病理診断医5名と臨床検査技師9名で主に以下の業務を行っています(2023年4月現在)
- 細胞診
- 病理組織診
- 病理解剖
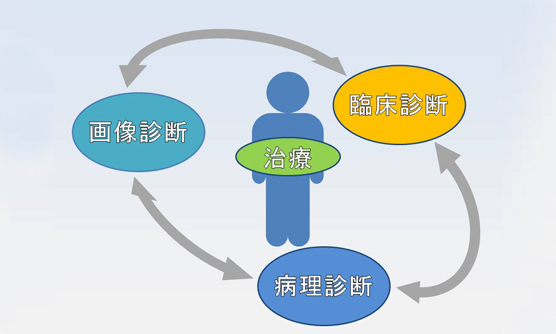
病理診断が臨床に提供する情報には2つの側面があります。
一つは治療方針を立てるためのデータです。炎症か腫瘍か、その種類、広がりなどを診断し、特に癌の診療では重要な鍵を握っています。
もう一つは、疾患理解のための解析です。日々の病理診断で、個々の症例を注意深く調べて、起こっていることを臨床医に還元していく中で、私たち(病理医、臨床医)自身がそれぞれの疾患を深く理解することが、現在、将来の診断、治療の足場を固めていくのだと、私たちは考えています。
広い間口、的確な診断
〈豊富かつ多彩な症例〉

〈正確かつ治療に則した診断〉
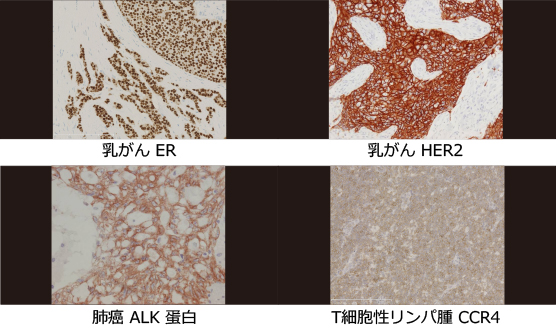
近年、悪性腫瘍(癌、肉腫など)に対する侵襲的な(癌をつぶすために体のほかの部分にも害のある)治療を行うには、病理組織診断がほぼ必須になっています。抗がん剤は「増殖が早い癌細胞を殺す薬」から「特別な種類の癌によく効く薬」に代わりつつあり、病理組織での癌の組織型(癌の種類)の診断が必要ですし、癌組織に起こっている遺伝子異常を調べるには、採取した組織、細胞に問題の腫瘍が含まれているのを顕微鏡で確認しておく必要もあります。新しい検査、新しい治療薬、治療法が次々と導入される今日、臨床の現場で必要とされている情報のポイントは目まぐるしく変化していますし、当院での独自の要求もあります。また、直接話さないと伝わりにくい事もあるので、臨床各科とカンファレンスを積極的に行っています。診断困難症例については、その領域を専門とする病理医にもコンサルトして診断の標準化に努めています。また、治療に関連した乳癌ホルモンレセプターやHER2蛋白、肺癌のALK蛋白、T細胞性リンパ腫のCCR4蛋白をはじめ、免疫染色の約80種類は院内で施行し、診断にかかる期間を圧縮しています。
診療実績
| 年別 | 解剖 | 細胞診 | 組織診 | ||||
| 迅速 | 手術 | 生検 | 他院 | 合計 | |||
| 2014年 | 36 | 11,336 | 869 | 4,383 | 7,698 | 292 | 13,242 |
|---|---|---|---|---|---|---|---|
| 2015年 | 36 | 11,338 | 896 | 4,851 | 8,081 | 301 | 14,129 |
| 2016年 | 34 | 11,337 | 955 | 5,785 | 7,811 | 331 | 14,882 |
| 2017年 | 37 | 11,509 | 977 | 5,825 | 8,628 | 380 | 15,810 |
| 2018年 | 28 | 10,975 | 1001 | 5,674 | 8,450 | 422 | 15,547 |
| 2019年 | 24 | 10,070 | 953 | 5,987 | 8,453 | 435 | 15,828 |
| 2020年 | 23 | 8,854 | 783 | 5,547 | 6,493 | 297 | 13,120 |
| 2021年 | 24 | 9,668 | 727 | 6,068 | 6,689 | 323 | 13,807 |
| 2022年 | 19 | 9,716 | 677 | 6,165 | 7,302 | 467 | 14,611 |
| 2023年 | 23 | 9,638 | 587 | 6,060 | 7,452 | 445 | 14,544 |
| 2024年 | 27 | 9,510 | 648 | 6,237 | 7,825 | 490 | 15,200 |
主な疾患・治療法
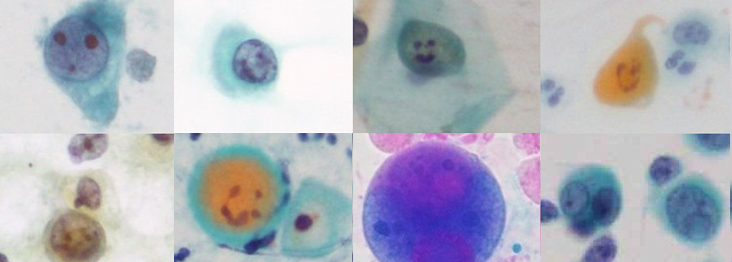
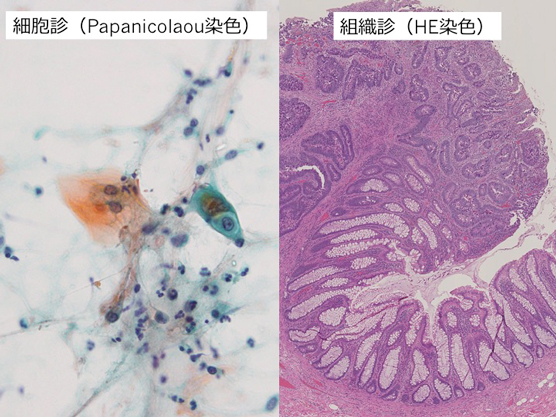
あらゆる臓器や体液から得られた細胞を顕微鏡で検査し、主に細胞形態から良悪の判定を行っています。細胞検査士がスクリーニング(細胞診では、異常な細胞をふるい分けること)を行い、異常な細胞がある場合には、細胞診専門医と共に診断しています。
採取方法と標本作成
| 穿刺吸引細胞診 | 穿刺針を用いて病変部を刺し、陰圧をかけながら抜き取って細胞を採取します。甲状腺、乳腺、肺、リンパ節など。 |
|---|---|
| 自然剥離細胞診 | 喀痰、尿、体腔液(胸水、腹水、心嚢液)など |
| 擦過細胞診 | 綿棒や専用のブラシで粘膜のこすって、取れた細胞をスライドガラスに塗抹(薄く塗り付け)ます。子宮頚部、膣部、子宮内膜など。 |
| 洗浄細胞診 | 気管支鏡検査や手術の最中に、生理食塩水などで腹膜や胸膜を洗って、吸い出した液から細胞をとります。気管支肺胞洗浄液、体腔(腹腔、胸腔)洗浄液など |
細胞採取後、素早くスライドガラスに塗布します。液体検体の場合は、遠沈後(遠心分離機を用いて細胞成分を沈殿させること)、得られた細胞をスライドガラスに塗抹します。95%エタノールで固定しパパニコロウ染色や乾燥固定ではギムザ染色等、目的に合わせて染色し、標本作製します。その標本を顕微鏡で観察し、細胞形態から良悪の判断をしています。生検より細い針なので、出血が少なく、患者さんの負担が軽く、何度も調べられます。組織塊の立体構造はわかりにくく、腫瘍の亜型分類には向いていません。
当院では
必要に応じて、細胞診標本から免疫染色を行ったり、残った検体がある場合にはセルブロック標本を作成するなど、細胞診の良悪の判定だけでなく、組織型や原発巣の推定まで検討しています。症例によっては、液状化検体から細胞標本を作成し(LBC;Liquid based cytology)、診断しています。
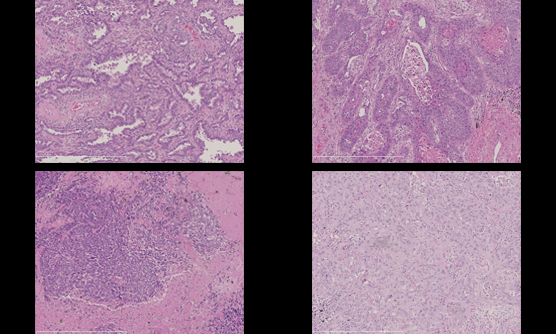
生検や手術検体から標本作製し、組織像を観察します。良悪だけでなく、病変の広がりや病態の把握に努めます。
病理組織診とは?
標本作製から診断
生検および手術で摘出された臓器・組織はホルマリンで固定されます。固定が完了していれば翌日に割を入れて病変や検体の肉眼観察を行い、診断に必要な箇所を選択し必要な数だけ組織をカセットに包埋します。脱水・脱脂を経て、パラフィン浸透させ、パラフィンブロックを作成します。パラフィンブロックの状態になると、薄く切ることができるので、おおよそ3〜5μmの薄さに切った標本をスライドガラスの上に載せます(薄切)。このままの状態では、何も見えないので、組織ではヘマトキシリン・エオジン染色を行い、顕微鏡で病理医が観察します。病変の質的診断だけでなく、必要に応じて、病変の広がりや切除断端の評価も行います。ホルモン療法や化学療法の感受性など、免疫染色を加えて検索します。
当院では
病理専門医が最終診断しています。診断にかかる日数は、おおよそ生検検体で採取後2〜3日、手術検体でおおよそ1〜2週間を目標に診断していますが、症例によっては、追加で免疫染色が必要な場合や、骨や石灰化成分が含まれる場合には、脱灰操作(切りやすくする操作)が必要な場合があり、更に標本作製や診断に日数がかかってしまうことがあります。
また、特殊な領域(リンパ腫関連、腎生検、肝生検)に関しては、院外の専門家の協力を得て診断しています。難解な症例は、国内外の専門家にコンサルテーションしています。
消化器(内科、外科、放射線診断科)、血液リンパ腫(血液内科)、乳腺(乳腺外科、細胞診検査士、超音波技師)、中枢神経(脳外科)、女性生殖器(産婦人科)、泌尿器(泌尿器科)、腎生検(腎臓内科)のカンファレンスを毎週行っています。

術中迅速診断とは?
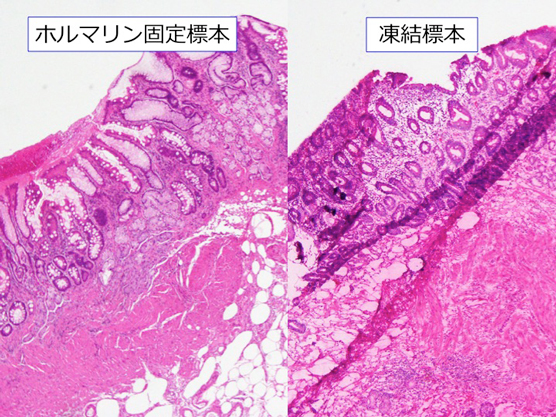
当院では
標本はできるだけ複数の病理医で確認し、提出から診断までおおよそ30分以内に、執刀医に診断を伝えるようにしています。検体数が多い場合や標本作製が難しい検体の場合には、少し時間がかかってしまうことがあります。手術後、凍結標本を解凍して、通常の病理組織診検体と同様にホルマリン固定し、包埋・薄切・染色を施行して、2〜3日後に診断の確認をしています。

病理解剖とは?
病理解剖とは、病気のために亡くなられた患者さんのご遺体を解剖し、臓器、組織、細胞を直接観察して詳しい医学的検討を行うことです。これによって精度の高い病理診断ができ、死因を正しく理解し、病変の広がりや治療の適切性、生前には判明していなかった病変についても検討することができます。
ご遺族の了承のもとに、病理医と臨床検査技師により、院内の専用施設で行われます。主に胸部、腹部を切開し、臓器を取り出して検索します。必要に応じて脳や脊髄も取り出して検索します。また、生前の経過によっては、その他の組織、血液なども採取して検索することがあります。
当院は教育病院でもありますので、当科の専攻医の教育だけでなく、若手臨床医の研鑽の支援も病理医の重要な勤めです。なかでも病理解剖は、彼らが今後より良い医療を提供し、独善的でない臨床医として成長する上で欠くべからざるものです。我々の力及ばず、主治医から病理解剖をお願いした際には、ご理解、ご協力お願いいたします。
当院では
死体解剖保存法で定められた死体解剖資格を持った病理医が執刀しています。標準的な胸部・腹部解剖では、おおよそ2〜3時間程度ですが、脳解剖がある場合や手術後の状態、体格によっては更に時間がかかる場合があります。胸部から下腹部にかけて切開されますが、解剖終了後、縫合し着衣した状態でご遺族のもとにお返しいたします。着衣の状態では、見えない部分で切開、縫合を行っています。脳の検索のため頭部切開を行った場合も、正面からは切開した傷が見えないようにして、縫合しています。
解剖終了後、必要に応じて組織標本を作成し、数ヶ月後に病理解剖診断書をまとめ、主治医に報告されます。症例によっては、CPC(臨床病理検討会)で、臨床経過と病理所見を提示し、診断や治療の妥当性、画像や検査所見の整合性や矛盾点などを担当医や病理医だけでなく様々な科の医師、初期臨床研修医、他職種を交えて議論しています。
詳しくは、病理学会HPも御覧ください。臨床研究
臨床研究
| 研究課題名 | 主任研究者 | 当院責任者 | 承認日 | 状態 | 説明文 (PDF) |
| 腎生検で診断の得られた足細胞陥入糸球体症の疾患概念の確立と臨床像および病理学的特徴の検討 |
清水 章 |
原 重雄 神戸市立医療センター中央市民病院 病理診断科 |
2025/9/22 | 進行中 | |
| 骨髄肉腫を対象としたFUS-ERG融合遺伝子とERG発現の観察研究
|
上原慶一郎 |
山下大祐 神戸市立医療センター中央市民病院 病理診断科 |
2024/5/14 | 進行中 | |
|
骨軟部腫瘍における治療標的・予後因子の解明 |
小田義直 |
原 重雄 神戸市立医療センター中央市民病院 病理診断科 |
2023/10/11 | 進行中 | |
|
病理組織検体を活用した造血器腫瘍の臨床病理学的研究 |
加留部謙之輔 |
山下大祐 神戸市立医療センター中央市民病院 病理診断科 |
2023/8/10 | 進行中 | |
|
腎癌・腎腫瘍の臨床病理学的検討とゲノム病理データベース構築 |
大橋瑠子 |
原 重雄 神戸市立医療センター中央市民病院 病理診断科 |
2022/12/2 | 進行中 | |
|
血管内リンパ腫の臨床病理学的及び遺伝学的解析 |
藤倉航平 ブリティッシュコロンビア大学 生命科学研究所 遺伝医学部門 |
山下大祐 神戸市立医療センター中央市民病院 病理診断科 |
2022/4/5 | 進行中 | |
| 病理診断にもとづく成人ランゲルハンス細胞組織球症(LCH)の疫学研究 | 東條有伸 東京大学医科学研究所附属病院 血液腫瘍内科 |
山下大祐 神戸市立医療センター中央市民病院 病理診断科 |
2020/11/19 | 進行中 |
お知らせ
当院病理で研修、就職を希望される方へ
専攻医
当院の病理診断プログラムは、地域の市中病院や大学とも連携するプログラムであり、詳細は下記をご参照下さい。
当院病理では、肉眼所見から組織所見への連続的、立体的な理解と、臨床情報との関連付けを重視しています。病理解剖と典型的な手術症例、生検症例がほぼ一人で診断できることを当初の目標に、各科とのカンファレンス、担当臓器の当番を繰り返しながら、研修を進めており、病理医としての経歴の早いうちに基本的なことを身につけておきたいという方にお勧め出来る研修内容です。院内、地方会などでのプレゼンテーションの機会が多いのも、臨床医と直接話をして彼らの考え方を知る機会が多いのも病院ならではです。
病理の専門研修プログラムはこちら紹介患者の院外標本は年々増加し、昨年は435件ありました。紹介元での病理組織診断が間違っていることは実際にはほとんどありませんが、当院での標本との組織像の比較が必要な場合があります。当院で化学療法、放射線療法や手術などの侵襲的な治療を行うにあたっては、悪性であることの確認や、治療法、薬剤の選択の為の組織型の確認が必要です。病理標本をぜひ紹介状に添えていただけるようにお願いいたします。
当院では病理医外来を行っておりません。
病理医が一般の患者さんに病理所見をご説明する病理医外来を開いている病院が増えつつありますが、当院ではその余裕がありません。病変の分布図を作成し、院内の検討会で臨床医に説明して、臨床医からご説明するのを支援しておりますのでご容赦ください。