1と4の相同性は65.5%なので異なる菌株由来ということになります。
患者さんへのお願い
微生物検査室では生き物を扱っているため、早急に結果を報告することが難しいこともありますが、出来るだけ早く病原菌を見つけ出し適切な抗生剤の情報を主治医に提供できるよう日々努力しています。
しかし、せっかく検体を提出していただいたのにも関わらず、検査に不適切な検体もあります。例えば、喀痰の場合は唾液の含まれる粘液状のものだと口腔内には常在菌がたくさんいるため、病原微生物以外の菌のみが発育してしまい、検査結果の意味がなくなってしまいます。正確な検査結果を報告するために、喀痰を提出していただく際には、まずはうがいをし、口腔内の常在菌をできるだけ減らしてから、膿性な喀痰を提出していただくようにお願いします。
*1 グラム染色:細菌がもつ細胞壁の構造の違いにより、濃紫色に染まるグラム陽性菌とピンク色に染まるグラム陰性菌に分類される。
*2 抗原:体内に入ってきた時に生体防御のため免疫反応を引き起こす物質(微生物の構造タンパクなど)の総称。この免疫反応の原理が臨床検査に用いられている。
*3 PCR法:サーマルサイクラーという機械と特殊な試薬を用いて、細菌がもつDNAを増幅させることにより、ごく少量の細菌の有無を容易に確認できる方法。
*4 アウトブレイク:一定期間内に、特定の場所で同一菌種による感染症が発症すること。
*5 相同性:遺伝子の特定の部分が進化的に共通の祖先をもっているもの。相同性の割合が高いものが同じ菌株由来だと判断できる。
あとがき
この6月から、2階生理検査室の待合廊下にかわいいお花が飾られるようになりました。この花は生理検査室や採血室の職員が、自宅の庭や貸し農園、道ばた?に咲いたり育てたりしている花を持ち寄って飾っています。お店で売っているような華やかな花ではありませんが、野の花であるがゆえに、かえってほっと心が落ち着き和むような気がします。
また、花を飾っていると患者さんや他の職員から「お花かわいいですね」と話し掛けていただいたりして、野の花効果は色々なところに発揮されるようです。
光り輝くような豪華で華麗な花ではなく、普段は気付かれないようにそっと咲きほころびながらも、横を通り過ぎる人の風景の中で心を和ませている野の花。
医師や看護師のように患者さんとずっと関わりを持つわけではなく、検査や採血の少しの時間だけに触れあう私たち臨床検査技師も、その短い時間だからこそ野の花のようにそっと、患者さんに気持ちよくまた安心して良い検査を受けていただけるように努めたいと思っています。
子宮頸癌検査の実際とHPVの関係について
病理検査室 尾松 雅仁
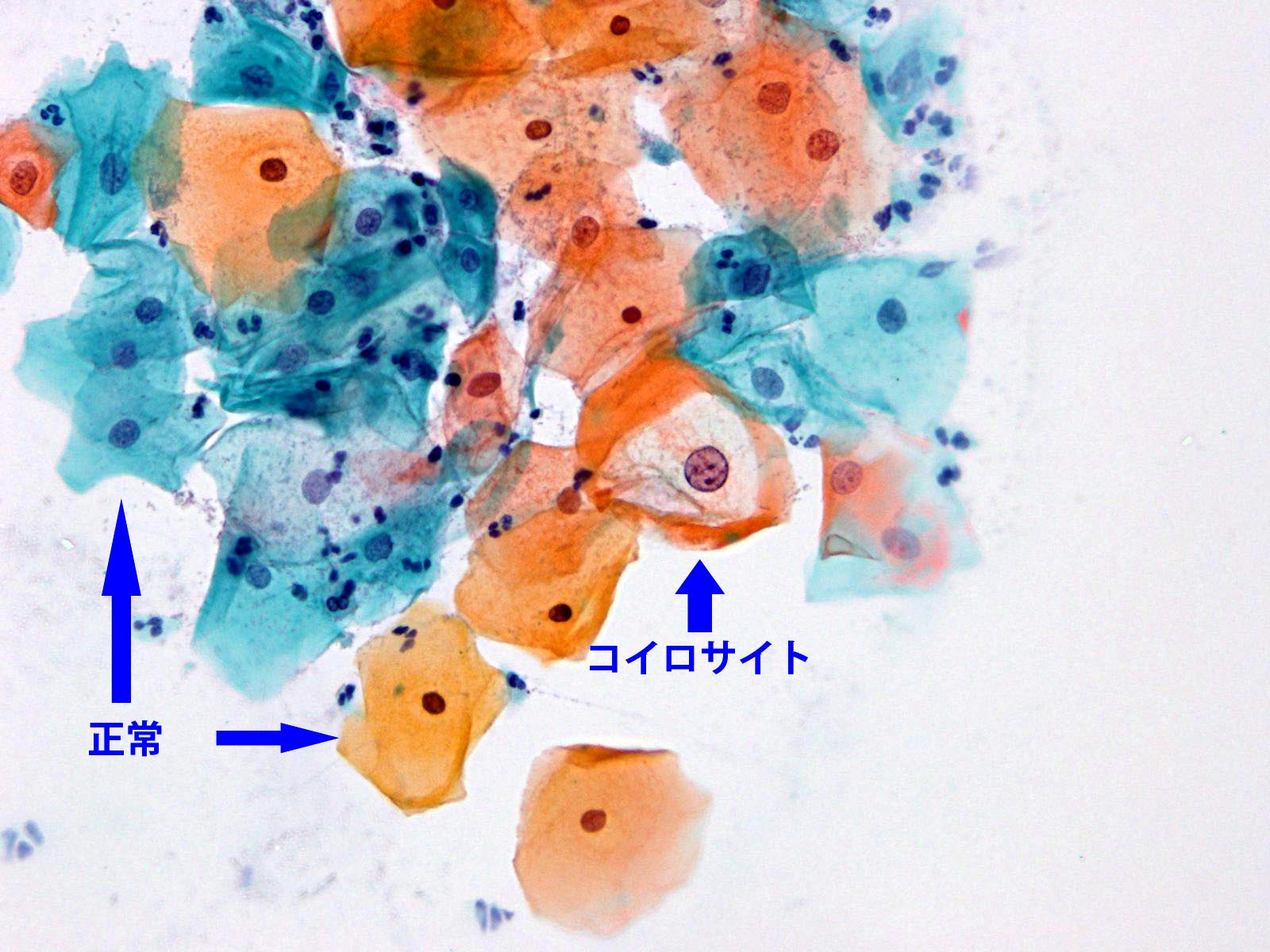
子宮頸癌は、HPV(ヒトパピローマウイルス)というウイルスによる感染がほとんどの原因ということが判っています。HPVは皮膚や粘膜に感染するウイルスで、現在、HPVには100種類以上の型が発見されており、発見順に番号がつけられています。性器粘膜に感染するHPVは発癌のリスクの程度によってハイリスク型とローリスク型に分けられており、ハイリスク型に分類されている型のうち16型、18型が特に発癌に関与しているとされています。
子宮頸癌は40~50歳代に好発しますが、近年では40歳未満の女性の子宮頸癌の罹患率が増加しています。しかし、異形成(子宮頸癌になる前の病変)が発見可能なため、定期的な子宮頸癌検診により異形成の段階で発見・治療することにより癌の発症を未然に防ぐ事が出来ます。また、現在では子宮頸癌の原因の大部分を占めるといわれているHPVウイルスの2価ワクチン(16型と18型)や、4価ワクチン(6型、11型、16型、18型)が開発されており、このワクチン接種をすることにより、発癌の予防効果が高いといわれています。
病理検査室では、子宮膣部・頸部の細胞診検査で、子宮頸癌やその前癌病変がないか、HPVやその他の感染症の検査をしています。そこで今回は病理検査室で行っている子宮頸癌の細胞診検査の実際をご紹介します。
A 細胞診検査の細胞採取および標本作製方法

B 各種細胞像とその特徴
① コイロサイト
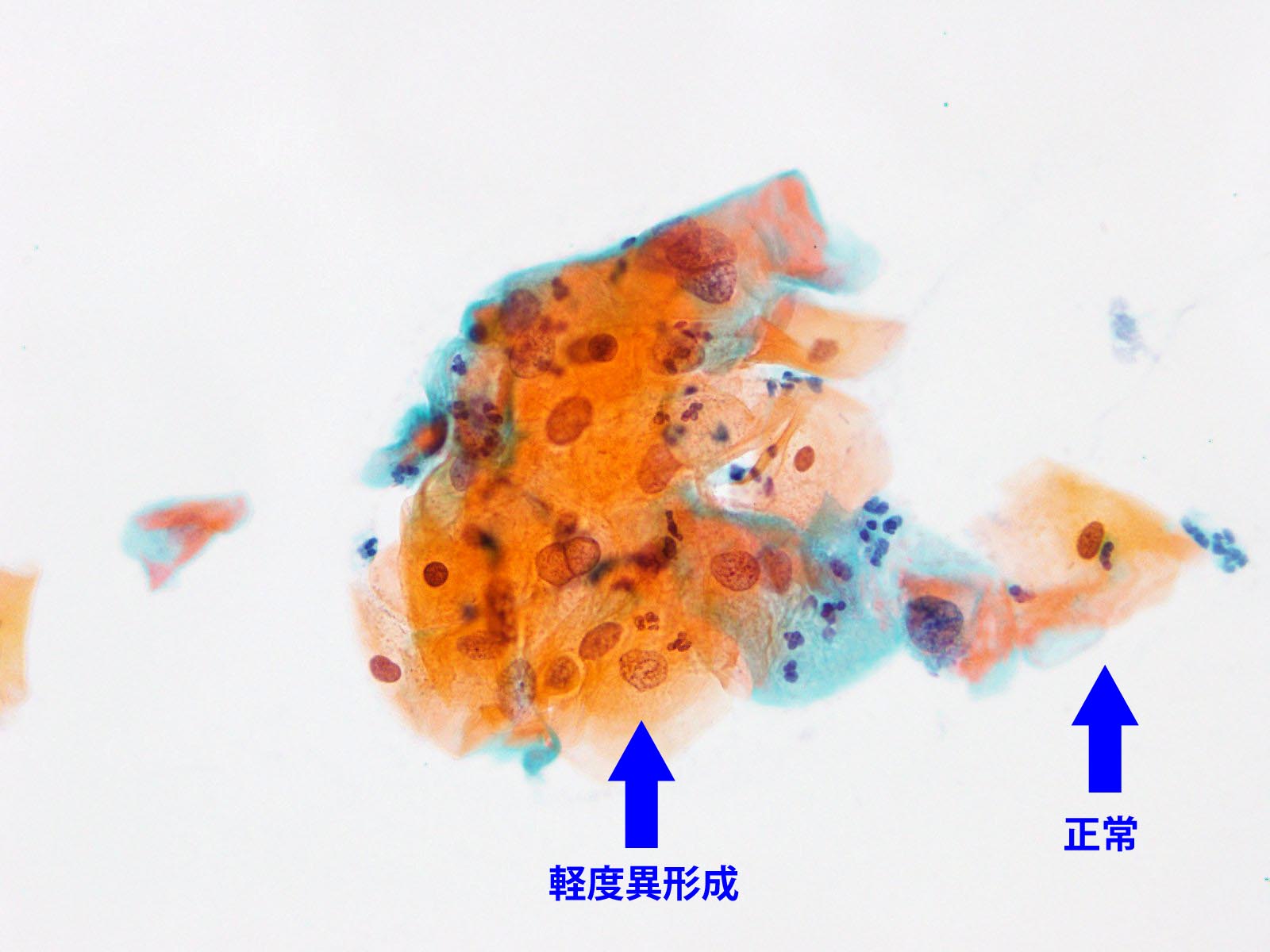
② 軽度異形成(mild dysplasia, low-grade squamous intraepithelial lesion [LSIL])
クラス分類:クラスⅢa
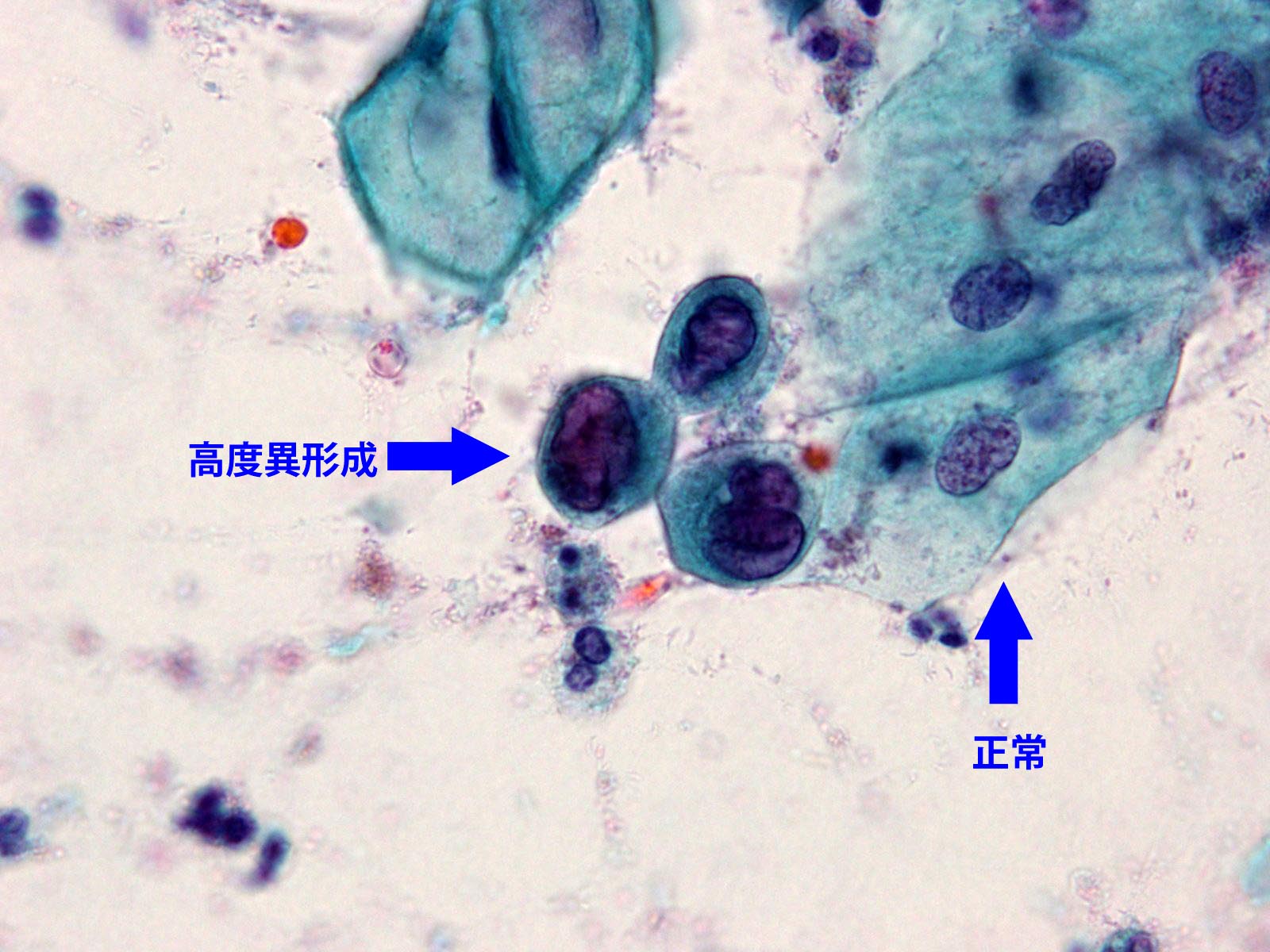
③ 高度異形成(severe dysplasia, high-grade squamous intraepithelial lesion [HSIL])
クラス分類:クラスⅢb
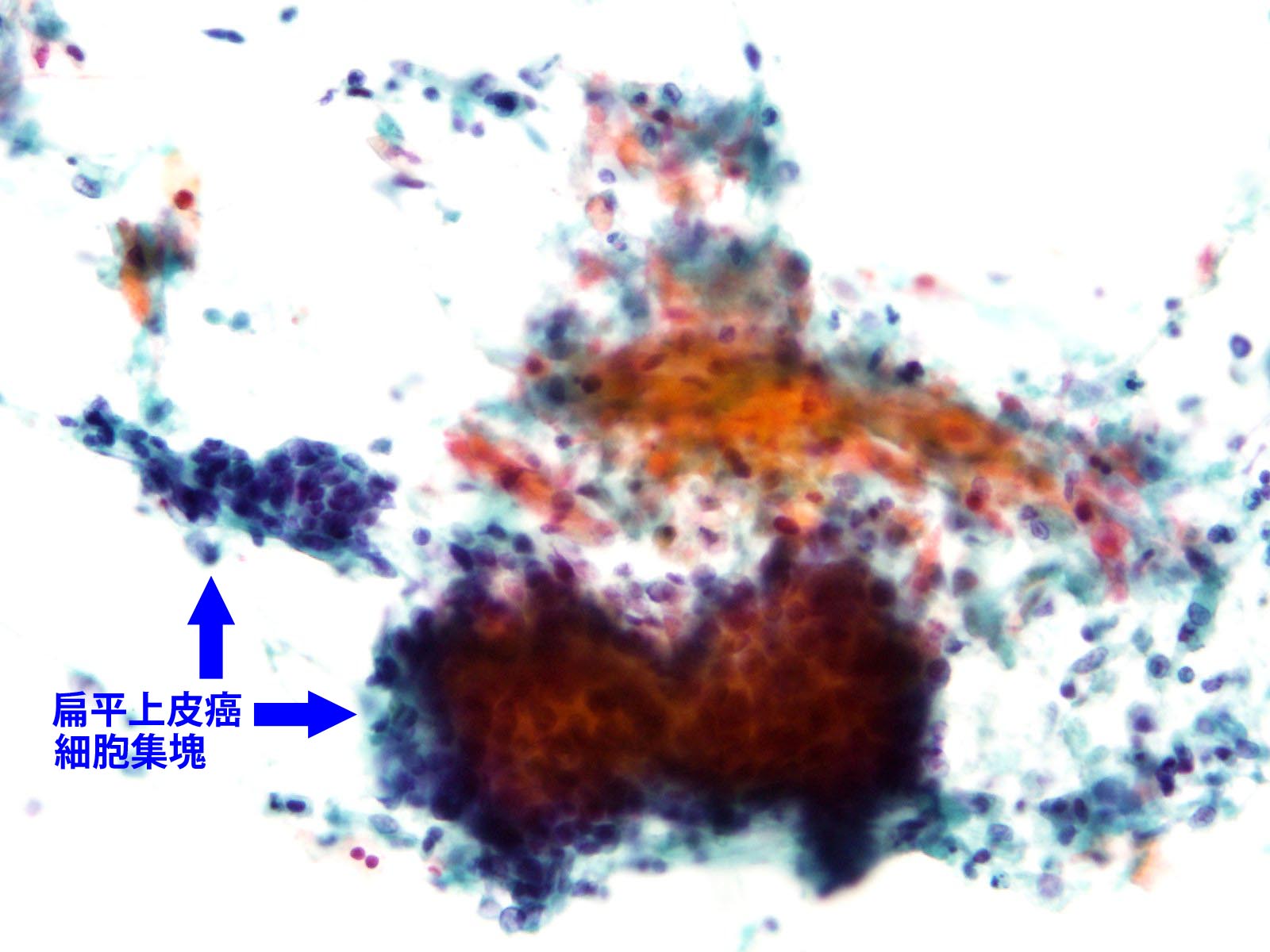
④ 扁平上皮癌 (squamous cell carcinoma) 浸潤癌
クラス分類:クラスⅤ
C まとめ
大部分の子宮頸癌はHPVの感染で発症する癌です。しかし、今回説明したように細胞診検査による細胞の異形成の確認により、早い時期に発見および治療できる癌です。定期的な子宮頸癌検診の実施やワクチン接種により予防できると考えられます。
*ワクチン接種はかなり高価(当院では、3回分合計で約52,000円前後)ですが、接種費用の助成をしている地方自治体もあります。神戸市では女子中学1年生から高校1年生までは全額助成しています。詳しくは、神戸市のホームページなどでご確認ください。
問い合わせ先
神戸市保健所 予防衛生課 結核・感染症係
TEL 078-322-6788
当院
TEL 078-302-4321(代表)
《追記6月20日》
平成25年6月14日に厚生労働省より「ヒトパピローマウイルス感染症の定期接種の対応について(勧告)」の中で、ワクチンの定期接種に関しては「副反応の発生頻度等が明らかになり、適切な情報提供ができるまでの間は積極的に勧奨すべきでない」との通知がなされています。詳細等は上記問い合わせ先、または各医療機関へご確認ください。
検査部ニュース
学術関係報告
論文発表
- Inoue D, Matsushita A, Kiuchi M, Takiuchi Y, Nagano S, Arima H, Mori M, Tabata S, Yamashiro A, Maruoka H, Oita T, Imai Y, Takahashi T.:Successful Treatment of γ-Heavy-Chain Disease with Rituximab and Fludarabine. Acta Haematol. 128: 139-143, 2012
学会発表
- 平成24年9月19日
大阪超音波研究会 大阪国際会議場
発表:菅原雅史、杤尾人司、鄭浩柄、他:「嚢胞性腫瘤様に描出された小児急性虫垂炎の一例」 - 平成24年9月19日
臨床医学検査学会関西支部総会 和歌山県 白浜
発表:野本奈津美、丸岡隼人、那須浩二、老田達雄:「6カラーフロサイトメトリーを用いた形質細胞性腫瘍のイムノフェノタイピング」
発表:山城明子、柴田洋子、田村明代、三木寛二、老田達雄:「検査相談室開設後5年間の報告」
発表:杤尾人司、崎園賢治、竹川啓史、江藤正明:
「アルコール禁患者におけるクロルヘキシジングルコン酸塩による静脈採血時の適正な消毒時間」 - 平成24年10月6日
日本超音波医学会 第39回関西地方会 大阪
発表:竹林真実子、岩崎信広、杉之下与志樹、他:「当院における過去5年間の腹部腫瘤の検討」
発表:岩崎信広、竹林真実子、杉之下与志樹、他:「急性膵炎を伴った膵仮性動静脈奇形(AVM)の一例」
発表:岩崎信広、竹林真実子、杉之下与志樹、他:「アメーバ感染により大腸憩室穿孔を来した一例」
発表:浜田一美、登阪貴子、佐々木翔、他:「濾胞癌術後残存葉にびまん性硬化型乳頭癌の発症を認めた一例」
発表:三羽えり子、荒木直子、岩崎信広、他:「造影超音波を施行した肝悪性リンパ腫の一例」
発表:菅原雅史、杤尾人司、濱田一美、他:「小児に発症した水腎症を伴う穿孔性虫垂炎の一例:嚢胞性腫瘤様に描出された機序について」
発表:野村菜美子、谷知子、紺田利子、他:「心電図上左室肥大が疑われたが、経胸壁心エコー検査にて左室壁肥厚を認めなかった2症例」 - 平成24年10月11日
日本聴覚医学会 国立京都国際会館 京都
発表:濵田 充生:「聴力検査で軽度の左右差を認めた片側性のAuditory neuropathyの一例」 - 平成24年11月5日
日本感染症学会中日本地方学会 アクロス福岡
発表:仁木真理恵、三木寛二、竹川啓史:「rep-PCR解析による緑膿菌の疫学調査」 - 平成24年11月30日
日本臨床検査医学会総会 京都
発表:丸岡隼人、老田達雄、石川隆之:「6カラーフローサイトメトリーによるB-ALLのイムノフェノタイピング」
講演
- 平成24年6月28日
腹部超音波カンファレンス 神戸
講演:岩崎 信広:「腹部腫瘤の超音波診断」 - 平成24年7月21日
生理部門システムフォーラム 大阪
講演:川井 順一:「部門システム導入への取り組み」 - 平成24年7月26日
第13回神戸グラム染色カンファレンス 神戸ANAクラウンプラザホテル
講演:竹川啓史:「キャッスルマン病患者に発症した蜂窩織炎の1症例」 - 平成24年9月21日
救急カンファレンス
講演:柴田洋子:「安全な輸血のために」 - 平成24年9月30日
臨床医学検査学会関西支部総会(和歌山白浜)
講演:竹川啓史:「グラム染色で行うべき最低限の報告」
講演:杤尾人司:「肝細胞癌(HCC)の評価のコツ」 - 平成24年9月15日
平成24年度感染管理認定看護師教育課程 神戸研修センター
講演:竹川啓史:「真菌および培養困難な微生物について」 - 平成24年9月21日
平成24年度感染管理認定看護師教育課程 神戸大学大学院保健学研究科
講演:竹川啓史:「微生物検査の概論・検査の基本操作」 - 平成24年9月22日
平成24年度感染管理認定看護師教育課程 神戸大学大学院保健学研究科
講演:竹川啓史:「培地の観察と判定」 - 平成24年9月23日
平成24年度感染管理認定看護師教育課程 神戸大学大学院保健学研究科
講演:竹川啓史:「抗酸菌検査・真菌観察・薬剤感受性の判定等」
あとがき
秋は学会の季節です。当臨床検査技術部のメンバーも医学検査学会・超音波学会・感染症学会などに精力的に学会発表を行ないました。H23年H24年採用の新人の発表も5題あり、本人の努力はもとより、指導する者も腕の見せ所といったところでしょうか。 今年は検査室全体で予演会が行なわれました。臨床検査は血液検査、細菌検査、病理検査、超音波検査等と幅広い分野にわかれるため、演者は聴衆に発表内容の予備知識を与えるため、まず、専門用語や測定原理など簡単な講義をして聴衆の理解を深めた後の発表となりました。新人は落ち着いてしっかり発表し、発表後の質疑応答にもりっぱに返答していました。専門外からの切り口での指摘もあり、大いに議論がかわされ意義のある会となりました。
検体検査の流れについて -検体採取から結果報告まで-
一般検査室 依岡 麻未、 生化学検査室 宮崎 千尋
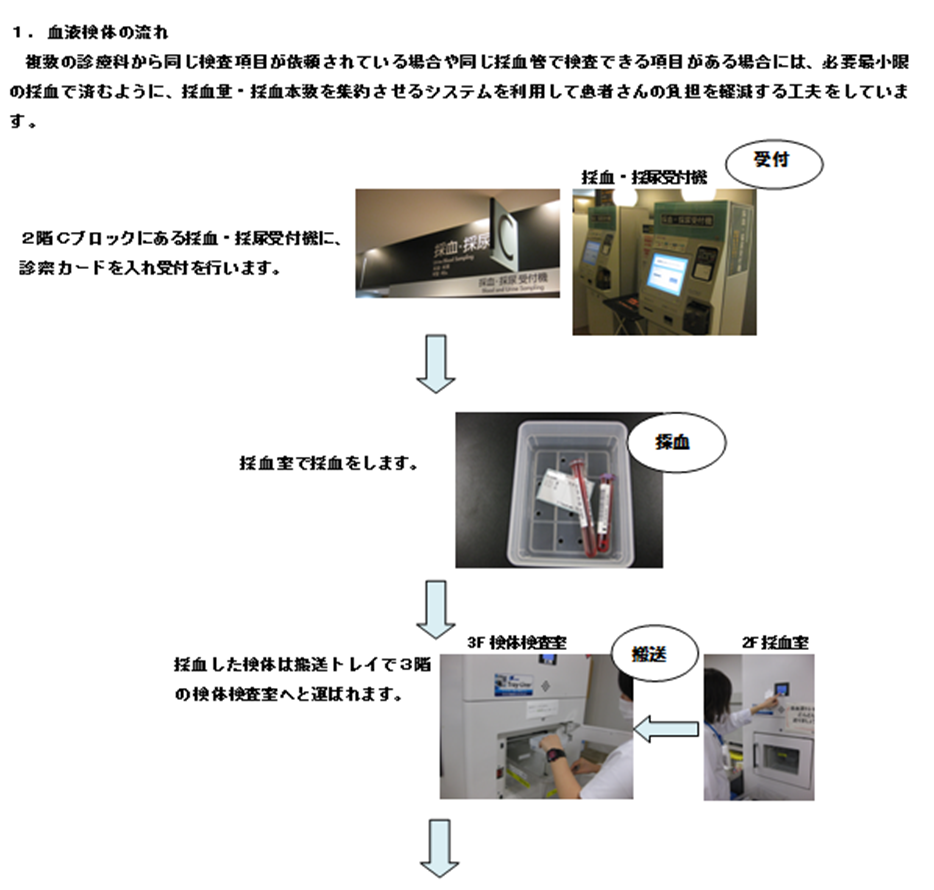
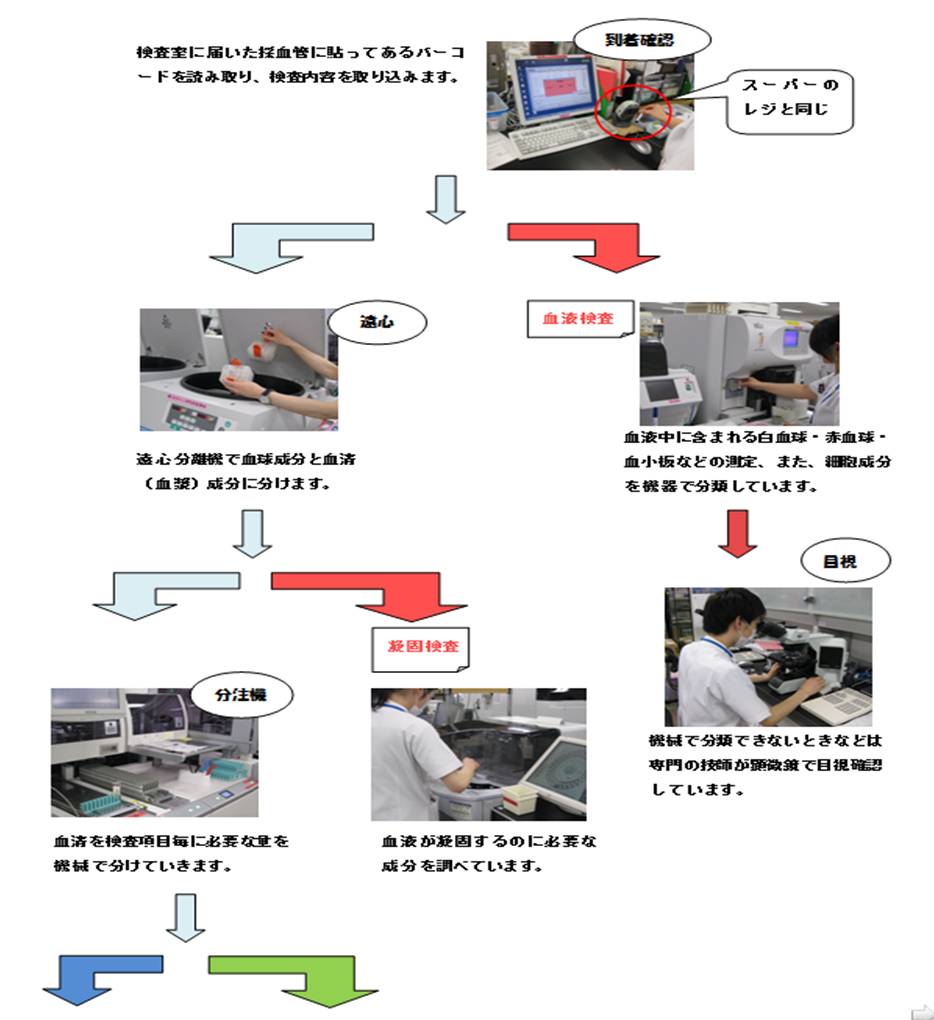
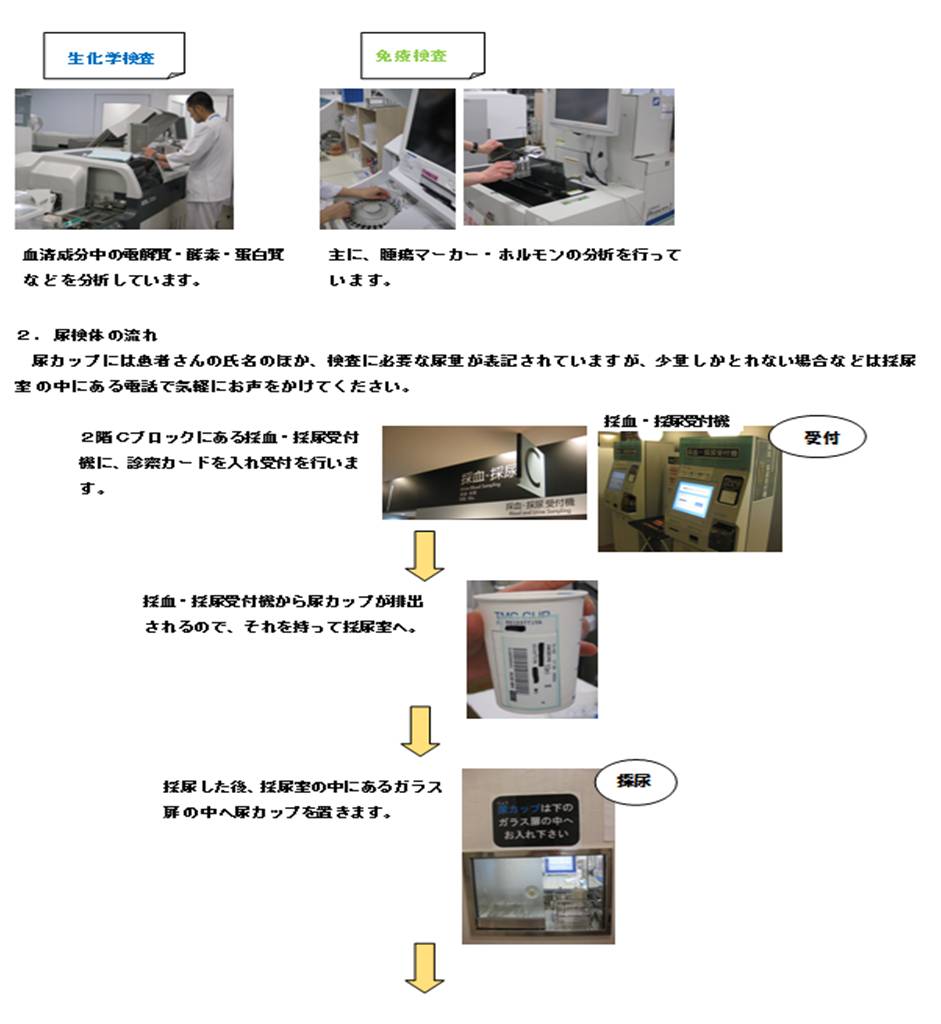
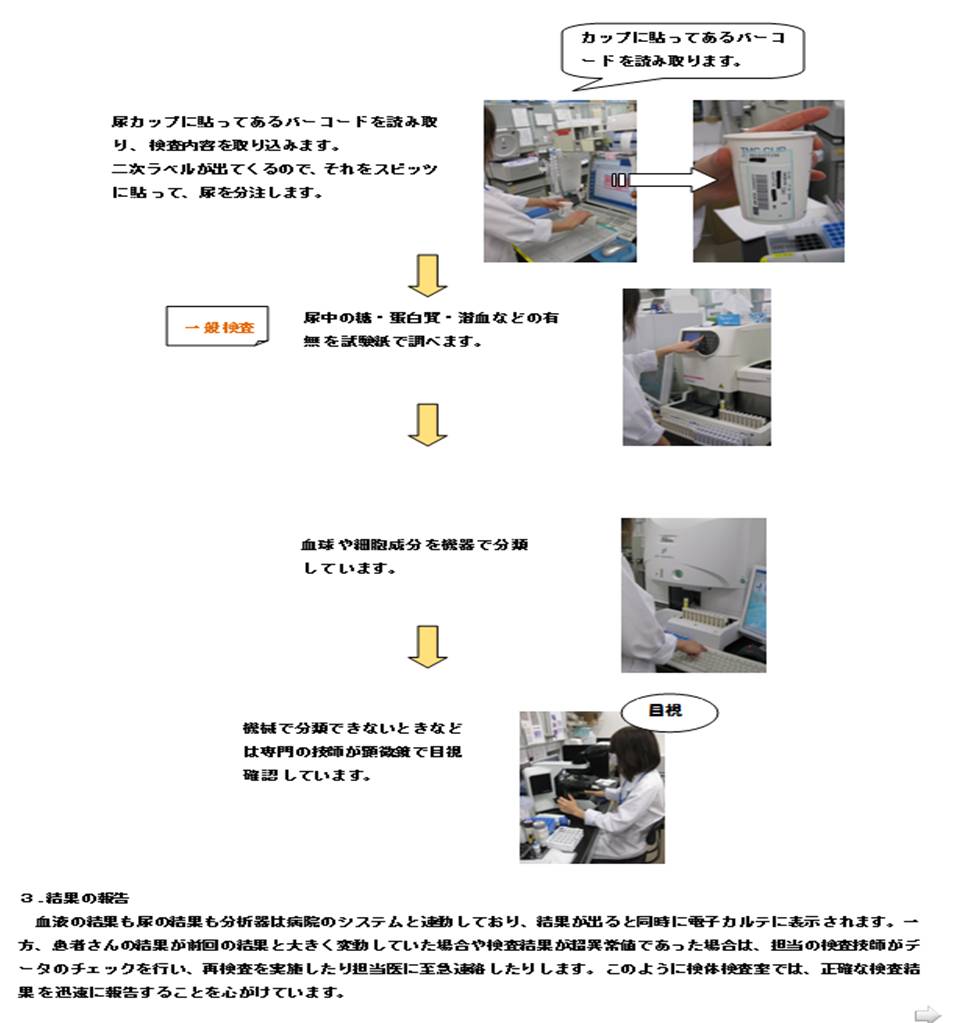
当院の検体検査室は2階と3階に位置しています。2階の採尿室の奥に一般検査室があり、主に採尿室から提出された尿の分析を行っています。また、採血室で採血された血液は搬送トレイで3階に搬送され、生化学検査、免疫検査、血液検査部門で分析を行っています。
当院の検査室では、正確な検査結果を迅速に報告するために様々な取り組みをしています。診察までに検査結果を提供できるよう、外来診察前検査では検査室に検体が届いてから1時間以内に結果を報告する即時報告を実施しています。即時検査対象項目は、肝機能や貧血の一般的な検査項目ばかりではなく、ホルモンや腫瘍マーカーまで100項目近くの検査を対象としています。また、検査結果から判断して、直ちに治療が必要な病態を表す検査値(パニック値)が検出された場合には、臨床検査技師が担当医に緊急連絡する体制をとっています。さらに、24時間365日緊急検査が実施できる体制を整え当院の救急医療を支援しています。
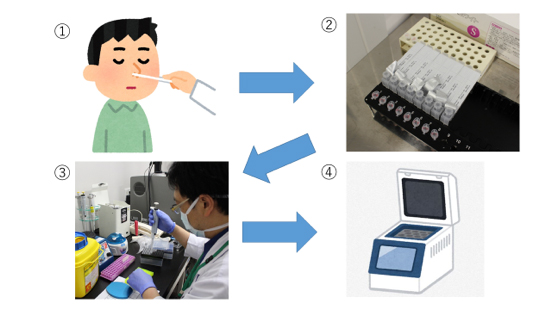
今回は患者さんから採血・採尿された後の検体が検査され結果が出るまでの流れを簡単にご紹介します。
食事や運動などによって影響を受ける血液検査項目についてはご理解いただけましたでしょうか?
前日や当日の運動や食事、飲酒、喫煙などで検査結果に影響を与え、変動してしまう場合があります。より正確な検査結果を提供するためには患者さんの協力が不可欠ですので、担当医から絶食等の指示がありましたらお守りいただくようお願いします。
また、スタッフ一同、迅速で正確な検査結果を各診療科に提供できるよう努力しておりますが、検査内容によっては時間がかかりますので、診察当日の検査の場合は、診察予約時間の1時間前には採血・採尿を済ませておくようお願いいたします。
検査部ニュース
学術関係報告
論文発表
- Inoue D, Matsushita A, Kiuchi M, Takiuchi Y, Nagano S, Arima H, Mori M, Tabata S, Yamashiro A, Maruoka H, Oita T, Imai Y, Takahashi T.:Successful Treatment of γ-Heavy-Chain Disease with Rituximab and Fludarabine. Acta Haematol. 128: 139-143, 2012
学会発表
- ○平成24年9月19日
大阪超音波研究会 大阪国際会議場
発表:菅原雅史、杤尾人司、鄭浩柄、他:「嚢胞性腫瘤様に描出された小児急性虫垂炎の一例」 - 平成24年9月19日
臨床医学検査学会関西支部総会 和歌山県 白浜
発表:野本奈津美、丸岡隼人、那須浩二、老田達雄:「6カラーフロサイトメトリーを用いた形質細胞性腫瘍のイムノフェノタイピング」
発表:山城明子、柴田洋子、田村明代、三木寛二、老田達雄:「検査相談室開設後5年間の報告」
発表:杤尾人司、崎園賢治、竹川啓史、江藤正明:
「アルコール禁患者におけるクロルヘキシジングルコン酸塩による静脈採血時の適正な消毒時間」
発表:秋田豊和, 高野弘美:「輸血検査受託施設への新人教育プログラム導入の試み」
発表:鈴木久惠, 井上史江, 宍戸裕貴子, 上野寿行:「当院におけるDダイマー定量値と疾患関連性の検索」
発表:長谷川美幸, 海妻哉予子, 木内峰代, 秋田豊和 :「自動電気化学発光免疫分析装置cobas e411によるTgAb 及びTPOAb測定試薬の基礎的検討」 - 平成24年10月6日
日本超音波医学会 第39回関西地方会 大阪
発表:竹林真実子、岩崎信広、杉之下与志樹、他:「当院における過去5年間の腹部腫瘤の検討」
発表:岩崎信広、竹林真実子、杉之下与志樹、他:「急性膵炎を伴った膵仮性動静脈奇形(AVM)の一例」
発表:岩崎信広、竹林真実子、杉之下与志樹、他:「アメーバ感染により大腸憩室穿孔を来した一例」
発表:浜田一美、登阪貴子、佐々木翔、他:「濾胞癌術後残存葉にびまん性硬化型乳頭癌の発症を認めた一例」
発表:三羽えり子、荒木直子、岩崎信広、他:「造影超音波を施行した肝悪性リンパ腫の一例」
発表:菅原雅史、杤尾人司、濱田一美、他:「小児に発症した水腎症を伴う穿孔性虫垂炎の一例:嚢胞性腫瘤様に描出された機序について」
発表:野村菜美子、谷知子、紺田利子、他:「心電図上左室肥大が疑われたが、経胸壁心エコー検査にて左室壁肥厚を認めなかった2症例」 - 平成24年10月11日
日本聴覚医学会 国立京都国際会館 京都
発表:濵田 充生:「聴力検査で軽度の左右差を認めた片側性のAuditory neuropathyの一例」 - 平成24年11月5日
日本感染症学会中日本地方学会 アクロス福岡
発表:仁木真理恵、三木寛二、竹川啓史:「rep-PCR解析による緑膿菌の疫学調査」 - 平成24年11月30日
日本臨床検査医学会総会 京都
発表:丸岡隼人、老田達雄、石川隆之:「6カラーフローサイトメトリーによるB-ALLのイムノフェノタイピング」
講演
- 平成24年6月28日
腹部超音波カンファレンス 神戸
講演:岩崎 信広:「腹部腫瘤の超音波診断」 - 平成24年7月21日
生理部門システムフォーラム 大阪
講演:川井 順一:「部門システム導入への取り組み」 - 平成24年7月26日
第13回神戸グラム染色カンファレンス 神戸ANAクラウンプラザホテル
講演:竹川啓史:「キャッスルマン病患者に発症した蜂窩織炎の1症例」 - 平成24年9月21日
救急カンファレンス
講演:柴田洋子:「安全な輸血のために」 - 平成24年9月30日
臨床医学検査学会関西支部総会(和歌山白浜)
講演:竹川啓史:「グラム染色で行うべき最低限の報告」
講演:杤尾人司:「肝細胞癌(HCC)の評価のコツ」 - 平成24年9月15日
平成24年度感染管理認定看護師教育課程 神戸研修センター
講演:竹川啓史:「真菌および培養困難な微生物について」 - 平成24年9月21日
平成24年度感染管理認定看護師教育課程 神戸大学大学院保健学研究科
講演:竹川啓史:「微生物検査の概論・検査の基本操作」 - 平成24年9月22日
平成24年度感染管理認定看護師教育課程 神戸大学大学院保健学研究科
講演:竹川啓史:「培地の観察と判定」 - 平成24年9月23日
平成24年度感染管理認定看護師教育課程 神戸大学大学院保健学研究科
講演:竹川啓史:「抗酸菌検査・真菌観察・薬剤感受性の判定等」
あとがき
いった。 にげた。 そして、さろうとしている。
2013年の月々ことである。
ホームページ更新予定日は過ぎた。時の流れがはやい。はやすぎる。
ありがたいことだ。
やることは多い。多すぎる。でもやれることがありがたい。
しあわせなことだ。
しかし、できていない。だから“時”がたつのがはやい。
検査部タイムズ「TEKARI」誕生からはや1年。
3か月に1度のわずか4回の更新ではあるが継続している。
着実に成長している。
立派になっている。
なにしろ内容がいい。寄稿者に感謝する。
2歳の誕生日を目指して、さあ、また一年ガンバロウ。
「神戸から世界へ発信、神戸中央市民病院 臨床検査技術部」
H.T
新病院移転後の輸血業務について
輸血検査管理室 楠本 寿子
検査部ニュース
学術関係報告
ain Disease with Rituximab and Fludarabine. Acta Haematol. 128: 139-143, 2012
学会発表
- 平成25年3月2日
第6回脳波・筋電図セミナー 京都 京都テルサ
発表:佐々木一朗 :「Cコース法的脳死判定について」 - 平成25年3月10日
ACC2013 Moscone center in San Francisco
発表:紺田利子、谷知子、古川裕 :「Mitral Annular Disjunction in Consecytive Cases:Echocardiographic Detection 」 - 平成25年5月18-19日
第62回日本医学検査学会
発表:上野寿行, 宮野悟, 田仲真樹子, 櫻井香織, 井上史江, 鈴木久恵, 秋田豊和, 丹羽欣正:「JAMT勧告法及びJSLH標準法案を用いた血液像トレーニングの評価」 - 平成25年5月18-19日
第62回日本医学検査学会
発表:森宏和, 宮崎千尋, 武市光司, 海妻哉予子, 秋田豊和, 高野弘美, 相川恭一郎:「新入社員および教育担当者育成プログラム(メンター制度)導入の試み」 - 平成25年5月18-19日
第62回日本医学検査学会
発表:依岡麻未, 鈴木千晶, 久恵啓史, 秋田豊和, 高野弘美, 相川恭一郎:「新入社員教育システム(メンター制度)の導入と取り組み効果について」
あとがき
“TEKARI”の特集記事を読むと自分の見識の狭さに愕然とさせられる。まさに“井の中の蛙大海を知らず”である。このことわざは「荘子」秋水篇の中の「井蛙不可以語於海者、拘於虚也」が原点とされ、「井の中に住む蛙にとっては井の中がすべてであり、大きな海があることを知らない」という意から見聞の狭い者をあざけっていう言葉である。検査を行っている我々も、ともするとそれぞれの“専門分野”という井の中で得意になり、他の事を考えなくなっていることがある。自分にとっての“井”を知り、さらに「大海を知り、少なくともその深さまで知る」ために“TEKARI”が今後も途絶えることなく情報を発信し、”井の中にいる自分“を見つめ直す機会となっていくことを井戸の中から青く澄みわたった天空を眺めながら願っている。
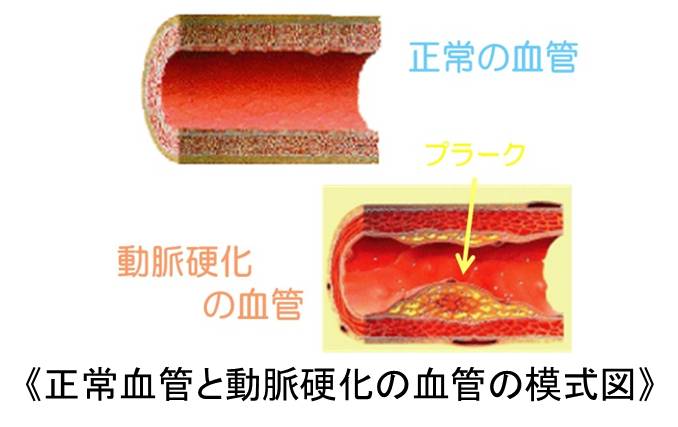
動脈硬化と脈波図検査(PWV/ABI)
生理機能検査 心肺部門 野本奈津美
日本動脈硬化学会によると、日本人の死因の第1位はがんですが、第2位の心疾患、第3位の脳血管疾患を合わせるとがんと同じぐらいの人々が亡くなっていると報告されています。これら心疾患や脳血管疾患の大多数は動脈硬化が原因で発症しています。
動脈硬化とは、動脈が年齢とともに変化して血管が弾力性を失い硬くなるとともに、血管壁にコレステロール等の脂質が沈着し、内腔が狭くなる状態をいいます。糖尿病、高血圧症や高脂血症といった生活習慣病があると、動脈硬化は発症しやすくなります。動脈硬化は狭心症や心筋梗塞などの虚血性心疾患、脳梗塞などの脳血管障害や閉塞性動脈硬化症といった病気の原因となります。
閉塞性動脈硬化症(ASO:arteriosclerosis obliterans)は、手や足の血管の動脈硬化によって血管が狭くなったり(狭窄)、血管が詰まったり(閉塞)し、末梢への血液の流れが悪くなることで手足に様々な障害が起こる疾患です。主な症状として、下肢冷感や間歇性破行(かんけつせいはこう:数十~数百m歩くと痛みのため歩けなくなるが、休むと症状が治まる)などがあり、重症になると安静時疼痛、下肢の壊死や皮膚潰瘍などが起こります。
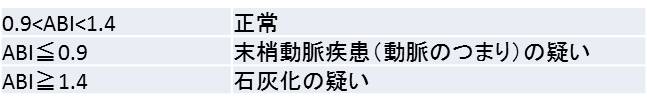
以上のことから、動脈壁の硬さや動脈のつまりを評価することは、さまざまな病気の原因となる動脈硬化の状態を知る上で大変重要です。これらは、脈波図検査である ABI(足関節/上腕血圧比)およびPWV(脈波伝播速度)という方法で評価することができます。
今回は、動脈壁の硬さや動脈のつまりを簡便かつ非侵襲的に評価することができる脈波図検査(ABI/PWV)について解説します。
ABI(足関節/上腕血圧比)とは
ABI(足関節/上腕血圧比)とは、足関節収縮期血圧/上腕収縮期血圧のことです。計算式は以下のようになります。
- 健常者では、下肢の血圧は上腕の血圧と同じかもしくは少し高くなっているため、ABIは1.00~1.29の範囲に入ります。
- 下肢血管の狭窄がある場合、下肢の血圧が低くなるためABIが0.9以下になります。
- 血圧の左右差がある場合も狭窄を疑う所見となります。
しかし、ABIが0.9以上でも狭窄が起こっている場合があります。血管が75%以上狭窄しないと血圧は急激に低下しないこと、糖尿病などでは動脈の石灰化があるため血管を締め付けるのにより高い圧が必要になり、測定値が高く表現されてしまう場合があることが理由として挙げられます。
そのため、ABIの数値だけでなく波形などを含め総合的に評価することが大切です。
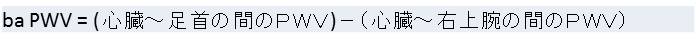
PWV(脈波伝播速度)とは
PWV(脈波伝播速度)とは、心臓から押し出された血液による拍動が動脈を伝わっていく速度のことです。当検査室ではba PWV(上腕-足首脈波伝播速度:Brachial-Ankle pulse Wave Velocity)を測定しています。計算式は以下のようになります。
- 健常者では、血管がしなやかで弾力性があり、脈波が血管壁に吸収されるため、速度は遅くなります。
- 血管壁が硬く厚いほど、脈波が血管壁で吸収されず速度は速くなります。
ba PWVには年齢別で基準値があり、年齢ともに高くなります。50代半ばまでは女性ホルモンの影響で女性の方が男性よりも低い傾向にありますが、60代を超えると差はなくなります。ba PWVを用いて血管年齢を推測することもできます。
引用)PWVによる動脈硬化早期診断、監修:西沢良記ほか、発行:協和企画
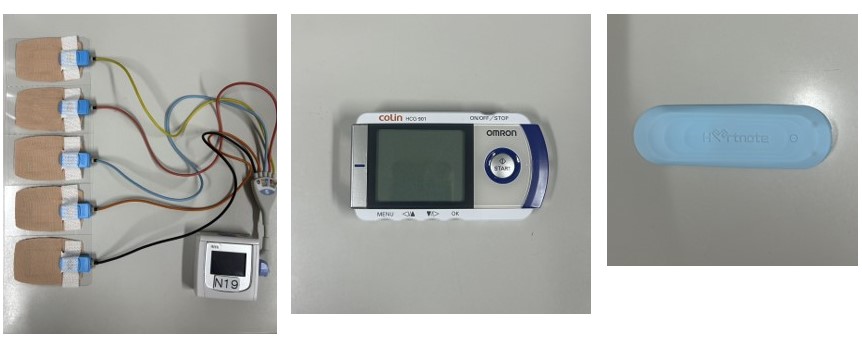
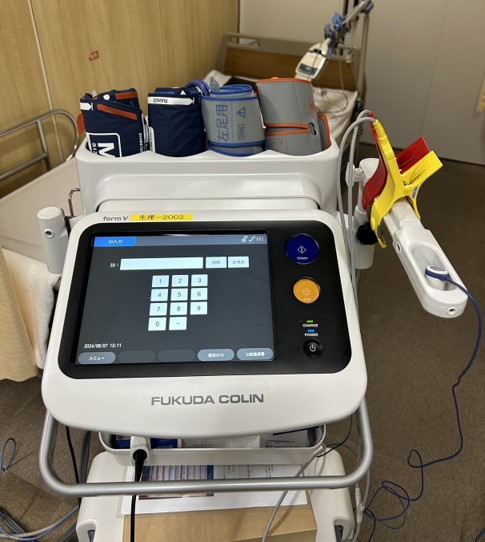
検査の実際
実際の検査の流れをご紹介します。機械と測定中の様子を下図に示しています。
- 仰臥位で5分程度安静にしてから検査を行います。
- 上腕(二の腕付近)と足首に血圧計を装着するため、厚手の服は脱いでいただきます。靴下は脱いでいただくか、かかとが見えるように下げていただきます。
- 血圧計を左右の上腕及び足首に、心電図用の電極を両手首に、心音図用のマイクを胸(肋間)に装着します。
- 血圧は4か所同時に2回測定を行います。透析をされている場合や手足に大きな怪我などをされている場合は、検査担当者にお伝えください。
- 検査中は心音の記録を行っていますので、動いたり、お話したりしないようにお願いいたします。
- 検査時間はお部屋に入っていただいてから10分程度です。
最後に
動脈硬化は無症候性(症状を感じない)に加齢とともに進展しますが、若年者においてもすでに動脈の硬化病変が認められています。したがって、動脈硬化は決して中・高年者だけの病変ではなく、より早期に診断し、より早い対策をとることが重要です。脈波図検査(PWV/ABI)は早期の動脈硬化を知るための検査法の一つであり、患者さんの負担も少なく簡便に行うことができます。下肢症状のある方、生活習慣病などリスクの高い方は是非、主治医に相談してみてください。
参考文献
PWVによる動脈硬化早期診断、監修:西沢良記ほか、発行:協和企画
採血のQ&A
外来採血室 田村 明代
Q1.採血を受ける時のよい服装はありますか?
A. 採血時には上着を脱いでいただきます。また、袖を上まで上げさせて頂きますので、袖口をまくったときに、なるべくきつくない服でおいでください。 袖口がきついと針を抜いたときに血が止まりにくくなります。
Q2.食事を摂ってきたけど大丈夫?
A. 医師から、採血検査を絶食で受けるようにと指示されている患者さん以外は、お食事されていても構いません。但し、他の絶食の検査と同日に受けられる場合はその検査の指示に従ってください。 (検査案内書の上方にある‘絶食で検査を受けてください’のところにチェックある方は絶食です) 採血へ絶食の指示があった場合でも、特殊な場合を除き水分の摂取は構いません。水分も摂らないようにと指示された以外は、普通に朝水分(水や白湯、お茶等)を摂ってきて頂くようお願いします。薬に関しては主治医にご確認ください。
Q3.採血をスムーズに出来る方法は?
A. 採血時にはどうしても緊張してしまいますが、緊張すると血管も縮んでしまいます。どうぞリラックスしてお受けください。また背筋を伸ばし、親指を中にして手を握っていただくと、血管も見えやすくなるようです。 朝から水を一滴も摂っていないと、血管も見えにくくなります。医師から水分制限を受けている方以外は、普通に朝水分(水や白湯、お茶等)を摂ってきて頂くようお願いします。
Q4.なぜ何本も採血するのですか?
A. 検査には、
1.血を固めてその上澄み(血清)を測定するもの
2.血を固めずにその上澄み(血漿)を測定するもの
3.分離せずにそのまま測定するもの
等あります。これら色々な検査によって採血管の中にはそれぞれ違う薬剤が入っているために、数本の採血が必要となってきます。
Q5.採血管をクルクル回しているのはなぜ?
A. 採血管には前述のようにたくさんの種類があり、検査の為の色々な薬剤が入っている採血管があります。これらの採血管では中の薬剤と血液とをよく混ぜる必要があり、採血者が手で混和する手間を省くために機械でクルクルと回して混和しています。
Q6.こんなに何本も血を採って大丈夫?
A. 血液は体重により違いはありますが、成人ではだいたい4~6L(体重のおよそ 1/13)が体の中をめぐっています。採血室では殆どの患者さんの採血は3-5本で採血量は20ml以内(約大さじスプーン1杯)ですので、体に流れている血液のだいたい1/250程度です。ご安心ください。
Q7.採血をした日はお風呂に入ってもいいの?
A. 血が止まっていれば入浴しても構いません。 但し、採血部位を強くこすったりしないようにして、当日は清潔にしていただくようお願いします。
Q8.採血後に消毒したところが赤くなってかぶれたりするのですが?
A. 採血をする時には、アルコールを染み込ませた綿を消毒に使用しています。 アルコールに過敏な方は、アルコール綿を使うと赤くなったり、かゆくなったり、腫れたりします。あらかじめ、申し出ていただければ別の消毒綿を使用します。数日経過してもかゆみや腫れがひかない場合はご相談ください。 また、テープにかぶれるという方も申し出ていただければ対応します。
Q9.採血後になぜ5分も押さえるの?
A. 血はすぐ止まるわけではありません。 綿の上からテープを貼っただけでは皮膚の穴しかふさがらないので、血管から出た血が皮下に溜まって青くなったり(内出血)します。 上からしっかり押さえることにより、血管の穴もふさがります。 また、採血後すぐに採血した方の手で重い物を持ったり、血圧測定などをすると、ふさがっていた穴から血液が漏れたりして内出血の原因になり、洋服を汚したりする場合がありますのでご注意ください。 血の止まりにくいお薬(ワーファリンやアスピリン等)を服用中の方はもっと長めに(10分程度)しっかり押さえて頂くようお願いします。
Q10.採血の後が青くなったけど?
A. 前述したように、採血後の押さえがしっかりしていないと、血液が皮下にもれて内出血をして青くなります。また、血管が細い人などの場合、採血技術も難しくて多少血管を傷つけてしまうこともあります。 特に痛みや熱などの無い場合は、そのままおいておけば血液が少しずつ細胞に吸収されていき、そのうち色が消えていきます。その際青あざが黄色く変色することがありますが、吸収される過程で赤血球の色素が変化しているだけですからご安心下さい。きれいになるのに1~4週間程度みてください。
Q11.採血の時とても痛かったです?
A. 痛い思いをさせて申し訳ありません。採血行為は採血針を刺すため、多少の痛みは生じてしまいます。採血時に激しい痛みがありましたら採血者にお知らせください。採血を中断します。殆どの痛みは採血が終われば無くなっていきますが、もしも採血後の続く強い痛みや手指までに拡がるシビレ等がある場合は、神経を損傷している可能性があります。 私達採血者は、常に細心の注意を払って採血業務を行っていますが、神経の走行は個人差が大きく、外からはその走行を確認することが出来ないため、神経損傷を100%回避出来ないのが現状です。 神経損傷は約1万回~10万回に1回の頻度で起こると言われており、通常の採血では損傷は軽度で症状は軽く一時的な事が殆どです。痛み、しびれが続く場合も、大抵は数日~1ヶ月以内で治まりますが、ごく稀に数ヶ月以上疼痛の続く場合があります。 もしも、このような症状がある場合は採血スタッフへ申し出てください。 スタッフ一同細心の注意を払って採血をおこないますが、気になる症状がありましたらお申し出ください。 また、採血に関して疑問に感じることや聞きたいことがあれば、遠慮無くスタッフへお聞きください。
検査部ニュース
学術関係報告
論文発表
- 平成25年9月11日
2013年日中港澳 院内感染対策学術研究会 中国 広州医学院第一附属病院
講師:竹川啓史:感染症診断、治療における臨床検査技師の役割と機能について - 平成25年9月14日
KMI第47回例会 大阪ナレッジキャピタル
講師:竹川啓史:感染制御システムについて - 平成25年9月15日
平成25年度感染管理認定看護師教育課程 日本看護協会 神戸研修センター
講師:竹川啓史:培養困難微生物・真菌について - 平成25年9月18日
細胞検査士養成講習 兵庫県臨床検査技師会 研修センター
検鏡実習:原留 成和 - 平成25年9月22日
平成25年度感染管理認定看護師教育課程 神戸大学医学部保健学科
講師:竹川啓史:真菌について - 平成25年9月28日
市民公開講座講演会 神戸市西区民センター
講師:原留 成和:病理検査と乳腺腫瘍
講師:簔輪 和士:乳腺の超音波検査-乳腺を診よう- - 平成25年10月19日-20日
第53回 日臨技近畿支部医学検査学会 福井
学術奨励賞受賞:野本奈津美:6カラーフロサイトメトリーを用いた形質細胞性腫瘍のイムノフェノタイピング
発表:野村菜美子:特徴的な理学的所見を示した感染性心内膜炎の一例
発表:濱田充生:ASSRで一側性難聴を示しCT、MRで蝸牛神経管の狭窄または蝸牛神経形成不全を認めた9例
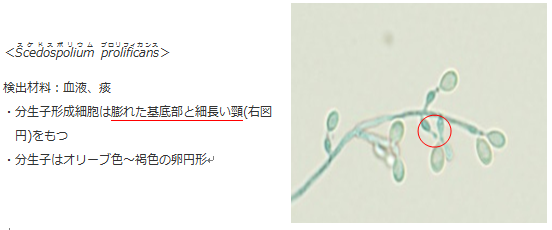
発表:内藤拓也:血液培養からScedospolium prolificansを検出した1例
発表:菅原雅史:限局型自己免疫性膵炎のUSにおける特徴的な膵管所見:膵癌との比較検討から
発表:宮本淳子:当院での救急部研修医向けグラム染色研修の取り組み - 平成25年11月9日
日本超音波医学会第40回関西地方学術集会 大阪
講師:岩崎信広:消化管 Screening超音波の系統的な手順―ピットフォールを回避するには?―
発表:成田祐美:US上、特に脂肪肝に合併して認められる肝血管腫周囲の低エコー部分についてのretrospectiveな検討
発表:三羽えり子:異物が原因と考えられる胃壁内膿瘍形成が疑われた1床例
発表:岩崎信広:小腸腫瘍性病変の超音波像について
発表:野本奈津美:三次元経食道心エコー図検査が左房粘液腫の診断に有用であった一例
あとがき
ズボラな性格の私が香丁木(コチョウギ)という小さな盆栽を育て始めました。枯らせてしまわないか不安でしたが、寒くなってもどんどん成長していく姿にいつの間にか愛情がわいてきてせっせとお世話をしては新しい葉が出ているのを見つけて喜ぶ毎日です。この木は春になると薄紫の花を咲かせるそうです。冬の間一緒に春を待ちたいと思います。(M.N)
検査相談室~患者サービスの向上を目指して~
検査情報管理室 山城明子
検査相談室は臨床検査技術部の業務の統計処理、検査システムの保守管理、臨床研究・治験業務の支援、委託業務の管理や運用の調整などを担う検査情報管理室の中にあります。
今回は検査相談室の業務をご紹介します。
院内職員からの臨床検査にかかわる問い合わせの窓口を一元化することにより、病院内の総ての臨床検査業務が円滑に機能することを目的として開設されました。下記のグラフは2007年の開設から2013年までの6年間の検査相談室への問い合わせ件数で、内容により質問・相談・要望・クレームに区別しています。5年目は新病院移転に伴った電子カルテ導入などのシステムや運用の変更により件数が大幅に増加しています。要望やクレームの内容に関しては部内で検討し、改善できることは対応してきました。この件数の中にはわずかですが患者さんからの問い合わせも含まれています。
今回は患者さんからの要望やクレームにより改善した事例を紹介します。
- 採血本数の減少 当院のような総合病院では並行して複数の診療科に受診されている方がいらっしゃいます。 新病院移転前は、複数科受診で同じ日に採血する際、同じ採血管であっても検査項目が異なる依頼の場合は 同一の採血管で数本採血することがありました。採血時に患者さんから『採血本数が多い』とのクレームもありました。 そこで、新病院移転に伴い、検査部門システムで採血管集約機能を入れ、外来採血時には採血管を集約して 採血本数を最小限にすることで、患者さんの負担軽減を実現しました。
- 2) 検査インフォメーションの発行 近年、患者さん自身の医療に対する関心が高くなっているため、外来採血室等で患者さんより検査項目の説明を求められる機会が多くなりました。 これに対応するために、検査項目・略語・項目の説明・基準範囲等を載せた検査インフォメーションを発行し、 採血室や診察受付等に置いて必要な患者さんにお配りするようにしています。
このように患者さんからのご意見を参考に業務改善やシステム改修を行い、患者サービスの向上に繋げることができました。現在でも公式には患者さんからの問い合わせには対応していませんが、将来的には検査の説明などを実施していければと考えています。
検査部ニュース
学術関係報告
学会発表
- 竹川啓史、大楠清文、内藤拓也、仁木真理恵、﨑園賢治:血液培養液の16SrRNA遺伝子解析によって迅速に同定されたHelicobactoer trogontum感染症の一例.第25回日本臨床微生物学会総会.名古屋.2014.2.1
- 仁木真理恵、丸岡隼人、竹川啓史、内藤拓也、﨑園賢治:Hybridizaion probe・Melting curve法を用いたMycobacterium kansasiiの検出. 第25回日本臨床微生物学会総会.名古屋.2014.2.1
論文発表
- Maruoka H, Inoue D, Takiuchi Y, Nagano S, Arima H, Tabata S, Matsushita A, Ishikawa T, Oita T, Takahashi T. IP-10/CXCL10 and MIG/CXCL9 as novel markers for the diagnosis of lymphoma-associated hemophagocytic syndrome. Ann Hematol. 2014 Mar; 93(3): 393-401.
あとがき
一雨ごとに暖かくなり、確実に春の訪れが近づいているようです。近づくにつれ、定年退職される方との勤務も少なくなり寂しい日々が続いています。諸先輩方の”てかり”を絶やさないように精進していきたいと思います。花冷えする季節ですので、暖かくしてお休みください。(H.T)
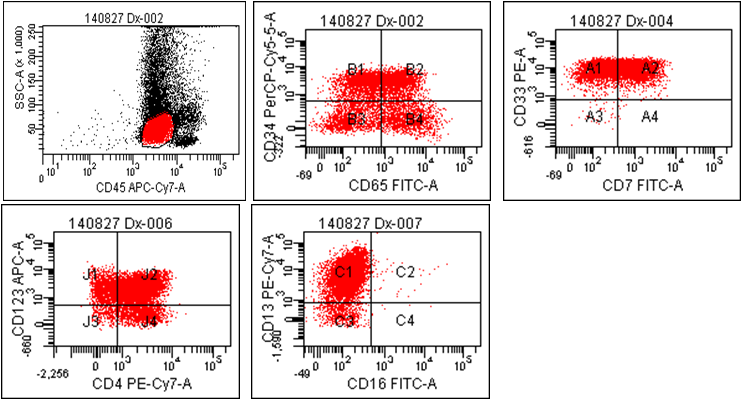
キメリズム検査について
細胞遺伝子検査室 吉田昌弘
キメリズム検査とは
まず、キメリズムと聞いて何を思い浮かべるでしょうか?流行りのエクササイズ!?
今回紹介するキメリズム検査とは、正常な血液細胞を作ることが困難な疾患(白血病、再生不良性貧血等)の患者さんに対する治療法の一つである造血幹細胞移植において、ドナー(提供者)の血液細胞がレシピエント(患者さん)の体にどの程度生着*1したのか、主に移植後の生着確認の指標として用いられる検査です。
そもそもキメリズムというのは、ギリシャ神話にでてくるキマイラが語源となっています。 キマイラとはライオンの頭と山羊の胴体、蛇の尻尾をもち、複数の生物が合成された聖獣です。移植後にドナーとレシピエントの血液細胞が組み合わさることからキメリズムという名前がついたと言われています。
移植後にドナーの血液細胞が本当に生着したのかどうか、一体どのようにして確認するのでしょうか?
移植前検査
ヒトのDNAの中には数塩基~数十塩基が繰り返された配列が多数存在し、その中でも比較的短い塩基配列の繰り返しをSTR(Short Tandem Repeat)と呼びます。これは個人によって異なるので、複数のSTRローカス(遺伝子座)の長さを調べることで個人を識別することができます。移植前にあらかじめ検査して、このSTRという個人を識別するための目印を決めておく必要があります。このSTR解析は、犯罪捜査におけるDNA鑑定や親子鑑定にも用いられている検査です。
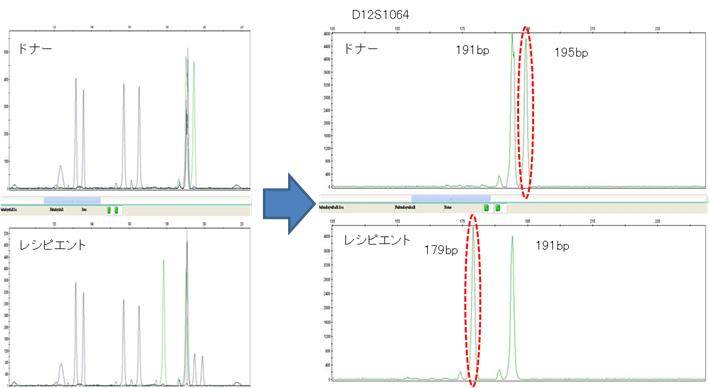
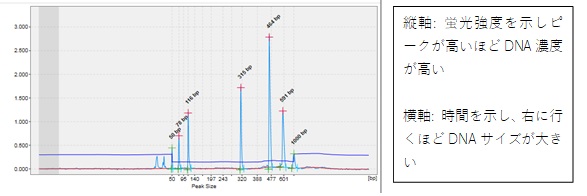
あらかじめ移植前にドナー、レシピエントの血液を採取し、複数のSTRローカスをターゲットとしたMultiplex STR-PCR法を用い、DNAを増幅させてSTRローカスを検索します。それが下の左図です。その中からドナーとレシピエントを明確に識別できる特有のSTRローカスを選択します。それが下の右図です。
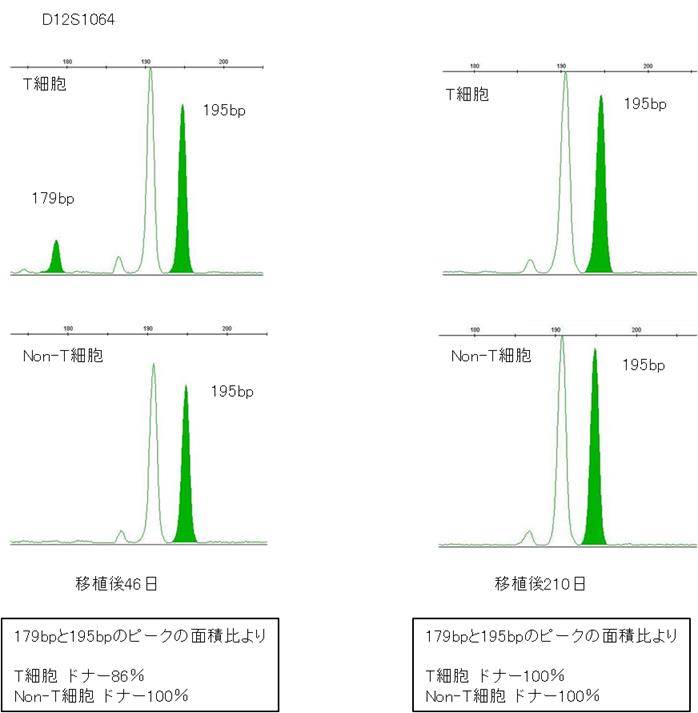
本例の場合、「D12S1064」というSTRローカスにおいて、ドナー195bp、レシピエント179bpと長さが異なるので目印として使用することが可能です。移植後はこのローカスのドナーピーク195bpとレシピエントピーク179bpを見ていくことになります。
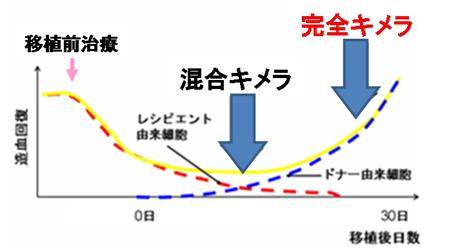
移植後キメリズム検査
造血幹細胞移植をすると、移植後の体内にはレシピエント由来とドナー由来の血液細胞が混在します。この状態を混合キメラといいます。その後ドナーの血液細胞がしっかり生着すると、レシピエントの体内においてレシピエントの血液細胞が消え、ドナーの血液細胞だけになります。このようにドナーの血液細胞がレシピエントに生着した状態を完全キメラといいます。
移植後は、このような生着の段階を確認する為に検査を実施します。検査は血液中のTリンパ球(T細胞)とTリンパ球以外の細胞 (Non-T細胞)に分けてそれぞれ解析をします。これは両者で解離がみられることがあり、移殖後の早期の生着、GVHD(移植片対宿主病) *2sup>、抗腫瘍効果など有意義な情報を得ることができるからです。
T細胞とNon-T細胞それぞれから採取したDNAをSTR-PCR法で増幅し解析を行います。
移植前に目印とした「D12S1064」というSTRローカスのドナーピーク195bpとレシピエントピーク179bpを検査することで、それぞれのピークの面積比からドナー由来の血液細胞がレシピエントの体内に何%生着したのかを確認することが出来ます。
上の左図は移殖後46日にキメリズム検査を実施した結果です。Non-T細胞ではドナーの195bpだけのピークなので面積比から計算しドナーが100%となります。一方、T細胞ではドナーの195bpのピークがほとんどですが、レシピエントの179bpのピークも若干見られます。面積比から計算した結果ドナーが86%となりました。
移殖後210日の検査結果が上の右図です。T細胞・Non-T細胞共にドナーの195bpのピークのみとなっておりレシピエントのピークは検出されていません。面積比から計算したドナーも100%となりドナーの血液細胞が完全に生着したといえます。
院内でキメリズム検査を実施するメリット
院内においてキメリズム検査を実施している施設は全国的に見ても少数です。外注検査では検査報告まで1~2週間かかることが多いですが、当院では院内検査を実施することにより、翌日に報告が可能となります。
移植後早期からキメリズム検査を実施することで、ドナーの血液細胞の生着確認をリアルタイムに判定することができます。また、拒絶の傾向を示した患者さんにも迅速な対応をとることができ、その後の治療方法の選択にもつながります。
当院の細胞遺伝子検査室は、血液内科の医師と密接な関わりがあり、血液内科と隣り合わせに検査室を構えることで情報を共有し、結果の報告や病態に応じた検査項目の変更や追加などの即時対応が可能となります。また、検査結果のカンファレンスなども随時行っています。
そして、このような環境下で新たな検査を積極的に導入し、さらに医師との連携を高めて、患者さんに安心できる質の高い医療を提供すること努めていきたいと考えています。
語句説明
*1生着:ドナーの造血幹細胞がレシピエントの骨髄に根付くこと。
*2GVHD(移植片対宿主病):ドナーから提供された移植片がレシピエントの身体や臓器そのものを敵とみなして攻撃する免疫反応。
検査部ニュース
学術関係報告
学会発表
- 1.野本奈津美、谷知子、紺田利子、角田敏明、川井順一、金基泰、北井豪、古川裕、北徹:当院における過去14年間での心臓腫瘍症例における心エコー図検査での検討.第78回日本循環器学会学術集会,東京,2014.3.22
- 2.尾松雅仁、原留成和、井本秀志、坂本紀子、森田明子、上原慶一郎、今井幸広:Pneumocystis jirovecii 感染7例の細胞像.兵庫県臨床細胞学会第30回総会.神戸.2014.3.15.
- 3. 紺田 利子、谷知子、藤井洋子、川井順一、金基泰、北井豪、古川裕、北徹:僧帽弁逸脱による重症僧帽弁逆流症例におけるMitral Annular Disjunctionについての検討.第78回日本循環器学会学術集会,東京,2014.3.21
あとがき
先日、願い事が叶うといわれている京都のあるお寺へ行ってきた。住所と名前と願い事を一つ唱えると、わらじを履いたお地蔵様が家まで来て、願いを叶えてくれるそうだ。願いを唱える前に住職のありがたい説法を聞いた。その中で「生まれて死ぬまで人は誰かと関わりながら生きているので『おかげさま、お世話様、お互い様』の言葉を忘れずに謙虚な心でいなければならない」といった内容があった。ふと自分を振り返ってみると忙しい毎日でこれらの言葉をあまり使っていない自分に気づいた。自分を見つめなおし、謙虚な心で日々精進していけば、きっとお地蔵様が家に来て、願い事を叶えてくれると信じている。(N.M)
検査室を飛び出そう!-ベッドサイド検査の現状-
神経機能検査室 中村 真実子
はじめに
生理検査室では、通常患者さんに検査室に来ていただき検査を実施しています。
しかし、さまざまな理由で患者さんが検査室に来ることができないケースがあり、その際、臨床検査技師が患者さんのもとへ伺って検査をしています。このような場合、検査室とは異なる環境であり検査を実施するにあたってさまざまな工夫が必要となります。
今回は、腹部・神経機能検査室の臨床検査技師が検査室を飛び出してどのように検査をしているのかベッドサイド検査を中心に紹介します。
出張する場所と実施している検査の種類
検査室を出て検査する場所として最も多いのはICU(集中治療室)などの重症部門です。ICUの患者さんは容態が不安定であることが多く、また多くの点滴や人工呼吸器などの医療機器を必要としているため検査室への移動が極めて困難であり危険を伴います。そのため検査技師が検査の機械をもって病室に出張して検査しており、これはベッドサイド検査あるいはポータブル検査と呼ばれています。腹部・神経機能検査室では脳波検査、腹部超音波検査、血管超音波検査、神経機能検査などでベッドサイド検査を実施しています。
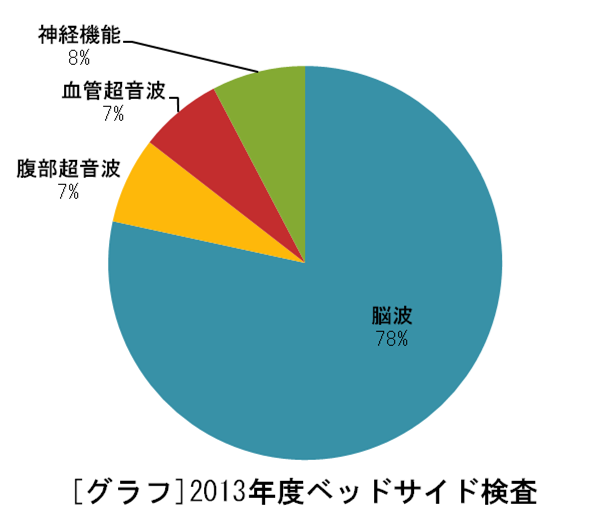
[グラフ]は2013年度のベッドサイド検査の割合を検査種ごとに示したものです。2013年度の総数は14,991件でその内ベッドサイド検査は338件実施されていました。当院では圧倒的に脳波検査の件数が多く、これは重症部門に入院されている患者さんはしばしば意識障害を伴っており脳波検査が意識障害の精査として依頼されるためだと考えられます。
神経機能検査も同様に脳機能の検査として依頼され出張することが多いです。
腹部超音波検査は主に肝臓、胆嚢、胆管などの評価、血管超音波検査は下肢深部静脈血栓(長期臥床等が原因で足の静脈にできる血栓)の探索の依頼が多いです。
検査室で行う検査との違い
検査室とそれ以外の場所で検査するのはどのような違いがあるのでしょうか。ベッドサイド検査の最も多い脳波検査を例に挙げて紹介します。
(1)検査機器
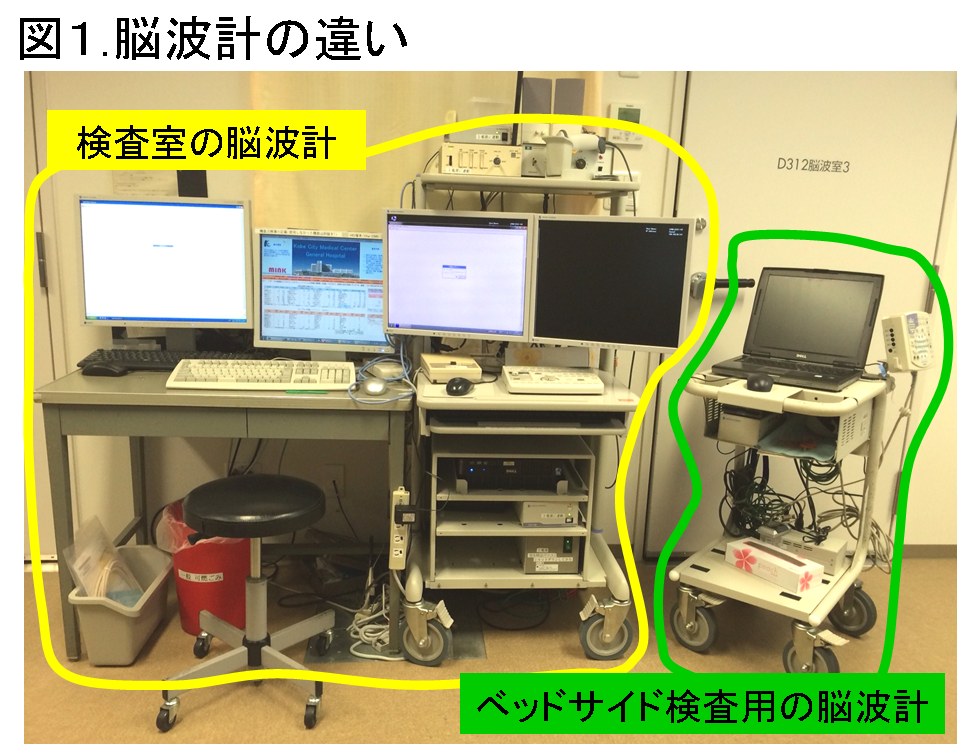
ベッドサイド検査を行うにはまず検査機器を運ばなければなりません。検査室で使用している脳波計は大型で容易に運ぶことができないため、ベッドサイド検査では一人で簡単に移動できる小型の脳波計を使用しています(図1)。
機械が小型であることは病室の限られた空間で検査する際にも他の医療機器等の邪魔にならず便利です。しかし、当院のベッドサイド検査用の脳波計には患者さんの状態を記録するビデオカメラが装備されていないため、検査技師が検査時の状態をメモにとるなどして詳細に記録する必要があるなど、機能面において検査室の脳波計より劣る部分があります。
(2)環境
通常、脳波検査はシールドルーム(図2)と呼ばれる部屋で実施しています。
この部屋は脳波検査にとってアーチファクト(本来記録されるべき脳活動以外を由来とする波形)の原因の一つである電磁波を遮断することができ、脳波の記録には最適な環境です。一方、ベッドサイド検査をすることの多いICUには医療機器をはじめとするアーチファクトの原因が多く存在し、脳波検査にとって必ずしも良い環境とはいえません。そのため、病棟スタッフに電源を切ることができる機器はコンセントを抜いてもらったり、電源を切ることのできない機器は患者さんからできるだけ距離をとるなどして、検査にとってできる限り良い環境に近づける工夫をしています。
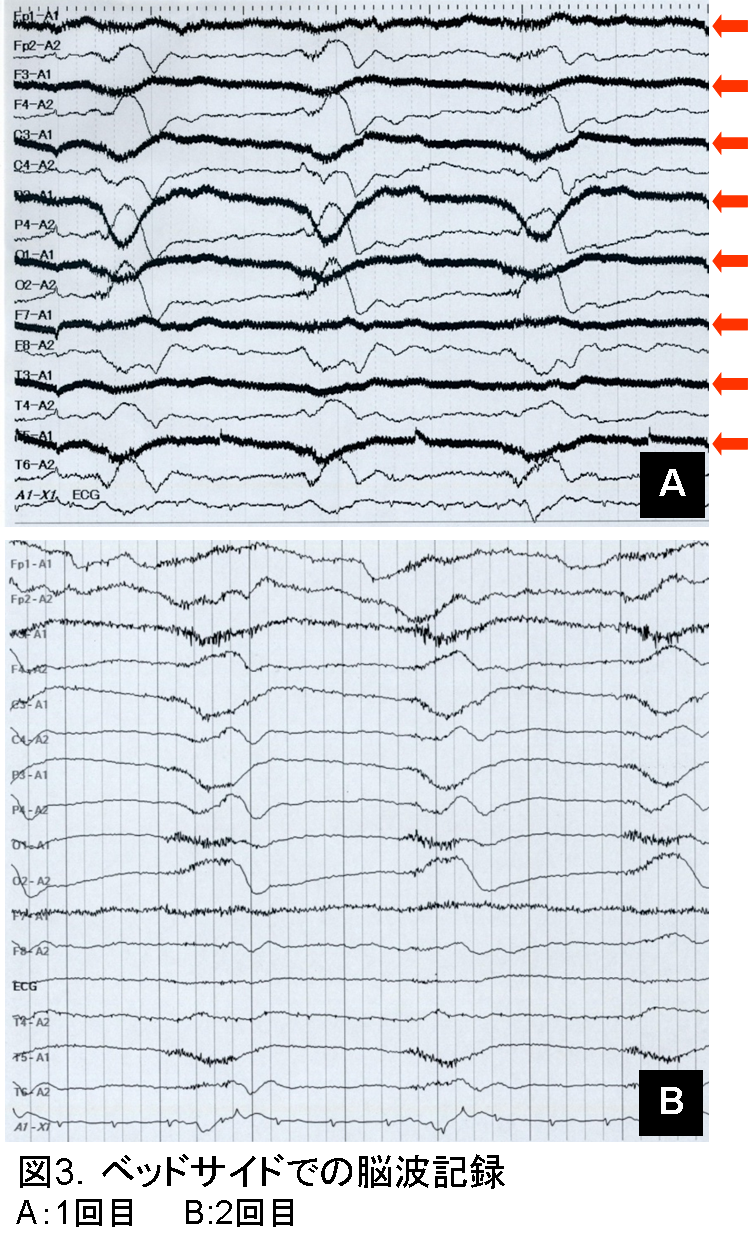
図3Aはベッドサイド検査にてアーチファクトが著明に混入した脳波です。線が太くなっているように見える部分(矢印)がアーチファクトの著明な部分で、これらはすべて頭の左側に装着した電極で記録されたものです。これでは本来の患者さんの脳波を判読することができず検査をした意味がありません。
ここからが検査技師の腕の見せ所です。波形からアーチファクトの主な原因が交流障害であろうと予想し、前述したような対策を講じました。しかし、脳波を判読できる程アーチファクトを除去することができなかったため、隣室やナースステーションなど病室外の環境の影響であろうと考え、時間をあらためて再検査することにしました。
図3BがAの約4時間後に再検査して記録された脳波です。Aと比較してアーチファクトが軽減しており、判読が可能です。おそらく病室外の電気的な環境が変化したためアーチファクトが軽減されたと考えられます。
このようにベッドサイド検査では検査技師の知識や経験が必要となる場面があり検査室での検査の”応用編”ともいえます。
臨床検査技師が検査室を飛び出すこと
検査室で仕事をしていると他職種のスタッフと関わることが少ないですが、ベッドサイド検査では患者さんの体を支えてもらったりアーチファクト対策に協力してもらうために 病棟スタッフと必ずといっていいほど関わりを持ちます。
他にも検査について質問されたり、私たちも分らないことを聞くなどしてお互いの知識を交換することもあり、専門外のことを学ぶことで視野が広がるというメリットがあります。検査室の検査では診療の中の検査の部分しか実際に見ることができませんが、検査室の外に行くことで視野が広がり、検査が医師の診察や看護師のケアなどを含めた大きな診療の流れの一つであることを実感できます。
その中でどのような検査をしたら患者さんの診療に役立てるのかを考えるきっかけとなり、臨床上有用な検査結果を報告する意欲へとつながると思います。また、普段あまり見ることのない検査技師の仕事を病棟スタッフに見てもらうことで検査技師という職業を知ってもらう良い機会にもなっていると考えられます。
このような職種間の相互理解が少しでもあるとスタッフ間の連携がスムーズになり患者さんの診療もよりスムーズに進めることができるようになります。
おわりに
ベッドサイド検査を中心に検査室以外での業務について紹介しました。ベッドサイド検査は今回紹介した脳波検査に限らず、装置や環境が検査室とは異なり、さまざまな工夫を要するため検査室での検査より大変な部分があります。しかし、病棟スタッフとの関わりを持つことで視野が広がり、相互理解を深める機会にもなっています。ベッドサイド検査以外にも感染対策チーム(ICT)や栄養サポートチーム(NST)、術中神経モニタリングなど検査室を飛び出して行う業務が多くあります。
いずれもさまざまな職種のスタッフの中で検査技師の専門性を発揮できる領域を見つけて活躍しています。この他にも病院の中で検査技師の力が必要とされ発揮できる場所を積極的に見つけていきたいと思います。
検査部ニュース
学術関係報告
論文発表
- 山城明子、菅沼直生子,柴田洋子、田村明代、老田達雄:検査相談室開設後6年間の報告.医学検査 63:366-373,2014
学会発表
- 森田明子,井本秀志,丸岡隼人,老田達雄,上野寿行,丹羽欣正:当院で経験した小腸浸潤を認めた慢性骨髄単球性白血病(CMML)の一症例. 第63回 日本医学検査学会,新潟,2014.05.17-18
- 田村明代,那須浩二,角田敏明,森田明子,仁木真理恵,内藤拓也,野本奈津美,中村真美子,成田祐美,老田達雄:当院臨床検査技術部における医療安全チームの取り組み. 第63回 日本医学検査学会,新潟,2014.05.17-18
- 岩崎信広:シンポジウム消化管超音波検査の進歩-腫瘍性疾患の超音波診断-目標とすべき診断レベル. 日本超音波医学会第87回学術集会、横浜、2014.5.11
- 成田祐美、杤尾人司、杉之下 与志樹、鄭 浩柄、今井幸弘、田村明代、岩崎信広、濱田一美、箕輪和士、猪熊哲朗:超音波にて肝血管腫の周囲に見られる低エコー域についての検討 日本超音波医学会第87回学術集会、横浜、2014.5.11
- 竹川啓史:真菌の基礎から臨床.福井県臨床検査技師会.福井.2014.7.12
- 竹川啓史:真菌同定の重要性 ~Exophiala dermatidisの症例を経験して~ .平成26年度近畿地区微生物合同研修会.大阪.2014.8.30
- 岩崎信広:やってみたくなる!消化管エコー-小腸疾患を中心に. 第5回小児小腸内視鏡研究会, 大阪, 2014.7.6
- 岩崎信広:消化管の超音波検査 –TURUGI-. GE Ultrasound seminar 大阪, 2014.7.13
- 岩崎信広:消化管の超音波検査 –TURUGI-. GE Ultrasound seminar 東京, 2014.8.3
- 川井順一:EPIQの使用経験と3次元心エコー法の活用.関西Structural Heart Diseaseセミナー 大阪,2014.8.9
- 川井順一:ぜん息・COPDの予防等に関する講習会 スパイロメータを用いた肺年齢測定実習について.神戸市・独立行政法人環境再生保全機構(予防事業部)神戸,2014.8.25
あとがき
臨床検査技術部のHPが新しく出来てから約2年半が経ちました。更新も今回でようやく10回目です。3ヶ月に一度の更新ですが、更新を重ねるごとに”TEKARI“がよりてかてかと輝くように、自分自身も磨き、より良い情報を発信していきたい。 (O.M)
カビと臨床検査
微生物検査室 内藤 拓也
夏には食中毒(O-157など)が発生しやすく、冬ではインフルエンザといった感染症が流行します。感染症は一般細菌やウイルスが多くを占めていますが、 細菌の中でも「真菌」によって起こる感染症もあります。 真菌は糸状菌、酵母に大きく分類でき、水や土壌、空気、動物などの環境中に多くが存在していることから菌を吸い込む肺や傷口といった皮膚からの感染が見られます。
糸状菌とは??
菌類のうち、菌糸と呼ばれる管状の細胞から構成されるものの総称です。
いわゆるカビやキノコをイメージしてもらえれば分かりやすいのではないかと思います。
何だか汚いイメージしか浮かんでこないですが、日本では食卓に欠かせない酒や味噌、 醤油に大昔から使われ、現在でも医薬品として使用され続けていることからも、人類はカビと共生してきました。(ex. 泡盛⇒アワモリコウジカビ、抗菌薬⇒ペニシリン など)
足の指や足底、爪に発症するあの水虫もTrichophyton rubrum(トリコフィトンルブラム)などといった糸状菌による感染症です。
感染部位によって深在性(内臓)真菌症、深在性(深部)皮膚真菌症、および浅在性(表在性)真菌症に分類され、代表される疾患には ①アスペルギルス症、②カンジダ症、③クリプトコッカス症が挙げられ、特に免疫力が低下している易感染者の場合に重篤な真菌症を引き起こしやすくなります。
今回は真菌の中でも糸状菌について、その検査法を紹介します。
糸状菌の検査
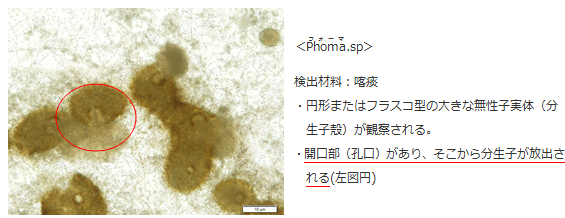
1.肉眼的観察
1)ジャイアントコロニー の作製
患者さんの検体(痰、皮膚、血液など)を培養し、培地にジャイアントコロニー(巨大で単一の菌塊)を発育させる事で、その発育速度や色(裏表)、 コロニー表面の状態、菌糸の状態などを観察します。一般細菌の多くは24時間程度で発育しますが、糸状菌は数週間かかる場合もあります。菌種によって発育条件(発育温度、培養時間)を考えながら行います。
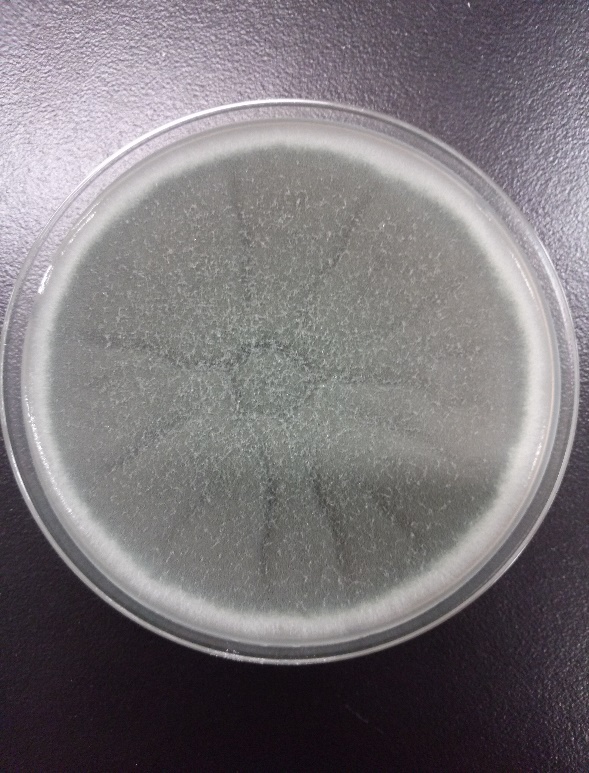
・綿状
・初めは白色で、後に灰色または淡灰色~黒色
・発育速度は速い
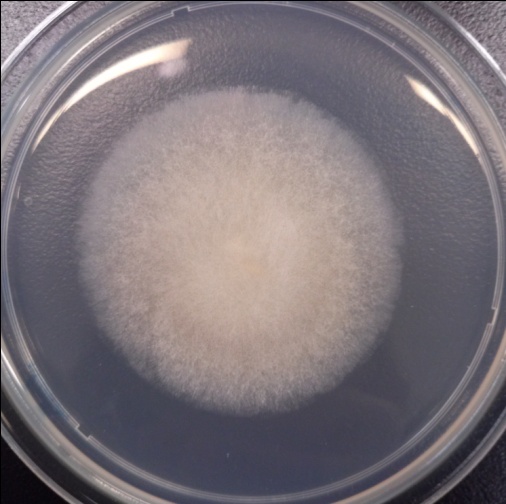
・若いコロニーは綿状、または湿潤、淡灰色~黒色
・成熟すると暗褐色~黒色
・古くなると白色の菌糸体が生じる
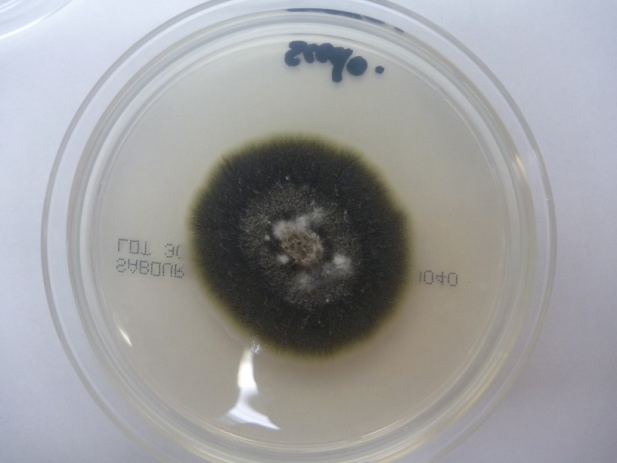
・白色の綿状から、やがて暗灰色~黒色に変化
・発育速度は速い
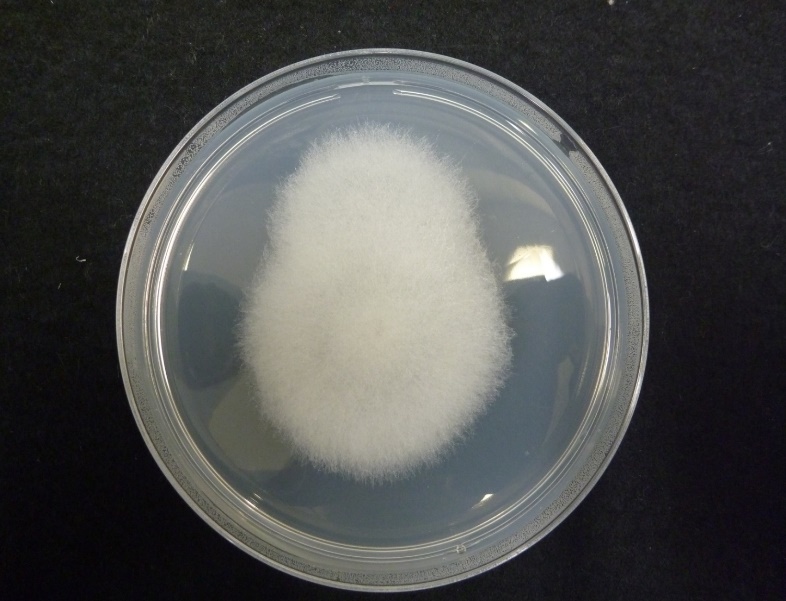
・表面はビロード状または粉末状
・辺縁は幅の狭い白い帯状
・裏面は白色~黄褐色
2.顕微鏡的観察
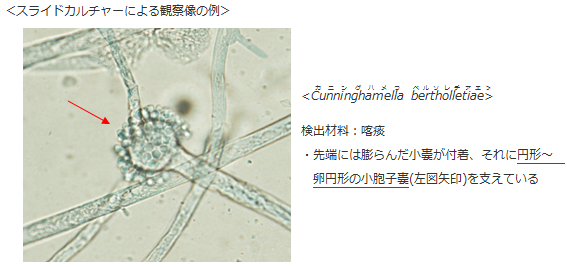
顕微鏡による観察では菌糸の状態、分生子(菌が形成する胞子)の大きさ・形・構造などといった形態を確認します。 例えば、下図のたんぽぽの綿毛が飛んでいるようにも見える菌はAspergillus属ですが、Aspergillus属であればいくつかのポイントを確認して菌名を同定します。
①分生子頭が円柱状か放射状か
②アスペルジラが単列か複列か
③細胞壁が滑面か粗面か
④分生子丙の色調が無色か褐色か
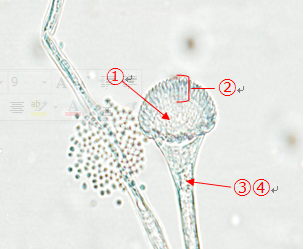
このように、分生子がどのように形成されているかを顕微鏡で観察するために、以下のような方法を行っています。
1)直接塗抹法(セロテープ法、捺印法)
培地に発育したコロニーの胞子をセロテープにくっつけ、スライドガラス上でラクトフェノール・コットンブルー液(染色液)を用いて染色します。直接塗抹法は非常に簡便で迅速に形態を観察する事ができます。
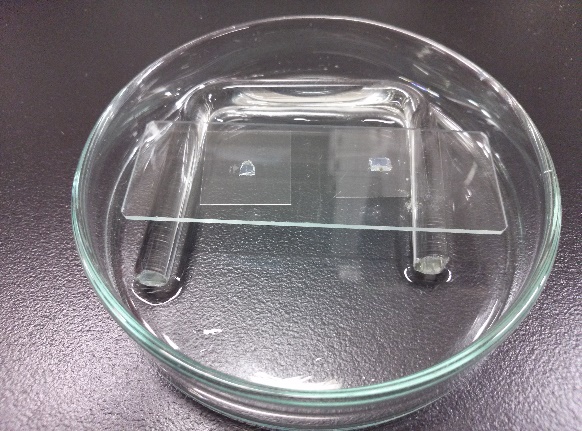
2)スライドカルチャーの作製
スライドガラス上の約5mm角の寒天培地に菌を接種し、培養の後に菌が付着したカバーガラスを顕微鏡で観察します。スライドカルチャーを作製すると時間はかかりますが、菌糸や分生子の形態的特徴をよりきれいに菌糸や分生子の形態的特徴を観察することができます。さらにカバーガラスの周囲をマニキュアなどで封入(空気を遮断して密閉)することで長期間標本を保存することができます。
3.薬剤感受性
菌の発育が見られるところでは、菌の生成する酸化還元酵素により指示薬の色調が青⇒赤(菌が発育:抗菌薬の効果がない濃度)に変化することを利用してどの薬がどの濃度であれば効果があるかを判定しています。真菌症治療薬が予め塗布されているパネルへ、規定濃度に調整した菌液を分注して培養にかけます。通常であれば培養から24時間で中間判定、48時間で最終判定を行います。
4.まとめ
真菌の場合は発育が遅い菌種であったり、顕微鏡による観察も経験が必要ですぐに同定できるとは限りません。しかしながら、真菌の中には効果がある薬が限られていたり、効果があった薬が効かなくなっている場合(耐性化)もあります。特に深在性真菌症や血流感染の場合は迅速な同定が求められ、当院では分子生物学的方法により遺伝子配列から菌を同定することも併用しています。
以前にも増して臨床検体から真菌を分離・同定しなければならない傾向にあり、一般に真菌は馴染みのない菌名や形態ばかりで戸惑うことの方が多いのが現状です。しかし、これからも希少な真菌に遭遇する可能性は十分に考えられます。治療へ迅速に貢献できるよう、更なる努力で技術や知識の向上を目指していきます。
参照
- 病原真菌同定の指針 奥平雅彦 文光堂 1986
- 医真菌 同定の手引き(第5版) D.H.ラローンほか 栄研化学株式会社
- http://www.bdj.co.jp/safety/articles/ignazzo/hkdqj2000005r4ix.html
検査部ニュース
学術関係報告
学会発表
- 丸岡隼人:血液シンポジウム フローサイトメトリーによるイムノフェノタイピング. 第54回日臨技近畿支部医学検査学会 神戸国際会議場 2014.9.20
- 吉田昌弘, 丸岡隼人, 藤原容子, 那須浩二, 老田達雄:悪性リンパ腫における免疫グロブリンL鎖再構成の検出系の確立. 第54回日臨技近畿支部医学検査学会 神戸国際会議場 2014.9.21
- 森田明子, 堀香菜, 菅原雅史, 坂本紀子,松浦亮一郎,井本秀志,田村明代,老田達雄:当院での肺多形癌(Pleomorphic carcinoma)の細胞学的検討. 第54回日臨技近畿支部医学検査学会 神戸国際会議場 2014.9.21
- 堀香菜,森田明子, 井本秀志,松浦亮一郎,田村明代,老田達雄:EBER-ISHにおける後固定の有用性の検討 第54回日臨技近畿支部医学検査学会 神戸国際会議場 2014.9.20
- 成田祐美, 栃尾人司, 濱田充生, 簑輪和士, 老田達雄:超音波検査で指摘し得た下腰ヘルニアの一例. 第54回 日臨技近畿支部医学検査学会 神戸国際会議場 2014.9.21
- 川井順一:【活用編】他メーカからのシステム更新と現在の運用(次期部門更新に思うこと). 第1回関西Vitaセミナー(生理検査部門システムフォーラム) グランフロント大阪ナレッジキャピタル 2014.9.13
- 森本美咲,竹川啓史,野上美由紀,内藤拓也,野村菜美子,﨑園賢治、田中佑果:Syncephalastrum racemosumによる人工膝関節津感染の1例.第54回 日臨技近畿支部医学検査学会 神戸国際会議場 2014.9.21
- 松下隆史:膵或いは膵周辺に腫瘤を形成した腹部悪性リンパ腫の1例. 第114回腹部超音波カンファレンス 2014.10.30
- 玉木恵里子:膵NETの1例. 第114回腹部超音波カンファレンス 2014.10.30
- 登阪貴子:膵外傷の1例. 第114回腹部超音波カンファレンス 2014.10.30
- 岩崎信広:消化管の超音波診断. 第114回腹部超音波カンファレンス 2014.10.30
- 岩崎信広:消化管エコーの光と影. 消化管エコーセミナー 大阪 2014.11.1
- 丸岡隼人, 吉田昌弘, 老田達雄, 石川隆之:Pfaffl法を用いたNPM1変異遺伝子の定量解析. 第61回日本臨床検査医学会学術集会, 福岡 2014.11.23
- 吉田昌弘, 丸岡隼人, 老田達雄:B細胞性悪性リンパ腫における免疫グロブリンL鎖再構成検査の有用性. 第61回日本臨床検査医学会学術集会, 福岡 2014.11.23
- 森田明子,丸岡隼人,老田達雄, 越智陽太郎,今井幸弘:乳腺に浸潤を認めたCD61陽性・MPO陽性のAMLの1例. 第61回日本臨床検査医学会学術集会, 福岡 2014.11.24
- 中野彩、谷知子、紺田利子、藤井洋子、中村仁美、三羽えり子、川井順一、菅沼直生子、野本奈津美、古川裕:重症度が異なるpradoxical low-flow low-gragient Aortic Stenosisの2例. 日本超音波医学会第41回関西地方会学術集会,京都,2014.11.22
- 宮本淳子、谷知子、紺田利子、藤井洋子、中村仁美、角田敏明、川井順一、菅沼直生子、野本奈津美、古川裕:心エコー図検査がStructural valvular deteriotation(SVD)の診断に有用であった2症例. 日本超音波医学会第41回関西地方会学術集会,京都,2014.11.22
- 栃尾人司、菅原雅史、今井幸弘、他:造影超音波の後血管相で転移性肝癌の周囲に見られるhyper enhance rim(HER)について:切除標本による病理組織学的検討. 日本超音波医学会第41回関西地方会学術集会,京都,2014.11.22
- 岩崎信広:(講演〉消化管エコーの光と影. 消化管エコーセミナー2014 in 大阪,2014.11.1
- 岩崎信広:(講演)画像診断におけるUSの役割-必要な知識と考え方- 第179回 大阪腹部超音波研究会,2014.11.14
- 松下隆史、栃尾人司、杉之下与志樹、他:急性胆嚢炎を契機に腹部USで発見し得た胆嚢癌~Mixed Adeno NeuroEndcrineCarcinomas(MANECs)の一例~本超音波医学会第41回関西地方会学術集会,京都,2014.11.22
- 玉木恵里子、栃尾人司、今井幸弘、木川雄一郎、他:「造影超音波検査を施行したmyeloid sarcomaの1例」日本超音波医学会第41回関西地方会学術集会,京都,2014.11.22
あとがき
最近めっきり寒くなりましたね。話題の爆弾低気圧がやってきて、朝起きるのがかなりつらくなってきたこの時期、皆様いかがお過ごしでしょうか。暑い時には熱いものを食べろとよく言いますが、寒い時にも熱いものはもってこいですよね。体の温まるものを食べると、外は寒くても体はポカポカです。特に冬は大人数で囲む鍋が最高ですね!大根おろしで好きなキャラを形作る3D鍋が近頃流行りのようですが、私たちはや はり王道の寄せ鍋が一番です。シメは雑炊でおなかいっぱいになるとなお良いですね。これで寒い冬を乗り切りましょう!!P.S.いつか神戸牛ですき焼きもしたいです☆ (M.K & K.H)
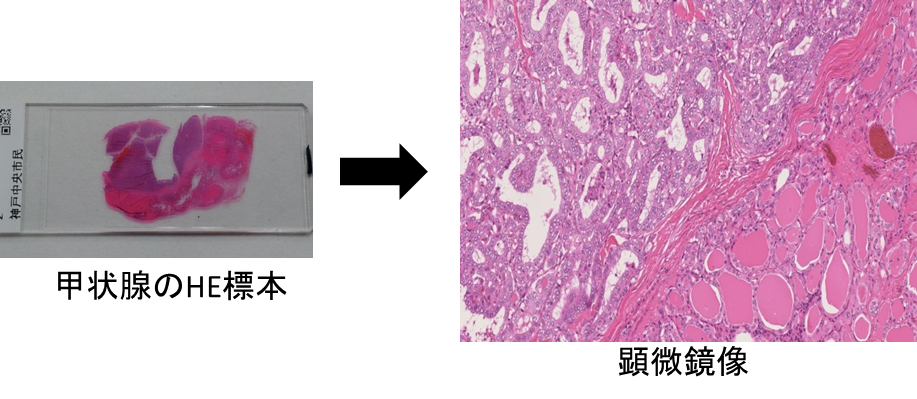
病理検査室の紹介
病理検査室 森本 美咲
病理検査とは、病変部から採取された組織や細胞を肉眼的・顕微鏡的に観察し、病気の診断(原因、良性・悪性の判定、進行度など)を行うことを目的としています。それでは実際に病理検査室でどのような検査が行われているのでしょうか? 病理検査には大きく分けて「組織診」と「細胞診」の2つがあります。それぞれの検査の流れを簡単にご紹介します。
組織診
組織診とは、病変部から採取した臓器や組織を標本にし、顕微鏡で観察することによって病気の診断を行うことです。
①固定・切り出し
内視鏡検査・外来などで採取された組織や手術で摘出された臓器は、ホルマリンという薬液につけて組織が傷むのを防ぎます(固定)。その後病理検査室に提出され、標本作製に適した大きさに切ります(切り出し)。
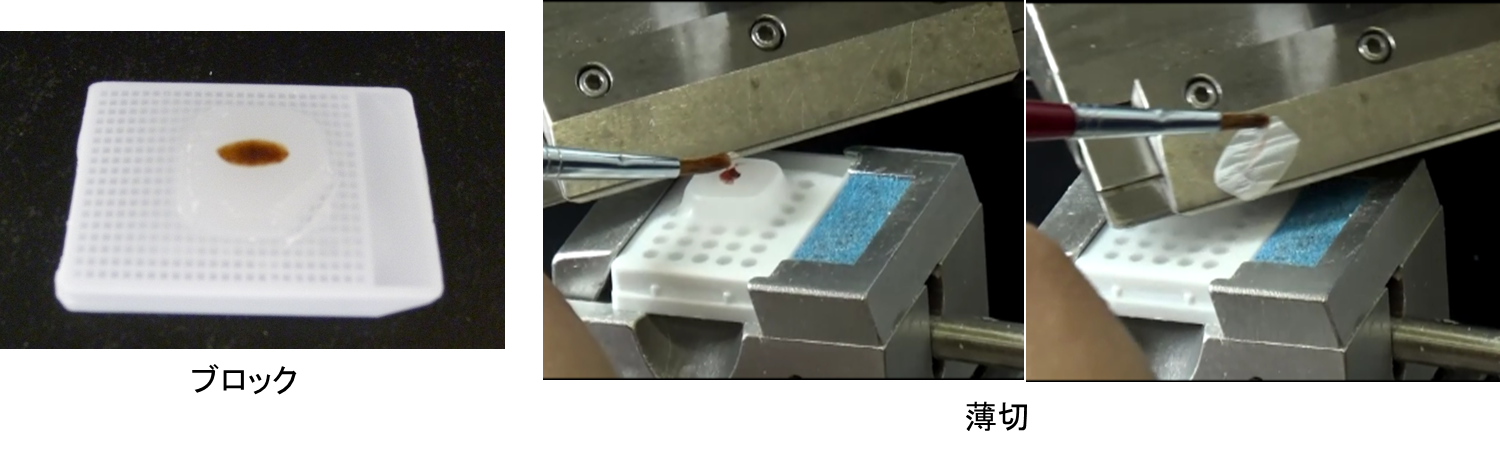
②包埋・薄切
切り出された組織をそのまま薄く切ることはできないので、パラフィンというロウの一種に組織を埋め込みブロックを作製します(包埋)。作製したブロックをミクロトームという機器を用いて約2~3μm( 1μmは1000分の1mm)の厚さに薄く切り、ガラスにはりつけます(薄切)。
③染色
組織や細胞の構造を観察しやすくするために、薄切した組織をさまざまな色素を用いて染色します。通常はヘマトキシリン・エオジン染色(HE染色)という染色を行いますが、必要に応じて、組織の特徴を観察するための染色(特殊染色、約40種類)や、組織や細胞に含まれる成分を染め出す染色(免疫染色、約100種類)を行うこともあります。
④鏡検・診断
出来上がった標本を病理医が顕微鏡で観察し診断します。
また、組織診では、手術中に病変部の良性・悪性の判定や摘出範囲を決めるために、組織の一部をとって検査する「術中迅速検査」も行っています。
手術室から検体が送られてくると、初めに病理医が切り出しを行い、その検体を専用の液体に埋め込み-80℃で急速冷凍します。出来上がったブロックを専用の機器で薄切し標本作製、染色を行った後、病理医による診断が行われます。標本作製時間は1組織10分程度と短く、迅速に診断を行うことができます。
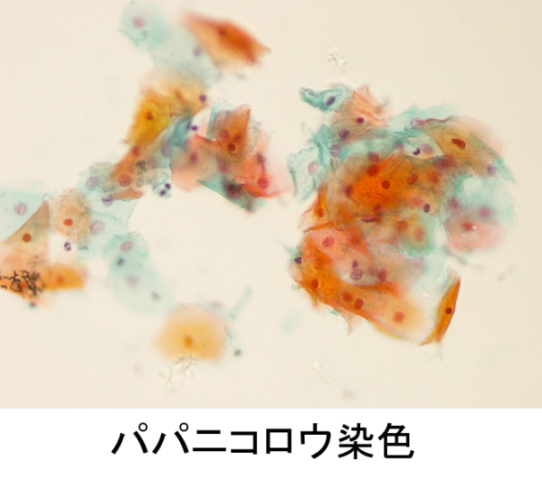
細胞診
細胞診とは、細胞一個一個、または細胞の小集団を顕微鏡で観察し、悪性細胞があるかどうかなどを調べることによって病気の診断を行うことです。
①塗抹・固定
検査材料は尿・喀痰・胸水・腹水・子宮頸部の細胞や、乳腺などを注射針で穿刺し、中の細胞を採取したものです。提出された検体をガラスに塗り、アルコールや乾燥による固定を行います。
②染色
組織診と同様に細胞を観察しやすくするために染色を行います。通常はパパニコロウ染色という染色を行い、必要に応じてその他の染色も行います。
③鏡検・診断
出来上がった標本を細胞検査士(細胞診を行うための認定資格をもった臨床検査技師)が顕微鏡で観察し、病理医と相談し診断しています。さらに、細胞診も組織診と同様に、必要な症例については術中迅速検査を行います。
当院の病理検査室では、組織診・細胞診の他に「病理解剖」も行っています。
病理解剖
ご遺族の承諾のもとに病死したご遺体を解剖して臓器を検査し、今後の医療に活かすため、死因、病気の進行の度合い、治療効果の程度、生前の診断は正しかったか、適切な治療がなされていたかなどを判断します。解剖は病理医が行い、臨床検査技師は介助にあたります。
検査部ニュース
学術関係報告
学会発表
- 紺田利子(発表):日本心エコー図学会第19回冬季講習会,2015.1.24-25
- 森田 明子:乳癌に浸潤を認めたCD61陽性・MPO陽性のAMLの一症例.第2回院内フォーラム,当院,2015.3.7
- 尾松 雅仁:当院で経験した子宮体部細胞診を契機に発見された卵管上皮内癌の一例.第31回兵庫県臨床細胞学会総会,神戸市,2015.3.7
- 玉木 恵里子:診断に苦慮した肝多血性腫瘍の一例.第180回大阪腹部超音波研究会,大阪,2015.3.12
- 岩崎 信広:腸間膜脂肪肉腫の一例.第129回大阪超音波研究会,大阪,2015.3.18
- 紺田 利子:エネルギー損失係数ELCo計測部位による大動脈弁狭窄症重症度の違いについての検討. 第26回日本心エコー図学会学術集会, 北九州市, 2015.3.26
- 川井 順一:重症大動脈弁狭窄症患者における大動脈基部の解剖学的特徴 -3次元経食道シネコー法による検討-. 第26回日本心エコー図学会学術集会, 北九州市, 2015.3.26
- 川井 順一:重症大動脈弁狭窄症患者における大動脈基部の計測-経食道3次元心エコー法とMDCTの比較検討-. 第26回日本心エコー図学会学術集会, 北九州市, 2015.3.27
あとがき
少し寒さが和らぎましたが、まだまだ油断してはいけません。寒暖差のせいで、風邪など引いていませんか?ただ今、桜の季節真っ盛りです。お花見&ピクニックの準備にとりかかるのはいか がでしょうか。私たちのおすすめは、芦屋川の桜です。川沿いで満開になった桜を眺めながら、おいしいものを 食べると日頃の疲れを癒してくれます。楽しいお花見に備えて、健康と料理の腕を準備しておきましょう!!P.S.病院前の桜もきれいですよ!(M.K&K.H)
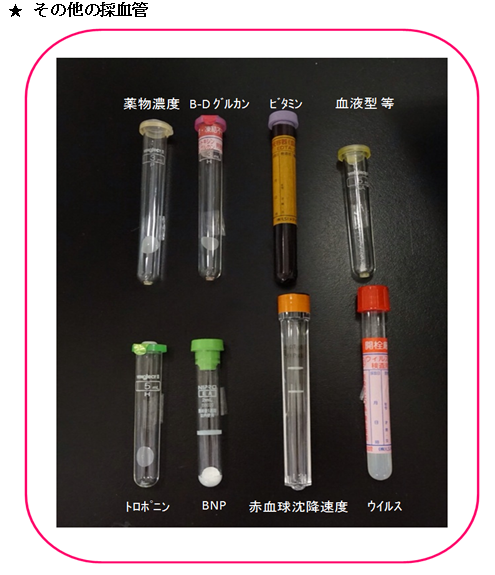
採血管の謎にせまる!
検体検査室 小坂・平野・加納
皆さん、採血は好きですか?きっと嫌いな人が多いのではないでしょうか。採血の時、次々に採血管が交換されるのを見て不思議に思った方はいませんか? 今回は、その採血管をご紹介したいと思います。
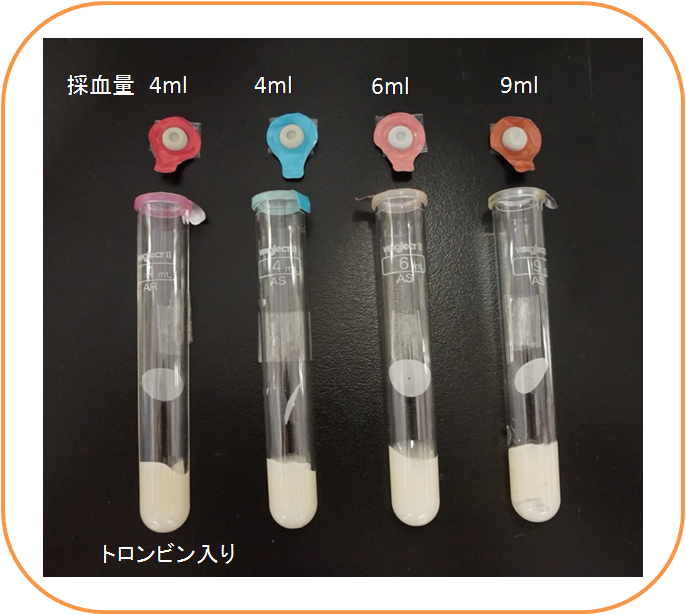
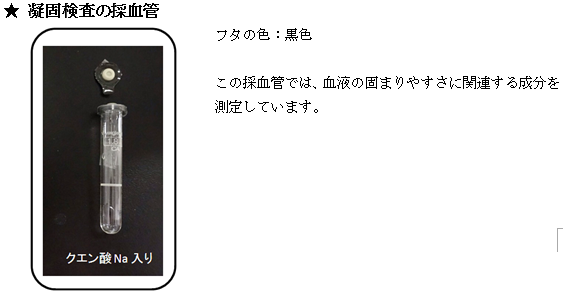
凝固促進剤と抗凝固剤について
血液を入れる前のまっさらの採血管をよく見ると中に何か(液体や粉末等)が入っているものがありますが、それらは正確な検査結果を出すために必要な薬品です。
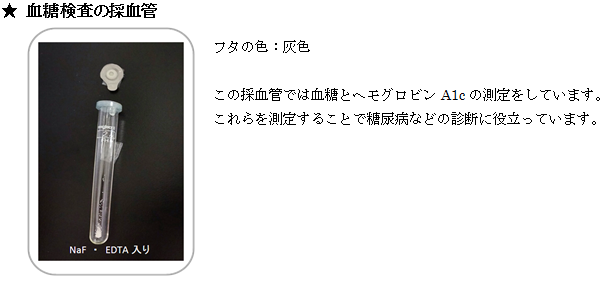
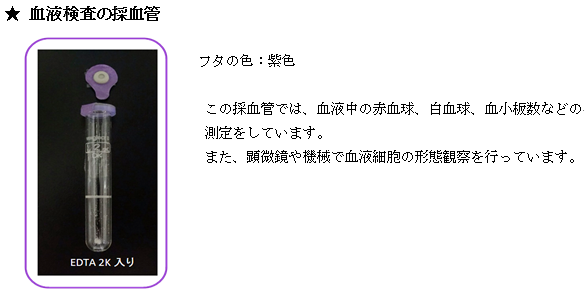
| 凝固促進剤 | トロンビン(生化学検査) 採った血液を固まりやすくさせる薬品です。検査結果を早く返すために必要です。 |
|---|---|
| 抗凝固剤 | EDTA(血液検査)、クエン酸ナトリウム(凝固検査) 採った血液を固まらないようにしておく薬品です。血液を固まらせずに、体の中にある状態に近いままで検査をするために必要です。 |
| 解糖阻止剤 | フッ化ナトリウム(血糖検査) 採血後、時間の経過とともに糖は分解し、血糖値はどんどん下がっていきます。その作用を止めるために必要な薬品です。 |
では、採血室でよく見かける採血管について詳しく見てみましょう!フタの色にも注目です!
この採血管では血清中のタンパク質、酵素、電解質などを測ることで、肝機能、心機能、腎機能、膵機能等患者さんの健康状態や、病気の程度を調べることができます。採血管の容量によってフタの色が違い、検査する項目数によって使い分けられています。
また、外来では診察当日に採血して、診察までに結果を出すことが多いので主に凝固促進剤(トロンビン)入りの容器を使っています。底にある白いものは血清分離剤(遠心分離*1した時に血液を血清と血球に分けます)、丸い紙は凝固促進フィルムです。
*1遠心分離:血液を1分間に3000回転させることにより、血球部分が底に沈んで血清(液体)部分と血球(固形成分)部分に分離することが出来ます。
採血管の種類は全部で50種類以上もあり、それぞれ検査の目的によって採血管を選択しています。この為、何本もの採血が必要となってきます。ほとんどの方は3~5本の採血がありますが、採血量は多くても大さじ一杯程度(20ml以下)です。
このように色々な採血管がありますがとてもカラフルで鮮やかで可愛いものが多いです。採血の時にはこんなところにも注目してみてください。ちょっと気がまぎれて痛くないかもしれませんよ?
検査部ニュース
学術関係報告
学会発表
- 紺田 利子:経胸壁心エコー図によるMitral annular disjuncton についての検討.
第79回日本循環器学会学術集会, 大阪, 2015.4.25 - 【講演】丸岡 隼人:悪性リンパ腫におけるイムノフェノタイピングの有用性.
近畿地区BDバイオサイエンスセミナー2015.京都.2015.04.11 - 森田明子:髄液細胞診に腸管症型T細胞リンパ腫(EATL)を認めた2症例.
第64回日本医学検査学会,福岡,2015.5.17 - 丸岡隼人:HRM法を用いたFLT3-ITD,NPM1変異遺伝子の検出系の確立.
第64回日本医学検査学会,福岡,2015.5.17 - 岩崎信広:ワークショップ;造影超音波検査は肝腫瘍以外の消化器疾患に必要か?
消化管腫瘍性病変における造影超音波検査の有用性について
日本超音波医学会第88回学術集会、東京、2015.5.23 - 岩崎信広:ワークショップ;消化管診断:超音波でどこまで診断できる?どこまで診断すべき?
小腸腫瘍性病変における超音波検査の有用性について
日本超音波医学会第88回学術集会、東京、2015.5.23 - 中村真実子:胆嚢悪性リンパ腫の一例.日本超音波医学会第88回学術集会、東京、2015.5.24
- 川井順一:ランチョンセミナー;新技術が変えるルーチン・エコー検査
心エコーのルーチンを変えるxMATRIXテクノロジー
第40回日本超音波検査学会 学術集会、横浜、2015.5.17 - 野村菜美子、竹川啓史、野上美由紀、内藤拓也、仁木真理恵、田中佑果、﨑園賢治、老田達雄:
Helicobactor cinaediによる化膿性椎体炎の1症例.第64回日本医学検査学会,福岡,2015.5.17 - 仁木真理恵、田村明代、角田敏明、野本奈津美、内藤拓也、森田明子、中村真実子、老田達雄:
当院臨床検査技術部における医療安全チームの活動報告.第64回日本医学検査学会,福岡,2015.5.16
あとがき
いよいよ5月も終わり、梅雨の季節が近づいてまいりました。最近はすっかり夏のような日差しの日も多く、早くも半袖・サンダルの出番となり、桜の頃が遠い昔のように思われます。 これからの季節、見ごろになるのがなんといってもアジサイですね。ちなみに、「紫陽花」の漢字は、唐の詩人・白居易がおそらくライラックに付けた名で、平安時代の学者・源順がこの漢字をアジサイにあてたことから、誤って広まったといわれているそうです(Wikipediaより)。 写真は実家のアジサイですが、早くも花をつけ始めた品種もあるようです。神戸市立森林植物園や神戸どうぶつ王国でも、毎年きれいなアジサイが展示されているので、少し足をのばして鑑賞しに行ってみてはいかがでしょうか。 (Y.S)
見逃しません!!輸血後感染症!!
輸血検査管理室 吉田 昌弘
輸血による感染症とは?
現在、我が国で輸血を受ける患者数は年間約120万人と言われています。このように輸血は誰もが受ける可能性のある身近な医療であり、患者さん自身でその安全性を正しく理解していくことが大事になってきます。輸血とは血液を作る力が低下しているとき、あるいは出血をして貧血状態になったときに、他人の血液で補う治療法です。
この輸血において、切り離すことのできない問題として輸血によるウイルス感染症があげられます。輸血によるウイルス感染症対策として、赤十字血液センターにて高感度にウイルスを検出できる核酸増幅検査(NAT)を導入したことにより、検査の精度は以前と比較して格段に向上し安全性が高まったといえます。
赤十字血液センターでNATが導入されて以降、当初の500検体プール法※1(1999年~2000年)から50検体プール法(2000年~2004年)、20検体プール法(2004年~2014年)、さらには1検体ずつ個別(2014年8月~)にNATが行われるように検査が厳格化されました。
しかし、献血者がウイルス感染直後のいわゆる『感染ごく初期』の場合、このNATをもってしても検出することは困難であり、検査でウイルスが検出できない時期(ウインドウピリオド)が発生することになります。現在は、輸血後のウイルス感染は限りなくゼロに近づいていますが、完全にゼロにすることができないのが現状です。
*1 検体プール法:検体をある程度まとめて検査する方法。まとめて行うので手間がかからないが、検体数が多ければ多いほど検出感度が悪い。
このような背景から、2004年4月1日に「生物由来製品感染等被害救済制度」が創設されました。この制度は、輸血製剤を適正に使用したにもかかわらず、その製品が原因で感染症等に罹患した場合、迅速に救済するための制度です。万が一、輸血によって何らかの病原ウイルスに感染した場合、上記制度で救済を受け、医療費、医療手当、障害年金などの給付を受けることができます。そして、この救済制度を受けるためには輸血前後の感染症検査が必要となってきます。
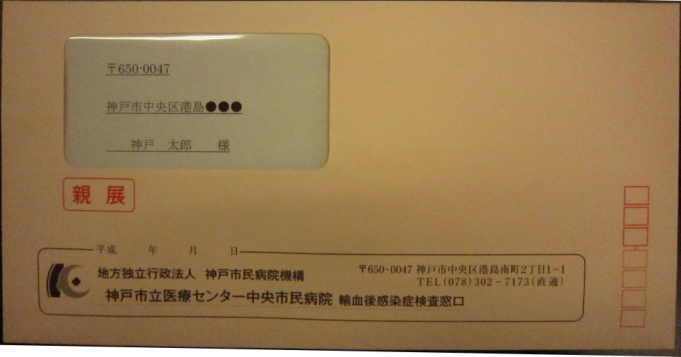
当院では2014年4月輸血実施分より、患者さんが輸血後3~4ヶ月後に感染症検査を受けていただくため、「輸血後感染症のおすすめ」のダイレクトメールをご自宅宛てに郵送しています。
そこで輸血後感染症検査に関わる様々な疑問を質問形式でお答えしていきます。
輸血後感染症って?その頻度は?
輸血が原因でB型肝炎ウイルス(HBV)、C型肝炎ウイルス(HCV)、エイズウイルス(HIV)などのウイルス感染症に罹患することです。2014年8月から1検体ずつ個別にNATを行うように検査が厳格化していったことで、さらに検出感度が高くなり、輸血後感染例数は、B型肝炎ウイルスが年間1例未満、C型肝炎ウイルスとAIDSウイルスに関しては数年~10年に1例未満になると推定されています。
検査項目は?
当院では、厚生労働省の「輸血療法の実施に関する指針」に準拠し、HBV核酸増幅検査、HCVコア抗原検査、HIV抗体検査の3項目を輸血後感染症検査として行っています。
輸血後感染症検査はなぜ必要なの?
NAT導入で、安全性が高まったとはいえ、ウイルス感染のリスクをゼロにすることは不可能です。そのために創設された「生物由来製品感染等被害救済制度」により救済を受けるために必要です。また、輸血によるウイルス感染症が疑われた場合、それを早い段階で察知し早期に治療介入することで重症化を防ぎます。
救済制度を受けるためには、輸血前後の感染症検査が必要になるとのことですが、輸血前の検査は全員実施しているの?
輸血前に感染症検査を実施しない場合もあります。しかし当院では、輸血前の患者様の血液を一定期間保存しています。万が一、患者さんに感染が認められた場合、輸血が原因でウイルス感染したことを証明するために、その血液を用いて詳細に検査することができます。
輸血後感染症検査はみんな受けているの?絶対受けないといけないの?
当院ではダイレクトメールを送った患者さんのうち60~70%の方が検査を受けています。検査を受けていただくことを推奨していますが、強制されるものではありません。
費用はどの程度かかるの?
検査費用は、健康保険3割負担で約3000円です(別途、初診の場合は約810円、再診の場合は約210円がかかります)。
検査結果はいつわかるの?
検査結果が出るまで約2週間かかります。結果については、担当医より説明がありますので外来受診をお願いします。
検査を受けたいです。どのように予約をとればいいの?
下記の当院輸血後感染症検査窓口までお電話下さい。
TEL:078-302-7173(平日の9:00~17:00)
ダイレクトメールに最後の輸血から3ヶ月後に検査が必要とありますが、5ヶ月後の検査でも大丈夫?
検査を受けていただくことは可能ですが、早期発見のため適切な時期として、最終輸血日から数えて3~4ヶ月後を推奨しています。目安となる日が近づいたら(輸血後約2ヶ月後)、当院からご自宅宛てにダイレクトメールを発送し、適切な時期の受診をお勧めしています。
万が一、輸血が原因で感染症にかかったら?
輸血が原因で感染症にかかった場合、健康被害を受けた方の救済を図るための生物由来製品感染等被害救済制度があります。これは医療費、医療手当、障害年金などの給付を受けることができる制度です。
ダイレクトメールの対象となる血液製剤は?
赤血球製剤、血漿製剤、血小板製剤などの「輸血用血液」が対象となります。
アルブミン製剤や免疫グロブリン製剤はダイレクトメールの対象ではないの?
アルブミン製剤、免疫グロブリン製剤、凝固因子製剤、フィブリン製剤などの「血漿分画製剤」については、当院からのダイレクトメールは発送していません。輸血後感染症検査の対象ではありませんが、もし気になるようでしたら当院輸血後感染症検査窓口まで電話し検査の予約をお願いします。
ただし、保険対象外となります。
NATで感染の判定ができない時期(ウインドウピリオド)の目安は?
B型肝炎ウイルスは約34日、C型肝炎ウイルスは約23日、エイズウイルスは約11日です。感染直後であるこの時期に献血された血液の場合、検査で感染の判定ができないため、その血液が輸血されることがあります。そのため、輸血後3~4ヶ月後に検査を受けていただくことをお勧めしています。
他の病院で検査を受けてもいいですか?
大丈夫です。もし当院からのダイレクトメールや連絡があった場合は、他の病院で検査する旨を伝えていただければ結構です。検査結果についてはとくに当院に知らせる必要はありません。
当院の輸血検査管理室では、より多くの患者さんが、輸血に対しての安全性を正しく理解したうえで、安心して輸血を受けていただきたいと考えています。
医師をはじめとする医療従事者、そして患者さんに、輸血と輸血後感染症検査はセットであるという認識を深めてもらい、輸血後感染症検査の実施率をより100%に近づけていけるように尽力していきます。
検査部ニュース
学術関係報告
論文発表
- 野本奈津美、谷知子:心臓腫瘍. 循環器臨床を変えるMDCT –そのポテンシャルを活かす-218-221、2015
- 杤尾人司:翼状針の斜め持ち、検査と技術43:305, 2015
- 杤尾人司:教科書には書いていない採血のコツ バトンリレースタイル法、検査と技術43:487, 2015
- 杤尾人司:教科書には書いていない採血のコツ:駆血帯の下止め、検査と技術43:487, 2015
学会報告、講演
- 川井順一:xMATRIXプローブを使用した心エコー検査の実際.第2 関西PHILIPS超音波セミナー
神戸,2015.7.4 - 岩崎信広:消化管の超音波診断-Lights and Shadows-GE Ultrasound Summer Forum2015
名古屋、2015.7.26 - 川井順一:心エコーのルーチンを変えるxMATRIXテクノロジー.第3回関西PHILIPS超音波セミナー
大阪(大阪マータンダイズ・マート),2015.7.12 - 森田明子:Anaplastic large cell lymphoma との鑑別に苦慮した Aggressive NK cell leulemia/lymphoma の2症例.第16回日本検査血液学会学術集会,
名古屋(名古屋国際会議場)2015.7.12
あとがき
梅雨も明け、暑い夏がやって来ました。夏の鮮やかな色彩が大好きです。とはいえ、暑いのも、寒いのも苦手なのですが…。桃やスイカなどの果物の美味しい季節でもあります。また、夏野菜には体を冷やす効果のあるものもあるようです。私の暑さ対策はスイカと寝具の工夫です。自分なりの工夫で猛暑を乗り切りましょう。こまめに水分補給して、熱中症には気を付けましょう。
涼しげな写真でもどうぞ。
肺機能検査について
生理機能検査 心肺部門 宮本淳子
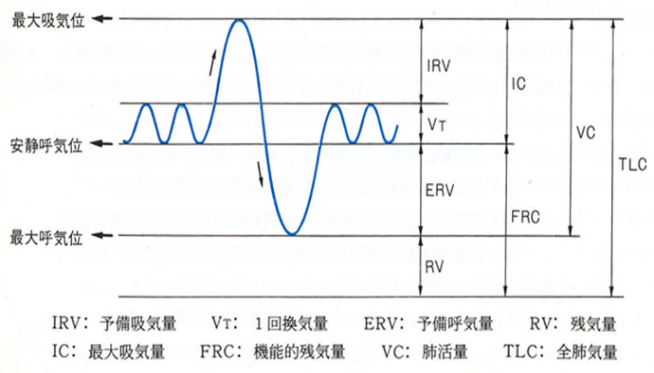
肺機能検査は生理機能検査の中の1つで、肺機能を客観的かつ定量的に評価することができます。
- 呼吸器疾患の換気障害程度や治療効果判定
- 手術前
- 障害認定
などに用いられ、肺機能の全体像を考える上で基本的な検査です。口から出入りする空気の量・速度を測定することにより肺の膨ら みやすさや気道の空気の流れやすさを評価することができます。測定値は年齢・身長・性別に基づく予測値と比較して評価されます。
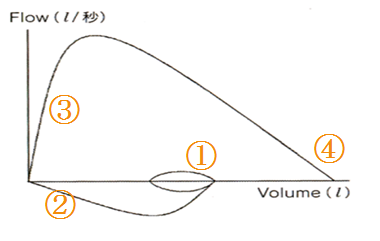
A 当院で行っている肺機能検査
肺活量(VC/SVC)、努力性肺活量(FVC)、機能的残気量(FRC)、肺拡散能力(DLCO)、気道可逆試験、気道抵抗などがあります。今回は肺活量(VC/SVC)と努力性肺活量(FVC)について紹介をします。
a. 肺活量:VC(vital capacity)/SVC(slow vital capacity)
- 肺気量分画の最も基本となる検査で、肺の容積変化量を示します。
- 測定はゆっくり・最大限に呼吸を行い、肺活量を含む 肺気量分画から各指標を計測します。
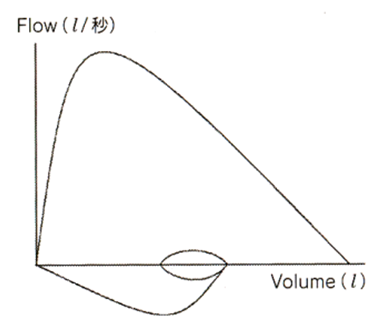
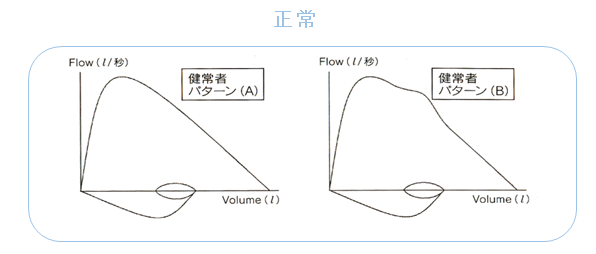
b. 努力性肺活量:FVC(forced vital capacity)
- 最大吸気位から最大呼気位まで、できるだけ強く速く呼出させて得られるフローボリューム曲線から各指標を計測します。
- ここで得られた肺活量を努力性肺活量(FVC)といい 呼吸筋力や気道抵抗を含む気道の狭窄を反映します。
B 実際の検査の流れ
a. 測定準備
- 検査は座った状態で行います。
- 椅子に深く腰掛け、背筋を伸ばし姿勢よく座るようにしましょう。
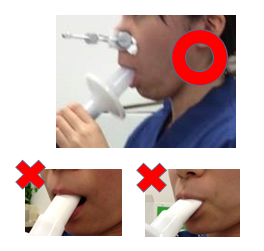
- マウスピースをくわえ、ノーズクリップを鼻に装着します。
注意点
*マウスピースは唇を密着させるようにしっかりくわえます。
*舌で穴をふさがないように気を付けてください。
b.肺活量(VC/SVC)
- 普段行っているような自然な呼吸(浅めの楽な呼吸)をします。
- 検査技師が合図をしますので、その合図にあわせて胸いっぱい吸います。
- 最大限吸ったらゆっくり吐き出します。
- 吐けなくなるまでしっかり吐き切ります。
- 2~4の深呼吸を2,3回繰り返して測定終了です。
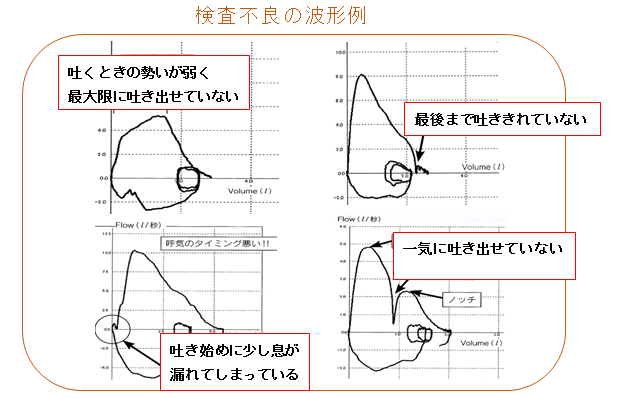
c.努力性肺活量(FVC)
- 自然な呼吸(楽な呼吸)から始めます。
- 検査技師が合図をしますので、胸いっぱい吸います。
- できるだけ強く、速く、一気に吐き出します。
- そのまま吐き続けて、最後まで吐き切ります。
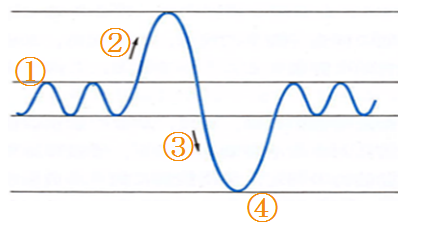
C 実際の検査結果
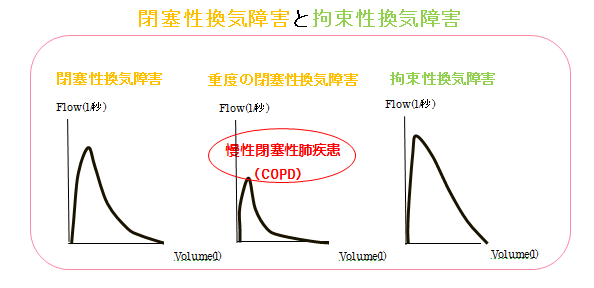
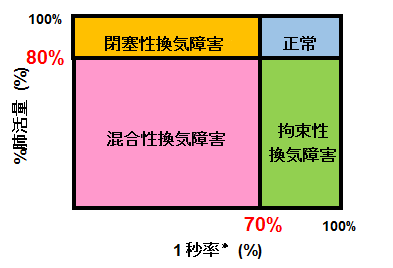
D 肺機能検査による換気障害分類
*1秒率とは:努力性肺活量で最初の1秒間で吐き出した量(1秒量)の割合
a. 閉塞性換気障害
空気の通り道が狭くなる通過障害です。息切れや呼吸困難などの症状を呈します。
| 主な疾患 | COPD(慢性気管支炎、肺気腫)、気管支喘息など |
|---|
b. 拘束性換気障害
肺の空気を入れる容量が少なる障害です。肺の弾性力の低下や肺容量減少、呼吸筋力の低下 などが原因で起こります。
| 主な疾患 | 間質性肺炎、肺線維症、じん肺症、肺切除術後、重症筋無力症など |
|---|
E 肺機能検査はこんなことに役立ちます
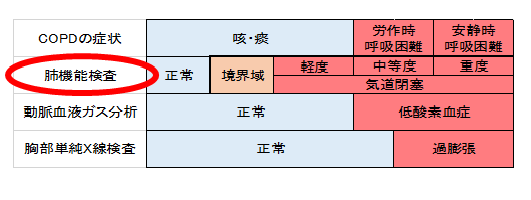
COPDの早期発見には肺機能検査が一番優れていて、重症度分類が可能です。

*慢性閉塞性肺疾患(COPD:chronic obstructive pulmonary disease)とは
タバコ煙を主とする有害物質を長期吸入・曝露することで生じる肺の炎症性疾患で、喫煙習慣を背景に発症する生活習慣病です。喫煙者の15~20%がCOPDを発症し、日本人の死亡原因の第9位(男性では7位)を占めています。大多数が未診断・未治療の状態であると考えられ、その早期発見が重要視されています。
最後に
肺機能検査は患者さんご本人の《最大努力》が必要な検査です。最大限の呼吸を行わないと呼吸機能を評価するための最良のデータは得られません。病態を考慮した上で最大努力を引き出せるよう私たち臨床検査技師は声かけしますので一緒に頑張りましょう♪ 検査への協力お願いします。
参考文献
Hyatt R, オフィススパイロメトリー選択・使用の実用ガイド 大崎 饒, 入江 正 著.
「呼吸機能検査トレーニング」, 中外医学社 羽白 高,柴田 正慶 著
「スパイロメトリーの基本と秘訣」,克誠堂出版
検査部ニュース
学術関係報告
論文発表
- 杤尾人司:教科書には書いていない採血のコツ:”正対し、背筋を伸ばした姿勢”から
検査と技術43:673, 2015 - 杤尾人司:教科書には書いていない採血のコツ:“ボクサー拳(こぶし)”で手背採血
検査と技術43:765, 2015 - 杤尾人司:教科書には書いていない採血のコツ:手背採血のための効果的トレーニング法:
“伸展輪ゴム刺し訓練” 検査と技術43:1149, 2015 - 杤尾人司:教科書には書いていない採血のコツ:成功につながる患者確認法:
「○○さん、○○さんは名前を何とおっしゃいますか?」 検査と技術43:1221, 2015 - Hitoshi Tochio, Masafumi Sugahara, Yukihiro Imai, Hiroshi Tei, Yoshiyuki Suginoshita, Nobuhiro Iwasaki, ichiro Sasaki, Michio Hamada, Kazushi Minowa, Tetsurou Inokuma, Masatoshi Kudo: Hyperenhanced Rim Surrounding Liver Metastatic Tumors in the Postvascular Phase of Sonazoid-Enhanced Ultrasonography: A Histological Indication of the Presence of Kupffer Cells. Oncology 89:33-41, 2015
共著論文
- Mayuko Izumi.,Hiroko Tsunemine, Yasuhiro Suzuki, Akihiro Tomita, Toshiko Kusumoto,Taiichi Kodaka, Kiminari Itoh, Takayuki Takahashi: Successful treatment of refractory cold hemagglutinemia in MYD88 L265P mutation-negative Waldenstrom`s macroglobulinemia with bortezomib. Int J Hematol 102: 238-243, 2015.
学会報告、講演
- 丸岡隼人:遺伝子検査の基礎と実習. アークレイ遺伝子アカデミー大阪2015. 京都.2015.08.08
- 岩崎信広:「進撃の消化管エコー-step after step goes far-」
第44回日本消化器がん検診学会近畿地方会 ランチョンセミナー講演,大阪(国際会議場)2015.8.29 - 岩崎信広:「消化管の超音波診断-lights and shadows-」GE ultrasound clinical seminar2015
超音波指導検査士によるセミナー講演、埼玉(ラフレさいたま)2015.8.30 - 竹川啓史:「真菌の検査法 ~基礎から臨床~」.第3回臨床微生物部門研修会
一般社団 法人岐阜県臨床検査技師会.岐阜.2015.9.12 - 奈須聖子:「尿沈渣検査に役立つ尿路感染症の基礎知識」.一般検査研修会
公益社団 法人兵庫県臨床検査技師会.神戸.2015.9.30 - 岩崎信広:特別企画「明日から役立つ超音波塾-腹痛編-USでLQQTSFAを診る-」
日本超音波医学会第42回関西地方会学術集会.大阪.2015.9.26 - 南佳織、岩崎信広、荒木直子、栃尾人司、簑輪和士、鄭浩柄、杉之下与志樹、橋田裕毅、猪熊哲朗、
今井幸広:一般演題「造影USが診断に有用であった虫垂粘液癌の一例」
日本超音波医学会第42回関西地方会学術集会.大阪.2015.9.26 - 川井順一:従事者向けCOPD講習会「スパイロメータの検査値の見方と肺年齢測定の 講義及び実習」.
神戸市保健福祉局健康づくり支援課主催. 神戸(勤労会館). 2015.09.03 - 玉木恵里子、栃尾人司、岩崎信広、簑輪和士、鄭浩柄、杉之下与志樹、猪熊哲朗、今井幸広:
「ソナゾイド造影超音波を施行した肝血管筋脂肪腫5症例の検討」
日本超音波医学会第42回関西地方会学術集会.大阪.2015.9.26 - 野本奈津美、谷知子、紺田利子、藤井洋子、中村仁美、三羽えり子、菅沼直生子、宮本淳子、中野彩、
角田敏明、川井順一、金基泰、太田光彦、北井豪、古川裕
「当院における過去15年間での心エコー図検査にて発見された心臓腫瘍症例の検討」
第63回日本心臓病学会学術集会. 横浜2015.9.20 - 堀香菜、谷知子、紺田利子、藤井洋子、川井順一、菅沼直生子、野本奈津美、北井豪、太田光彦、
古川裕「開口部の診断に苦慮した冠動脈瘻の1症例」
日本超音波医学会第42回関西地方会学術集会.大阪.2015.9.26 - 山本駿, 丸岡隼人, 白石祐美, 野本奈津実, 吉田昌弘, 山内容子, 老田達雄:
COLD-PCR による変異遺伝子検出感度の向上-JAK2V617F検出を例に-.
第55回日本臨床衛生検 査技師会近畿支部医学検査学会,大阪,2015年10月18日 - 城本千裕, 尾松雅仁, 松浦亮一郎, 井本秀志, 森田明子, 菅原雅史, 森本美咲, 末岡馨,田代明人, 田村明代,
老田達雄, 今井幸弘 :キシレンフリーの製剤を用いた細胞診標本における退色の検討.
第55回日本臨床衛生検査技師会近畿支部医学検査学会,大阪,2015年10月17日 - 末岡馨, 菅原雅史, 松浦亮一郎, 尾松雅仁, 井本秀志, 森田明子, 森本美咲, 城本千裕, 田代明人,
田村明代, 老田達雄, 今井幸弘 :リンパ節の凍結切片作成時におけるアーチファクトの検討.
第55回日本臨床衛生検査技師会近畿支部医学検査学会,大阪,2015年10月17日 - 松下 隆史 佐々木 一朗 南 佳織 中村 真実子 濱田 一美 黒田 真百美 幸原 伸夫
検査結果の判読に苦慮した多発性神経炎の一例 第55回日本臨床衛生検査技師会近畿支部医学検査学会,
大阪,2015年10月18日 - 南 佳織 佐々木 一朗 松下 隆史 中村 真実子 濱田 一美 黒田 真百美 :
僧帽筋における反復刺激試験のテクニカルノート.
第55回日本臨床衛生検査技師会近畿支部医学検査学会,大阪,2015年10月18日 - 丸岡隼人:造血器腫瘍におけるFCMと遺伝子検査の有用性.
福井県臨床衛生検査技師会遺伝子・血液合同研修会.福井.2015年10月31日 - 岩崎信広:超音波検査を活用しよう(腹痛編). 当院救急部オープンセミナー. 神戸. 2015年10月28日
- 竹川啓史:真菌・培養困難な微生物.日本看護協会.
平成27年度感染管理認定看護師教育課程.神戸.2015年10月12日 - 田中佑香 竹川啓史 内藤拓也 﨑園賢治 老田達雄:
Corynebacterium kroppenstedtii による乳腺炎の1例 - 佐々木一朗,松下隆史, 中村真実子,南佳織,登阪貴子,杤尾人司,簑輪和士,老田達雄,
IOM(intraoperative neurophysiological monitoring)における動的記録の有用性.
第55回日本臨床衛生検査技師会近畿支部医学検査学会,大阪,2015年10月18日 - 松下 隆史, 佐々木 一朗, 南 佳織, 中村 真実子, 濱田 一美, 黒田 真百美, 幸原 伸夫:
複合筋活動電位(CMAP)の振幅と持続時間~異なる計測法間での相関, 第54回日本神経生理学会
学術大会,大阪,2015年11月6日 - 森田明子,井本秀志, 尾松雅仁,田代明人, 上原慶一郎, 今井幸弘 :
当院の臨床検査技術部内での細胞検査士の取り組み.
第54回日本臨床細胞学会秋期大会,名古屋,2015年11月22日 - 尾松雅仁,井本秀志, 森田明子 ,田代明人, 上原慶一郎, 今井幸弘 :
子宮体部細胞診を契機に発見された卵管上皮内癌の一例.
第54回日本臨床細胞学会秋期大会,名古屋,2015年11月22日 - 中村 真実子,佐々木 一朗, 松下 隆史, 南 佳織,濱田 一美, 黒田 真百美, 幸原 伸夫:
当院における副深腓骨神経の頻度の検討, 第54回日本神経生理学会 学術大会,大阪,2015年11月6日 - 竹川啓史:真菌の同定と薬剤感受性について.第18回微生物検査研究会.神戸.2015年11月17日.
- 﨑園賢治:グラム染色のいろは.救急オープンセミナー.当院.2015年11月4日
- 山本駿,丸岡隼人,老田達雄:JAK2 V617F allele burden高感度定量法の確立.
第62回日本臨床検査医学界学術集会,岐阜,2015年11月20日 - 岩崎信広:デスモイド腫瘍、消化管エコーセミナー 2015、大阪、2015年11月14日
あとがき
すっかり寒くなり、冬らしさが日に日にましていきますね。神戸では12月4日から13日の間「神戸ルミナリエ」が開催されました。「神戸ルミナリエ」は、阪神淡路大震災犠牲者の鎮魂の意を込めるとともに、都市の復興・再生への夢と希望を託し毎年開催されています。来場の際には、それぞれが震災について振り返ったり、震災被害者の方々の鎮魂と復興を願いたいものですね。今年からLED電球にかわり例年とは違った趣があるので、ぜひみなさまも来年足を運んでみてはいかがでしょうか。インフルエンザやノロウイルスの流行時期ともなりましたので、体調にお気をつけてお過ごしください。 (M.M)
採血室の紹介
採血室 川井 順一
はじめに
採血には痛みを伴いますが、患者さんから採血された血液から得られる情報は病気の診断や、病状の把握にとても役立っています。今回の「TEKARI」では、当院の外来採血室をご紹介します。
当院外来採血室の概要
- 当院の外来採血室は、7ブースあり、スタッフ7名および事務スタッフ1名で採血業務を行っています。
- スタッフは、国家資格を有する「臨床検査技師」と「看護師」で構成されています。
- 採血件数は、一日に500~700件の採血を行ない、多い日には800件を超える場合もあります。
採血を受けられる患者さんへのお願い
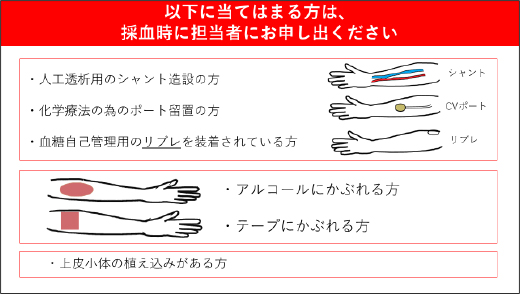
合併症や医療事故防止のため、以下の項目を確認致しますので、該当する方は採血前にお申し出ください。
- 採血時に気分が悪くなったことがある。
- アルコール、紙テープ(サージカルテープ)、手袋(ラテックス)でかぶれやすい。
- 血が止まりにくい(血液をサラサラにする薬を飲んでいる)。
- 人工透析をしている(シャント側の腕を避けて採血します)。
- 化学療法の点滴やCT検査など造影剤の注入を予定している。
- 治験目的などでポートの植え込みをされている。
その他採血に関して不安があるなど、気になることは何でも相談してください。
当院外来採血の実際
当院外来採血室の実際の流れを紹介します。
1. 検査受付
- 受付は、自動受付機、あるいは受付Cカウンター(Cブロック受付)にて行います。
- 自動受付機による受付は、午前7時30分より開始します。
- 受付Cカウンターの受付は、午前8時15分より開始します。受付終了時間は午後5時30分です。
- 採血開始時間は、午前8時30分より開始します。
- 自動受付機に診察券を通していただき、メッセージにしたがって操作してください。
- 受付番号票や採尿コップ(医師からの依頼があれば自動で出てきます)を取ってください。
- 最後に、診察券を取ってください。
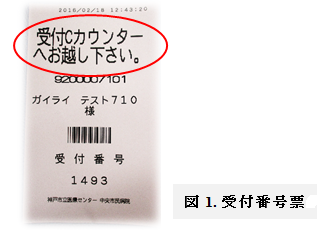
- 受付番号票に「受付Cカウンターへお越し下さい。」(図1)が印刷されたときには、確認したいことがありますので受付Cカウンターまでおまわりください。
2. 採血室中待合への入室
- 電光掲示板に受付番号票の番号が表示されましたら、採血室中待合にお入りください。
- 採血をスムーズに行うため、あらかじめ肘が出るところまで衣服の袖を上げておいてください。
- 中待合に入られましたら、採血ブースの上にあります電光表示板に受付番号票の番号が表示されるまで、椅子に座ってお待ちください。
- 順番がきましたら、採血ブースから電子音が鳴り、電子音声にて患者さんの誘導メッセージが流れます。
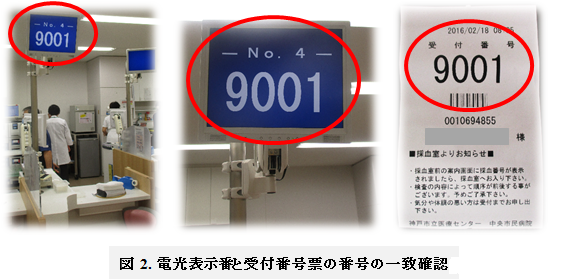
(注意)気分が悪い方や検査の内容により優先的に採血を行う場合があります。そのような場合には順番が前後することがありますので、ご理解、ご協力をお願いします。 - 採血ブースの上にあります電光表示板と受付番号票の番号が一致するところ(図2)に、荷物を置いてお座りください。
3. 採血前の本人確認
採血室では、採血を安全かつ間違いなく行うためにご本人確認をさせていただいています。
- 採血ブースの椅子に座られましたら、受付番号票をスタッフに渡してください。
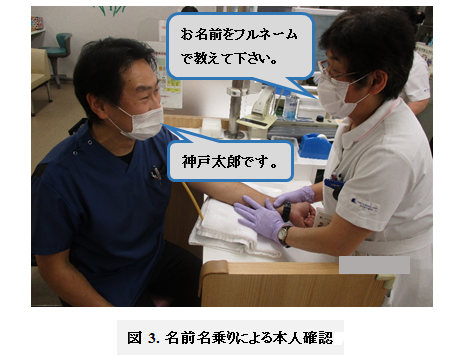
- 採血担当者は患者さんご自身でお名前を名のってください。ご協力をお願いします(図3)。
4. 採血
①採血前の準備
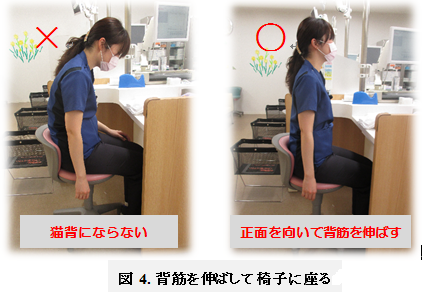
a. 患者さんは、背筋を伸ばして椅子に座っていただきます(図4)。
(理由)姿勢を伸ばすことで血管が拡張して、血管を確認しやすくなります。
杤尾人司.“正対し、背筋を伸ばした姿勢”から.検査と技術 vol 43, p.673, 2015
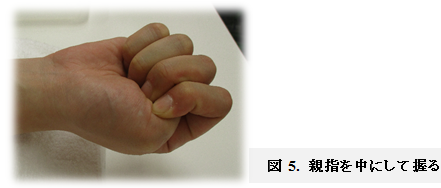
b. 採血するときには、親指を中にして握っていただきます(図5)。
(理由) 静脈の血流量が増えることで血管が拡張して、血管を確認しやすくなります。
*この他、手指を温める、手を下にしばらく下していただくなどお願いすることがあります。また、水分をしっかり取って頂いたり、採血時にリラックスして頂くと血管がわかりやすくなります。
- ベッド採血希望の患者さん
ご気分がすぐれないとき、失神やめまいを起こした既往がある患者さんは、ベッド上で採血いたしますのでお申し出下さい。 - 車椅子の患者さん
車椅子の患者さんは、車椅子に座ったまま対応させていただきますので、そのまま該当のブースでお待ち下さい。
② 穿刺(せんし)
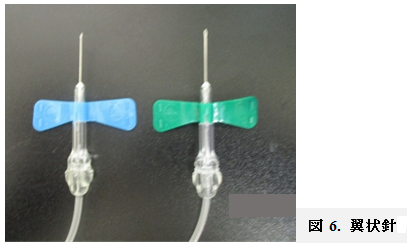
a. 当院の採血室では、原則として全例に翼状針(図6)を使用します。
b. 採血で使用する手袋は、患者さんごとに新しいものに交換し、感染防止対策に努めています。
c. 皮膚の消毒は、通常はアルコール綿を使用します。アルコールでかぶれなどがある患者さんは、スタッフにお申し出ください。 アルコールの入っていない消毒薬(ヘキシジン)を用います(図7)。ただし、ヘキシジンの消毒効果を高めるため、30秒~60秒間かけて消毒をします。
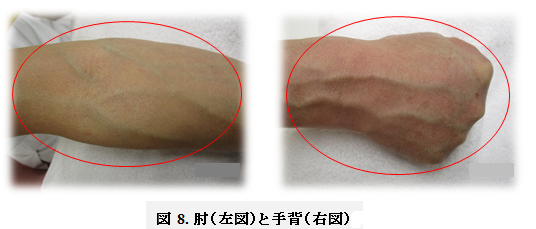
d. 通常は、肘部の表在静脈から採血しますが、両側の肘が採血不能な場合には、手背など他の血管から行います(図8)。
e. 検査に使うための採血量では、通常貧血にはなりません。
f. 採血後の血液が量不足であったり、検査に不適(溶血や凝固)であったりした場合、まれに再度採血をお願いすることがあります。ご理解、ご協力をお願いします。
③ 採血後
a. 採血終了後、乾綿で穿刺部位を圧迫止血し、紙テープを貼付します。紙テープでかぶれるなどの既往がある方は事前に申し出て下さい。
b. 患者さんは、採血後5分程度、採血部位をもまずに圧迫止血して下さい(図9)。
c. 採血部位をもんでしまうと止血を阻害し、内(皮下)出血して採血部位が青くなることがあります。
d. ワーファリンなど血液をさらさらにするお薬を内服中の患者さんは、10分間以上圧迫止血して下さい。
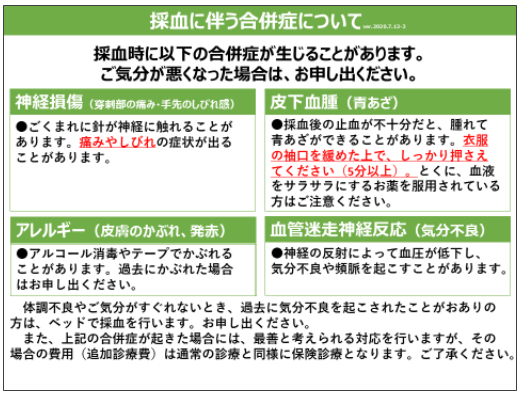
採血の合併症
a. 内(皮下)出血 採血部位の圧迫止血が不十分だったり、採血部位をもんだりすると、採血部位が青くなったり、腫れたりすることがあります。内出血は、通常は数日~数週間で体内に吸収されます。もし、内出血しているところが広がったり、腫れ、痛みが持続している場合は採血室スタッフにお申し出下さい。
b. 神経損傷 採血後に、手指へ拡がる痛み、しびれなどが生じ、一定時間が経過した後も持続することがあります。もし、手指に痛みやしびれが持続している場合は、採血室スタッフにお申し出ください。
c. 失神・めまいなど 採血時の失神やめまいは、迷走神経反射が原因とされています。採血に対する緊張や不安により生じると考えられています。症状としては、顔面蒼白、気分不快、動悸などの症状が現れます。採血時に気分が悪かったり、失神やめまいを起こした既往がある患者さんは、ベッド上で採血いたしますのでお申し出下さい。
最後に
採血によって患者さんの痛みを伴うことは、採血スタッフ一同痛感しております。 また、採血がうまくいかず、患者さんにはご迷惑をかけるケースも時にはあります。 採血をする側としては、できるだけ患者さんに痛みが少なく、早く採血したいと心がけています。 ご理解、ご協力をお願いします。
検査部ニュース
学術関係報告
論文発表
- 杤尾人司:教科書には書いていない採血のコツ⑨:痛みを最小限にする穿刺法、
検査と技術43:1305, 2015 - 杤尾人司:教科書には書いていない採血のコツ10:”あ、逆血がない”,,,穿刺失敗時の原因と対処、
検査と技術44:47, 2016 - 杤尾人司:教科書には書いていない採血のコツ11:”あっ、血が止まった” その時、どうする?
検査と技術44:217, 2016 - 杤尾人司:教科書には書いていない採血のコツ12:血管迷走神経反射(VVR)回避法「患者を笑顔に」
検査と技術44:427, 2016
学会報告、講演
- 香原美咲:USにて腫瘤形成性膵炎を疑った膵癌の2例.
第106回 腹部オープンカンファレンス, 神戸, 2015.12.03 - 丸岡隼人:遺伝子変異解析の基礎.日臨技近畿支部 遺伝子部門研修会.京都.2016.01.23
- 野本奈津美, 太田光彦, 紺田利子, 川井順一, 角田敏明, 菅沼直生子, 中嶋正貴, 山根崇史, 谷知子, 古川裕:
術中経食道心エコー図にて二尖弁が疑われた高度大動脈弁狭窄症に対し経カテーテル的大動脈弁植え込み術を施行した一例. 第82回神戸臨床心エコー図研究会, 神戸, 2016.1.30 - 佐々木一朗:法的脳死判定.第9回脳波筋電図セミナー 関西脳波筋電図研究会.京都.2016.01.29
- 佐々木一朗:誘発電位ハンズオン.第9回脳波筋電図セミナー 関西脳波筋電図研究会.京都.2016.01.29
- 奈須聖子,竹川啓史,内藤拓也,﨑園賢治:当院における過去10年間の血液培養検査の解析.
第27回日本臨床微生物学会総会・学術集会.宮城・仙台,2016.1.30 - 竹川啓史:ワ-クショップ院中八策 ~よりよい微生物検査の報告を目指して~ 真菌検査,
第27回日本臨床微生物学会総会・学術集会,宮城・仙台.2016.1.30 - 田代明人,井本秀志, 森田明子, 尾松雅仁,上原慶一郎,今井幸弘:好中球に中毒性顆粒を認め、G-CSF産生が示唆された転移性腫瘍の1例.第32回兵庫県臨床細胞学会総会,神戸,2016年3月5日
- 丸岡隼人:フローサイトメーターを用いた検査についての質疑応答.
BD FACSTM クリニカルソリューションセミナー in 京都 2016,京都,2016年3月19日 - 岩崎信広、他、メッケル憩室の超音波像について.131回大阪超音波研究会、大阪、2016年3月9日
- 宮本淳子,谷知子,紺田利子,藤井洋子,川井順一,角田敏明,菅沼直生子,野本奈津美,太田光彦,金基泰,古川裕:「重症大動脈弁狭窄症の種々の病態における左房機能について-経胸壁心エコー図における検討」第80回日本循環器学会学術集会,仙台,2016.03.18-20
あとがき
桜もちらほら咲きはじめたこの時期、今年も何時ものように別れと出会いがあります。 当検査部でも、長年検査部の為に尽くしてこられた3名の定年退職者がいらっしゃいます。 何時もおおらかで明るく、落ち込んでいるときには『なんとでもなるわよ!』と元気を与えてくれ、 また、仕事のスキルを上げるためには手を抜かず勉強する姿勢を示してくれた先輩。 何時も出た結果に安易に妥協せず、少しでもおかしいと思えば原因をとことん追及する姿や、 子育ても仕事も一生懸命続けていく道筋を示し、検査技師としてだけでなく一人の女性としても目標だった 先輩。私が新人の時初めての業務を一緒に組み『ケンサ』の『ケ』の字から教えていただいた検査の師匠。 どの方とも別れ難く、居なくなられると思うと心もとなく不安になります。 3人の先輩達からは、本当に書ききれないほどの沢山のことを、言葉だけでなくその後ろ姿で教えていただきました。特に師匠には、今の私の検査技師としての原点の形を作っていただいたと思っています。 検討の仕方、データーの読み方、発表の仕方などは勿論ですが、そういった形のあるものだけではなく、 『常に回りを見ろ』『状況を読め』『一歩でも二歩でも先のことを考えて動け』といった、 自分自身の在り方を教えていただきました。まだまだ師匠の域に達するには程遠く、毎日反省と後悔の繰り返しですが、常に師匠の言葉を胸にし少しでも尊敬する師匠に近づけたらと思っています。 4月になれば、また新しい出会いの人達が来ます。彼らが、私と同じ様に素晴らしい先輩達に巡り合い、 検査技師として、一人の人間として大きく成長してくれることを期待します。( A.T)
造血器腫瘍の微小残存病変(MRD)評価について
細胞遺伝子検査室 白石 祐美
はじめに
白血病や悪性リンパ腫といった造血器腫瘍の診断や,治療後の微小残存病変(minimal residual disease:MRD)の評価方法として,光学顕微鏡による標本の観察,染色体分析,フローサイトメトリー, PCR法といった様々な方法がありますが,それぞれの方法によって,検出感度は異なります(フローサイトメトリー,PCR法,微小残存病変については「特集第1号 遺伝子検査:FLT3変異とNPM1変異について」 もご覧ください)。当検査室では,このフローサイトメトリーとPCR法を併用することで,多面的な検査を行うことが可能となっています。今回のTEKARIでは,この2つの方法の実際について,症例をあげてご紹介します。
症例1:悪性リンパ腫
他院でCTを行った際に,偶発的にリンパ節腫張を指摘され,その後リンパ節生検によって悪性リンパ腫と診断された症例です。
左:リンパ節のスタンプ標本画像です。N/C比(核/細胞質の比率)が高く,小型の腫瘍細胞が多数確認されます。
右:IgH再構成検査(※1)の電気泳動(PAGE)の結果です。陽性を示すバンド(矢印)が認められます。(一番右のバンドは陽性コントロールです。)
*1 IgH再構成検査:通常,B細胞は分化・成熟段階において,多様な抗体を生み出すために,免疫グロブリン遺伝子の再構成によって多種多様なクローンを生じる。 しかし腫瘍においては単一クローンが増殖するために, 再構成によって生じた遺伝子配列は同一となる。この性質を利用して,PCR法によって検出する検査である。
上図はフローサイトメトリーの結果です。これにより,腫瘍細胞は 小型であり,CD19+,CD20+,CD10+,CD43-,CD45+,Lambda+という特徴を有することが明らかとなりました。
また,骨髄へのリンパ腫細胞の浸潤の有無を確認するために,骨髄液の検査が行われました。
左:骨髄液の塗抹標本像です。骨髄液中には様々な種類の細胞が観察されますが, リンパ腫細胞の浸潤ははっきりしません。
右: 高感度IgH再構成検査(※2)の結果です。上段がリンパ節生検時の結果であり,下段が今回の骨髄液を用いた結果です。その値はほぼ一致しており, リンパ節で認められた腫瘍細胞と同一の細胞が骨髄液中にも存在することが明らかとなりました。
*2 高感度IgH再構成検査:IgH再構成検査にて陽性となった症例については、その情報をもとに、症例特異的なプライマーを選択し、semi nested PCR法により、 より感度を高めたPCR法を実施している。結果はフラグメント解析により、PCR産物長を測定することで、陽性/陰性の判定を行う。
骨髄液のフローサイトメトリーの結果です。過去の陽性パターンをもとに,症例に特異的な抗体パネルを用いることで,より高感度にリンパ腫細胞の浸潤を捉えることができます。 今回は、リンパ節生検で得られた、CD10+,CD20+,CD43-,CD45+,Lambda+という情報をもとに検査を行い、当検査においても骨髄液の細胞中の0.1%に浸潤が認められました。
症例2:急性骨髄性白血病
発熱を機に近医を受診され、白血球数異常を指摘されたため当院で精査を行い、急性骨髄性白血病と診断された一例です。
骨髄液を用いた、初発時のフローサイトメトリーの結果です。CD4+CD7+CD16-CD34+CD45dim+CD123+という特徴をもった腫瘍細胞が、骨髄液中の54%に認められます。 この結果を利用して、定期的に骨髄液の検査を行い、フローサイトメトリーを用いて治療の効果をモニタリングしていきます。
また、腫瘍細胞にはNPM1遺伝子の変異が認められたので、この変異遺伝子の骨髄液中での発現量を測定することで、 PCR法の面からも病勢をモニタリングすることが可能でした。 以下は、初発時の発現量を1として、その後の変化をグラフで表したものです。フローサイトメトリーの結果と類似し、発現量は徐々に上昇が認められ,再発時 (MRD4)には急上昇していますが、骨髄移植後には極めて低いレベルまで低下しています。
結語
今回ご紹介したように、フローサイトメトリーとPCR法という2つの側面から検査を行うことで、標本の観察だけでは明らかにならなかった腫瘍細胞の存在を知ることができる場合もあり、 これらの検査はMRDの評価に有用であると考えられます。当検査室では、新規検査項目の追加や、現行法の改善などを積極的に行っており、 高感度かつ正確性の高い結果を迅速に臨床に提供していけるように日々研鑽しています。
検査部ニュース
学術関係報告
論文発表
- 杤尾人司:教科書には書いていない採血のコツ⑨:痛みを最小限にする穿刺法、
検査と技術43:1305, 2015 - 杤尾人司:教科書には書いていない採血のコツ10:”あ、逆血がない”,,,穿刺失敗時の原因と対処、
検査と技術44:47, 2016 - 杤尾人司:教科書には書いていない採血のコツ11:”あっ、血が止まった” その時、どうする?
検査と技術44:217, 2016 - 杤尾人司:教科書には書いていない採血のコツ12:血管迷走神経反射(VVR)回避法「患者を笑顔に」
検査と技術44:427, 2016
学会報告、講演
- 香原美咲:USにて腫瘤形成性膵炎を疑った膵癌の2例.
第106回 腹部オープンカンファレンス, 神戸, 2015.12.03 - 丸岡隼人:遺伝子変異解析の基礎.日臨技近畿支部 遺伝子部門研修会.京都.2016.01.23
- 野本奈津美, 太田光彦, 紺田利子, 川井順一, 角田敏明, 菅沼直生子, 中嶋正貴, 山根崇史, 谷知子, 古川裕:
術中経食道心エコー図にて二尖弁が疑われた高度大動脈弁狭窄症に対し経カテーテル的大動脈弁植え込み術を施行した一例. 第82回神戸臨床心エコー図研究会, 神戸, 2016.1.30 - 佐々木一朗:法的脳死判定.第9回脳波筋電図セミナー 関西脳波筋電図研究会.京都.2016.01.29
- 佐々木一朗:誘発電位ハンズオン.第9回脳波筋電図セミナー 関西脳波筋電図研究会.京都.2016.01.29
- 奈須聖子,竹川啓史,内藤拓也,﨑園賢治:当院における過去10年間の血液培養検査の解析.
第27回日本臨床微生物学会総会・学術集会.宮城・仙台,2016.1.30 - 竹川啓史:ワ-クショップ院中八策 ~よりよい微生物検査の報告を目指して~ 真菌検査,
第27回日本臨床微生物学会総会・学術集会,宮城・仙台.2016.1.30 - 田代明人,井本秀志, 森田明子, 尾松雅仁,上原慶一郎,今井幸弘:好中球に中毒性顆粒を認め、G-CSF産生が示唆された転移性腫瘍の1例.第32回兵庫県臨床細胞学会総会,神戸,2016年3月5日
- 丸岡隼人:フローサイトメーターを用いた検査についての質疑応答.
BD FACSTM クリニカルソリューションセミナー in 京都 2016,京都,2016年3月19日 - 岩崎信広、他、メッケル憩室の超音波像について.131回大阪超音波研究会、大阪、2016年3月9日
- 宮本淳子,谷知子,紺田利子,藤井洋子,川井順一,角田敏明,菅沼直生子,野本奈津美,太田光彦,金基泰,古川裕:「重症大動脈弁狭窄症の種々の病態における左房機能について-経胸壁心エコー図における検討」第80回日本循環器学会学術集会,仙台,2016.03.18-20
あとがき
梅雨が明け、セミも鳴き始めて、すっかり夏らしくなってきた今日この頃、皆様いかがお過ごしでしょうか? 花火大会にお祭り、海やプールなど・・・ 夏はイベントが盛りだくさんでワクワクしちゃいますね!! そんな夏を思いっきり楽しむために、夏バテ予防策をご紹介したいと思います。 ぜひ実践してみて下さい☆
- クーラーの温度は27℃設定で!
- 暑さで食欲がなくても、ご飯をしっかり食べましょう!
- 冷たいものばかりではなく、温かいものも飲みましょう!
- シャワーになりがちな季節ですが、湯ぶねに浸かりましょう!
- ・いものを食べて、代謝アップ!(食べ過ぎには注意)
これらを参考にして、暑い夏をENJOY気分で乗り切りましょう♪ くれぐれも水分補給は十分に行い、熱中症にはご注意下さい!!
神経伝導検査について
生理機能検査神経部門 田中佑果
はじめに
私たち人間は歩いたり、話をしたりと当たり前のように生活しています。もし神経に障害が発生すれば、こうした日常の単純な動作さえ困難になってきます。今回はこうした神経系の疾患を診断する神経機能検査について説明します。神経機能検査は主に、どの神経に異常があるのか、またどの位置が障害されているのかなどを調べる検査をしています。当院では、神経伝導検査、体性感覚誘発電位(SEP)、反復刺激検査、聴性脳幹反応(ABR)など色々な検査を行っていますが、今回はその中でも代表的な神経伝導検査を紹介します。
神経は脳や脊髄にある「中枢神経」とそこから全身に分布する「末梢神経」とに分類されます。さらに末梢神経は、脳が命令を出すことによって手足を動かす「運動神経」と、手足で感じた感覚を脳に伝える「感覚神経」に大きく分類されます。神経伝導検査では、この運動神経と感覚神経に電気刺激を与え興奮させることで、その反応を筋肉や神経上から記録し、神経の速さや伝わり方を評価します。
検査の流れ
- 仰向けになって寝ていただきます。
- 電極を手足に貼ります。
- 次に刺激電極で皮膚の上から微弱な電気を流し、測定していきます。電気といっても低周波の肩こりの治療器と同じようなものです。個人差はありますが、ピリピリとした痛みを伴う場合があります。1つの神経につき数ヵ所刺激します。(上肢の場合だと手首・肘・二の腕など、下肢の場合だと足首と膝裏など)
- 最後にメジャーで刺激間の長さを測ります。
※検査時間はだいたい30分くらいですが、目的とする神経が多かったりすると1時間ほどかかるときもあります。
検査結果
刺激すると、このような波形が出てきます。
運動神経を刺激して得られる波形は複合筋活動電位(compound muscle action potential:CMAP)、感覚神経を刺激して得られる波形は感覚神経活動電位(sensory nerve action potential:SNAP)と言われ、この波形から主に次の4つの項目をみて波形を解析していきます。
| ① 潜時(Latency) | 波形が立ち上がるまで→刺激してから筋肉あるいは神経が興奮するまでの時間 |
|---|---|
| ② 持続時間(Duration) | 波形の立ち上がりから基線に戻るまで→神経伝導速度にばらつきがないかどうか |
| ③ 振幅(Amplitude) | 基線と頂点との差→刺激が伝わった神経の数 |
| ④ 神経伝導速度 | メジャーで測定した刺激間の距離÷潜時 |
※神経伝導速度の正常値は上肢が50~60cm/s、下肢が40~50cm/sです。
検査結果の解釈
神経細胞は、下図のように神経細胞体から軸索が伸び、軸索の周りに髄鞘が取り巻いています。軸索は神経情報を伝達する働きを、髄鞘は伝達速度を速くするという働きがあります。
末梢神経の異常は軸索の障害、髄鞘の障害および両者が混在した病変に大別することができます。
| 〈軸索の障害〉 | 軸索が変性することで神経の情報を伝達できなくなるため振幅が小さくなりますが、神経伝導速度は正常範囲であることが多いです。主な疾患は、外傷や血管炎、薬物等の中毒によるものなどがあります。 |
|---|---|
| 〈髄鞘の障害〉 | 髄鞘が障害されることで神経線維によって神経伝達速度にばらつきが生じるため、CMAPは多相性となり、持続時間が長くなります。主な疾患は、ギラン・バレー症候群、慢性炎症性脱髄性多発神経炎(CIDP)、シャルコー・マリー・トゥース病などがあります。 |
神経伝導検査の注意事項
神経伝導検査は皮膚の温度や身長、年齢などで検査結果が変わります。また、微弱な電気を流すのでピリピリとした痛みを感じることがありますが、身体への悪影響はないので安心して検査を受けていただくことができます。
最後に
神経機能検査は、生理機能検査の中でも心電図や超音波検査に比べて比較的受ける頻度の少ない検査です。神経の検査と言われてもあまりイメージできない分野だと思うので、分からないことや気になることがあれば、気軽に質問してください。また、特にこの検査は力が入ってしまうと正しい波形が得られないため、検査が進まなくなってしまいます。最良の結果を得るためには患者さんの協力が必要です。一緒に頑張りましょう。
参考文献
神経伝導検査 ポケットマニュアル、医歯薬出版株式会社 臨床検査学講座第3版 生理機能検査学、医歯薬出版株式会社
検査部ニュース
学術関係報告
論文発表
- 杤尾人司:教科書には書いていない採血のコツ12:血管迷走神経反応(VVR)の回避法「患者を笑顔に」 検査と技術44:293, 2016
- 玉木恵里子, 杤尾人司, 木川雄一郎, 今井幸弘, 黒田真百美, 荒木直子, 登阪貴子, 橋本一樹, 簑輪和士, 加藤大典:造影超音波検査で化学療法前後のVascularityの変化を評価した 乳腺のMyeloid Sarcomaの1例, 日本超音波医学会2016- Vol.43 (No.3):509-514
- 杤尾人司, 玉木恵里子、今井幸広、岩崎信広、鄭浩柄、杉之下与志樹、簑輪和士、猪熊哲朗:ソナゾイド造影超音波の残存を認めた血管筋脂肪腫におけるCD68陽性細胞の腫瘍内局在について, 肝臓 2016,57:302-304
学会報告、講演
- 森田明子:急性骨髄性白血病におけるFLT3-ITD発現量の意義.第17回日本検査血液学会、福岡、 2016.8.6.
- 丸岡隼人:HRM解析を用いたAML遺伝子変異スクリーニング法.第17回日本検査血液学会,福岡,2016.8.6.
- 白石祐美, 丸岡隼人, 山本駿, 矢野由希子, 末岡馨, 老田達雄:HRM解析を用いたAMLにおけるRAS遺伝子検査法の確立. 第65回日本医学検査学会, 神戸, 2016.09.03
- 香原美咲, 松下隆史, 中村真実子, 南佳織, 菅原雅史, 佐々木一朗, 杤尾人司, 簑輪和士:手根管症候群では近位部の伝導速度が低下する-MCV、F波を用いた検討-. 第65回日本医学検査学会, 神戸, 2016.09.03
- 野本奈津美, 田村明代, 内藤拓也, 中村真実子, 仁木真理恵, 森田明子, 角田敏明, 老田達雄:当院臨床検査技術部におけるTeam STEPPS導入への取り組み. 第65回日本医学検査学会, 神戸, 2016.09.04
- 奈須聖子,竹川啓史,野上美由紀,仁木真理恵,内藤拓也,野村菜美子,神田彩,﨑園賢治:当院における過去10年間の血液培養検査の解析. 第65回日本医学検査学会, 神戸, 2016.09.04
- 森田明子、丸岡隼人、田代章人、尾松雅仁、井本秀志、上原慶一郎、今井幸弘:胸水細胞診を契機に早期診断に至ったTリンパ芽球性リンパ腫(T-LBL)の一例. 第65回日本医学検査学会, 神戸, 2016.09.03.
- 菅原雅史、井本秀志、松浦亮一郎、井本秀志、老田達雄:盲腸検体におけるEBER-ISH非特異反応についての検討. 第65回日本医学検査学会, 神戸, 2016.09.03.
- 杤尾人司、(森恵里子)、荒木直子、岩崎信広、簑輪和士、占野尚人、鄭浩柄、杉之下与志樹:超音波検査が有用であった食物残渣が充満した食道憩室(Zenkar憩室)の一例 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 松下隆史、岩崎信広、佐々木一朗、杤尾人司、江藤正明、鄭浩柄、杉之下与志樹、猪熊哲朗、大西栄次郎、今井幸弘:大腿神経原発後腹膜神経鞘腫の一例 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 松下隆史、香原美咲、中村真実子、浜田一美、佐々木一朗、幸原伸夫:脛骨神経F波最小潜時と脛骨神経体性感覚誘発電位(SEP)P40との相関-F波最小潜時からみたP40の予測-.第46回日本臨床神経生理学会 学術大会,福島,2016.10.27
- 田中佑果、登阪貴子、岩崎信広、佐々木一朗、杤尾人司、簑輪和士、鄭浩柄、杉之下与志樹、猪熊哲朗、島田誠一:超音波検査が有用であった卵巣滑脱ヘルニアの一症例 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 岩崎信広、シンポジウム「腹部超音波検査の進歩と新たなる展開」消化管超音波検査の原石-“initial 5 minutes” Ultrasonography in the gastrointestinal desease- 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 香原美咲, 岩崎信広, 佐々木一朗, 杤尾人司, 杉之下与志樹, 鄭浩柄, 猪熊哲朗:異なる臨床経過をたどったGVHD腸炎の2例. 日本超音波医学会第43回関西地方会学術集会,大阪, 2016.10.29
- 山本駿,太田光彦,紺田利子,角田敏明,菅沼直生子,野本奈津美,大畑淳子,谷知子,加地修一郎,古川裕:消化管の解剖学的位置異常に心エコー図検査が有用であった一例.日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
あとがき
日に日に寒さが増してきましたが、皆様いかがお過ごしでしょうか。そろそろコタツとみかんが恋しい季節となりましたね。みかん2~3個で1日分のビタミンCがとれるそうです。みかんのビタミンCには寒い冬を乗り切るためのパワーがたっぷりつまっているので、みかんを食べて冬を元気に乗りきりましょう! インフルエンザなどの流行時期となりますので、体調にお気をつけてお過ごしください。
血液培養検査について
微生物検査室 野上 美由紀
血液培養検査は、血液中の菌の有無や菌の種類を調べる検査です。血液は通常無菌状態ですが、菌が検出される場合は重篤な感染症につながる可能性があり、注意が必要です。
1. 血液培養検査の目的
本来、無菌状態である血液から菌が検出された場合、検出された菌の薬剤感受性検査を行うことにより、適切な抗菌薬を選択することができます。 菌にもたくさんの種類、性質があり、それらの違いによって治療で使用すべき抗菌薬が異なってきます。 原因となる菌はグラム陽性球菌(ブドウ球菌、レンサ球菌等)、グラム陰性桿菌(大腸菌、緑膿菌等) 、真菌など様々です。
2. 菌血症と敗血症
血液中に菌が証明されると菌血症と言い、その菌が原因で引き起こされる全身性炎症反応症候群を敗血症と言います。
全身性炎症反応症候群 systemic inflammatory response syndrome SIRS とは発熱や白血球増加などの全身の炎症の徴候によって特徴づけられる病態(SIRSの診断基準に合致する病態)です。
| SIRSの診断基準 |
下記項目のうち2項目以上が当てはまる場合
|
|---|
3. 血液の採取
菌には酸素を好む好気性菌と、酸素を嫌う嫌気性菌がいるので、好気ボトルと嫌気ボトルに採血します。菌の検出率を上げるためと、起炎菌とコンタミネーションとの判断をし易くするため、好気・嫌気ボトルを1セットとして通常2セット採血します。菌の検出率は、セットの数により以下のように違いがあります。
| 1セット | 73.2% |
|---|---|
| 2セット | 93.9% |
| 3セット | 96.9% |
このようにセット数が多いほど菌の検出率が上がります
4. 培養
培養陽性になった時点で、鏡検や菌名の同定・薬剤感受性検査に進みます。
5. 同定・薬剤感受性検査
1. 血液培養.陽性になったら、まずグラム染色をして鏡検します。見えた菌によって、 “ブドウ球菌の疑い”、“腸内細菌の疑い”など鏡検の結果を主治医に報告します。 鏡検で見えた菌に応じて、迅速法の薬剤感受性検査を行います。 血液寒天培地、チョコレート寒天培地、マッコンキー寒天培地などで培養します。
2. 迅速法により菌名を同定し、薬剤感受性検査を行い主治医に中間報告をします。
菌による見た目の違いや、簡易テスト、感受性で判断します。
薬剤に効果があると阻止円(菌の生えない輪っか)ができる。その大きさを測定し判定します。
3. 分析機器や同定キットにより菌名を同定し、薬剤感受性検査を行い主治医に最終報告をします。
6. まとめ
血液培養陽性になった場合、非常に重篤な状態に陥る事があります。血液培養陽性になり鏡検で菌を認めた時点で主治医に第一報を入れます。 迅速法での同定・薬剤感受性検査の結果が出たら中間報告をし、詳しい同定・薬剤感受性検査の結果が確定したら最終報告をするというように、 その時点で分っている情報を迅速に主治医に提供するように努めています。血液から菌が検出される原因は、感染性心内膜炎や尿路感染症などがあります。 迅速で正確な検査を行うのはもちろんですが、その感染巣や感染源の特定に関わる検査結果についても可能な限り情報提供をするように心がけています。
検査部ニュース
学術関係報告
学会報告、講演
- 松下隆史、香原美咲、中村真実子、浜田一美、佐々木一朗、幸原伸夫:脛骨神経F波最小潜時と脛骨神経体性感覚誘発電位(SEP)P40との相関-F波最小潜時からみたP40の予測-.第46回日本臨床神経生理学会 学術大会,福島,2016.10.27
- 杤尾人司、(森恵里子)、荒木直子、岩崎信広、簑輪和士、占野尚人、鄭浩柄、杉之下与志樹:超音波検査が有用であった食物残渣が充満した食道憩室(Zenkar憩室)の一例 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 松下隆史、岩崎信広、佐々木一朗、杤尾人司、江藤正明、鄭浩柄、杉之下与志樹、猪熊哲朗、大西栄次郎、今井幸弘:大腿神経原発後腹膜神経鞘腫の一例 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 田中佑果、登阪貴子、岩崎信広、佐々木一朗、杤尾人司、簑輪和士、鄭浩柄、杉之下与志樹、猪熊哲朗、島田誠一:超音波検査が有用であった卵巣滑脱ヘルニアの一症例 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 岩崎信広、シンポジウム「腹部超音波検査の進歩と新たなる展開」;消化管超音波検査の原石-“initial 5 minutes” Ultrasonography in the gastrointestinal desease- 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 香原美咲, 岩崎信広, 佐々木一朗, 杤尾人司, 杉之下与志樹, 鄭浩柄, 猪熊哲朗:異なる臨床経過をたどったGVHD腸炎の2例. 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 山本駿,太田光彦,紺田利子,角田敏明,菅沼直生子,野本奈津美,大畑淳子,谷知子,加地修一郎,古川裕:消化管の解剖学的位置異常に心エコー図検査が有用であった一例. 日本超音波医学会第43回関西地方会学術集会, 大阪, 2016.10.29
- 田代章人、井本秀志、森田明子、尾松雅仁、上原慶一郎、今井幸弘:好中球に中毒顆粒を認めG-CSF産生が示唆された転移性腫瘍の1例.第55回日本臨床細胞学会秋期大会、大分、2016.11.18.
- 丸岡隼人:造血器腫瘍における遺伝子検査 ~検査の原理と臨床的有用性について~. 奈良県臨床検査技師会・日本染色体遺伝子検査学会合同研修会, 奈良県, 2016.12.10
あとがき
寒さもゆるみ暖かくなってきましたが、皆様いかがお過ごしでしょうか。この時期、ウイルスなど目に見えない菌や花粉と戦っている方も少なくないことでしょう。ここで免疫力を上げる方法をいくつかご紹介したいと思います。
- 笑う
- 軽い運動をする
- 良い睡眠をとる
- 乳酸菌をとる
- 免疫力の上がる食事をとる (ブロッコリー、にんにく、納豆、きのこ、大根など)
これらを参考にして、免疫力アップを実践してみて下さい。 3月は別れの季節、4月は出会いの季節とこれから生活や仕事においても大きく変化が生じてきます。皆様健康に気をつけて4月からの新生活も頑張っていきましょう!
乳がんと病理検査
病理検査室 森本 美咲
最近話題となっている「乳がん」は、女性がかかるがんの中で最も多く、年々増加していると言われています。乳がんの一般的なスクリーニング検査としては、問診、触診、マンモグラフィー、超音波検査などがあります。臨床的に疑いがあると、MRI検査や病理検査などが行われ、悪性所見がないかどうか判断されます。
今回は、乳がんを疑われた場合や実際に乳がんと判明した場合、どのような病理検査(病理診断)が行われているのかを簡単にご紹介します。
病理検査については「特集第13号 病理検査室の紹介」をご覧ください。
乳がんに関する病理検査には大きく2つの役割があります。
1つ目は、乳房にしこりなどがある場合に病変の一部を採取して、がんかどうかを顕微鏡で調べます。痛み止めとして局所麻酔を行い、注射針より太い針で病変組織を採取します。採取された組織を標本にして顕微鏡で観察し、良性か悪性かを判断します。
2つ目は、乳がんと診断された場合に、乳がんの種類や性質、大きさ、進行度、転移の有無などを調べます。例えば、下の写真はどちらも乳がんですが、種類の異なる乳がんです。乳がんの種類によって組織の見え方にも違いがあり、臨床的予後が異なります。
さらに、乳がんの治療にも病理検査は深く関わっています。乳がんの治療は原則的には外科的切除(手術)であり、抗がん剤などの薬物療法(ホルモン療法、化学療法、分子標的治療)と放射線療法が併用されます。乳がんの進行度や転移の有無が治療方針に関係するというのはご存知の方も多いと思いますが、薬物療法の方針も病理検査により決定されることがあります。
乳がんには、女性ホルモンの一種であるエストロゲンやプロゲステロンが強く結合するエストロゲン受容体(ER)とプロゲステロン受容体(PgR)を持っているがん細胞があります。例えば、エストロゲン受容体を持っているがん細胞では、エストロゲンがその受容体に結合してがん細胞を増殖するように刺激します。このような乳がんでは、エストロゲンが結合できないようにブロックするホルモン療法が有効になります。ホルモン受容体の有無は、病理検査の免疫染色*1によって調べることができます。
また、分子標的治療薬*2が積極的に治療に使われるようになってきました。乳がんでは、細胞の表面に存在し、乳がんの増殖に関係しているとされているタンパク質(HER2)の作用を抑制する薬が注目されています。HER2タンパクを持っている乳がんには分子標的治療薬が適応となるため、当病理検査室ではHER2タンパクの有無も免疫染色を用いて調べています。
簡単にですが、乳がんと病理検査についてお話させていただきました。今回は紹介できませんでしたが、手術中に病変部の摘出範囲を決めるための「術中迅速検査」や、乳房から採取した細胞や分泌物を検査する「細胞診検査」も行っています。このように、病理検査は乳がんの診断、治療方針の決定に深くかかわっており、とても重要で不可欠な検査です。乳がんだけに限りませんが、迅速に正確な結果を提供できるようにスタッフ一同努力しています。
語句説明
*1免疫染色:組織や細胞に含まれるタンパク成分を染め出す染色。
*2分子標的治療薬:がんの発生や増殖などに関係する特定のタンパク質や遺伝子をターゲットにして、がん細胞の増殖を抑える薬。
検査部ニュース
学術関係報告
学会報告、講演
- 竹川啓史:臨床検査の現場で行う「真菌同定」の現状と課題.第28回日本臨床微生物学会総会・学術総会, 長崎, 2017.1.21
- 佐々木一朗:誘発電位測定.第10回関西脳波・筋電図セミナー,京都,2017.1.21
- 丸岡隼人:FCMの測定原理とデータの見方・考え方.第27回日臨技近畿支部血液研修会. 大阪府.2017.2.4
- 尾松雅仁:アミノ酸含有電解質製剤の投与制限実施前後でのBacillus cereus菌血症発 生件数の変化、第32回日本静脈経腸栄養学会学術集会、岡山、2017.2.23.
- 中 彩乃:悪性黒色腫に免疫染色を施行した1例、兵庫臨床細胞学会第33回総会、神戸、2017.3.4.
あとがき
新緑が眩しい季節になりました。皆様いかがお過ごしですか?窓から差し込む光がとてもキラキラしていて、思わず出掛けたくなってしまいますよね。さて、そんな過ごしやすい季節もあっと言う間、すぐに梅雨の憂鬱な季節に突入します。「ばいう」とはもともと中国から伝わった言葉で、当初は「黴雨」(黴[かび]がよく生えるため)という字だったところを、6月にその実が熟す梅の字に変えて「梅雨」となったという節があります。この梅の実はじめじめとした梅雨の時期の心身の不調によい効果があるそうです。一日一粒の梅干しと素敵な傘で梅雨を乗り切りましょう!
検体検査室の紹介
検体検査室 入江 礼香
皆さんが病院に来て採血をした後、その採血管は検体検査室に運ばれてきます。血液だけでなく尿検体やその他検体も運ばれてきます。そして、生化学検査・血液検査・一般検査等に分類し、様々な検査項目を測定しています。
採血
採血は、大人になっても少し怖いと感じる方も多いのではないでしょうか。採血管がたくさん出てくると、ギョッとしますよね。血液の総量は体重のおよそ8%なので、体重が50㎏の人では血液量は4000mL程度あります。先生がオーダーする検査項目によりますが、平均採取量10~20mL、採血管の本数が最も多い人でも50mLくらいなので心配いりません。そんなに多くはないのだと知っていれば少し安心ですよね。
検査には、全血(血液のまま)を用いるもの、血液を凝固させて分離した上澄み(血清)を用いるもの、抗凝固剤を混ぜて血液を固まらなくして分離した上澄み(血漿)を用いるものなど、検査する目的に応じて採血管の種類や本数が異なります。また、血液の凝固を防ぐ抗凝固剤にも検査項目によっていくつかの種類があります。抗凝固剤には血液の細胞を観察するのに適したEDTA(塩)や、血液ガスの測定に利用されるヘパリンなどがよく使用されています。
血球(赤血球・白血球・血小板)は全て造血幹細胞から分化して作られます。この造血幹細胞から成熟血液細胞になる過程(造血)は成人の場合、頭蓋骨や胸骨、肋骨、大腿骨などの骨髄で行われます。しかし骨髄の発達が未熟な段階である胎生期には主に肝臓や脾臓で造血が行われ、出生後に造血の場が骨髄へと徐々に代わっていきます。
血液の約45%は赤血球・白血球・血小板などの細胞成分で占められています。これらをまとめて血球といいます。残りの約55%は血漿とよばれています。血漿の90%が水、それに電解質(Na、K、CL等)や蛋白質、糖、アミノ酸、脂質、ビタミンやホルモン、老廃物などが溶けています。何らかの疾患や病態によっては、血液中の成分のバランスが変化したり、健康時には見られないような成分が現れたりします。
赤血球の主な役割は酸素運搬です。これはヘモグロビンが酸素と結合する能力を持っていることで成り立っています。赤血球の成分は蛋白質と電解質溶液で、蛋白質の95%以上がヘモグロビンです。赤血球にも寿命があります。120日間体内で活動した赤血球はマクロファージにより食べられ消えていってしまいます。
検査結果
| ①ALT(GPT) | 参考基準値 8-40 U/L | 肝臓に多く含まれている酵素です。 肝臓の障害、肝臓が生成する胆汁が流れる胆道の障害が起こると血液中に漏れ出し、濃度が高くなります。 |
|---|---|---|
| ②AST(GOT) | 参考基準値 8-40 U/L | 肝細胞をはじめ、腎臓や心臓の細胞内に多く含まれてる酵素です。 肝細胞などに障害が起こると血液中に流れ出るので、濃度が高くなります。 他の検査結果との関係性を見ながら、肝臓の障害の有無を判断します。 |
| ③γ-GT | 参考基準値 < 70 U/L | 肝臓、腎臓、膵臓、小腸などに含まれている酵素です。 肝臓の働きの1つであるアルコールや薬剤などを解毒する際、その働きを助けます。 そのため、飲酒により数値が高くなります。 |
| ④LD | 参考基準値 120-250 U/L | 肝臓をはじめ、心筋、血液、筋肉などの様々な臓器に存在する酵素です。 細胞がダメージを受けると血液中に流れだし、濃度が高くなります。 他の検査結果との関係性を見ながら、肝臓の障害の有無を判断します。 |
| ⑤総蛋白、アルブミン | 参考基準値 総蛋白 6.5-8.5 g/dL,アルブミン 3.9-4.9 g/dL | 肝臓には蛋白の合成を行う働きがあります。 肝臓の機能が低下すると、生成される蛋白の量が減るため、肝臓の異常を見つけることが出来ます。この検査では、血液から(赤血球や白血球などの)血球成分を除いた血清を用いて行います。 アルブミンは蛋白の一種で、血清蛋白のおよそ半分以上を占めています。 |
患者さまの待ち時間を少しでも短くするため、そして正確で信頼できる検査データを提供するため、我々スタッフ一同全力で取り組んでおります。
それでも、検体が検査室に到着してから、各検査項目毎に仕分けられ、必要な処理(遠心分離など)を行った後、測定を行い結果が出るまでには約1時間程度必要です。そして、前回測定した結果と大きく変化している場合や基準値を超えている場合には再検査を行うことで、正しい検査結果を報告するように努めています。
検査部ニュース
学術関係報告
学会報告、講演
- 堀香菜、太田光彦、大畑淳子、野村菜美子、野本奈津美、菅沼直生子、紺田利子、藤井洋子、角田敏明、谷知子、古川裕、小山忠明:大動脈弁置換術前後における左室流出路の形態変化:三次元経食道心エコー図を用いた検討.日本心エコー図学会第28回学術集会,名古屋,2017.4.23
- 丸岡隼人:抗体パネル作成の基礎知識と抗体パネル作成ワークショップ.BD FACS クリニカルソリューションセミナー IN 京都 2017, 京都,2017.5.20
- 森田明子:胸水中に腫瘍細胞が出現した胎児型横紋筋肉腫の1例.第58回日本臨床細胞学会総会 春期大会、大阪、2017.5.27.
- 菅原雅史、田代章人、南 佳織、森本美咲、尾松雅仁、森田明子、松浦亮一郎、井本秀志:肺癌における2種類のクローンの抗PD-L1抗体の染色性についての検討.第66回日本医学検査学会、千葉、2017.6.17.
- 南 佳織、菅原雅史、田代章人、森本美咲、尾松雅仁、森田明子、松浦亮一郎、井本秀志:CK-MNF116の染色性に異常が認められた一症例.第66回日本医学検査学会、千葉、2017.6.17.
- 森本美咲、菅原雅史、田代章人、南 佳織、尾松雅仁、森田明子、松浦亮一郎、井本秀志:腎血管筋脂肪腫におけるE-cadherinの発現:第66回日本医学検査学会、千葉、2017.6.18.
- 森田明子:混合表現型急性白血病(MPAL)の3症例.第66回日本医学検査学会,千葉、2017.6.18.
- 丸岡隼人:B細胞性悪性リンパ腫の診断における免疫グロブリン遺伝子再構成検査の有用性-微量生検材料を対象として-.第66回日本医学検査学会、千葉、2017.6.18.
- 矢野由希子:Hairy cell leukemia患者5例におけるBRAFV600E変異の検出.第66回日本医学検査学会、千葉、2017.6.18.
- 佐々木一朗:大脳誘発電位の基本と応用(検査室と手術室).第66回日本医学検査学会スキルアップセミナー、千葉、2017.6.16.
- 佐々木一朗:高感度脳波記録環境シミュレータを用いた教育モデルの導入と効果.第66回日本医学検査学会スキルアップセミナー、千葉、2017.6.17.
- 菅沼直生子、紺田利子、藤井洋子、野本奈津美、野村菜美子、大畑淳子、掘香奈、山本駿、城本千裕、長野真弥、角田敏明:開心術後に急速拡大した心尖部echo free spaceを偶発的に捉え診断に至った1例.第85回神戸臨床心エコー図研究会、神戸、2017.06.10
- 森田明子、丸岡隼人:急性骨髄性白血病におけるFLT3-ITD,NPM1変異と抗原発現の関連について.第18回日本検査血液学会、札幌、2017.7.22
- 丸岡隼人,小野祐一郎,加藤大祐,平本展大,末岡馨,矢野由希子,吉田昌弘,森田明子,簑輪和士,石川隆之:B細胞分離とHRM解析を用いた原発性マクログロブリン血症におけるMYD88L265P変異解析法.第18回日本検査血液学会、札幌、2017.7.23
- 岡馨,丸岡隼人,吉田昌弘,白石祐美,矢野由希子,簑輪和士,石川隆之:Multiplex PCR法を用いた骨髄増殖性腫瘍における遺伝子変異検出法の確立. 第18回日本検査血液学会、札幌、2017.7.23
- 佐々木一朗:法的脳死判定について~A to Z~.平成29年度5類型対象施設研修会,茨 城,2017.7.1.
あとがき
“夏の暑さもあと少し”と思ってからが毎年長い気がします。夏の疲れが出たのか風邪をひきかけてしまいました。夏は外気温とクーラーのきいた室内との温度差で体調を崩しやすいそうです。熱中症はもちろんのこと体調管理には注意しましょう。お買い物に出かけると、お店のカラーはすっかり秋色に変わっていました。植え込みから時々虫の声が聞こえるようにもなりました。秋はそこまで来ています。涼しくなってからのお出かけやイベントを楽しみに、好きなアイスやスイーツを食べたりして少し自分を甘やかしながら夏を乗り切りたいと思います。皆様も頑張り過ぎて夏バテなどされませんように。
造血幹細胞移植について
輸血検査管理室 張允禧
造血幹細胞移植とは?
造血幹細胞移植とは、病気にかかった血液細胞を健康な細胞と取り替える治療法です。腫瘍細胞や免疫担当細胞を「前処置」と呼ばれる化学療法や全身放射線治療で破壊した後、健康な造血幹細胞を点滴で移植します。
白血病やリンパ腫、多発性骨髄腫、再生不良性貧血などの病気が造血幹細胞移植の適応となります。造血幹細胞移植は、患者さん自身の造血幹細胞を事前に採取して凍結保存しておいて、前処置の後に移植する「自家移植」と、ドナー ※1の造血幹細胞を採取し前処置後の患者さんに移植する、「同種移植」の2種類に分けられます。
移植の成否に関わる「HLA」
造血幹細胞移植のドナーは患者さんの白血球のタイプ(HLA)が適合していなくてはいけません。いわゆる血液型(ABO型)が赤血球のタイプであるように、白血球にも様々なタイプがあります。その中でも、造血幹細胞移植において重要なのはHLA-A, -B, -DRの3種類であり、これらが 一致するドナーを探します。血縁者からドナーが見つからないときは、骨髄バンクを利用してドナーを探します。日本骨髄バンクでは、全国でドナー登録された「ドナー候補者」と患者さんとの仲介を行っています。
HLAが異なるとどうなるの?
移植されたドナー由来の造血幹細胞が非自己と認識され、患者由来の免疫担当細胞に排除されてしまうことを拒絶といい、そのような合併症を「生着不全」と言います。生着不全が起こると感染のリスクが高まり、場合によっては再移植をする事もあるため、患者さんの負担が大きくなります。これに対して、移植した造血幹細胞が生着した後、移植を受けた患者さんを攻撃してしまう合併症を、「GVHD(移植片対宿主病)」と言います。GVHDが起こると特に皮膚、肝臓、消化管が傷害され、重度の場合は致命的になります。HLAのタイプが異なると、このような重篤な合併症を生じる危険性が高くなります。このように、HLAが一致したドナーを選ぶことは、移植を受けた患者さんの予後を大きく左右する重要なポイントとなります。
造血幹細胞移植の種類
造血幹細胞移植は、細胞の由来と採取部位によって3種類に分ける事ができます。ひとつずつ、特徴と利点・欠点を紹介します。
1)骨髄移植
ドナーの骨髄から造血幹細胞を採取し移植する方法です。骨盤の後ろ側にある腸骨の色々な部位を何十回か穿刺して採取します。
2)臍帯血移植
分娩後の胎盤・臍帯に残った胎児由来の血液(臍帯血)に含まれる造血幹細胞を移植する方法です。臍帯血移植は、日本臍帯血バンクネットワークの登録施設でのみ受けることができます。
3)末梢血幹細胞移植
通常、造血幹細胞は骨髄にあり末梢血にはほとんどありませんが、G-CSFを投与することで、造血幹細胞を末梢血内に集め採取する方法です。
当院における造血幹細胞移植
当院では、骨髄移植、臍帯血移植、および末梢血幹細胞移植を行っています。2016年には、骨髄移植8件 / 臍帯血移植24件 / 末梢血幹細胞移植41件(うち同種移植が10件、自家移植が31件)の移植が行われました。※先端医療センターでの移植含む
また、末梢血幹細胞自家移植の際には、血液内科医師や薬剤師と協力して細胞調整を行っています。
まとめ
- 造血幹細胞移植の概要について簡単に紹介させていただきました。
- 造血幹細胞移植には、臨床検査技師だけでなく、医師や看護師、薬剤師、臨床工学技士、放射線技師等、様々な職種の医療従事者が関わっています。
- 輸血検査管理室でも、チーム医療の一員として他職種間で連携をとりながら、少しでも多くの患者さんの移植の成功に貢献できるよう、日々努力しています。
用語説明
※1 ドナー:移植細胞の提供者のこと。
参考文献
・病気が見える 血液vol.5, 医療情報化学研究所 編集, メディックメディア 発行
・目で見る造血幹細胞移植カウンセリング・ブック, NOVARTIS ONCOLOGY 発行
検査部ニュース
学術関係報告
学会報告、講演
- 丸岡隼人:造血器腫瘍のおけるFCMおよび遺伝子検査の有用性.福井県臨床検査技師会 染色体・遺伝子部門/臨床血液部門合同研修会,福井,2017.09.30
- 大畑淳子, 太田光彦, 紺田利子, 角田敏明, 金基泰, 北井豪, 加地修一郎, 谷知子, 小山忠明, 古川裕:大動脈弁置換術後14年目に急性の人工弁機能不全を認めた1例.日本超音波医学会第44回関西地方会学術集会, 大阪, 2017.09.23
- 岩崎信広:「多血性肝腫瘍の一例(解答編)」、「上行結腸perivascular epithelioid celltumorの一例」第134回大阪超音波研究会、大阪国際会議場、2017.9.20
- 岩崎信広:ワークショップ“超音波で考える腹部疾患”「消化管」. 日本超音波医学会第44回関西地方会学術集会、大阪、2017.9.23
- 岩崎信広:「腹部エコーのはじまり」第3回兵庫県地域医師超音波ハンズオンセミナー、神戸、2017.9.18
- 岩崎信広:「膵臓・腎臓」第3回兵庫県地域医師超音波ハンズオンセミナー、神戸、2017.9.10
- 菅原雅史:「膵臓・腎臓の超音波検査」「膵臓・腎臓」第3回兵庫県地域医師超音波ハンズオンセミナー、神戸、2017.9.18
- 田中佑果:「膵臓・腎臓」第3回兵庫県地域医師超音波ハンズオンセミナー、神戸、2017.9.18
- 田中佑果,杤尾人司,鄭浩柄,岩崎信広,佐々木一朗, 簑輪和士,杉之下与志樹,今井幸弘,猪熊哲朗:特徴的なUS像を呈した粘液癌肝転移の一例.日本超音波医学会第44回関西地方会学術集会, 大阪, 2017.09.23
- 菅原雅史,杤尾人司,岩崎信広,佐々木一朗,簑輪和士,杉之下与志樹,鈴木一生,藤倉航平,今井幸広:ヘルニアを契機にUS診断した停留精巣腫瘍に随伴する清策水腫の一例. 日本超音波医学会第44回関西地方会学術集会, 大阪, 2017.09.23
- 山本駿,太田光彦,紺田利子,角田利明,野本奈津実,野村菜美子,谷知子,加地修一郎,小山忠明,古川裕:外巻き生体弁を使用した大動脈弁置換術後に早期の構造的弁劣化をきたした2例.日本超音波医学会第44回関西地方会学術集会, 大阪, 2017.09.23
- 松下隆史,岩崎信広, 杤尾人司,杉之下与志樹,鄭浩柄,猪熊哲朗,今井幸広:造影USにて特異的な像を呈した硬化性血管内皮腫の一例. 日本超音波医学会第44回関西地方会学術集会, 大阪, 2017.09.23
- 玉木 明子:骨髄中の赤芽球が50%を超えた時の考え方.第57回日臨技近畿支部医学検査学会、京都、2017.10.29.
- 井本 秀志:病理検査室のインシデントとその対策~当院の作業手順から見えてくる事は?~.第57回日臨技近畿支部医学検査学会、京都、2017.10.29.
あとがき
季節の移り変わりは体調も変化しやすく、今年はとくに10月に入ってからの寒暖差が多きく 夏から秋を飛び越えて冬が来たかのような気温の変化に体も心も衣替えできずに戸惑っています。イギリスの自然科学者チャールズ・ロバート・ダーウィンは “It is not the strongest of the species that survives, nor the most intelligent that survives. It is the one that is most adaptable to change.” (最も強い者が生き残るのではなく、最も賢い者が生き延びるのでもない。唯一生き残ることが出来るのは、変化できる者である。) という名言を遺されています。たかが気温の変化でこのような名言を引用するのはと思われるかもしれませんが、私たちは気温という自然現象の一部分にしか過ぎない変化でさえ大きな影響を受けます。現代社会においては抗うことのできない変化も多く存在し 、適応できないような場合も多々あります。しかし、心身ともに余裕をもって生きてゆくためには少しでも多くの事に適応できる者になるよう努力をしていく必要があります。戸惑わないよう一歩踏み込んでみませんか。
心電図検査について
生理機能検査室 心肺部門 長野真弥 ・ 則政文子
A) 心電図検査って?
はじめに
皆さんは健康診断、もしくは病院で心電図検査を受けたことがありますか。世の中には色々な検査がありますが心電図検査は比較的馴染みのあるものではないでしょうか。どういった検査かと言うと、その名の通り心臓の働きを調べる検査の一つです。心臓という臓器は微量の電気を周期的に発生していて、その電気が心臓の筋肉(心筋)を伝わることによって、収縮・拡張し、その力で全身に大量の血液を送っています。心電図検査は、その電気の状態をチェックして、心臓が規則正しく動いているか、心筋に傷害がないか、などを検査しているのです。
心臓の電気の伝わり方(刺激伝導系)
心臓の興奮刺激は右心房にある洞結節で一定時間ごとに発生します。この間隔によって心臓の拍動の速さ、つまり「心拍数」が決まります。洞結節で発生した興奮刺激は心房の収縮を引き起こし、心房内の心筋を通って房室結節へと伝わります。さらに興奮刺激は房室結節からヒス束→左脚・右脚→プルキンエ線維へと順々に伝わり、心室の収縮を引き起こします。簡単に言うと、この刺激伝導系の電気の流れを波形として表したのが心電図となります。
以下の図は刺激伝導系の仕組みをわかりやすく説明したものです。
心電図ってどんな波形?
心電図波形は正常であれば以下のようにP波、QRS波、T波、そしてU波の順に波形が出現していきます。先に述べたように心電図は心臓の電気の流れを表しており、私たち臨床検査技師は各波形成分を細かく観察しながら検査を進めていきます。
B) どうやって検査するの?
- まず胸、両手首、両足を出してベッドに仰向けに寝ていただきます。この時、足は軽く開いて両手は体から少し離します。
- 洗濯バサミのような四肢電極を手足に、そしてタコの吸盤のような胸部電極を胸にそれぞれつけていきます。少し冷たく感じることはありますが、痛みは伴いません。
- 電極をつけ終わったら、体の力を抜いてリラックスし、手足等を動かさないようにします。記録自体は1分、長くても2分程度で終わりますが、動いたり体に力が入ったりスムーズに記録できない場合は時間がかかります。
- 記録が終わりましたら電極を外して検査終了です。検査準備から終了までスムーズにいけば5分程度です(患者さんの状態や検査の状況によりこの限りではありません)。
C) 検査のコツ(綺麗な心電図をとるために…)
当院では私たち臨床検査技師が心電図をとる際に、心がけていることがあります。それは「波形を判読する上で支障のない」心電図波形を残すことです。普段ルーチン業務をしていると以下のような様々なケースに遭遇することになります。そんな時、「少々汚い波形やけど、ま、いっか!」と簡単にあきらめるのではなく、何とかして綺麗な波形となるよう努力をしています。
-例-
Ⅰ. モニターに心電図波形が出ない
対応) 四肢誘導電極が乾燥していないか、断線がないか等の確認。
Ⅱ. 筋電図の混入
対応) 全身の力が入り過ぎているのでリラックスするように声掛けをする。枕の位置を変えてみる。
Ⅲ. 四肢誘導の基線の揺れ
対応) 体動はないか、皮膚との接触はどうか、電極が乾燥していないか、電極の金具に緩みはないかどうか、の確認。
Ⅳ. 胸部誘導全体の揺れ
対応) 呼吸による影響を除く(大きな息をさせない、息止めをしてもらう)。
Ⅴ. 各々の基線の揺れ
対応) 皮膚との接触、電極外れの確認。 胸毛、乾燥肌、仰臥位になれない場合、痩せ型の人の場合はクリームを使用する。
Ⅵ. 乳幼児が検査に来たときは?
対応) 小児用のシールタイプの電極を使用する(じっとしておくことが難しく、通常の電極では外れやすいため)。
Ⅶ. 四肢切断の方や震えがとまらない場合は?
対応) 四肢電極を肩・腰で代用する(末梢側で計測するより中枢側の方が影響が少ない)。
D) 検査室からのお願い!(スムーズに検査を受けていただくために…)
- 服を脱いでいただく必要はありませんが、手首と足首そして胸を出しやすいような服装で来ていただくとスムーズに検査が行えます(検査日はワンピースやボディースーツの着用はなるべくご遠慮下さい)。
- 特に女性の方はタイツやストッキングの着用はなるべく避けていただくと助かります(足首にも電極を付けるため、タイツ等は脱いでいただくことになります)。
- 腕時計程度なら構いませんが、多くのアクセサリー(ネックレス等)を身に着けておられる場合は、検査中は取り外していただくことがあります。
E) 実際の波形(心電図で判明!様々なタイプの不整脈)
< 解説 > 正常波形。
・QRS波の形は同じで、出現するタイミングも早すぎず、遅すぎず、一定のリズムである。
< 解説 > 心室性期外収縮。
・4拍目、5拍目にそれまでとは形の異なるQRS波が、より早いタイミングで2連続で出現。いわゆる「脈が飛ぶ/脈が抜ける」と言われるタイプの不整脈。
・「期外収縮」は、本来電気が発電される正常な場所ではない場所から電気が速く発電されてしまう為に発生します。
< 解説 > 心房細動(頻脈性)。
・いわゆる「胸がドキドキする」といった頻脈タイプの不整脈の代表。
・心臓を動かす為の電気が異常に速くつくられたり、電気の通り道が異常な場所に出来て、そこを電気が通ってしまう為に発生します。
< 解説 > 高度房室ブロック。
・脈がゆっくりとなる徐脈タイプの不整脈の一つ。
・徐脈は、心臓を動かす為の電気が作られなくなったり、電気の通り道の途中で電気が通らなくなってしまう為に発生します。
・何もしていないのにフラッとするといった症状がある場合は、心臓を動かす電気の作り方に異常があって一時的に心臓が止まっている可能性もあるので注意が必要です。
F) 最後に
簡単にですが心電図検査についてまとめました。本検査は不整脈や狭心症、そして心筋梗塞といった怖い病気を発見する手がかりになり得る重要な検査となります。一見シンプルに見える検査ですが、私たち臨床検査技師は様々な工夫をしながら最良の検査データを臨床医に提供できるよう日々努力しています。 短時間で終わり、苦痛のない安全な検査ですので、今後検査を受ける機会があれば是非安心して来院していただければと思います。
参考文献
・循環機能検査技術教本監修: 一般社団法人日本臨床衛生検査技師会
・病気がみえるvol.2 循環器第4版
・ハート先生の心電図教室 part 1 改訂第二版
検査部ニュース
学術関係報告
尾人司:教科書には書いていない採血のコツ12:血管迷走神経反射(VVR)回避法「患者を笑顔に」
検査と技術44:427, 2016
学会報告、講演
- 田代章人、井本秀志、森田明子、尾松雅仁、中綾乃、山下大祐、今井幸弘:子宮ポリープ状異型腺筋腫(Atypical polypoid adenomyoma APAM)の細胞像.第56回日本臨床細胞学会秋季大会、福岡、2017.11.19.
- 中綾乃、井本秀志、森田明子、尾松雅仁、田代章人、菅原雅史、山下大祐、上原慶一郎、今井幸弘:悪性黒色腫に免疫染色を施行した1例.第56回日本臨床細胞学会秋季大会、福岡、2017.11.19.
- 山本駿,太田光彦,紺田利子,角田敏明,菅沼直生子,野本奈津美,野村菜美子,大畑淳子,堀香奈,佐々木康博,金基泰,北井豪,山根崇史,江原夏彦,小堀敦志,木下愼,加地修一郎,古川裕,小山忠明:Trifecta弁を使用した大動脈弁置換術後に早期の構造的弁劣化をきたした2症例に関する検討.第8回日本心臓弁膜症学会,東京,2017.11.24.
- 松下隆史:神経電動検査と上肢3点で計測した皮膚温の相関.第47回日本臨床神経生理学会学術大会、横浜,2017.11.30
- 佐々木一朗:術中神経モニタリングの先にあるもの.第54回日本臨床神経生理学会技術講習会、横浜,2017.12.1
- 吉田昌弘:造血器腫瘍における遺伝子検査を学ぼう!.第9回シスメックスユーザー研修 会.兵庫.2017.12.02
- 矢野由希子:フローサイトメトリーはなぜすごいのか.第9回シスメックスユーザー研修 会.兵庫.2017.12.02
- 竹本優允,奈須聖子,野上美由紀,仁木真理恵,神田彩,有働仁美,牧田実央,竹川啓史: Salmonella O4群菌血症による閉鎖筋膿瘍、骨髄炎の1症例. 第23回兵庫県医学検査学会. 神戸.2017.12.10.
- 有働仁美,奈須聖子,野上美由紀,仁木真理恵,神田彩, 竹本優允,牧田実央,竹川啓史:当院で検出された糞線虫症2例. 第23回兵庫県医学検査学会. 神戸.2017.12.10.
- 中山友理香,松浦亮一郎,井本秀志,森田明子,尾松雅仁,田代章人,中綾乃,森本美咲,南 佳織,今井幸弘: パラフィン切片における好酸菌染色法の検討.第23回兵庫県医学検査学会. 神戸.2017.12.10.
あとがき
毎年、年明けは、なにか新しいことを始めようという気持ちになりますが、気が付けば、もう2月も半ば。結局、何も始めることが出来ずに、毎年、時間だけが過ぎてゆきます。 もうすぐ3月、弥生とも呼ばれております。諸説ありますが、「草木がいよいよ生い茂る月」という意味の「木草(きくさ)弥(い)や生(お)ひ茂る月(づき)」が詰まって「やよい」になったという説があります。 少しでも早く春を感じられればと思い、庭に梅を植えていますが、その梅がちらほら咲きはじめました。少しづつではありますが、春が近づいてきています。 さて、新しい年度から、なにを新たに始めようかと、思案中です。
新型コロナウイルスのPCR検査について
細胞遺伝子検査室 姫野真由子
PCR(polymerase chain reaction)とは、特別な試薬と機器を使って目的とする遺伝子を増幅させる技術のことです。この技術はヒトの病的遺伝子の検出や、ウイルスの検出に利用されています。
当院ではこの技術を使って、主に白血病・悪性リンパ腫などの血液疾患に見られる遺伝子異常を調べていますが、ここ最近の新型コロナウイルス(SARS-CoV-2)流行に伴い、今までのノウハウを生かして院内で新型コロナウイルスのPCR検査を始めました。今回は新型コロナウイルスのPCR検査についてご紹介します。
新型コロナウイルス 検査の大まかな流れ
- 綿棒で患者さんの鼻咽頭から検体を取る
- 検査室にてウイルスからRNAを抽出する
- PCRの試薬を準備する
- CFX96(専用の機械)にかけて、結果判定する
RNA抽出
ウイルスそのものをそのままPCRにかけることはできないので、Maxwell RSCという専用の機械を用いてRNAを抽出します。
綿棒についたウイルスを一旦溶液の中に落としたものと、試薬を混ぜて機械に投入すれば約40分でRNA抽出が完了します。
一見簡単そうに思えるRNA抽出ですが、曝露リスクがあるため安全キャビネット内で作業します。また手袋を二重にし、エプロン・マスク・ゴーグルを着用して、こまめにアルコール綿で手指消毒をしています。
検査法について
国立感染症研究所が提示している新型コロナウイルス病原体検出法のうち、当院ではリアルタイムOne-step RT-PCR法を採用しています。ウイルスから抽出したRNAをcDNAに変換する逆転写反応(RT)と、リアルタイムPCRを組み合わせたものです。RTとリアルタイムPCRを1本のチューブで連続して行なうためコンタミネーションの心配がなく、操作が簡便です。
※逆転写反応(RT):逆転写酵素によりRNAをcDNAに変換する操作のことです。RNAはそのままPCRに使用することができないため、RNAを使ったPCRを実施するときはcDNAに変換する必要があります。
PCRとは
PCRとは、検体と特殊な試薬を混ぜてサーマルサイクラーという機械にかけることで、目的遺伝子を増幅する技術のことです。
PCRはディネーチャー、アニーリング、伸長反応を1サイクルとして、この流れを何度も繰り返すことで遺伝子を増幅します。
| ディネーチャー | DNAを高温で熱することで、二本鎖の状態から一本鎖にするステップです。 |
|---|---|
| アニーリング | 一本鎖になったDNAに、プライマーをくっつけるステップです。プライマーは、増やしたい目的遺伝子に合うように設計された短い遺伝子配列のことです。 |
| 伸長反応 | アニーリングでくっついたプライマーからDNAが伸びて、新しい二本鎖DNAを作り出すステップです。 |
リアルタイムPCRとは
DNAを鋳型としてPCRを行い、鋳型DNAが増幅する様子を 蛍光色素を用いてリアルタイムに測定することで鋳型DNAの定量を行なう手法です。
リアルタイムPCRには様々な手法がありますが、新型コロナウイルスの検出には蛍光色素が標識されたプローブを用いる方法で行なわれます。
プローブは、レポーター(蛍光色素)とこれを阻害するクエンチャーが標識された短い遺伝子配列であり、アニーリングの時に鋳型DNAにくっつきます。このときレポーターはクエンチャーに阻害されているため、励起光を当てても蛍光を発することができません。
伸長反応が進むとプローブは分解され、レポーターは励起光に反応して蛍光を発します。この蛍光を読み取ることで定量をしています。
結果の解析
リアルタイムPCRが終わると、以下のような曲線が作られます。
この曲線は増幅曲線といいます。縦軸が蛍光量、横軸がサイクル数(反応時間)です。
リアルタイムPCRが進行し、ある一定の蛍光量に達したとき、この図のように曲線が立ち上がります。この場合は陽性と判定します。PCRの反応時間内に蛍光量が増えない場合、曲線は平坦なままとなり、陰性と判定します。
この場合、1と2は曲線が立ち上がっているので陽性、3は平坦なままなので陰性と判定します。
まとめ
PCRは一見簡単に見えますが、試薬の入れ間違いやコンタミネーションなどに気を使わなくてはならない検査です。またPCRは検体の質により偽陰性の可能性が少なからずあるため、重要な検査ではありますが、絶対的な検査とは言えません。
そのため、
「PCR陰性=コロナにかかっていない」
とはなりません。
PCRだけでなく、肺のレントゲンや臨床症状、患者さんの問診等の情報を総合的に考えることが重要です。
外来採血室のご紹介
外来採血室 山本剛
採血により身体中を流れている血液成分を調べることで、「病気の診断」や「病状の把握」を行うために必要な医療行為です。採血は静脈から血液を採取するため安全性の高い手技になりますが、まれに「採血合併症」が起こることもあります。採血で確認したい生体情報が採血合併症の危険性より高いと判断された場合に担当医より採血がオーダーされます。「採血合併症」については後述しますが、採血の必要性と危険性をご理解した上で採血を受けて頂きますようお願いします。
2.採血を受けられる患者さんへのお願い
医療安全の観点から採血時に以下の内容について確認を行います(図1)。該当する方は採血時に採血スタッフにお申し出ください。
1)採血を行う腕の確認
採血は駆血帯(くけつたい)で静脈にある血液をせき止めて行いますが、駆血帯を巻くことができない場合があります。下記に該当する患者さんは事前にお申し出ください。
①人工透析用のシャント造設がある方
②化学療法の為にポート留置されている方
③血糖自己管理用のリブレを装着されている方
④上皮小体の植え込みがある方
また、アレルギー歴がある場合も採血時にお申し出ください。
⑤アルコールに対するアレルギー歴がある:アルコール以外の消毒薬を使います。
⑥テープに対するアレルギー歴がある:絆創膏や紙包帯を使います。
2)採血合併症についてのご案内
採血時はまれに次のような健康被害(採血合併症)を生じることがあります(図2)。
①神経損傷:刺した場所の痛みや手先のしびれ感がでます。
②皮下血腫(青あざ):採血した後に止血が十分でないときにできます。
③アレルギー:消毒用アルコールやテープでかぶれて赤くなったり、かゆくなったりします。
④血管迷走神経反射(気分不良):刺した時に神経の反射で起こします。血圧が低下したり、頻脈になります。
3.採血までの流れ
1)受付
①受付は自動受付機、またはC受付(有人)で行います。診察券をご準備ください。
②受付で『受付番号』の発番をおこなってください。番号が出ない場合はC受付(有人)で発券を行ってください。
③受付時間の開始時間は以下の通りです。
ア)自動受付機:AM7:30から開始しています。
イ)C受付(有人):AM8:15から開始します。
なお、自動受付機でも内容確認が必要な場合は「受付Cカウンターへお越し下さい。」と表示されます。その場合はC受付(有人)にお回り頂くことがあります。ご了承ください。
④掲示板に『受付番号』が表示されるまで外待合でお待ちください。表示されたら採血室にお入りください。
⑤長袖を着用している場合は採血する側の腕を出してお待ちください。
2)採血の準備
①採血台の掲示板に『受付番号』が表示されたら採血台までお進みください。
②『受付番号票』を採血担当者にお渡しください。名前の確認時に必要です。
③本人確認のため「お名前」と「生年月日」をお聞きします。
④項目(レニン採血など)によっては30分間安静後に採血を実施することがあります。担当医の指示に従ってください。
⑤糖負荷試験の場合はブドウ糖液を飲んだ後に30分、60分、120分後に採血を行います。
3)採血の実施
①主に肘から採血を行いますので、採血枕に肘を乗せてください。
②親指を中にして軽く握ってください。
③肘は伸ばして採血をします。
④肘で採れない場合は前腕や手背で採血をさせて頂くことがあります。
⑤車いすをご利用している場合は座ったままで採血を行います。その場合は順番が前後することがございます。ご了承ください。
⑥気分がすぐれないとき、過去に気分不良になった場合は、ベッド上で採血をしますのでお申し出ください。
⑦抜針後は採血した場所を5分間しっかりと押さえてください(圧迫止血)。血液をサラサラにするお薬を服用している方は10分間しっかりと押さえてください。
4.採血室の混雑状況
午前中は大変混雑しますので、採血のみで来院される方は14時以降が比較的空いており、おすすめです(図3)。採血室の待ち時間解消のためにご協力お願いします。
当院臨床検査技術部はISO15189の認定を取得しております。外来採血室ではTAT(turn around time:検査にかかる応答時間)管理により患者さんの待ち時間改善に努めております。2019年度から2020年度にかけては待ち時間短縮するためにスタッフの配置や業務内容を改善し待ち時間を大幅に短くすることができました(図4)。今後も継続的に待ち時間調査を行い、更なる待ち時間短縮に努めてまいります。
5.外来採血室の概要
①外来採血室は9ブース設置し、臨床検査技師と看護師が採血の担当をしています。
②臨床検査技師による採血業務は検体検査や生理検査に関わらず全ての職員が対応しています。
③採血患者数は毎日500~700名程度です。
④採血システムはシスメックスCNAで構築されており、採血管供給装置はBC-ROBO 8001 RFIDを2機設置しています。
⑤新人教育用に年間を通して色々な研修を行っています。
6.その他
①当日は採血しやすい服でご来院ください。
②袖が詰まった服装の場合は肘で採血ができなかったり、止血が十分に行えない場合があります。
◆◆特集第27号◆◆
関節リウマチの活動性評価を中心とした当院における関節エコーの取り組み
腹部超音波検査室 矢野由希子
関節リウマチ(rheumatoid arthritis:RA)とは
関節リウマチ(rheumatoid arthritis:RA)とは
滑膜関節*):主に四肢にある可動性の高い関節。手関節、手指・足趾関節、肘・肩関節、膝・足関節が含まれる。
RAの評価法
従来RAの診断には2010 ACR/EULARで提唱された関節リウマチ診断基準が用いられている(図1)。この基準においてRAの診断には圧痛や腫脹の評価が重要となるが、これらは患者や診察者の主観によるところが大きく時に正確な診断が困難となることがある。
そこで圧痛や腫脹を客観的に評価することができる画像検査として簡便で安全性が高くかつ感度の高い超音波検査が注目され、2011年2月に日本リウマチ学会により「関節エコー撮像法ガイドライン」が策定された。この標準化で滑膜増殖および炎症所見の半定量スコアが提示され(図2・3)、関節におけるRAの活動性の視覚的評価および客観性の高いフォローアップが可能となった。
当院で経験したRA症例
患 者:73歳 女性
主 訴:手の痛み
現病歴:5ヶ月前から両手、両手指関節痛が出現。改善、増悪を繰り返している。 血液検査ではCRP
0.18mg/dL、赤沈1時間値20mm。MRIでは明らかな異常所見は認めず。腫脹は両手指とも軽度で
圧痛はなし。RAが疑われたが確診に至らず両手の手関節及びMCP関節、PIP関節、IP関節にエコー
を実施した。
両手関節(橈側、尺側)及び両手のMCP関節(上図左赤丸で示す部位)に滑膜増殖が認められた。上図右に右手第5指MCP関節のエコー画像を示す(GSグレード2,PDグレード2)。
抗CCP抗体,RFともに陰性であったがエコー所見よりseronegative RAとして治療が開始された。
10ヶ月後,両手指ともに滑膜増殖の改善を認めた。右手第5指MCP関節の滑膜増殖も改善(GSグレード0,PDグレード0)を認めた。
当院で経験した症例
患 者:36歳 男性
主 訴:両側アキレス腱の痛み
現病歴:15年前から運動時に左側優位のアキレス腱の痛みが出現(月1回程度)。症状は数日~2週間程度
持続する。他院で整形外科などを受診するも改善せず3ヶ月前に当院を受診。
血液検査ではCRP 0.54 mg/dL、抗核抗体40倍(Homogeneous/Speckled)。末梢神経、筋障害なし。骨盤・腰椎X線検査、仙腸関節MRIいずれも異常所見を認めず。若年男性のアキレス腱痛であり、脊椎関節炎などを疑い足部を中心にエコーを実施した。
腱付着部炎のスクリーニングで腱付着部炎は認めなかったが左側優位に両側アキレス腱の肥厚および内部血流の亢進を認めた。X線検査でも左側18mm、右側13mm(男性のアキレス腱の正常値は4-5mm)と左側優位のアキレス腱の肥厚を認めた。血液検査でLDLコレステロールが265mg/dLと高値であったため家族性高コレステロール血症が疑われ、遺伝子検査を行ったところ原因4遺伝子の一つであるLDLRの変異がヘテロ接合体で検出され確定診断となった。関節エコーが腱周囲の病変の精査に有用であった症例である。
最後に
ガイドラインによって標準化されたものの、関節エコーは超音波検査である以上検査結果が術者の熟練度に依存する、MRIやCTと比較すると再現性や客観性が劣るという短所がある。しかし放射線暴露なく複数の関節を簡便かつ詳細に短時間、低コストで評価できることは関節エコーの大きな強みであり、治療が長期に渡る傾向があるRAの活動性評価を中心に重要な役割を果たしている。
参考文献
1)一般社団法人日本リウマチ学会.“メディカルスタッフのためのライフステージに応じた関節リウマチ支援者ガイド”. https://www.ryumachi-jp.com/medical-staff/life-stage-guide/,2024年7月閲覧
2)日本リウマチ学会 関節リウマチ超音波標準化委員会.リウマチ診療のための関節エコー撮像法ガイドライン.羊土社.2011
3)谷村一秀.関節エコー画像診断の進歩.臨床リウマチ.2016,vol.28,p.7-15
POT法によるMRSAの解析
微生物検査 神田 彩
近年、薬剤耐性菌の蔓延・拡散が問題視されています。薬剤耐性菌とは抗菌薬に対して薬剤耐性を獲得し抗菌薬が効かない・効きにくい状態に変化した細菌です。薬剤耐性菌による感染症は治療薬の選択肢が限られるためしばしば治療が難航し、死亡率も高いことが報告されています。
なかでも、メチシリン耐性黄色ブドウ球菌(MRSA)は医療現場で最も多く検出される薬剤耐性菌であり、院内感染の原因菌として感染対策を実施すべき非常に重要な病原菌のひとつです。当院では感染制御チーム(ICT)の活動の一環としてMRSAを含む薬剤耐性菌の検出状況を監視しており、院内感染を減らすよう努めています。臨床検査技師もICTの一員としてカンファレンスやラウンドに参加しており、微生物検査室からは薬剤耐性菌に関する情報を提供することでその活動に貢献しています。その一助としてPOT法を導入し、遺伝子型を決定することで院内伝播や持ち込みなどの感染情報を提供しています。
今回はPOT法の原理や利点、ICTでの活用法などをご紹介します。
POT法とは
検出されたMRSAが院外から持ち込まれたものなのか、病院内で伝搬したものかを判断する必要が出てきます。院内伝搬が疑われる症例が複数報告された場合には、アウトブレイク(ある集団の中で突発的に多数の感染症が発症すること)を防ぐため、感染経路や範囲を特定し対策を講じる必要が生じるからです。薬剤感受性のパターンや在院日数などから、外部からの持ち込みか院内伝搬かを推定してきた時代がありましたが、近年は分子疫学的な手法を用いた解析法が使用されています。MRSAの持つDNAの一部を解析することによってそれが同一のクローンであるかを解析する方法です。以前より用いられてきたのがパルスフィールドゲル電気泳動法という方法ですが、手技が煩雑なことにより日常検査としてはあまり普及しませんでした。そこでより簡単に実施することを目的に開発されたのがPOT法です。その菌が同一か否かを識別することに重点を置いた手法であり、(1)高い菌株識別能力(2)半日程度で実施可能な迅速性(3)一般的な実験機器で実施できる簡便さ が特徴です。
POT法はMRSAの持つ複数の遺伝子断片を増幅しその電気泳動パターンをスコア化する手法です。3つの数値で表記され、同一株であれば数値が全て一致します。
操作手順
- 培養したMRSAからDNAを抽出する
- 2種類のマルチプレックスPCR(一度のPCR反応で複数のDNAを同時に増幅する技術)
- アガロースゲル電気泳動
- バンドパターン読み取り
- バンドの有無を0と1に置き換えスコア化しPOT値算出
- 各検体でPOT値の比較解析
POT法導入当初はアガロースゲルを用いた手法を用いてきましたが、操作も解析も時間がかかるのが問題でした。そこでより早く正確なデータを得るためキャピラリー電気泳動装置(図3)というアガロースゲルに代わる装置を導入しています。
泳動したゲルを染色・撮影し、目視でバンドの有無を確認していた従来法(図4左)と比較して、所要時間が大幅に短縮(図4右)されたことに加え、図5のようにデータがデジタル化されたことにより解析もより簡便になりました。図5は図4右の縦1列の電気泳動の詳細を示します。
データの解析
得られた電気泳動のパターンをスコア化しPOT1-3の3つの数値で表します。表1は実際に測定・解析したデータになりますが、赤枠で囲った2つのサンプルは3つの数字がすべて一致しています。したがってこの2つのMRSAは同一のクローンである可能性が考えられます。
ICTでの活用
毎週行われているICTカンファレンスではMRSAの検出状況を報告しており、持ち込みか院内感染かを判断しています。入院日数や過去歴に加えてPOT番号も表記することでより正確に状況を把握することが可能となりました。同じ病棟で複数のMRSAが検出された場合、検出されたMRSAのPOT番号がすべて同じであれば院内伝搬が疑われ、さらに感染対策をすべき範囲も検討をつけることができます。
POT法とキャピラリー泳動法が導入されたことにより短時間で大量の分枝疫学解析を行うことができるようになりました。当院ではMRSAのほかにClostridioides difficile, Pseudomonas aeruginosa, Acinetobacter sp, Enterobacter cloacae complex等、院内感染対策に重要な細菌のPOT法も実施可能となっています。検査室では今後も迅速で詳細な情報を提供できるように新しい技術にも積極的に取り組んでいきたいと思います。
がんゲノム医療の検体作製について
病理検査室 中山友理香
「がんゲノム医療」という言葉を聞いたことがあるでしょうか。がんゲノム医療とは、がん患者さんによって異なるがんの遺伝子変化を調べ、その情報に基づいて診断や治療を行う医療のことです。これまでのように体の”どこに”がんができたかで治療を考えるのではなく、がんの原因となる遺伝子の変化に着目します。遺伝子の変化は「がん遺伝子パネル検査」などで見つけます。がん遺伝子パネル検査では、一度に数十から数百の遺伝子を調べます。現在、がん遺伝子パネル検査を受けることができる病院はがんゲノム医療中核拠点病院やがんゲノム医療拠点病院、がんゲノム医療連携病院に限られています。当院はがんゲノム医療連携病院のため検査を受けることが可能です。病理検査室ではがん遺伝子パネル検査用の検体作製を行っていますが、がん遺伝子パネル検査では適した検体を作製することが重要です。がん遺伝子パネル検査用の検体作製についてご紹介します。
がん遺伝子パネル検査用の検体はがん組織検体や血液です。病理検査室ではがん組織検体を用いて検体作製を行います。がん組織検体は始めに通常の病理検査を行うため、組織診の手順で検査を進めます(詳しくは2015年4月更新分のTEKARIのバックナンバーをご覧ください)。がん遺伝子パネル検査用の検体では固定時間も大切なので、固定不足や固定しすぎにならないように検査をしています。
組織診用に提出されたがん組織検体はがん細胞のみで構成されているわけではなく、壊死や出血を伴ったり、様々な成分で構成されています。がん遺伝子パネル検査ではがん細胞の遺伝子の変化を確認するため、がん細胞の多く含まれる検体が適しています。がん細胞の含まれる割合を腫瘍含有率といいます。組織診後にがん遺伝子パネル検査を行うことが決定したら、病理医が組織診で作製したブロックの中から腫瘍含有率の高いブロックを選びます。
ブロックが決まったら、薄切をします。他院で病理検査を行いがん遺伝子パネル検査で使用できるブロックをお持ちの方の当院での検体作製はここからになります。がん組織検体の大きさや腫瘍含有率によって含まれる遺伝子の量が異なるため、ブロック毎に薄切枚数を確認し、決定した枚数分薄切を行います。5μmの厚さの未染色標本を10枚以上薄切し、最後の1枚はHE染色をします。すべての工程に共通することですが、コンタミネーションに気をつけます。がん遺伝子パネル検査用の薄切を行う前は作業場を患者さん毎に清掃します。使用する刃や水、手袋など使い捨てできる物は患者さん毎に新しい物を使用します。薄切者はマスク、手袋を着用し薄切をします。別患者さんの検体からのコンタミネーションとともに、薄切者からのコンタミネーションも防ぎます。
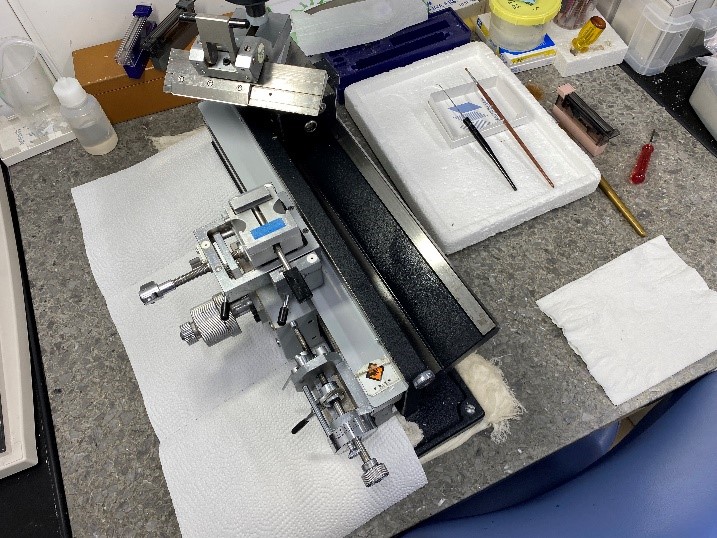
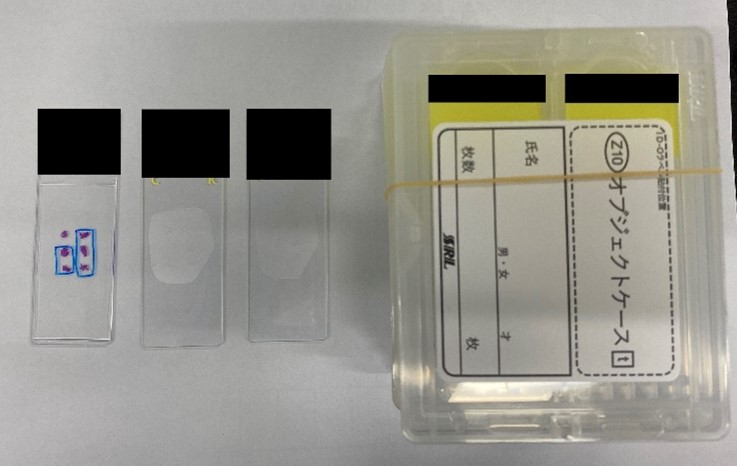
がん遺伝子パネル検査には注意点がいくつかあります。
・がん遺伝子パネル検査は①標準治療がない固形がん②局所進行もしくは転移があり、
標準治療が終了した固形がんの患者さんが対応です。また、全身状態の確認も行われます。
・現段階では検査を受けて、治療につながる割合は10~20%と報告されています。
臨床検査技術部では患者さんが適切な治療を受けられるよう日々業務に取り組んでいます。また、更新される知識をアップデートし、医療に貢献できるよう勉強会などにも参加しています。
参考文献
・がん情報サービス
https://ganjoho.jp/
・遺伝センター Genome & Genetics Center 神戸市立医療センター中央市民病院
https://chuo.kcho.jp/department/genetics/
臨床検査技術部実績
検査実績 2024年度
| 部門名称 | 項目 | 件数 |
|---|---|---|
| 緊急検査 | 生化学・血液検査など | 957,229 |
| 採血 | 外来採血室 | 147,337 |
| 腹部エコー | 腹部超音波 | 8,901 |
| 造影超音波 | 151 | |
| 体表エコー | 体表(乳腺・甲状腺・血管等)超音波 | 3,210 |
| 頭頸部エコー | 頭・頸部超音波 | 2,427 |
| 心エコー | 経胸壁心臓超音波 | 13,865 |
| 経食道心超音波 | 524 | |
| 運動負荷心超音波 | 51 | |
| 薬物負荷心超音波 | 13 | |
| 心電図 | 安静心電図 | 27,477 |
| 肺機能 | 肺機能 | 2,658 |
| 聴力平衡・神経機能 | 聴力平衡機能 | 6,104 |
| 神経機能検査 | 805 | |
| 脳波 | 脳波 | 1,379 |
| 輸血 | ABO血液型検査 | 16,388 |
| 抗体スクリーニング検査 | 20,923 | |
| 輸血製剤 | 自己血 | 197単位 |
| 赤血球濃厚液 | 14,958単位 | |
| 新鮮凍結血漿 | 8,555単位 | |
| 濃厚血小板 | 30,890単位 | |
| アルブミン製剤 | 1,361単位 | |
| 微生物 | 微生物検査 | 14,8078 |
| 結核検査 | 6,643 | |
| 微生物迅速検査 | 159,774 | |
| 感染症スクリーニング検査 | 79,935 | |
| 細胞遺伝子 | フローサイトメトリー | 3,064 |
| 造血器腫瘍遺伝子検査 | 5,249 | |
| 日和見感染症ウイルス検査 | 1,306 | |
| 骨髄像検査 | 759 | |
| 病理 | 組織検査 | 15,204 |
| 細胞診検査 | 9,511 | |
| 免疫抗体 | 13,578 | |
| 解剖件数 | 26 | |
| 検体検査 | 生化学検査 | 5,426,592 |
| 免疫検査 | 246,685 | |
| 血液検査 | 867,717 | |
| 尿一般検査 | 125,431 | |
| 治験・臨床研究 | 取扱い件数 | 1,252 |
各種認定資格取得者数
| 部門名称 | 項目 | 件数 |
|---|---|---|
| 病理 | 国際細胞検査士 | 3名 |
| 細胞検査士 | 13名 | |
| 二級臨床検査士 | 7名 | |
| 認定病理検査技師 | 4名 | |
| 輸血 | 認定輸血検査技師 | 3名 |
| 細胞治療認定管理師 | 9名 | |
| 生理検査 | 超音波検査士(消化器) | 9名 |
| 超音波検査士(循環器) | 12名 | |
| 超音波検査士(体表臓器) | 6名 | |
| 超音波検査士(血管) | 1名 | |
| 超音波検査士(泌尿器) | 1名 | |
| 超音波検査士(健診) | 1名 | |
| 超音波指導検査士(腹部) | 1名 | |
| 二級臨床検査士(呼吸生理学) | 1名 | |
| 認定技術師(術中脳脊髄モニタリング) | 2名 | |
| 専門技術師(神経伝導) | 1名 | |
| 専門技術師(脳波) | 1名 | |
| 血管診療技師 | 2名 | |
| フットケア指導士 | 1名 | |
| 微生物 | 認定臨床微生物検査技師 | 1名 |
| 感染制御認定微生物検査技師 | 1名 | |
| 二級臨床検査士(微生物) | 3名 | |
| 細胞遺伝子 | 遺伝子分析科学認定士 | 2名 |
| 検体検査 | 認定血液検査技師 | 5名 |
| 認定一般検査技師 | 2名 | |
| 認定救急検査技師 | 1名 | |
| 二級臨床検査士(臨床化学) | 4名 | |
| 二級臨床検査士(血液学) | 8名 | |
| 二級臨床検査士(免疫血清学) | 1名 | |
| その他 | NST専門臨床検査技師 | 1名 |
| 認定クリニカル・トキシコロジスト | 1名 | |
| 一般毒物劇物取扱者 | 6名 | |
| 特定化学物質及び四アルキル鉛等作業主任者 | 7名 | |
| 有機溶剤作業主任者 | 7名 | |
| エックス線作業主任者 | 1名 | |
| 第2種ME技術者 | 1名 | |
| 臓器移植院内コーディネータ | 2名 | |
| 肝炎医療コーディネーター | 1名 | |
| 医療情報技師 | 1名 | |
| 医用画像情報専門技師 | 1名 | |
| 医療安全管理者 | 3名 | |
| 化学物質管理者 | 6名 | |
| 糖尿病療法指導士 | 1名 |
所属学会
| 日本医真菌学会 | 日本医療情報学会 | 日本化学療法学会 |
| 日本環境感染学会 | 日本感染症学会 | 日本肝臓学会 |
| 日本検査血液学会 | 日本循環器病学会 | 日本静脈経腸栄養学会 |
| 日本心エコー図学会 | 日本神経生理学会 | 日本性感染症学会 |
| 日本造血細胞移植学会 | 日本組織細胞化学会 | 日本中毒学会 |
| 日本超音波医学会 | 日本超音波検査学会 | 日本聴覚医学会 |
| 日本フットケア学会 | 日本分子生物学会 | 日本脈管学会 |
| 日本輸血細胞治療学会 | 日本臨床衛生検査技師会 | 日本臨床化学学会 |
| 日本臨床救急医学会 | 日本臨床検査医学会 | 日本臨床細胞学会 |
| 日本臨床生理学会 | 日本臨床微生物学会 | 脳神経超音波学会 |
| 病理技術研究会 | 日本臨床検査自動化学会 | 日本医用画像情報専門技師会 |
採用情報
レジデント制度について
当院では、臨床検査技師のレジデント制度を採用しています。
その目的は、実務経験に基づいた講義と臨床実務実習を通じて、高度専門医療に対応した臨床検査並びにチーム医療を実践できる臨床検査技師を育成することです。
教育体制
レジデント制度における研修は、全部門研修を3ヶ月、その後専門研修を21ヶ月の計2年間のプログラムで行います。詳細は以下の通りです。
全部門研修
全部門(輸血検査管理室・細胞遺伝子検査室・病理検査室・微生物検査室・生理検査室)において研修をおこない、臨床検査全般の知識を習得する。
専門研修
下記の専門コースを1つ選択し、それぞれの専門分野における知識・技術を習得する。
輸血・細胞治療コース
1年目は、輸血一般業務の取得、および細胞調製作業を中心とした研修体制とする。2年目は、認定輸血検査技師、細胞治療認定管理師など希望する資格取得を目指した研修を行う。資格取得条件を満たしていない場合でも、同様の研修を行うため、今後の資格取得や輸血・細胞治療のキャリア構築にも大きなプラスとなる。
造血器腫瘍検査コース
1年目は、造血器腫瘍全般についての知識習得および細胞形態検査(骨髄像の判読)、遺伝子検査、フローサイトメトリー検査の習得を目的とした研修を行う。2年目は、上記検査に加えて新規検査項目の開発に携わりつつ、研修中に得られた実績を学会発表することを最終目的とする。
細胞検査士コース
1年目は、婦人科細胞診の診断と検体処理を重点的に実施し、以降は研修の進行程度に応じて、泌尿器・呼吸器・消化器・体腔液・乳腺・甲状腺等その他の領域の細胞診の診断業務の研修を実施し、全ての部位の細胞診断の習得を目標とする。
臨床微生物検査・感染制御習得コース
1年目は、一般細菌の塗抹・培養・同定・感受性検査を中心に臨床微生物検査の基礎を研修し習得を行う。AMRで問題となる耐性菌検出の習得を目指す。2年目は、1年目の応用に加え、当院のICTチームと活動し、院内の感染制御の習得を中心に研修する。
超音波診断(心臓)コース
1年目は、超音波検査の基礎・原理およびスクリーニング検査についてOJTを中心とした研修からはじめ、疾患を有する症例について臨床実務経験を積むことを主眼とする。2年目は、実務経験を重ねつつ、希望があれば経食道心エコー図検査の補助、術中経食道心エコー図検査の補助、運動・薬物負荷心エコー図検査も研修も行う。また、症例・データ解析についての学会発表や論文作成について研修する。
募集情報はこちら